Abstract
Background
The choice of implant design plays an important role for primary fixation of a TKA. Short-keeled tibial components allow implantation through a smaller approach with less femorotibial subluxation.
Questions/purposes
The purpose of this study was to detect early implant failure resulting from aseptic loosening after cemented short-keeled and standard tibial baseplate implantation.
Methods
Between 2008 and 2010, a group of 160 consecutive patients (with 80 standard and with 80 short-keeled tibial trays) received cemented TKAs. At 1-year followup, patients were examined clinically and radiographs were analyzed regarding aspects of radiolucency. The components were divided into five zones on each radiographic view and the measurements of the 10 zones were added.
Results
The mean sum of radiolucencies was increased significantly with the short-keeled baseplates. In the current study, short-keeled tibial trays revealed a revision rate of 6.3% after 1-year followup. In contrast, none of the standard tibial baseplates were revised.
Conclusions
The implantation of cemented, short-keeled tibial components is linked to an increased rate of early loosening. Therefore, the indication for cemented, short-keeled component implantation should be reviewed.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
TKA is a successful procedure and the gold standard in the treatment of end-stage degenerative joint disease or deformity of the knee. A couple long-term followup studies of standard TKA have shown excellent results for pain reduction, functional improvement, and survivorship of 90% to 95% at 15 years [2, 18]. Since minimally invasive surgery (MIS) in TKA has been introduced, the development of new surgical techniques, instruments, and implants has been driven forward. Improved pain management, a shorter hospital stay, substantially lower blood loss, and a shorter surgery duration, all supposedly related to the less aggressive surgery, are some advantages of MIS techniques [3, 10, 12–14, 16, 22].
New, smaller implants were designed to develop MIS techniques. Short-keeled tibial baseplates allow implantation through a smaller approach with less femorotibial subluxation. The design of the implant plays an important role for primary stability, in particular in the case of a reduced surface area in contact with the bone. High implant-bone stress levels, particularly on rather weak cancellous bone, have been implicated as the predominant cause for aseptic tibial component loosening, the most frequent cause for TKA failure [4]. Although some MIS tibial components, for instance, the Miller-Galante II (Zimmer, Warsaw, IN, USA) with four pegs, have done very well in a long-term study [19], the overall clinical outcome and survivorship data for those baseplates are rare. The purpose of this study was to examine whether there is an increased risk of early implant failure resulting from aseptic loosening for short-keeled tibial components. Therefore, we clinically compared these new components with standard tibial components. As a result of a reduced fixation surface for cemented, short-keeled tibial implants, we hypothesized an increased risk for aseptic loosening assessed by the development of radiolucent lines and the need for revision compared with conventional tibial components. Furthermore, we aimed to detect whether other factors such as BMI, tibial component size, age, and sex influenced the rate of tibial loosening.
Material and Methods
Between 2008 and 2010, a group of 160 consecutive patients received cemented TKAs (Genesis II; Smith & Nephew, Memphis, TN, USA). After introduction of the Genesis II MIS tibial tray, a series of 80 consecutive patients (2009–2010) underwent surgery with this prosthesis. To form a comparison group we identified 80 consecutive patients who underwent TKA in the year before the MIS group (2008–2009) with a standard tibial tray. All prostheses were implanted by one surgeon (CH). There were 99 women and 61 men with an average BMI of 30 kg/m² (range, 20–53 kg/m²) and an average age of 65 years (range, 42–86 years). Both groups had a similar distribution of patient characteristics (Table 1).
Both tibial components are available in eight side-specific, asymmetric sizes and have an identical design of the tibial baseplate. The standard design has a tibial stem with a Morse taper to be connected with a stem extension if needed and two fins at the stem to increase rotational stability. The short-keeled design offers no Morse taper connection and the dimension of the stem is shortened slightly compared with a standard implant. In addition, the fins for rotation stability are slightly reduced. In 155 patients, a cruciate-retaining femoral component was used with a deep-flex inlay. The tibial sagittal cut has a 3° slope, whereas 4° is additionally implemented into the inlay design. In five cases, a posterior-stabilized femoral component was used with the same deep-flex posterior-stabilized inlay design (short-keeled group: one female [both knees], age 56 years, BMI 24 kg/m²; standard group: three males, aged 79, 54, and 59 years, BMI 27, 30, and 31 kg/m²).
For surgical exposure of the knee we used a standard medial parapatellar approach keeping it as small as possible in both groups with patellar subluxation and tibiofemoral dislocation. All components were implanted with the same high-viscosity cementing technique. After performing cuts and the trial implantation, the bone was cleaned with pulsatile lavage. Holes were drilled into sclerotic areas. High-viscosity cement (Refobacin Bone Cement; Biomet Inc, Warsaw, IN, USA) was attached to the surfaces of both parts and after implantation, the original inlay was attached quickly to reduce micromovements during cement curing. The leg was kept in extension until the cement was completely cured. The local ethics committee approved the investigation.
All patients were examined clinically and radiographs were analyzed for the development of radiolucent lines subsequent to surgery and at 6 weeks and 1 year after TKA. In the current study, as much as possible the radiographs at 1-year followup were taken as a basis for radiolucency measurements. The overall mean followup was 16 months (range, 8–31 months). The mean followup in the standard group was 18 months (range, 9–31 months) and in the MIS group 13 months (range, 8–22 months).
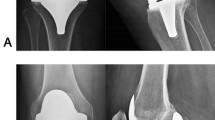
The tibial components were divided into five zones on each of the AP and the lateral standing radiographs (Fig. 1). Measurements were performed after calibration of each radiograph using the known implant dimensions. The measurements of the 10 zones were added to achieve an overall radiolucent value in millimeters for each knee (CH, CR). We performed crosschecking for intraobserver and interobserver reliabilities without any specific statistical testing.
Furthermore, we compared all patients with regard to age, sex, BMI, inlay, and tibial component size to examine influencing factors for aseptic loosening.
The revision surgeries were indicated in patients with persistent pain and radiological evidence of loosening.
To compare both implants and the created groups, we performed an ANOVA. Pearson’s test was used to confirm correlations between radiolucency and patient-related parameters. All tests were two-sided and the significance level was fixed at α = 0.05. The evaluation was performed using the analytical software SPSS® for Mac OS X, Version 20.0 (IBM Corp, New York, NY, USA).
Results
The average radiolucent value was significantly increased (p < 0.01) with the short-keeled baseplates (Fig. 2). On average, taking all 10 zones together, the overall radiolucent value was 1.21 mm (SD ± 0.52) increased.
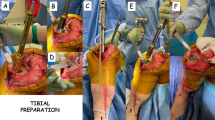
In total, five patients with a short-keeled tibial tray underwent revision surgery as a result of persistent pain and loosening (Fig. 3A–B). At the time of revision, the mean followup was 13 months (range, 10–19 months). The patients (three women, two men) who had revision surgery were on average 63 years old (range, 56–74 years) with an average BMI of 30 kg/m² (range, 26–33 kg/m²). One Size 3 tibial tray and two Sizes 5 and 6 were loosened. All patients had a cruciate-retaining femoral component with a 9-mm polyethylene inlay. None of the patients who received a posterior-stabilized femoral component underwent revision surgery as a result of persistent pain and aseptic loosening. In four of the five revision cases failure of fixation occurred at the cement-implant interface (Fig. 3C).
Concerning influencing factors for aseptic loosening, none of the examined parameters revealed statistical significance (p = 0.13–0.87).
Discussion
As part of our interest in the MIS TKA technique, we performed a trial of implantation of short-keeled tibial trays. We performed 80 short-keeled tibial baseplates between 2009 and 2010. The purposes of this study were to examine the rate of loosening of these short-keeled implants and their tendency to form radiolucent lines. We found an unacceptably high rate of tibial loosening, which did not appear to be related to patient factors such as BMI, sex, or tibial size. We observed early implant failure of a cemented, short-keeled tibial baseplate in five patients, whereas none of the standard trays in the comparative series have been revised. All five patients had persistent pain and aseptic loosening (Fig. 3).
There are some limitations to our study. First, the study was retrospective and observational bias cannot be ruled out. The follow-up, especially of the short-keeled trays, is short. However, this is somewhat mitigated by the higher rates of failure in this group. Second, there was no special radiologic standardization (eg, fluoroscopy-guided radiographs, obtaining oblique and other special views to ensure exact parallel view to the bone-implant interface). However, all radiographs were standing AP and lateral exposures and were performed in a standardized manner. Additionally, no measures of reproducibility were performed for the radiographic measurements.
High stress levels on the underlying implant surface (implant interfaces, the cement, and the cancellous bone in the proximal tibia) have been implicated as the predominant risk factor of loosening [4, 7]. Aseptic loosening of the tibial component remains a major cause of failure in TKA and may be related, directly or indirectly, to micromotion [26]. Micromotion at the implant-cement or bone-cement interface causes generation of wear particles, which is supposed to be the main reason for aseptic loosening in the mid- and long term [11]. In the short-term, mechanical failure of implant fixation might be an overloaded bone-cement or more likely a cement-implant failure. Therefore, the primary fixation marks one cornerstone for longevity of the prosthesis. Considering the stem design, it has to be taken into account that a stemmed baseplate has a higher fixation area and therefore gives the implant more stability in deep flexion and reduces tilting forces. This is in line with the observations of Yoshii et al. [29] and Kraemer et al. [15] who concluded that a stemmed tibial implant reduces the tendency for liftoff and subsidence in the frontal and sagittal planes. The use of an intramedullary stem and avoidance of varus-valgus malpositioning of components have been advocated to reduce the mentioned bone-implant stresses [17, 28]. We did not detect any influencing factors for loosening in addition to the implant design such as BMI, tibial component size, age, or sex. Therefore, the increased revision rate for the short-keeled tibial baseplate may be caused basically by the design of the tibial component.
A cement penetration of 3 to 5 mm is considered optimal for implant fixation [9]. All patients in our study had the tibial surfaces prepared with pulsatile lavage before the tibial baseplate was placed. Pulsatile lavage allows for better cement penetration that increases the tensile and shear strength of the cement-bone interface and therefore the probability of successful implantation [6, 20]. Despite observing these standards, five patients (6.3%) with short-keeled tibial baseplates underwent revision surgery as a result of aseptic loosening. The failure in four of the five cases was related to the implant-cement interface (Fig. 3C). Debonding of the roughened baseplate from the underlying cement mantle causes wear debris between the two surfaces. The produced particulate metal and cement debris lead to rapid osteolysis and early failure [8, 21, 23, 25, 27]. This may explain the parallel observation of debonding and radiolucencies.
The expected long-term success of standard TKA should be at least 10 years as evidenced by studies which found 10 year 90% survivorship [2, 18], and long-term patient satisfaction of 80% [1]. The standard tray used in our study (the Genesis II CR; Smith & Nephew) had a survivorship of 98% at 5 to 11 years followup (mean, 9.5 years) in a previous study [5]. Sharkey et al. [24] differentiated between early and late complications after TKA. In their experience 25% of early failures were the result of infection followed by arthrofibrosis (18%). In contrast, aseptic loosening (33%) and wear/osteolysis (44%) are the main reasons for late failures.
Stemmed tibial components also have some disadvantages. Exposure of the knee has to be more extensive to place the tray with the stem. This procedure also requires increased femorotibial subluxation with higher stresses on the posterior capsule and soft tissue.
Our study suggests that implantation of a short-keeled tibial component is linked to an increased rate of early aseptic loosening. Therefore, the indication for a short-keeled component implantation should be reviewed.
References
Baker PN, van der Meulen JH, Lewsey J, Gregg PJ; National Joint Registry for England and Wales. The role of pain and function in determining patient satisfaction after total knee replacement: data from the National Joint Registry for England and Wales. J Bone Joint Surg Br. 2007;89:893–900.
Berger RA, Rosenberg AG, Barden RM, Sheinkop MB, Jacobs JJ, Galante JO. Long-term followup of the Miller-Galante total knee replacement. Clin Orthop Relat Res. 2001;388:58–67.
Bonutti PM, Mont MA, Kester MA. Minimally invasive total knee arthroplasty: a 10-feature evolutionary approach. Orthop Clin North Am. 2004;35:217–226.
Bourne RB, Finlay JB. The influence of tibial component intramedullary stems and implant-cortex contact on the strain distribution of the proximal tibia following total knee arthroplasty: an in vitro study. Clin Orthop Relat Res. 1986;208:95–99.
Bourne RB, McCalden RW, MacDonald SJ, Mokete L, Guerin J. Influence of patient factors on TKA outcomes at 5 to 11 years followup. Clin Orthop Relat Res. 2007;464:27–31.
Breusch SJ, Norman TL, Schneider U, Reitzel T, Blaha JD, Lukoschek M. Lavage technique in total hip arthroplasty: jet lavage produces better cement penetration than syringe lavage in the proximal femur. J Arthroplasty. 2000;15:921–927.
Ducheyne P, Kagan A 2nd, Lacey JA. Failure of total knee arthroplasty due to loosening and deformation of the tibial component. J Bone Joint Surg Am. 1978;60:384–391.
Duffy GP, Muratoglu OK, Biggs SA, Larson SL, Lozynsky AJ, Harris WH. A critical assessment of proximal macrotexturizing on cemented femoral components. J Arthroplasty. 2001;16(8 suppl 1):42–48.
Ebramzadeh E, Sarmiento A, McKellop HA, Llinas A, Gogan W. The cement mantle in total hip arthroplasty: analysis of long-term radiographic results. J Bone Joint Surg Am. 1994;76:77–87.
Hernandez-Vaquero D, Noriega-Fernandez A, Suarez-Vazquez A. Total knee arthroplasties performed with a mini-incision or a standard incision: similar results at six months follow-up. BMC Musculoskelet Disord. 2010;11:27.
Jacobs JJ, Shanbhag A, Glant TT, Black J, Galante JO. Wear debris in total joint replacements. J Am Acad Orthop Surg. 1994;2:212–220.
Kelly MJ, Rumi MN, Kothari M, Parentis MA, Bailey KJ, Parrish WM, Pellegrini VD Jr. Comparison of the vastus-splitting and median parapatellar approaches for primary total knee arthroplasty: a prospective, randomized study. Surgical technique. J Bone Joint Surg Am. 2007;89(suppl 2):80–92.
Kim YH, Sohn KS, Kim JS. Short-term results of primary total knee arthroplasties performed with a mini-incision or a standard incision. J Arthroplasty. 2006;21:712–718.
Kolisek FR, Bonutti PM, Hozack WJ, Purtill J, Sharkey PF, Zelicof SB, Ragland PS, Kester M, Mont MA, Rothman RH. Clinical experience using a minimally invasive surgical approach for total knee arthroplasty: early results of a prospective randomized study compared to a standard approach. J Arthroplasty. 2007;22:8–13.
Kraemer WJ, Harrington IJ, Hearn TC. Micromotion secondary to axial, torsional, and shear loads in two models of cementless tibial components. J Arthroplasty. 1995;10:227–235.
Laskin RS. Minimally invasive total knee arthroplasty: the results justify its use. Clin Orthop Relat Res. 2005;440:54–59.
Lewis JL, Askew MJ, Jaycox DP. A comparative evaluation of tibial component designs of total knee prostheses. J Bone Joint Surg Am. 1982;64:129–135.
Lidgren L, Robertsson O. Annual Report 2008. The Swedish Knee Arthroplasty Register. Dept. Of Orthopedics, Lund University Hospital. Available at: http://www.knee.nko.se/english/online/uploadedFiles/112_SVK_2008Engl_1.1.pdf. Accessed September 20, 2012.
Miller CW, Pettygrow R. Long-term clinical and radiographic results of a pegged tibial baseplate in primary total knee arthroplasty. J Arthroplasty. 2001;16:70–75.
Miskovsky C, Whiteside LA, White SE. The cemented unicondylar knee arthroplasty: an in vitro comparison of three cement techniques. Clin Orthop Relat Res. 1992;284:215–220.
Ong A, Wong KL, Lai M, Garino JP, Steinberg ME. Early failure of precoated femoral components in primary total hip arthroplasty. J Bone Joint Surg Am. 2002;84:786–792.
Reid JB 3rd, Guttmann D, Ayala M, Lubowitz JH. Minimally invasive surgery: total knee arthroplasty. Arthroscopy. 2004;20:884–889.
Schmalzried TP, Zahiri CA, Woolson ST. The significance of stem-cement loosening of grit-blasted femoral components. Orthopedics. 2000;23:1157–1164.
Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13.
Sylvain GM, Kassab S, Coutts R, Santore R. Early failure of a roughened surface, precoated femoral component in total hip arthroplasty. J Arthroplasty. 2001;16:141–148.
Vanlommel J, Luyckx JP, Labey L, Innocenti B, De Corte R, Bellemans J. Cementing the tibial component in total knee arthroplasty: which technique is the best? J Arthroplasty. 2011;26:492–496.
Vaughn BK, Fuller E, Peterson R, Capps SC. Influence of surface finish in total hip arthroplasty. J Arthroplasty. 2003;18(7 suppl 1):110–115.
Walker PS, Greene D, Reilly D, Thatcher J, Ben-Dov M, Ewald FC. Fixation of tibial components of knee prostheses. J Bone Joint Surg Am. 1981;63:258–267.
Yoshii I, Whiteside LA, Milliano MT, White SE. The effect of central stem and stem length on micromovement of the tibial tray. J Arthroplasty. 1992;7(suppl):433–438.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Ries, C., Heinichen, M., Dietrich, F. et al. Short-keeled Cemented Tibial Components Show an Increased Risk for Aseptic Loosening. Clin Orthop Relat Res 471, 1008–1013 (2013). https://doi.org/10.1007/s11999-012-2630-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2630-y