Abstract
Purpose of Review
Proximal humerus fractures are challenging injuries to treat and will become more common with an aging population. The purpose of this paper is to review the recent literature regarding the role of open reduction and internal fixation for this injury.
Recent Findings
Complex proximal humerus fractures present a significant challenge in the elderly. The introduction of locked plating has improved surgical management of these injuries; however, complications including avascular necrosis, primary screw cutout, and secondary screw cutout remain obstacles. Newer technologies aim to combat these issues, with promising early results.
Summary
Complex proximal humerus fractures call for experienced surgeons and remain challenging with high complication rates with open reduction and internal fixation. Newer fixation methods aim to reduce these complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal humerus fractures represent the seventh most common fracture overall and, among patients older than 65, the third most common [1, 2]. As the population ages, this fracture will be encountered more often. In fact, a 2006 study from Finland noted the incidence of these fractures has tripled since 1970 [3]. Efforts to determine optimal treatment of this injury are ongoing since Dr. Charles Neer’s classification and treatment recommendations nearly 50 years ago [4, 5]. Advances in technology such as locked plating and computed tomography have allowed for solutions for poor bone quality as well as improved preoperative evaluation. The purpose of this paper is review the recent literature of geriatric proximal humerus fractures and the role of open reduction internal fixation.
Fracture Evaluation and Classification
Evaluation of proximal humerus fractures begins with a physical exam. Patients will often present with pain, limited range of motion, and ecchymosis about the shoulder. It is important to perform a thorough neurovascular exam since up to one in three can present with nerve injury by physical exam [6, 7]. An EMG study reported the most commonly affected are the axillary, suprascapular, and radial nerves—53, 37, and 24%, respectively. These are felt to be traction injuries with approximately 95% recovering at 3–4 months. It should be noted that sensation about the deltoid does not indicate that the axillary nerve is intact [8]. One suggestion is to place the hands over the deltoid and elbow to feel for deltoid contraction and abduction [9]. About 10% of these patients have an additional fracture, highlighting the importance of a secondary exam [10].
Radiographs including true AP, scapular Y, and axillary views are critical for evaluation. Attention should be paid to the tuberosities and alignment of the glenohumeral joint. Computed tomography (CT) may be helpful in evaluation of the medial calcar or any displacement. In our experience, CT is recommended with three- and four-part fractures and fracture-dislocations to assist in preoperative planning. MRI can be used to evaluate for rotator cuff tear, which can be seen in about 40% of proximal humerus fractures [7].
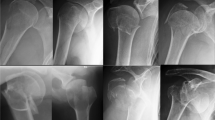
Dr. Charles Neer described four landmarks as the basis for his classification: anatomic neck, surgical neck, greater tuberosity, and lesser tuberosity [4, 5]. A displaced part was represented by minimum 1 cm displacement or angulation of 45° or more. However, these parameters were initially arbitrarily defined with variable interobserver reliability [11]. Additionally, Arbeitsgemeinschaft fur Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) modified the Neer classification and focused on impaction and displacement. The AO/OTA classification was updated in 2018 to better integrate the original Neer classification [12]. These fractures can occur in multiple permutations and include the possibility of anterior or posterior dislocation. From the radiographs, head impaction angle can be measured as described by Hertel [13]. A head inclination angle less than 130° can be considered varus impacted and greater than 140° can be considered valgus impacted (Fig. 1).
AP and axillary radiographs from a 66-year-old female who sustained a left valgus impacted proximal humerus fracture during a motor vehicle collision. She underwent open reduction internal fixation with locked plating. At 3 months follow-up, her four-part fracture had healed and clinically, she was pain free with satisfactory range of motion
Additionally, bone quality can be evaluated on the AP radiographs. There are two widely used techniques: the deltoid tuberosity index (DTI) and the Tingart measurement [14, 15]. Briefly, DTI can be measured at an area just proximal to the deltoid tuberosity where the outer cortical borders are parallel; the ratio between the outer cortical and inner endosteal diameter is referred to as the DTI. A DTI < 1.4 is used to indicate poor bone stock [14]. Separately, the Tingart measurement can be obtained by the ratio of the outer cortical and inner endosteal diameter compared with the same measurement obtained 20 mm distal.
Bone density overall is a predictor of screw cut out as well as reduction quality [16,17,18]. However, bone quality is not associated with Neer fracture patterns; a study by Spross found no correlation between more complex fracture patterns and bone quality [19]. With regard to outcome, multiple studies have demonstrated no significant difference in functional outcome, motion, and complication rates between older and younger geriatric patients with proximal humerus fractures [20,21,22]. In other words, age alone should not be a contraindication for surgical fixation since those who are older can achieve the same outcomes as the younger geriatric population. Another study evaluating outcomes of proximal humerus fractures in the elderly has identified social independence as an important factor in their outcome [10]. This would indicate that physiologic age is a more important factor compared to chronologic age in considering treatment options [23]. Thus, bone quality and social independence can serve as surrogates for physiologic age and hence guide treatment decisions.
Anatomical Considerations
The anatomical deforming forces generally predict fracture displacement, and the humerus is no different. The greater tuberosity is subject to the pull of the supraspinatus, infraspinatus, and teres minor, producing posterosuperior displacement. The subscapularis inserts on the lesser tuberosity and produces medial displacement. Additionally, the humeral shaft is pulled medially due to the pectoralis major. Finally, the deltoid inserts laterally on the humerus, which leads to a lateral deforming force.
The vascular supply to the proximal humerus is provided by the anterior and posterior humeral circumflex arteries, which arise from the axillary artery. The anterior humeral circumflex artery branches superiorly into the arcuate artery, which enters near the anatomic neck [24]. The location of the main vascular supply explains why anatomic neck fractures have a high rate of avascular necrosis whereas valgus-impacted four-part fractures are less at risk compared to other four-part fractures. Hertel determined factors that contribute to avascular necrosis, including a calcar fragment less than 8 mm, disrupted medial hinge, or anatomic neck involvement [25]. The same study found that head-splitting fractures in isolation do not necessarily lead to avascular necrosis. A subsequent study has revealed that head-splitting fractures with associated tuberosity fractures are at risk for avascular necrosis [26]. Notably, avascular necrosis does not necessarily portend a poor outcome; Gerber reported a series of 13 patients with AVN with the majority reporting minimal pain and excellent or good outcome [27]. Injury to the axillary artery has been reported; however, this is very uncommon [28].
The axillary nerve is not often encountered during surgical exposure; however, care should be taken during the approach given its proximity and variability. The axillary nerve is also vulnerable during screw placement near the surgical neck when utilizing anterolateral plates [29]. The radial nerve courses posteriorly down the humeral shaft before turning laterally through the intermuscular septum. Consequently, the radial nerve is at risk when directing screws in a posterior direction when placing shaft screws when using long plates.
Treatment Options
Multiple factors must be considered in determining optimal treatment for geriatric proximal humerus fractures, such as fracture pattern, patient functional status, patient health, and surgeon preference. Additionally, more recent studies emphasized the distinction between physiologic age and chronologic age [10, 22]. Guy et al. surveyed surgeon preference for displaced three- and four-part proximal humerus fractures and found a trend towards surgery for younger patients but no consensus for older patients—45 years old versus 68 [30]. These subjective factors complicate the decision to operate as well as in interpreting studies. In fact, a recent Cochrane review which evaluated over 20 randomized controlled trials concluded that there is insufficient evidence to support treatment recommendations at this time [31]. However, there was significant heterogeneity between the studies, including type of surgical treatment, fracture pattern, and age. Open reduction internal fixation with locked plating was often categorized with arthroplasty in the surgical treatment group, which may confound outcomes. These reports underscore the complexity of geriatric proximal humerus fractures and the multiple factors that contribute towards the decision for surgical intervention.
Generally, the authors recommend a treatment ladder based on the complexity of the fracture pattern. Nondisplaced or minimally displaced fractures of the proximal humerus can be treated successfully without surgery. These types of fractures comprise about 50% of all proximal humerus fractures [32]. Arthroplasty has become a viable treatment option for proximal humerus fractures. A comparison to open reduction internal fixation is beyond the scope of this review, though there are many reports comparing the two with their respective benefits and faults [2, 33,34,35]. When surgery is indicated, our preference is for open reduction internal fixation since it preserves bone stock, maintains the option for arthroplasty, and restores native anatomy. From our experience, indications for arthroplasty include unreconstructable fracture patterns, head-splitting fracture, extruded head with no tuberosity attachment or with significant soft tissue stripping, and presence of chronic massive rotator cuff tear.
Two-Part Fractures
Two-part fractures of the proximal humerus can involve either the surgical neck or the tuberosities and account for 33% of all proximal humerus fractures [32]. Two-part fractures involving the surgical neck that are minimally displaced respond well to nonoperative management with acceptable outcomes [10]. Additionally, fractures involving the greater tuberosity also respond well to nonoperative management if less than 5 mm displacement; however, full recovery may take up to 12 months [36]. Generally, patients with advanced physiologic age and minimal displacement are recommended for nonoperative treatment.
Open reduction internal fixation for two-part proximal humerus fractures involving the surgical neck is most beneficial with significant displacement and, critically, acceptable bone quality. Reoperation rates for locking plate fixation can be up to 30%, with the most common cause being screw cutout [37]. Varus angulation and medial comminution have been shown to be risk factors for complication. Strategies to minimize complications include use of bone graft, divergent screws, and ensuring fixation within the medial calcar [17, 38].
Three- and Four-Part Fractures
Proximal humerus fractures with three or four parts make up about 20% of all proximal humerus fractures [32]. Studies evaluating outcome following nonoperative management reveal low functional scores [10, 39]. However, patients are pain free and report satisfaction with their function. These studies emphasize the need to evaluate functional demand and social independence when managing these fractures. The Proximal Fracture of the Humerus: Evaluation by Randomisation (PROFHER) trial is one of the largest studies available on the topic. The authors found no difference in outcomes between operative and nonoperative management of proximal humerus fractures [40].
Locking plates—also known as angular stable plates—were developed as a solution for reliable fixation in osteoporotic bone. Modern designs include anatomic contouring, multiple options for screw placement into the humeral head, and screw pegs to combat cutout. A cadaveric study has shown the biomechanical superiority of locking plates compared to conventional plates [41]. As a result, there has been an increase in the use of locking plates for proximal humerus fractures and, consequently, more reports in the literature [9].
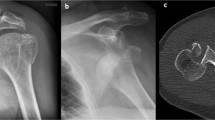
Treatment of three- and four-part fractures with locked plating can be challenging. Multiple studies have shown complication rates up to 49% [42,43,44, 45•]. The most common reported complications are avascular necrosis, malreduction, primary screw cutout, and infection. Due to the divergent screw trajectory and spherical humeral head, it can be difficult to fully evaluate for primary screw cutout inteaoperatively. Spross et al. performed a cadaveric study evaluating primary cutout and determined that standard AP and outlet views may miss nearly half of screw cut outs [46•]. A unique complication with locked plating involves screw penetration through subchondral bone with subsequent articular involvement due to the fixed angle construct [43]. Risk factors for failure include poor bone quality, age, poor reduction of medial calcar, nonanatomic reduction, and tobacco use [18, 47]. The authors noted that the number of risk factors correlated with the failure rate, up to 85.7% failure rate when four risk factors were present [18]. Further analysis reveals risk factors for complications include fracture-dislocation, head-splitting type fractures, and varus displacement [42]. Thus, even with the advantages of modern fixation technology, fixation of complex proximal humerus fractures remains a technically demanding procedure (Fig. 2).
AP and axillary views of a right proximal humerus fracture from a 60-year-old female sustained from a ground level fall. She underwent open reduction internal fixation with locked plating. Four weeks postoperatively, she developed persistent pain to her right shoulder. AP and axillary views demonstrate subchondral collapse of the humeral head with screw penetration. She subsequently underwent removal of hardware
Despite the high reported complication rate, functional outcomes following locked plating of proximal humerus fractures are acceptable. Brunner et al. reported a Constant score of 72 after 12 months among 157 patients with an average age of 55 [48]. Sproul et al. performed a systematic review that included over 500 patients with an average age of 62 [44]. At a mean follow-up of 29 months, they reported a Constant score of 74. Additional studies also report Constant scores in the same range [49,50,51]. Sudkamp et al. noted in their study that the majority of their complications were due to surgical technique; thus, they conclude that locked plating can provide good functional outcomes with a low complication rate. This has been consistent with the author’s personal experience. Strategies to optimize outcome include anatomic reduction, hardware visualization, and periosteal preservation.
Managing three- or four-part proximal humerus fractures with poor bone quality is of particular interest in this patient population. The use of a fibular strut allograft to provide additional structural support combined with locked plating has shown promising results. Hinds et al. reported a Constant score of 83 using this technique in geriatric patients [21]. Additionally, a systematic review of use of these grafts found a reoperation rate of 4.4%, significantly lower than that seen with locked plating alone [52]. While total patients are relatively low, these results are promising.
Future Directions
Technological advancements will continue to combat the problem of poor bone quality. Newer generation locking plates are available, and early results are encouraging. Rodia et al. reported 1 year follow-up of 54 patients with proximal humerus fractures treated with an updated locking plate and noted a Constant score of 75 with only five complications, none of which required revision surgery [53]. Schliemann et al. reported good functional scores at 2 years using a carbon fiber reinforced polyetheretherketone plate [54].
Problem areas remain which include potential screw penetration particularly with valgus impacted fractures which can settle and result in intra-articular screw penetration. Solutions include the use of pegs instead of screws as well as allograft cortical struts. A newer device which shows promise is an expandable nitinol mesh cage for the proximal humerus (Conventus, Minneapolis, MN). This cage provides a broad surface area to support a valgus impacted head as well as fills the void present in the intertubercular area in elderly osteoporotic patients. This lack of bone combined with poor medial support is likely the reason varus angulated fractures are still problematic. Fulkerson et al. reported a significantly decreased reoperation rate when using this device compared to historical controls (5.6 vs 19%) [55•]. The cage can provide medial support as well as a surface for screws to gain purchase (Fig. 3).
Imaging from a 72-year-old female who sustained a left complex proximal humerus fracture from a ground level fall. CT reveals poor bone stock that would complicate reconstruction. She underwent open reduction internal fixation with a proximal humerus cage. Radiographs at 3 months reveal healing fracture with no evidence of complication. Clinically, her range of motion was close to her uninjured side and she was pain free
Conclusions
Complex proximal humerus fractures remain a challenging problem for orthopedic surgeons. Technological advancements have improved fracture evaluation and surgical management, however, complications remain prevalent. The authors advocate for open reduction and internal fixation in order to restore native anatomy and preserve the option for arthroplasty. Future technologies designed to reduce complications are promising.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–7 Available from: http://linkinghub.elsevier.com/retrieve/pii/S0020138306003238.
Nho SJ, Brophy RH, Barker JU, Cornell CN, MacGillivray JD. Management of proximal humeral fractures based on current literature. J Bone Joint Surg Am. 2007 [cited 2014 May 8];89(Suppl 3):44–58. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17908870.
Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006;442:87–92 Available from: http://www.ncbi.nlm.nih.gov/pubmed/16394745.
Neer CS. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077–89 Available from: http://www.ncbi.nlm.nih.gov/pubmed/5455339.
Neer CS. Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am. 1970;52(6):1090–103 Available from: http://www.ncbi.nlm.nih.gov/pubmed/5455340.
Fjalestad T, Hole MØ, Blücher J, Hovden IAH, Stiris MG, Strømsøe K. Rotator cuff tears in proximal humeral fractures: an MRI cohort study in 76 patients. Arch Orthop Trauma Surg. 2010;130(5):575–81 Available from: http://www.ncbi.nlm.nih.gov/pubmed/19685061.
Gallo RA, Sciulli R, Daffner RH, Altman DT, Altman GT. Defining the relationship between rotator cuff injury and proximal humerus fractures. Clin Orthop Relat Res. 2007;458:70–7 Available from: http://www.ncbi.nlm.nih.gov/pubmed/17308477.
Visser CP, Tavy DL, Coene LN, Brand R. Electromyographic findings in shoulder dislocations and fractures of the proximal humerus: comparison with clinical neurological examination. Clin Neurol Neurosurg. 1999;101(2):86–91 Available from: http://www.ncbi.nlm.nih.gov/pubmed/10467902.
Green A. Proximal humerus fractures and fracture-dislocations. In: Browner BD, Jupiter J, Krettek C, Anderson P, editors. Skeletal trauma: basic science, management, and reconstruction, vol. 2. 5th ed. Philadelphia: Elsevier/Saunders; 2015. p. 1423–53.
Clement ND, Duckworth AD, McQueen MM, Court-Brown CM. The outcome of proximal humeral fractures in the elderly: predictors of mortality and function. Bone Joint J. 2014;96–B(7):970–7 Available from: http://www.ncbi.nlm.nih.gov/pubmed/24986953.
Bernstein J, Adler LM, Blank JE, Dalsey RM, Williams GR, Iannotti JP. Evaluation of the Neer system of classification of proximal humeral fractures with computerized tomographic scans and plain radiographs. J Bone Joint Surg Am. 1996;78(9):1371–5 Available from: http://www.ncbi.nlm.nih.gov/pubmed/8816653.
Meinberg E, Agel J, Roberts C. Fracture and dislocation classification compendium 2018. J Orthop Trauma. 2018;32 1–170 p.
Hertel R, Knothe U, Ballmer FT. Geometry of the proximal humerus and implications for prosthetic design. J Shoulder Elb Surg. 2002;11(4):331–8 Available from: http://linkinghub.elsevier.com/retrieve/pii/S1058274602000216.
Spross C, Kaestle N, Benninger E, Fornaro J, Erhardt J, Zdravkovic V, et al. Deltoid tuberosity index: a simple radiographic tool to assess local bone quality in proximal humerus fractures. Clin Orthop Relat Res. 2015;473(9):3038–45 Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s11999-015-4322-x.
Mather J, MacDermid JC, Faber KJ, Athwal GS. Proximal humerus cortical bone thickness correlates with bone mineral density and can clinically rule out osteoporosis. J Shoulder Elb Surg. 2013;22(6):732–8 Available from: http://www.ncbi.nlm.nih.gov/pubmed/23183030.
Spross C, Zeledon R, Zdravkovic V, Jost B. How bone quality may influence intraoperative and early postoperative problems after angular stable open reduction–internal fixation of proximal humeral fractures. J Shoulder Elb Surg. 2017;26(9):1566–72 Available from: http://linkinghub.elsevier.com/retrieve/pii/S1058274617301337.
Jung S-W, Shim S-B, Kim H-M, Lee J-H, Lim H-S. Factors that influence reduction loss in proximal humerus fracture surgery. J Orthop Trauma. 2015;29(6):276–82 Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00005131-201506000-00004.
Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger FS. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011;42(11):1283–8 Available from: http://www.ncbi.nlm.nih.gov/pubmed/21310406.
Mazzucchelli RA, Jenny K, Zdravkovic V, Erhardt JB, Jost B, Spross C. The influence of local bone quality on fracture pattern in proximal humerus fractures. Injury. 2018;49(2):359–363. https://doi.org/10.1016/j.injury.2017.12.020
Grawe B, Le T, Lee T, Wyrick J. Open reduction and internal fixation (ORIF) of complex 3- and 4-part fractures of the proximal humerus. Geriatr Orthop Surg Rehabil. 2012;3(1):27–32 Available from: http://journals.sagepub.com/doi/10.1177/2151458511430662.
Hinds RM, Garner MR, Tran WH, Lazaro LE, Dines JS, Lorich DG. Geriatric proximal humeral fracture patients show similar clinical outcomes to non-geriatric patients after osteosynthesis with endosteal fibular strut allograft augmentation. J Shoulder Elb Surg. 2015;24(6):889–96 Available from: http://linkinghub.elsevier.com/retrieve/pii/S1058274614005850.
Goch AM, Christiano A, Konda SR, Leucht P, Egol KA. Operative repair of proximal humerus fractures in septuagenarians and octogenarians: does chronologic age matter? J Clin Orthop Trauma. 2017;8:50–3.
Schumaier A, Grawe B. Proximal humerus fractures: evaluation and management in the elderly patient. Geriatr Orthop Surg Rehabil. 2018;9:215145851775051.
Rockwood C. The shoulder. 4th ed. Philadelphia: Saunders; 2009.
Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elb Surg. 13(4):427–33 Available from: http://www.ncbi.nlm.nih.gov/pubmed/15220884.
Gavaskar AS, Tummala NC. Locked plate osteosynthesis of humeral head-splitting fractures in young adults. J Shoulder Elb Surg. 2015;24(6):908–14 Available from: http://www.ncbi.nlm.nih.gov/pubmed/25476989.
Gerber C, Hersche O, Berberat C. The clinical relevance of posttraumatic avascular necrosis of the humeral head. J Shoulder Elb Surg. 7(6):586–90 Available from: http://www.ncbi.nlm.nih.gov/pubmed/9883418.
Thorsness R, English C, Gross J, Tyler W, Voloshin I, Gorczyca J. Proximal humerus fractures with associated axillary artery injury. J Orthop Trauma. 2014;28(11):659–63 Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00005131-201411000-00009.
Ninck J, Heck S, Gick S, Koebke J, Pennig D, Dargel J. Versorgung von Humeruskopffrakturen. Unfallchirurg. 2013;116(11):1000–5 Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s00113-012-2242-8.
Guy P, Slobogean GP, McCormack RG. Treatment preferences for displaced three- and four-part proximal humerus fractures. J Orthop Trauma. 2010;24(4):250–4 Available from: http://www.ncbi.nlm.nih.gov/pubmed/20335760.
Handoll HHG, Brorson S. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2015;11(11):CD000434 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26560014.
Bergdahl C, Ekholm C, Wennergren D, Nilsson F, Möller M. Epidemiology and patho-anatomical pattern of 2,011 humeral fractures: data from the Swedish Fracture Register. BMC Musculoskelet Disord. 2016;17(1):159 Available from: http://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-016-1009-8.
Burkhart KJ, Dietz SO, Bastian L, Thelen U, Hoffmann R, Müller LP. The treatment of proximal humeral fracture in adults. Dtsch Arztebl Int. 2013;110(35–36):591–7 Available from: http://www.ncbi.nlm.nih.gov/pubmed/24078839.
Gallinet D, Clappaz P, Garbuio P, Tropet Y, Obert L. Three or four parts complex proximal humerus fractures: hemiarthroplasty versus reverse prosthesis: a comparative study of 40 cases. Orthop Traumatol Surg Res. 2009;95(1):48–55 Available from: http://linkinghub.elsevier.com/retrieve/pii/S1877056808000042.
Thorsness R, Iannuzzi J, Noyes K, Kates S, Voloshin I. Open reduction and internal fixation versus hemiarthroplasty in the management of proximal humerus fractures. Geriatr Orthop Surg Rehabil. 2014;5(2):56–62 Available from: http://journals.sagepub.com/doi/10.1177/2151458514527292.
Rath E, Alkrinawi N, Levy O, Debbi R, Amar E, Atoun E. Minimally displaced fractures of the greater tuberosity: outcome of non-operative treatment. J Shoulder Elb Surg. 2013;22(10):e8–11 Available from: http://linkinghub.elsevier.com/retrieve/pii/S1058274613000906.
Olerud P, Ahrengart L, Söderqvist A, Saving J, Tidermark J. Quality of life and functional outcome after a 2-part proximal humeral fracture: a prospective cohort study on 50 patients treated with a locking plate. J Shoulder Elb Surg. 2010;19(6):814–22 Available from: http://linkinghub.elsevier.com/retrieve/pii/S1058274609005382.
Newman JM, Kahn M, Gruson KI. Reducing postoperative fracture displacement after locked plating of proximal humerus fractures: current concepts. Am J Orthop (Belle Mead NJ). 2015;44(7):312–20 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26161759.
Zyto K. Non-operative treatment of comminuted fractures of the proximal humerus in elderly patients. Injury. 1998;29(5):349–52 Available from: http://www.ncbi.nlm.nih.gov/pubmed/9813677.
Handoll HH, Keding A, Corbacho B, Brealey SD, Hewitt C, Rangan A. Five-year follow-up results of the PROFHER trial comparing operative and non-operative treatment of adults with a displaced fracture of the proximal humerus. Bone Joint J. 2017;99–B(3):383–92 Available from: http://online.boneandjoint.org.uk/doi/10.1302/0301-620X.99B3.BJJ-2016-1028.
Hessmann MH, Hansen WSM, Krummenauer F, Pol TF, Rommens PM. Locked plate fixation and intramedullary nailing for proximal humerus fractures: a biomechanical evaluation. J Trauma. 2005;58(6):1194–201 Available from: http://www.ncbi.nlm.nih.gov/pubmed/15995470.
Solberg BD, Moon CN, Franco DP, Paiement GD. Locked plating of 3- and 4-part proximal humerus fractures in older patients: the effect of initial fracture pattern on outcome. J Orthop Trauma. 2009;23(2):113–9 Available from: https://insights.ovid.com/crossref?an=00005131-200902000-00006.
Spross C, Platz A, Rufibach K, Lattmann T, Forberger J, Dietrich M. The PHILOS plate for proximal humeral fractures—risk factors for complications at one year. J Trauma Acute Care Surg. 2012;72(3):783–92 Available from: http://www.ncbi.nlm.nih.gov/pubmed/22491570.
Sproul RC, Iyengar JJ, Devcic Z, Feeley BT. A systematic review of locking plate fixation of proximal humerus fractures. Injury. 2011;42(4):408–13 Available from: http://www.ncbi.nlm.nih.gov/pubmed/21176833.
• Gupta AK, Harris JD, Erickson BJ, Abrams GD, Bruce B, McCormick F, et al. Surgical management of complex proximal humerus fractures—a systematic review of 92 studies including 4500 patients. J Orthop Trauma. 2015;29(1):54–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25162974. Updated systematic review of current literature regarding complex proximal humerus fracture.
• Spross C, Jost B, Rahm S, Winklhofer S, Erhardt J, Benninger E. How many radiographs are needed to detect angular stable head screw cut outs of the proximal humerus—a cadaver study. Injury. 2014;45(10):1557–63 Cadaveric study illustrating difficulty in verifying screw placement intraoperatively.
Osterhoff G, Hoch A, Wanner GA, Simmen H-P, Werner CML. Calcar comminution as prognostic factor of clinical outcome after locking plate fixation of proximal humeral fractures. Injury. 2012;43(10):1651–6 Available from: http://www.ncbi.nlm.nih.gov/pubmed/22579397.
Brunner F, Sommer C, Bahrs C, Heuwinkel R, Hafner C, Rillmann P, et al. Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma. 2009;23(3):163–72 Available from: http://www.ncbi.nlm.nih.gov/pubmed/19516088.
Südkamp N, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg Am. 2009;91(6):1320–8 Available from: http://www.ncbi.nlm.nih.gov/pubmed/19487508.
Solberg BD, Moon CN, Franco DP, Paiement GD. Surgical treatment of three and four-part proximal humeral fractures. J Bone Joint Surg Am. 2009 [cited 2014 May 21];91(7):1689–97. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19571092.
Xu J, Zhang C, Wang T. Avascular necrosis in proximal humeral fractures in patients treated with operative fixation: a meta-analysis. J Orthop Surg Res. 2014;9(1):31 Available from: http://josr-online.biomedcentral.com/articles/10.1186/1749-799X-9-31.
Saltzman BM, Erickson BJ, Harris JD, Gupta AK, Mighell M, Romeo AA. Fibular strut graft augmentation for open reduction and internal fixation of proximal humerus fractures. Orthop J Sport Med. 2016;4(7):232596711665682 Available from: http://journals.sagepub.com/doi/10.1177/2325967116656829.
Rodia F, Theodorakis E, Touloupakis G, Ventura A. Fixation of complex proximal humeral fractures in elderly patients with a locking plate: a retrospective analysis of radiographic and clinical outcome and complications. Chinese J Traumatol = Zhonghua chuang shang za zhi. 2016;19(3):156–9 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27321296.
Schliemann B, Hartensuer R, Koch T, Theisen C, Raschke MJ, Kösters C, et al. Treatment of proximal humerus fractures with a CFR-PEEK plate: 2-year results of a prospective study and comparison to fixation with a conventional locking plate. J Shoulder Elb Surg. 2015;24(8):1282–8 Available from: http://linkinghub.elsevier.com/retrieve/pii/S1058274615000142.
• Fulkerson E, Paterson P. Proximal humeral fracture fixation using the PH Cage: a retrospective study of 125 patients to a minimum of 6 months post treatment. In: Orthopaedic Trauma Association Annual Meeting 2017. 2017. p 162. Early results of proximal humerus cage construct showing lower complication rate.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
John Wyrick reports personal fees from Stryker and Smith and Nephew, outside the submitted work. Rafael Kakazu declares no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Geriatric Orthopedics
Rights and permissions
About this article
Cite this article
Kakazu, R., Wyrick, J.D. Management of Complex Proximal Humerus Fractures: What Is the Role of Open Reduction and Internal Fixation?. Curr Geri Rep 7, 264–271 (2018). https://doi.org/10.1007/s13670-018-0261-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-018-0261-1