Abstract
Introduction
External fixation can be performed in poor bone and soft tissue conditions, and can be used in patients with poor general conditions or multiple injuries as a rapid, mini-invasive procedure. The purpose of the current study was to evaluate the effectiveness and safety of the Ilizarov external fixator in the management of proximal humeral fractures.
Materials and methods
Between May 2011 and December 2013, 14 patients with displaced proximal humeral fractures were enrolled in the current study. Nine patients were males and five were females, with mean age 42.9 years (range 21–55). All fractures were acute. The mode of injury was road traffic accident in eight patients and fall in six patients. There were six patients with two-part fracture, one of them with fracture dislocation, and eight patients presented with three-part fracture, two of them with fracture dislocation. All fractures were fixed using the Ilizarov external fixation.
Results
The average operative time was about 67 min (range 50–90). The mean follow-up period was (18) months (range 12–28). Healing was obtained in all 14 patients in a mean of 10.4 weeks (range 8–14). At the final follow-up, the mean constant score was 73.1 points (range 60–97 points), the mean visual analog score (VAS) for pain 3.2 (range 1–5), the mean DASH score 31.8 points (range 10–55 points), and the mean satisfaction VAS 7.6 (range 4–10).
Conclusion
The Ilizarov external fixation is an effective technique in managing proximal humeral fractures with good outcome and low complication rates.
Level of evidence
Level IV, case series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since Neer [1] published his classification system of proximal humeral fracture with a clear definition of displaced fractures, a significantly high agreement on treatment recommendation was found among experienced shoulder surgeons. Low agreement, however, was found about fixation modality [2], with variable fixation techniques, including closed or open reduction and fixation with wires, plates, sutures, or external fixators [3].
External fixation can be performed in poor bone and soft tissue conditions, so it is the fixation modality of choice in open fractures, or in fractures with soft tissue compromise, hindering open reduction and internal fixation. External fixators could be also used in patients with poor general conditions or multiple injuries as a rapid, mini-invasive procedure [4].
The proximal humerus fracture, as demonstrated by Codeman [5], consists of four main fragments: the articular fragment, the greater tuberosity, the lesser tuberosity, and the shaft, with each of the latter three parts deformed in a different direction by the pull of the attached muscles. Such complex fracture configuration makes fixation by a monoplanar external fixator difficult. A review of the literature revealed only a few reports on external fixation of proximal humeral fractures [6,7,8] and only one case series of the Ilizarov external fixation in open proximal humeral fractures [9].
The purpose of the current study was to evaluate the effectiveness and safety of the Ilizarov external fixator in the management of proximal humeral fractures. We hypothesize that the Ilizarov external fixator could provide rigid fixation for proximal humeral fractures, with low rate of complications.
Patients and methods
Between May 2011 and December 2013, 14 patients with displaced proximal humeral fractures were enrolled in the current study. The inclusion criteria were displaced proximal humeral fractures. Exclusion criteria included floating shoulder injury or previous shoulder fracture or pathologies such as advanced arthritis or rotator cuff arthropathy. Displacement was defined as translation of a fracture fragment more than 1 cm, or angulations of more than 45° [1].
The study was approved by the ethical committee of the university. All patients signed an informed consent after a clear explanation of the procedure and alternative options.
All patients were examined clinically, with a record of the soft tissue condition and neurovascular status especially the axillary nerve. Radiologic evaluation included anteroposterior (AP) and lateral scapular X-rays that were used to classify the fractures according to Neer classification [1]. CT scans were done for all patients for further evaluation of fracture configuration.
Operative technique
All patients underwent surgery under general anesthesia. Patients were positioned supine with the arm in slight abduction, on an orthopedic table, with access for intraoperative fluoroscopy.
Closed reduction was attempted, under image control in case of fracture without dislocation. If the reduction was satisfactory, assembly of the Ilizarov began from proximal to distal. If the reduction was not satisfactory, a 2 mm K-wire was used as a joystick to assist reduction. In case of fracture dislocation, closed reduction of the humeral head was achieved by inserting a 6 mm cancellous half-pin attached to a T-handle in the head through the fracture under image control, followed by gently gliding and levering the head inside the glenoid.
The first step of the Ilizarov assembly was to insert a 5 or 6 mm cancellous half-pin from lateral to medial in the humeral head and to stop 1 cm away from the articular surface in the subchondral bone. A second and third half-pin were then inserted from the anterolateral and posterolateral positions, keeping the proximal arch in a perpendicular position to the head in both transverse and sagittal planes.
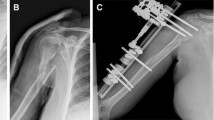
The second step was insertion of a distal arch below the insertion of the deltoid muscle, at the junction of the middle and lower one-third of the humerus in the safe zones. The last step was manipulation of both arches to adequate reduction, followed by connecting the distal and proximal arches (Fig. 1).
Postoperative care and follow-up
Patients were encouraged to start passive shoulder exercises as soon as possible after surgery. After 2 weeks, active assisted exercises were allowed. By the 6th week, active exercises were encouraged. Routine pin care was explained to all patients.
Follow-up X-rays were done postoperatively and every 2 weeks till union, then every month for the next 6 months and then annually thereafter. Each time, the stability of the construct was tested. Removal of the fixator was done after complete fracture union under general anesthesia.
At the final follow-up constant score, Disabilities of the Arm Shoulder snd Hand (DASH) score, visual analog score (VAS) for pain, and VAS for patient satisfaction were recorded. Satisfaction was recorded as 0–10 score where 10 was fully satisfied and 0 not satisfied at all. The shoulder range of motion was recorded using a goniometer (Fig. 2).
a Preoperative X-ray showing displaced surgical neck fracture. b, c, d Postoperative photograph, immediate postoperative with pendular exercises and active assisted range of motion, respectively. e Postoperative radiograph with signs of union. f Photograph at last follow-up showing external rotation. g Photograph at last follow-up showing internal rotation. h Radiograph 3 months after removal of the fixator
Results
Nine patients were male and five were female, with a mean age 42.9 years (range 21–55). The mode of injury was road traffic accident in eight patients and fall in six patients. All fractures were acute with an average 8 days (range 5–13) from injury. There were six patients with two-part fracture (one of them presented with fracture dislocation) and eight presented with three-part fracture (two of them presented with fracture dislocation).
The average operative time was about 67 min (range 50–90). The mean follow-up period was (18) months (range 12–28). Healing was obtained in all 14 patients in a mean of 10.4 weeks (range 8–14). The fixator was removed 2 weeks after union. The mean time of fixation was 12.42 weeks (range 10, 16). Rehabilitation followed the same protocol used for internal fixation. All patients returned to work by the 4th month.
At the final follow-up, the average postoperative flexion was 148.6° (range 120–180), abduction 137.9° (range 110–170), extension 19.2° (range 5–40), external rotation 37.5° (range 10–50), and internal rotation 30° (range 10–40).
At the final follow-up, the mean Constant score was 73.1 points (range 60–97 points), the mean VAS for pain 3.2 (range 1–5), the mean DASH score 31.8 points (range 10–55 points), and the mean satisfaction VAS 7.6 (range 4–10) (Table 1).
Superficial pin tract infection occurred in ten patients and was managed by local dressing and oral antibiotics. One patient with three-part fracture dislocation developed avascular necrosis (AVN) of the humeral head, but was satisfied and refused any further intervention.
Gradual adjustment of fixation was required in two cases with distraction and varus deformity. No neurovascular complications were met in the current series. There were no cases of nonunion or malunion or secondary displacement.
Discussion
Closed reduction and percutaneous pinning of unstable fractures of the proximal part of the humerus is a well-described technique that minimizes soft tissue dissection with lower risks of infection and AVN, and less blood loss than open techniques [10]. However, difficult reduction, inadequate fixation leading to secondary displacement, and prolonged immobilization leading to stiffness are reported complications [11, 12].
The use of external fixation provides adequate fixation stability while allowing early mobilization. Good or excellent results and minimum complications have been reported compared with open reduction and internal fixation. However, secondary displacement was reported [7, 13].
The Ilizarov fixator is characterized by circular fixation with high stability against bending, shear, and torsion, as well as the probability of adjusting inadequate reduction or secondary displacement during follow-up. Dhar et al. [13] used the Ilizarov apparatus to improve alignment in proximal humeral fractures treated initially by a unilateral external fixator in three patients.
In the current study, we used the Ilizarov external fixation to manage proximal humeral fractures in 14 patients, with union achieved in all the patients after an average of 10 weeks with comparable shoulder functions achieved in other series using external fixators [7, 9, 11, 14] (Table 2).
Our results are also comparable to the results obtained by internal fixation in a systematic review study that included 12 studies with 514 proximal humeral fracture patients treated with locked plates [15]. At the last follow-up, the patients achieved a mean Constant score of 74 and a mean DASH score of 27. The average Constant score and DASH scores in our series were 73.1 and 31.8, respectively.
Sproul et al. in his systematic review of complications following locked plates reported 49% overall rate of complications, including varus malunion 16%, AVN 10%, screw perforation of the humeral head into the joint 8%, subacromial impingement 6%, and infection 4%. The reoperation rate was 14% [15]. To decrease soft tissue compromise, mininvasive proximal humeral plates were used [16]. Ruchholtz et al. reported good outcome results in 80 cases of proximal humeral fracture using a polyaxial locking plate introduced through the mininvasive technique. The complication rate was high with 16.3% of patients requiring revision and two cases with revision twice [17].
Complications were reported after external fixation. Kristiansen and Kofoed [7] in his series of 27 patients treated by Hoffman’s external fixation reported secondary displacement in two patients, deep infection with pin loosening in two, aseptic loosening in two, AVN in two, and nonunion in one. Ebraheim et al. [11] using mini-fixator reported four cases of secondary displacement, two of nonunion, and one of sympathetic dystrophy. In the current study, we reported one case of AVN and ten cases of superficial pin tract infection. We did not report any cases of secondary displacement or nonunion. One major advantage of external fixation is the versatility of correcting secondary displacement. However, we did not have any secondary displacement in our series, probably due to the young age group with good bone quality and adequate fixation stability.
An important limitation of this study was the small number of cases and the lack of comparison with other patients managed with different surgical techniques. In the current study, the presented proximal humeral fracture fixation method needs experience with the techniques of the Ilizarov external fixator.
Conclusion
The Ilizarov external fixation is an effective technique in managing proximal humeral fractures, allowing indirect reduction, without further jeopardizing head blood supply, and stable fixation with the potential ability for later adjustment of fixation.
References
Neer C (1970) Displaced proximal humerus fractures. Part1. Classification and evaluation. J Bone Joint Surg (Am) 52(6):1077–1089
Brorson S (2013) Fractures of the proximal humerus: history, classification, and management. Acta Orthop 84(Supp 351):1–32
Drosdowech D, Faber K, Athwal G (2008) Open reduction and internal fixation of proximal humerus fractures. Orthop Clin N Am 39(4):429–439
Sisk T (1983) External fixation. Historic review, advantages, disadvantages, complications, and indications. Clin Orthop Relat Res 180:15–22
Codman E (1934) Rupture of the supraspinatus tendon and other lesions in or about the subacromial bursa. Thomas Todd, Boston
Martin C, Guillen M, Lopez G (2006) Treatment of 2- and 3-part fractures of the proximal humerus using external fixation: a retrospective evaluation of 62 patients. Acta Orthop 77(2):275–278
Kristiansen B, Kofoed H (1987) External fixation of displaced fractures of the proximal humerus. Technique and preliminary results. J Bone Joint Surg Br 69(4):643–646
Kristiansen B, Kofoed H (1988) Transcutaneous reduction and external fixation of displaced fractures of the proximal humerus. A controlled clinical trial. J Bone Joint Surg Br 70(5):821–824
Karatosun V, Alekberov C, Baran Ö, Serin E, Alici E, Balci C (2002) Open fractures of the proximal humerus treated with the Ilizarov method. Acta Orthop 73(4):460–464
Chen C, Chao E, Ueng S, Shih C (1998) Closed management and percutaneous fixation of unstable proximal humerus fractures. J Trauma 45:1039–1045
Ebraheim N, Wong F, Biyani A (1996) Percutaneous pinning of the proximal humerus. Am J Orthop 25:501–506
Fenichel I, Oran A, Burstein G, Pritsch MP (2006) Percutaneous pinning using threaded pins as a treatment option for unstable two- and three-part fractures of the proximal humerus: a retrospective study. Int Orthop 30(3):153–157
Dhar S, Butt M, Mir M, Ali M, Kawoosa A (2008) Use of the Ilizarov apparatus to improve alignment in proximal humeral fractures treated initially by a unilateral external fixator. Strateg Trauma Limb Reconst 3(3):119–122
Uzer G, Yıldız F, Author E, Elmadağ M, Pulatkan K (2015) Treatment of unusual proximal humeral fractures using unilateral external fixator: a case series. Eur J Orthop Surg Traumatol 25(4):683–687
Sproul R, Iyengar J, Devcic Z, Feeley B (2011) A systematic review of locking plate fixation of proximal humerus fractures. Injury 42(4):408–413
Aguado H, Mingo J, Torres M, Alvarez-Ramos A, Martín-Ferrero M (2016) Minimally invasive polyaxial locking plate osteosynthesis for 3–4 part proximal humeral fractures: our institutional experience. Injury 47(Suppl3):S22–S28
Ruchholtz S, Hauk C, Lewan U, Franz D (2011) CKühne. Minimally invasive polyaxial locking plate fixation of proximal humeral fractures: a prospective study. J Trauma 71(6):1737–1744
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Both authors have no conflict of interest to disclose and did not receive any fund or research grants.
Ethical approval
The study was approved by the ethical committee of Benha University and was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
All patients signed an informed consent after a clear explanation of the surgical procedure.
Rights and permissions
About this article
Cite this article
Meselhy, M.A., Singer, M.S. Management of proximal humeral fractures by the Ilizarov external fixator. Arch Orthop Trauma Surg 137, 1279–1284 (2017). https://doi.org/10.1007/s00402-017-2749-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2749-0