Abstract
Introduction
Cementless fixation of the tibial component is critical as reduced initial stability leads to implant failure. In this experimental in vitro study, a new fixation method of the tibial component using polyaxial locking screws is evaluated using Roentgen stereophotogrammetric analysis (RSA).
Materials and Methods
A special prototype of a tibial component with four polyaxial locking screws was tested on 10 fresh-frozen human tibia specimens. The components were tested with an axial load of 2000 N for 10,000 cycles. Radiographs in two views were performed before loading, after 1000 and after 10,000 cycles, respectively. Besides rotation and translation along the x-, y-, and z-axes, endpoints for RSA were maximum subsidence (MaxSub), maximum lift off (MaxLiftOff) and maximum total point motion (MTPM).
Results
MaxSub increased from −0.5 mm (SD = 0.2) after 1000 cycles to −0.9 mm (SD = 1.1). MaxLiftOff was 0.1 mm after 1000 cycles and did not increase after 10,000 cycles. The MTPM was 0.7 mm (SD = 0.3) after 1000 cycles and 1.1 mm (SD = 1.1) after 10,000 cycles. Two out of nine implants showed an MTPM ≥ 1.0 mm after 10,000 cycles.
Conclusions
Polyaxial locking screws can potentially improve the initial stability of tibial components. The results of this study indicate that the use of such screws in total knee arthroplasty may be of interest in the future. Further experimental and clinical investigation is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cementing of total knee arthroplasties (TKA) as the fixation method provides excellent short- and long-term ability [8, 29, 31, 41, 51]. Nevertheless, aseptic loosening, especially of the tibial component remains an unsolved problem of cemented TKA [16, 21, 45].
Some Roentgen stereophotogrammetric analysis (RSA) studies have shown that the initial stability of cemented tibial components is excellent, whereas migration processes of the prostheses increase over the years [35, 39]. This migration can potentially lead to implant failure.
This is problematic since the requirements concerning the longevity and durability of total knee replacements have risen over recent years because more and more younger patients need TKA [22, 25, 31]. Therefore, there has been renewed interest in cementless fixation methods.
Although hydroxyapatite (HA) coated TKA have led to improved initial stability [17, 34, 36, 37], cementless fixation methods remain controversial mainly due to inferior initial stability. RSA studies comparing cementless and cemented TKA have shown a higher amount of migration of cementless TKA during the first postoperative years [7, 39]. These movements are of importance: It could be demonstrated that sizable early migration is a predictor for later loosening of the prosthesis [32, 48]. Therefore, screw augmentation has been used to improve the initial stability of cementless TKA [14, 62]. However, there are some reports about problems with conventional bone screws [5, 15, 28].
Cementless designs with screws typically use conventional non-locking polyaxial screws. The use of polyaxial and locking screws for fixation of tibial components in TKA has, to the authors’ best knowledge, not yet been described in the literature. In traumatology, uniaxial locking plate systems improve the durability of osteosynthesis, especially in complex and unstable fractures [6, 24, 58]. Some experimental and clinical trials compared uni- and polyaxial locking plates and showed very good biomechanical features for both groups [3, 9, 38, 40, 60]. The authors consider the higher amount of flexibility while inserting the screws as one of the main advantages of polyaxial systems compared to uniaxial systems.
This experimental, radiostereogrammetric in vitro study seeks to evaluate the influence of a new cementless fixation method using polyaxial locking screws on the migration and initial stability of tibial components.
Methods
The prototype
To conduct the examination of a cementless fixation method with polyaxial locking screws, a prototype of a tibial tray was constructed in the biomechanical craft centre of the Department of Orthopaedics and Rheumatology at the University Hospital, Marburg, Germany.
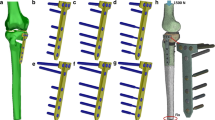
The tibial tray is made of steel. On the lower surface of the tibial component, there are four cones with screw holes for the corresponding polyaxial locking screws (Fig. 1). These cones are impacted into the tibial bone. The screws can be inserted at a polyaxial angle of 30°. The locking mechanism is achieved by screw nuts that can be placed in the threaded screw holes of the prostheses (Fig. 2). The polyethylene (PE) inlay is fixed to the prostheses with two central screws. Figure 3 provides an overview of all parts of the prototype.
The locking mechanism was constructed according to the polyaxial locking plate system NCB® (Zimmer, Warsaw, IN, USA). The NCB system is used for the stabilisation of complex bone fractures [12, 13, 19, 46, 47].
Implantation process, cyclic loading and radiological assessment
The prototype was implanted in 10 fresh-frozen human tibia specimens from the Anatomical Institute of the University of Düsseldorf, Germany. Since the prototype was not available in different sizes, the specimen were chosen according to the diameter of the prototype to eliminate the bias of size mismatch.
Before the implantation process, all soft tissue was removed from the tibia. Preparation of the specimens was performed with original Genesis II TKA system instruments for uncemented implants (Smith & Nephew, Schenefeld, Germany). First, the extramedullary tibial alignment guide and cutting block were assembled. The proximal tibia was cut at 8 mm with a posterior slope of 3°. After resection of the tibial condyles, the prosthesis was impacted into the tibial bone. Then, four screw channels were bored into the cancellous bone and the screws were inserted. After locking of the screws, the PE inlay was placed.
For RSA analysis, at least eight tantalum markers of 1.0 mm diameter were placed in the apophysial part of the tibia specimen. All markers were put in randomly using a special applicator (RSA Biomedical, Umeå, Sweden). Furthermore, seven markers were added to the PE inlay in a predefined arrangement.
Before cyclic loading, an initial radiograph using standardised RSA technique was taken of each tibial specimen. After removal of the PE inlay, the specimens were put in a special holder and fixed with cement. This holder was then mounted in a computer-controlled universal testing machine (81806-EDC100, Frank, Weinheim, Germany). Testing of the specimens was done with an axial load of 2.000 N epitomising the approximate peak load during a physiological walking cycle of a patient weighing 70 kg [33]. The axial forces of the testing machine could be applied on the main weight-bearing zone of the tibial component using a special utility which could be adapted to the size of the prosthesis. There were no rotational or angular forces applied to the prostheses. A total of 10,000 loading cycles were performed, representing the axial forces acting on the operated knee during the first 8 postoperative weeks.
Radiostereogrammetric analysis
Before and after loading for 1000 and 10,000 cycles, respectively, a radiograph using standardised RSA technique was taken (Fig. 4). All radiographs were taken simultaneously in two views (anteroposterior and mediolateral). For this purpose, each specimen was put in a special Plexiglass-Cage (RSA Biomedical, Umeå, Sweden) in a neutral position. The cage consists of four walls with incorporated tantalum markers in a defined position. The simultaneous acquisition of the radiographs was performed with two X-ray tubes arranged in an orthogonal position (Multix Up, resp. Vertix, Siemens AG, Forchheim, Germany). Afterwards, all pictures were digitalised with an AGFA ADC Compact (Agfa HealthCare, Cologne, Germany) and exported to import them to the RSA software (UMRSA 4.1, RSA BioMedical, Umeå, Sweden).
The endpoints of the RSA were translational and rotational movements along the x-, y- and z-axes. Furthermore, maximum subsidence (MaxSub), maximum lift off (MaxLiftOff) and maximum total point motion (MTPM) were measured. Prosthesis failure was defined as MTPM > 1.0 mm. The three-dimensional configuration of the tantalum markers representing a segment (bone and inlay) is considered as a rigid body [56]. Within the testing process, the RSA software checks for dislocation of the tantalum markers. In case of extensive tantalum marker dislocation, the respective marker cannot be used for determination of the rigid body model. If less than three stable tantalum markers are available the calculation of a rigid body is not possible.
According to Adalberth et al., the accuracy of this RSA method is 0.1° for all rotational movements, and 0.1 mm for all translations, MaxSub, MaxLiftOff and MTPM, respectively [1].
Statistical analysis
Statistical analysis was done with SPSS for Windows, Version 11.0 (SPSS Inc., Chicago, IL, USA). G*Power, Version 3.1.9.2 (University of Kiel, Germany) was used for power analysis to determine the sample size. Power analysis was conducted using Wilcoxon signed-rank test (one sample case), a significance level of 0.05, and a power of 80 %. Normality was tested using Kolmogorov–Smirnov Test. Since there was no Gaussian normal distribution, the migration values were compared using the nonparametric Mann–Whitney U test. For all statistical tests, a significance level of p < 0.05 was used.
Results
Group descriptives
Altogether 5 left-sided and 5 right-sided specimens were used. After the implantation process, one right-sided specimen had to be excluded due to extensive tantalum marker dislocation.
There were 5 male and 4 female donors with a mean age of 81.9 years (SD = 10.6)
Rotational and translational migration
There were low overall rotational and translational migration values of the tibial component. The highest amount of rotation both after 1000 (0.3°, SD = 0.4) and 10,000 cycles (0.8°, SD = 1.0) was observed around the x-axis and the highest amount of translation was found along the y-axis (1000 cycles −0.2 mm, SD = 0.2; 10,000 cycles −0.6 mm, SD = 0.8). The changes after both testing cycles were statistically insignificant (p > 0.05, Table 1).
MaxSub, MaxLiftOff and MTPM
After 1000 cycles of loading, the tibial component had subsided −5 mm (SD = 0.2). During the following loading cycles, the prosthesis continued subsiding but without statistical significance (−0.9 mm, SD = 1.1, p > 0.05). There was only a minimal amount of lift off after 1000 cycles (0.1 mm, SD = 0.0); during the following 9000 cycles, further lift off was not observed. The MTPM rose from 0.7 (SD = 0.3) to 1.1 mm (SD = 1.1). The results are summarised in Table 2.
The analysis revealed one outlier: in that case, the MTPM was 3.8 mm after 10,000 cycles. The average MTPM without the outlier was 0.7 mm after 10,000 cycles. Based on a limit value of ≥ 1.0 mm for MTPM after 10.000 cycles, 2 out of 9 (22 %) implants exceeded the critical value. When excluding the outlier, 1 out of 8 (12.5 %) implants failed.
Discussion
The aim of this study was to evaluate the influence of a polyaxial fixed-angle fixation method on the initial stability of the tibial component of TKA using the RSA technique.
After 1000 and 10,000 cycles, respectively, the prototype with polyaxial locking screws showed low overall migration values. Among the 9 tested specimen, there was one with a much higher MTPM score was observed. The most likely explanation for this outlier is the presence of micro-fractures that can occur during the implantation- and loading-process [10].
Compared to previous in vitro RSA examinations from our group that have been performed under the same testing circumstances in the same laboratories with comparable specimen regarding gender and age, the performance of the prototype used in this study is excellent, especially when compared to a conventional cementless fixation with tibial stem and four non-locking screws. Efe et al. found a median MTPM of 5.9 mm after 10,000 cycles of loading; MaxSub was −2.5 mm and MaxLiftOff was 1.3 mm [11]. Under the same testing circumstances, there were lower migration values for the prototype with polyaxial locking. Skwara et al. compared two types of cementing of tibial components in another in vitro examination. The setting of the examination was the same as in this study. After 10,000 cycles, the mean MTPM for the tibial component with surface cementing was 0.9 mm which is similar to the MTPM found in our investigation. The tibial component with deep stem cementing showed much higher migration values (MTPM = 2.6 mm) [52]. In contrast, Luring et al. found a higher MaxiLiftOff in cases where only the tibial baseplate was cemented compared to a fully cemented tibial tray [30].
In further in vitro studies, various cementless designs have been evaluated with regards to their initial stability.
One study showed that a fixation with pegs alone and tibial stem alone do not provide a sufficient initial stability. A combination of tibial stem and non-locking screws showed the lowest migration values [23]. Sumner et al. compared three different designs with regards to bony ingrowth [55] and migration [54] in an animal model. The tibial stem with non-locking screws only showed the lowest migration and the highest amount of osseointegration. The prosthesis with screws and pegs showed a comparable migration but worse bony ingrowth. A fixation with pegs alone led to higher migration values compared to the other fixation methods. However, pegs and a bladed tibial stem have shown to improve rotational stability [59]. Similarly, Volz and colleagues found the lowest amount of migration for the Anatomic Modular Knee (non-locking screws plus tibial stem) and the Miller Galante I (non-locking screws plus pegs) [57]. These results contrast with the migration values of the cementless Genesis II component with tibial stem and four non-locking screws found in the study of Efe et al. [11]. An important factor leading to these controversy results might be the fact that, the success of a fixation with non-locking screws appears to be directly dependent on bone quality and density [27].
The 10,000 cycles of loading used in this examination represent the forces acting on the knee during the first 8–12 weeks.
Various clinical RSA studies have been performed. Ryd et al. found migration of more than 1 mm in the first 6–12 postoperative weeks [48]. Carlsson et al. and Albrektsson et al. described similar results after 3 months (0.9 mm [7] and 1.2 mm [4]).
Comparing our results with the findings for cementless tibial components of clinical RSA studies after 8–12 weeks, the prototype with polyaxial locking screws shows excellent migration behaviour. Without the outlier, the mean MTPM was 0.7 mm. However, comparison with clinical studies is difficult since in vivo effects like osteolysis or bone ingrowth could not be simulated.
In two studies, there are lower MTPM scores (approx. 0.4 mm) for the Miller Galante II prosthesis [44, 49]. A comparable MTPM was found for the Tricon Stem [18] and PFC [7, 39]. In most studies, there is an MTPM exceeding 1 mm [4, 18, 42, 48, 50]. Compared to HA-coated tibial components, the prototype with polyaxial locking screws shows intermediate migration results [7, 39, 43, 44].
Most RSA studies found MTPM scores between 0.3 and 0.5 mm for cemented tibial components after 12 weeks [7, 43, 48, 50]. Wilson and colleagues found 0.5 mm motion after 6 months [61].
Despite higher initial migration values, cementless TKA appear to stabilise over time, whereas cemented TKA continues to migrate [7, 35, 39]. Carlsson et al. concluded that cementless designs could perform equally or even better than cemented designs if the problem of worse initial stability could be solved [7]. An important step was the development of HA coating [2, 36].
To improve the initial stability of cementless designs, additional screw augmentation has been evaluated over the past 20 years. Various experimental studies have shown that additional fixation in combination with pegs or a tibial stem can improve the initial stability of tibial components [23, 26, 54, 55, 59, 63]. However, in clinical trials using these two types of cementless TKA, screw-related osteolysis was observed in 12–55 % of cases, leading to aseptic loosening in 8–23 % [5, 28, 53]. On the other hand, there are positive results concerning clinical and radiological criteria in two clinical trials using the Natural Knee TKA [14, 20]. This might indicate that not only the use of screws but also other factors such as manufacturing, design and porous coating have an influence on the appearance of radiolucent lines around screws [14]. As a consequence, it appears to be possible to reduce screw associated osteolysis by optimising the aforementioned factors. This is of importance if the presented prototype is used in a clinical series.
Bone quality seems to be of particular importance for the success of cementless TKA [26, 27]. The use of screws and an additional central stem seems to increase initial stability especially in patients with poor bone quality [26]. In this study, we did not measure bone density prior to the experiments which is one of the limitations of this study. However, the sample can be considered representative due to the relatively high mean age (81.9 years) and balanced ratio between male and female specimen. Nevertheless, the impact of bone quality on the migration of our prototype remains unclear.
A possible explanation for the encouraging results of the prosthesis fixed with polyaxial locking screws is the excellent biomechanical attributes of the prototype attributed to the use of polyaxial locking screws [9, 40]. Besides firm fixation, the flexibility that is obtained by the possibility of adapting the angle of the screws seems to be of importance [60]. During the experiments, we tried to choose an angulation that was oriented on the physiological load axis of the tibia.
A limitation of this study is the type of loading. Cyclic loading of the prostheses with only axial forces can only approximately be considered physiological. Furthermore, this study is lacking a control group as well as a bone density measurement prior to the experiments. In addition, we did not examine the influence of screw position on migration of the prosthesis.
Despite these limitations, the findings in this study are well comparable, especially to the previous studies performed by our group; Another strength of the study is the fact that this is the first study to examine the use of polyaxial locking screws for the fixation of tibial components. Furthermore, we used a well-established and accurate method for measuring migration.
Conclusions
Fixation with polyaxial locking screws offered a strong initial fixation with a low amount of migration. This new fixation method could potentially improve the initial stability of tibial components. To confirm the good results of this study, further experimental and clinical investigation is needed. Further studies should include various control groups such as a group of non-locking screws, screws plus keel and keel fixation only. Additionally, bone density should be measured prior to the experiments and the influence of screw angulation should be examined.
References
Adalberth G, Nilsson KG, Kärrholm J, Hassander H (2002) Fixation of the tibial component using CMW-1 or Palacos bone cement with gentamicin: similar outcome in a randomized radiostereometric study of 51 total knee arthroplasties. Acta Orthop Scand 73(5):531–538
Akizuki S, Takizawa T, Horiuchi H (2003) Fixation of a hydroxyapatite-tricalcium phosphate-coated cementless knee prosthesis. Clinical and radiographic evaluation seven years after surgery. J Bone Joint Surg Br 85(8):1123–1127
Al-Mouazzen L, Chou DT, Kyriakopoulos G, Hambidge J (2014) Polyaxial versus uniaxial volar locking plate for distal radial fractures. J Orthop Surg (Hong Kong) 22(1):9–12
Albrektsson BE, Carlsson LV, Freeman MA, Herberts P, Ryd L (1992) Proximally cemented versus uncemented Freeman-Samuelson knee arthroplasty. A prospective randomised study. J Bone Joint Surg Br 74(2):233–238
Berger R, Lyon J, Jacobs J, et al (2001) Problems with cementless total knee arthroplasty at 11 years followup. Clin Orthop Relat Res 392:196–207
Biggi F, Di Fabio S, D’Antimo C, Trevisani S (2010) Tibial plateau fractures: internal fixation with locking plates and the MIPO technique. Injury 41(11):1178–1182
Carlsson A, Bjorkman A, Besjakov J, Onsten I (2005) Cemented tibial component fixation performs better than cementless fixation: a randomized radiostereometric study comparing porous-coated, hydroxyapatite-coated and cemented tibial components over 5 years. Acta Orthop 76(3):362–369
Cournapeau J, Klouche S, Bauer T, Hardy P (2015) Survival and functional results after a mean follow-up of 9 years with the Ceragyr® highly congruent mobile-bearing TKA. Orthop Traumatol Surg Res 101(4):455–460
Cullen A, Curtiss S, Lee M (2009) Biomechanical comparison of polyaxial and uniaxial locking plate fixation in a proximal tibial gap model. J Orthop Trauma 23(7):507–513
Dodd CA, Hungerford DS, Krackow KA (1990) Total knee arthroplasty fixation. Comparison of the early results of paired cemented versus uncemented porous coated anatomic knee prostheses. Clin Orthop Relat Res (260):66–70
Efe T, Figiel J, Danek S, Tibesku CO, Paletta JR, Skwara A (2011) Initial stability of tibial components in primary knee arthroplasty. A cadaver study comparing cemented and cementless fixation techniques. Acta Orthop Belg 77(3):320–328
El-Zayat BF, Ruchholtz S, Efe T et al (2012) NCB-plating in the treatment of geriatric and periprosthetic femoral fractures. Orthop Traumatol Surg Res 98(7):765–772
Erhardt JB, Grob K, Roderer G, Hoffmann A, Forster TN, Kuster MS (2008) Treatment of periprosthetic femur fractures with the non-contact bridging plate: a new angular stable implant. Arch Orthop Trauma Surg 128(4):409–416
Ferguson RP, Friederichs MG, Hofmann AA (2008) Comparison of screw and screwless fixation in cementless total knee arthroplasty. Orthopedics 31(2):127
Goldberg VM, Kraay M (2004) The outcome of the cementless tibial component: a minimum 14-year clinical evaluation. Clin Orthop Relat Res 428:214–220
Gunst S, Fessy MH (2015) The effect of obesity on mechanical failure after total knee arthroplasty. Ann Transl Med 3(20):310
Hansson U, Ryd L, Toksvig-Larsen S (2008) A randomised RSA study of Peri-Apatite HA coating of a total knee prosthesis. Knee 15(3):211–216
Hilding MB, Lanshammar H, Ryd L (1996) Knee joint loading and tibial component loosening. RSA and gait analysis in 45 osteoarthritic patients before and after TKA. J Bone Joint Surg Br 78(1):66–73
Hoffmann MF, Lotzien S, Schildhauer TA (2016) Clinical outcome of interprosthetic femoral fractures treated with polyaxial locking plates. Injury 47(4):934–938
Hofmann A, Evanich J, Ferguson R, Camargo M (2001) Ten- to 14-year clinical followup of the cementless natural knee system. Clin Orthop Relat Res 388:85–94
Khan M, Osman K, Green G, Haddad FS (2016) The epidemiology of failure in total knee arthroplasty: avoiding your next revision. Bone Joint J 98-B(1 Suppl A):105–112
Kim YH, Park JW, Kim JS (2016) A comparison of 5 models of total knee arthroplasty in young patients. J Arthroplast 31(5):994–999
Kraemer WJ, Harrington IJ, Hearn TC (1995) Micromotion secondary to axial, torsional, and shear loads in two models of cementless tibial components. J Arthroplasty 10(2):227–235
Lattmann T, Meier C, Dietrich M, Forberger J, Platz A (2011) Results of volar locking plate osteosynthesis for distal radial fractures. J Trauma 70(6):1510–1518
Lee JH, Barnett SL, Patel JJ, Nassif NA, Cummings DJ, Gorab RS (2016) Ten Year Follow-Up of Gap Balanced, Rotating Platform Total Knee Arthroplasty in Patients Under 60 Years of Age. J Arthroplasty 31(1):132–136
Lee RW, Volz RG, Sheridan DC (1991) The role of fixation and bone quality on the mechanical stability of tibial knee components. Clin Orthop Relat Res 273:177–183
Lee TQ, Barnett SL, Kim WC (1999) Effects of screw types in cementless fixation of tibial tray implants: stability and strength assessment. Clin Biomech (Bristol, Avon) 14(4):258–264
Lewis PL, Rorabeck CH, Bourne RB (1995) Screw osteolysis after cementless total knee replacement. Clin Orthop Relat Res 321:173–177
Long WJ, Bryce CD, Hollenbeak CS, Benner RW, Scott WN (2014) Total knee replacement in young, active patients: long-term follow-up and functional outcome: a concise follow-up of a previous report. J Bone Joint Surg Am 96(18):e159
Luring C, Perlick L, Trepte C et al (2006) Micromotion in cemented rotating platform total knee arthroplasty: cemented tibial stem versus hybrid fixation. Arch Orthop Trauma Surg 126(1):45–48
Meftah M, White PB, Ranawat AS, Ranawat CS (2016) Long-term results of total knee arthroplasty in young and active patients with posterior stabilized design. Knee 23(2):318–321
Molt M, Toksvig-Larsen S (2015) 2-year follow-up report on micromotion of a short tibia stem. A prospective, randomized RSA study of 59 patients. Acta Orthop 86(5):594–598
Morrison JB (1970) The mechanics of the knee joint in relation to normal walking. J Biomech 3(1):51–61
Nelissen RG, Valstar ER, Rozing PM (1998) The effect of hydroxyapatite on the micromotion of total knee prostheses. A prospective, randomized, double-blind study. J Bone Joint Surg Am 80(11):1665–1672
Nilsson K, Kärrholm J, Carlsson L, Dalén T (1999) Hydroxyapatite coating versus cemented fixation of the tibial component in total knee arthroplasty: prospective randomized comparison of hydroxyapatite-coated and cemented tibial components with 5-year follow-up using radiostereometry. J Arthroplasty 14(1):9–20
Nilsson KG, Henricson A, Norgren B, Dalen T (2006) Uncemented HA-coated implant is the optimum fixation for TKA in the young patient. Clin Orthop Relat Res 448:129–139
Normand X, Pinçon JL, Ragot JM, Verdier R, Aslanian T (2015) Prospective study of the cementless “New Wave” total knee mobile-bearing arthroplasty: 8-year follow-up. Eur J Orthop Surg Traumatol 25(2):349–354
Obert L, Loisel F, Huard S et al (2015) Plate fixation of distal radius fracture and related complications. Eur J Orthop Surg Traumatol 25(3):457–464
Onsten I, Nordqvist A, Carlsson AS, Besjakov J, Shott S (1998) Hydroxyapatite augmentation of the porous coating improves fixation of tibial components. A randomised RSA study in 116 patients. J Bone Joint Surg Br 80(3):417–425
Otto R, Moed B, Bledsoe J (2009) Biomechanical comparison of polyaxial-type locking plates and a fixed-angle locking plate for internal fixation of distal femur fractures. J Orthop Trauma 23(9):645–652
Parratte S, Ollivier M, Lunebourg A, Verdier N, Argenson JN (2016) Do stemmed tibial components in total knee arthroplasty improve outcomes in patients with obesity? Clin Orthop Relat Res. doi:10.1007/s11999-016-4791-6
Pijls BG, Nieuwenhuijse MJ, Schoones JW, Middeldorp S, Valstar ER, Nelissen RG (2012) RSA prediction of high failure rate for the uncoated Interax TKA confirmed by meta-analysis. Acta Orthop 83(2):142–147
Pijls BG, Valstar ER, Kaptein BL, Fiocco M, Nelissen RG (2012) The beneficial effect of hydroxyapatite lasts: a randomized radiostereometric trial comparing hydroxyapatite-coated, uncoated, and cemented tibial components for up to 16 years. Acta Orthop 83(2):135–141
Regnér L, Carlsson L, Kärrholm J, Herberts P (2000) Tibial component fixation in porous- and hydroxyapatite-coated total knee arthroplasty: a radiostereo metric evaluation of migration and inducible displacement after 5 years. J Arthroplasty 15(6):681–689
Ries C, Heinichen M, Dietrich F, Jakubowitz E, Sobau C, Heisel C (2013) Short-keeled cemented tibial components show an increased risk for aseptic loosening. Clin Orthop Relat Res 471(3):1008–1013
Röderer G, Erhardt J, Graf M, Kinzl L, Gebhard F (2010) Clinical results for minimally invasive locked plating of proximal humerus fractures. J Orthop Trauma 24(7):400–406
Ruchholtz S, El-Zayat B, Kreslo D et al (2013) Less invasive polyaxial locking plate fixation in periprosthetic and peri-implant fractures of the femur–A prospective study of 41 patients. Injury 44(2):239–248
Ryd L, Albrektsson BE, Carlsson L et al (1995) Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg Br 77(3):377–383
Ryd L, Carlsson L, Herberts P (1993) Micromotion of a noncemented tibial component with screw fixation. An in vivo roentgen stereophotogrammetric study of the Miller-Galante prosthesis. Clin Orthop Relat Res 295:218–225
Ryd L, Lindstrand A, Stenstrom A, Selvik G (1990) Porous coated anatomic tricompartmental tibial components. The relationship between prosthetic position and micromotion. Clin Orthop Relat Res 251:189–197
Schlegel UJ, Bruckner T, Schneider M, Parsch D, Geiger F, Breusch SJ (2015) Surface or full cementation of the tibial component in total knee arthroplasty: a matched-pair analysis of mid- to long-term results. Arch Orthop Trauma Surg 135(5):703–708
Skwara A, Figiel J, Knott T, Paletta J, Fuchs-Winkelmann S, Tibesku C (2009) Primary stability of tibial components in TKA: in vitro comparison of two cementing techniques. Knee Surg Sports Traumatol Arthrosc 17(10):1199–1205
Stem E, Hicks B, Roper W (2008) Screw osteolysis in the cementless anatomic modular knee arthroplasty. Orthopedics 31(1):77
Sumner DR, Berzins A, Turner TM, Igloria R, Natarajan RN (1994) Initial in vitro stability of the tibial component in a canine model of cementless total knee replacement. J Biomech 27(7):929–939
Sumner DR, Turner TM, Dawson D, Rosenberg AG, Urban RM, Galante JO (1994) Effect of pegs and screws on bone ingrowth in cementless total knee arthroplasty. Clin Orthop Relat Res 309:150–155
Valstar ER, Gill R, Ryd L, Flivik G, Borlin N, Karrholm J (2005) Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 76(4):563–572
Volz RG, Nisbet JK, Lee RW, McMurtry MG (1988) The mechanical stability of various noncemented tibial components. Clin Orthop Relat Res 226:38–42
Wahnert D, Hoffmeier KL, von Oldenburg G, Frober R, Hofmann GO, Muckley T (2010) Internal fixation of type-C distal femoral fractures in osteoporotic bone. J Bone Joint Surg Am 92(6):1442–1452
Walker PS, Hsu HP, Zimmerman RA (1990) A comparative study of uncemented tibial components. J Arthroplasty 5(3):245–253
Wilkens K, Curtiss S, Lee M (2008) Polyaxial locking plate fixation in distal femur fractures: a biomechanical comparison. J Orthop Trauma 22(9):624–628
Wilson DA, Richardson G, Hennigar AW, Dunbar MJ (2012) Continued stabilization of trabecular metal tibial monoblock total knee arthroplasty components at 5 years-measured with radiostereometric analysis. Acta Orthop 83(1):36–40
Yamanaka H, Goto K, Suzuki M (2012) Clinical results of Hi-tech Knee II total knee arthroplasty in patients with rheumatoid arthritis: 5- to 12-year follow-up. J Orthop Surg Res 7:9
Yoshii I, Whiteside L, Milliano M, White S (1992) The effect of central stem and stem length on micromovement of the tibial tray. J Arthroplasty 7(Suppl):433–438
Acknowledgments
The authors want to thank the Anatomical Institute of the University of Düsseldorf for donating the tibia specimen. Furthermore, we thank our biomechanical engineers for constructing the prototype used in this study
Author information
Authors and Affiliations
Corresponding author
Additional information
C. Benzing and A. Skwara contributed equally.
Rights and permissions
About this article
Cite this article
Benzing, C., Skwara, A., Figiel, J. et al. Initial stability of a new cementless fixation method of a tibial component with polyaxial locking screws: a biomechanical in vitro examination. Arch Orthop Trauma Surg 136, 1309–1316 (2016). https://doi.org/10.1007/s00402-016-2517-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-016-2517-6