Abstract
Study design
Retrospective case–control study.
Purpose
To compare the safety and efficacy of the Zero-profile (Zero-p) integrated plate and spacer device to that of an anterior cervical plate and cage in patients undergoing anterior cervical discectomy and fusion (ACDF).
Summary of background data
Anterior cervical plating system has provided good results, including higher fusion rate and improved alignment since its use. However, adjacent-level ossification development (ALOD) and dysphagia have been usually reported associating with plates.
Methods
This was a retrospective control study. Sixty-two patients with cervical radiculopathy or myelopathy were treated with an anterior plate and cage or Zero-p implant between January 2011 and December 2011. The mean follow-up was 33.1 months in the plate and cage group and 30.6 months in Zero-p group. Patient demographics, operative details and complications were reviewed. The clinical outcomes were evaluated using the Japanese Orthopaedic Association (JOA) scores and JOA recovery rate before and after operations. Incidence of cephalad and caudal ALOD on the lateral radiographs was studied at preoperation, immediate postoperation and last follow-up. Incidence of dysphagia was also recorded after operation according to Bazaz–Yoo dysphagia index.
Results
Thirty-two patients received an anterior plate and cage and 30 received the Zero-p implant. There were no statistical differences in patient demographics, operative details between the two groups. The JOA scores significantly increased compared with preoperational measurements in both groups (p < 0.05), but the JOA recovery rate was similar (72.2 % for plate and cage group and 77.0 % for Zero-p group, p > 0.05). ALOD occurred in 12 (18.8 %) of the 64 cephalad and caudal adjacent segments in plate with cage group, and only 1 (1.6 %) of 63 adjacent levels (including three noncontiguous cases) presented with ALOD in Zero-p group. The difference was significant (p < 0.01). The incidence of dysphagia in the Zero-p group was lower compared with that in the plate with cage group, and the symptom duration was much shorter (p < 0.01). Both groups had no adverse events associated with the implant or implant surgery.
Conclusions
The Zero-profile implant is safe and efficacious after ACDF. It can reduce the rate of adjacent-level ossification development and dysphagia compared to anterior plate and cage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cervical discectomy and fusion (ACDF) with plating and cage system has been the standard of care for symptomatic cervical degenerative disc disease. As plates and cages provide many advantages including higher fusion rate, disc height, good cervical lordosis and improved alignment, their use will continue [1–3]. However, plates have been proved to associate with higher rates of adjacent-level ossification development (ALOD) and dysphagia [4–6]. In view of this, a new Zero-profile integrated plate and spacer device (Zero-p, Synthes, Switzerland) was developed and approved for use in patients with degenerative cervical disc diseases by the US Food and Drug Administration (FDA) in 2008. So far, many studies about this new Zero-p implant demonstrated that it produced good clinical and radiological outcomes that were comparable to those for nonintegrated plate-and-spacer constructs [7–10]. However, no report in the language of English was found to clarify its effect on reducing ALOD.
In China, this new Zero-p implant was first implemented in our department in 2011. So we conducted a retrospective control study with a 2–3 years follow-up to prove it reducing rate of ALOD and dysphagia.
Materials and methods
Patient population
Between January 2011 and December 2011, 62 patients were selected to undergo ACDF. The inclusion criteria were the following: age older than 20 years; prolapsed cervical discs at levels from C3–C4 down to C6–C7; presenting with a cervical radicular syndrome or neurological deficit with or without neck pain; failing conservative treatment for at least 6 weeks. Patients who had had dysphagia before surgery, and who had had preoperative anterior osteophytes cephalad or caudad to the level subsequently treated with the anterior cervical plate were excluded from the study. The plate was used when the last digit of the admission number is odd number; otherwise, the Zero-p was used. Thirty-two patients received an anterior plate and cage and 30 received the Zero-p implant. There were 22 males and 10 females with a mean age of 42.8 years (range 30–65 years) in plate and cage group, and 20 males and 10 females with a mean age of 44.1 years (range 33–61 years) in Zero-p group. The mean duration of postoperative follow-up was 33.1 months (range 24–42 months) in plate and cage group and 30.6 months (range 20–40 months) in Zero-p group. Fifteen patients underwent the ACDF with plating system at one level; 10, at two levels and 7, at three levels. Of Zero-p patients, 13 were at one level, 9 at two levels and 8 at three levels.
Zero-p integrated plate and spacer device
In 2008, the Zero-p integrated plate and spacer device (Synthes GmbH Switzerland, Oberdorf, Switzerland), based on an anterior stand-alone stabilization implant of the lumbar spine, was approved by the United States FDA to be an alternative to the traditional separate interbody spacer and plate device for ACDF. It combines an interbody spacer with an anterior plate, which does not protrude outside the intervertebral disc space as anterior cervical plates do. The polyetheretherketone (PEEK) interbody spacer contains a radiopaque marker for visualization during fluoroscopy and lacks carbon fibers, thereby reducing the risk of systemic uptake. A small titanium plate, which is preassembled with the interbody spacer, provides an interface for anchorage. Four screws are placed within the plate at a 2.5° medial or lateral angle and a 40° cranial or caudal angle. In operation, the device should be placed 2 mm behind the anterior column in the lateral view and in the center of the disc space in the antero-posterior view.
Radiological evaluation
The radiographs of the cervical spine before surgery, at immediate postoperation and last follow-up were made with the standard tube-to-film distance (1.8 m) for all patients. The ALOD severity on lateral films was classified into four grades using the previously described grading system: grade 0 (no ALOD formation), grade 1 (ALOD extends across less than 50 % of the disc space), grade 2 (ALOD extends greater than or equal to 50 % of the disc space), and grade 3 (complete bridging of the adjacent disc space) [4] (Fig. 1). Each independent observer determined the grade of ALOD twice on two separate occasions, and the average of the four measurements was used as the final grade. There were 64 adjacent levels in plate and cage group, but 63 adjacent levels in Zero-p group because three patients presented with noncontiguous cervical spondylosis, which was C3/4 and C5/6 in two patients, and C4/5 and C6/7 in one patient.
Lateral radiographs of the cervical spine, made at the time of final follow-up, showing the different grades of adjacent-level ossification. a Grade 0, no adjacent-level ossification; b grade 1, ossification extending across <50 % of the adjacent disc space (arrow); c grade 2, ossification extending across ≥50 % of the adjacent disc space (arrow); d grade 3, complete bridging of the adjacent disc space (arrow)
Clinical evaluation
The clinical outcomes were evaluated using the JOA scores before and after surgery. A JOA recovery rate (RR) was also calculated, which was defined according to the rationale of Hirabayashi [11] in that RR = (postoperative JOA score − preoperative JOA score)/(17 − preoperative JOA score) × 100. RR results were grouped as 75 % or more (excellent), 50–74 % (good), 25–49 % (fair), and less than 25 % (poor).
The presence of dysphagia was evaluated at postoperative follow-up 2 weeks and 3–24 months following the procedure. Severity of dysphagia was graded as none (no episodes of swallowing problems), mild (rare episodes of dysphagia), moderate (occasional swallowing difficulty with specific food), or severe (frequent difficult swallowing with majority of food), according to Bazaz–Yoo [12].
Statistical analysis
Comparison of gender, operation level and ALOD between the two groups was used the Chi-square test. Comparison of mean age, duration of follow-up, blood loss and operation time between the two groups, and JOA scores before and after operation was used independent sample t test. The correlation coefficients for intraobserver and interobserver variabilities of the technique for grading the severity of ALOD was evaluated using Spearman correlation test. All statistical analyses were used SPSS statistical package (version 12.0; SPSS, Inc., Chicago, IL, USA). A p value of <0.05 was considered to be significant.
Results
Demographics and operative details
Preoperative age, gender, surgical level in the two groups were not different (p > 0.05). The mean operating times (from incision to closure) for one-, two- and three-level Zero-p procedures were 55, 89 and 122 min, respectively, and it was 61, 90 and 130 min in plate and cage group, respectively. No statistical difference was found although the mean operating time is slightly longer in plate and cage group than Zero-p group (p > 0.05). There was no significant difference in the mean blood loss between the two groups, with the mean blood loss was 150 ml (SD 46) in Zero-p group and 155 ml (SD 52) in plate and cage group. No patient received blood transfusion (Table 1).
Radiological findings
The correlation coefficients for intraobserver and interobserver variabilities of the technique for grading the severity of the ALOD were r = 0.97 (p < 0.01) and r = 0.93 (p < 0.01), respectively.
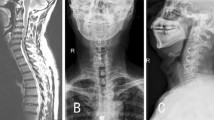
Ossification developed in 12 (18.8 %, 9 in cephalad and 3 in caudal) of the 64 cephalad and caudal adjacent disc spaces in plate and cage group (Fig. 2). Eight (66.7 %) of the 12 ALOD was grade-1, 3 (25 %) was grade-2 and 1 (8.3 %) was grade-3. However, only 1 (1.6 %) of 63 adjacent levels presented with ALOD (grade-2) in Zero-p group (Fig. 3). The difference of ALOD between the two groups was significantly different (p < 0.01).
Adjacent-level ossification development in plate and cage group. a Lateral preoperative radiograph of the cervical spine showing degeneration at C5–C6, but no ossification at adjacent levels of C4–C5 and C6–C7; b immediate postoperative radiographs showing ACDF with plate and cage at C5–C6; c 3 years after operation, ALOD (grade 1) could be seen at C4–C5 (arrow)
Adjacent-level ossification development in Zero-p group. a, b Lateral radiograph of the cervical spine before and immediate after surgery showing ACDF at C4–C5 and C5–C6, but no ossification at adjacent levels of C3–C4 and C6–C7; c ossification of grade 2 developed at C6–C7 (arrow) 3 years after operation
Clinical outcomes
The postoperative JOA score at latest follow-up differed significantly from their respective preoperative JOA score in both groups (p < 0.05). The mean and standard deviation RR was 72.2 ± 18.1 % for Zero-p group and 77.0 ± 13.5 % for plate and cage group (p > 0.05). RR was excellent in 7 patients, good in 20 patients, fair in 4 patients, and poor in one patient in plate and cage group; whereas, in Zero-p group, RR was excellent in 6 patients, good in 18 patients, and fair in 6 patients.
The incidence and the duration of postoperative dysphagia in the Zero-p and plate with cage groups are shown in Fig. 4. To rule out the approach-related effect for anterior exposition of 3 levels in cervical spine, we performed a subgroup comparison and investigated the numbers of patients with postoperative dysphagia between the Zero-p and plate with cage groups. The number of patients with postoperative dysphagia increases with anterior exposition levels but the Zero-p group still consistently outperforms the plate with cage group at all postoperative time points for each level of anterior exposition.
Discussion
Anterior cervical discectomy and fusion is the standard surgical treatment for symptomatic cervical degenerative disc disease after conservative medical management fails [13]. Many surgeons prefer to add an anterior plate in fusion procedures for enhancing stabilizing properties, as several studies suggest this leads to increased fusion rates and reduced failure rates, particularly in multilevel procedures [14, 15]. However, the application of a plate may lead to soft tissue damage, dysphagia and hardware failure such as fracture, migration and so on, especially in multilevel procedures [16]. Therefore, stand-alone cages were introduced to be an alternative choice for anterior cervical fusion and it was proved to give good results, but stand-alone cages had a relatively high incidence of implant subsidence with secondary kyphotic deformity that may lead to adjacent cervical segment disease in the long term [17]. Otherwise, biomechanical studies have suggested that cervical cages should be supplemented with additional external or internal supports to prevent excessive movement in flexion–extension [18]. So, the Synthes Company has come up with an all-in-one solution—a Zero-profile integrated plate and spacer device. The Zero-p has produced as good a rate of fusion and biomechanical stability as does a plate-and-cage construct, and both procedures corrected cervical kyphosis and improved cervical alignment since its use [7–10]. We asked whether this Zero-p implant would be associated with a low rate of ALOD and dysphagia.
ALOD is thought to be a type of heterotopic ossification, rather than a secondary degeneration developing at the adjacent segment discs. This is because several studies have shown that the ossification occurs in soft tissues that do not form bone under normal conditions. More importantly, this bone matures within the first 2 years after surgery, in contrast to adjacent segment degeneration, in which osteophytic bone and disc degeneration gradually increase over time [19, 20]. In our study, we also distinguish ALOD from adjacent segment degeneration (ASD). One reason is that we find many patients having no signs of ASD, such as intervertebral disc narrowing, vertebral slip, and signal intensity changes on MRI, even if there is obvious and severe ALOD. Otherwise, we find that the base of ALOD is situated anterior to the vertebral body, covering about half of it. However, the osteophytes seen in ASD are located antero-inferiorly in the vertebral body, covering no more than one-third of it. We therefore believe that the pathological mechanism of ALOD differs from that of osteophytic growth in ASD, but this will require further study.
Park et al. [4] demonstrated that the ossification occurred at a significantly higher rate and was more severe in patients with plates within 5 mm of an adjacent disc space. Lee et al. [21] thought that techniques using a short plate with an oblique screw trajectory resulted in significantly reduced incidence and severity of ALOD. Many studies suggested that the closer the plate was to the adjacent disc space, the higher and greater the ossification. The mechanism may be related to irritation of the anterior aspect of the adjacent level by a cervical plate and stripping of anterior longitudinal ligament [22]. In clinical, we now attempt to place anterior cervical plates ≥5 mm from adjacent disc spaces in order to reduce ALOD in those patients using cage and plate. On the basis of these results, a Zero-p integrated plate and spacer device was designed to reduce the incidence of ALOD. In our study, the incidence of ALOD in patients with Zero-p implant was only 1.6 %, significantly lower than that in patients with plate and cage (18.8 %). This may because that the plate of Zero-p does not protrude outside the intervertebral disc space, which can minimize the irritation of the adjacent cervical structures.
Dysphagia is another well-known postoperative complication related to anterior cervical plate. The incidence of dysphagia after anterior cervical fusion with plating is reported to vary between <1 and 62 % [7, 23]. The possible causes include postoperative soft tissue edema, esophageal injury, postoperative hematoma, and adhesive formations around implanted cervical plates, and many preventative measures have been put forward [24]. According to Lee et al. [25], a thinner anterior cervical plate could significantly reduce the rate of dysphagia compared to a thick one. Although the profile of current anterior plates is thinner than that of earlier designs, the plates are still somewhat bulky and may contribute to postprocedure dysphagia. In order to reducing dysphagia, the design of Zero-p device has no profile and the whole device can be inserted into the intervertebral space to avoid stimulating the esophagus directly and mitigating the adhesions of the esophagus. According to our study, the incidence and severity of dysphagia in the Zero-p group is lower compared with that in the cage with plate group in all the follow-up time point and the duration of dysphagia is much shorter, which is consistent with the aim of Zero-p and previous study [10].
The Zero-p implant is relatively simple to insert and the mean operating time and blood loss are relatively lower; however, it does have some disadvantages. For example, the lower screws of C3/4 and the upper screws of the C6/7 implant are hard to introduce at an optimal angle, especially in patients with a short neck or high sternum.
Conclusions
The Zero-profile implant is safe and efficacious for ACDF. It can reduce rate of adjacent-level ossification development and dysphagia compared to anterior plate and cage. However, some deficits existed in our article. First, as with most one-center studies, the number of patients included in our study was insufficient. Second, the span of the follow-up was relatively short. A multi-center, large sample and long-term follow-up study is needed to promote the reliability of the current research.
References
Lee CH, Hyun SJ, Kim MJ et al (2013) Comparative analysis of 3 different construct systems for single-level anterior cervical discectomy and fusion: stand-alone cage, iliac graft plus plate augmentation, and cage plus plating. J Spinal Disord Tech 26:112–118
Song KJ, Taghavi CE, Lee KB et al (2009) The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine 34:2886–2892
Kaiser MG, Haid RW Jr, Br Subach et al (2002) Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 50:229–236 discussion 36–38
Park JB, Cho YS, Riew KD et al (2005) Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg Am 87:558–563
Zeng JH, Zhong ZM, Chen JT et al (2012) Early dysphagia complicating anterior cervical spine surgery: incidence and risk factors. Arch Orthop Trauma Surg 133(8):1067–1071
Riley LH 3rd, Skolasky RL, Albert TJ et al (2005) Dysphagia after anterior cervical decompression and fusion: prevalence and risk factors from a longitudinal cohort study. Spine 30:2564–2569
Wang ZD, Zhu RF, Yang HL et al (2014) The application of a zero-profile implant in anterior cervical discectomy and fusion. J Clin Neurosci 21(3):462–466
Qi M, Chen H, Liu Y et al (2013) The use of a zero-profile device compared with an anterior plate and cage in the treatment of patients with symptomatic cervical spondylosis. Bone Joint J 95-B(4):543–547
Vanek P, Bradac O, P Delacy et al (2013) Anterior interbody fusion of the cervical spine with zero-p spacer. Spine 38(13):792–797
Miao J, Shen Y, Kuang Y et al (2013) Early follow-up outcomes of a new zero-profile implant used in anterior cervical discectomy and fusion. J Spinal Disord Tech 26(5):193–197
Hirabayashi K, Miyakawa J, Satomi K et al (1981) Operative results and postoperative progression of ossification among patients with ossification of posterior longitudinal ligament. Spine 6:354–364
Bazaz R, Lee MJ, Yoo JU et al (2002) Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine 27:2453–2458
Li J, Zheng Q, Guo X et al (2013) Anterior surgical options for the treatment of cervical spondylotic myelopathy in a long-term follow-up study. Arch Orthop Trauma Surg 133(6):745–751
Bohler J, Gaudernak T (1980) Anterior plate stabilization for fracture dislocations of the lower cervical spine. J Trauma 20:203–205
Anderson DG, Albert TJ (2002) Bone grafting, implants, and plating options for anterior cervical fusions. Orthop Clin North Am 33:317–328
Kapu R, Singh M, Pande A et al (2012) Delayed anterior cervical plate dislodgement with pharyngeal wall perforation and oral extrusion of cervical plate screw after 8 years: a very rare complication. J Craniovertebr Junction Spine 3(1):19–22
Gercek E, Arlet V, Delisle J, Marchesi D (2003) Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J 12:513–516
Shimamoto N, Cunningham BW, Dmitriev AE et al (2001) Biomechanical evaluation of stand-alone interbody fusion cages in the cervical spine. Spine 26:432–436
Park JB, Watthanaaphisit T, Riew KD (2007) Timing of development of adjacent-level ossification after anterior cervical arthrodesis with plates. Spine J 7:633–636
Yang JY, Song HS, Lee M et al (2009) Adjacent level ossification development after anterior cervical fusion without plate fixation. Spine 34:30–33
Lee DH, Lee JS, Yi JS et al (2013) Anterior cervical plating technique to prevent adjacent-level ossification development. Spine J 13(7):823–829
Ishihara H, Kanamori M, Kawaguchi Y et al (2004) Adjacent segment disease after anterior cervical interbody fusion. Spine J 4(6):624–628
Smith-Hammond CA, New KC, Pietrobon R et al (2004) Prospective analysis of incidence and risk factors of dysphagia in spine surgery patients: comparison of anterior cervical, posterior cervical, and lumbar procedures. Spine 29:1441–1446
Joaquim AF, Murar J, Savage JW et al (2014) Dysphagia after anterior cervical spine surgery: a systematic review of potential preventative measures. Spine J 14(9):2246–2260
Lee MJ, Bazaz R, Furey CG et al (2005) Influence of anterior cervical plate design on dysphagia: a 2-year prospective longitudinal follow-up study. J Spinal Disord Tech 18:406–409
Acknowledgments
This study was supported by the National Natural and Science Foundation of China (No. 81201428).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, H., Chen, D., Wang, X. et al. Zero-profile integrated plate and spacer device reduces rate of adjacent-level ossification development and dysphagia compared to ACDF with plating and cage system. Arch Orthop Trauma Surg 135, 781–787 (2015). https://doi.org/10.1007/s00402-015-2212-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2212-z