Abstract
IDH wild type (IDHwt) anaplastic astrocytomas WHO grade III (AA III) are associated with poor outcome. To address the possibilities of molecular subsets among astrocytoma or of diagnostic reclassification, we analyzed a series of 160 adult IDHwt tumors comprising 120 AA III and 40 diffuse astrocytomas WHO grade II (A II) for molecular hallmark alterations and established methylation and copy number profiles. Based on molecular profiles and hallmark alterations the tumors could be grouped into four major sets. 124/160 (78 %) tumors were diagnosed as the molecular equivalent of conventional glioblastoma (GBM), and 15/160 (9 %) as GBM-H3F3A mutated (GBM-H3). 13/160 (8 %) exhibited a distinct methylation profile that was most similar to GBM-H3-K27, however, lacked the H3F3A mutation. This group was enriched for tumors of infratentorial and midline localization and showed a trend towards a more favorable prognosis. All but one of the 120 IDHwt AA III could be assigned to these three groups. 7 tumors recruited from the 40 A II, comprised a variety of molecular signatures and all but one were reclassified into distinct WHO entities of lower grades. Interestingly, TERT mutations were exclusively restricted to the molecular GBM (78 %) and associated with poor clinical outcome. However, the GBM-H3 group lacking TERT mutations appeared to fare even worse. Our data demonstrate that most of the tumors diagnosed as IDHwt astrocytomas can be allocated to other tumor entities on a molecular basis. The diagnosis of IDHwt diffuse astrocytoma or anaplastic astrocytoma should be used with caution.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Classification of diffuse astrocytic tumors
The classification of astrocytomas according to WHO 2007 predominantly relies on the evaluation of histopathology and immunohistochemistry [12]. In recent years molecular parameters have been developed and proven powerful astrocytoma classifiers. In fact, the previously well accepted and quite harmonious WHO classification scheme for astrocytomas has experienced challenges by molecular findings that are not reflected in morphology. The presence of isocitrate dehydrogenase 1 (IDH1) and isocitrate dehydrogenase 2 (IDH2) mutations in the majority of diffuse astrocytomas WHO grade II (A II) and anaplastic astrocytomas WHO grade III (AA III) and their association with a more favorable course, especially in AA III are strong evidence that heterogeneous tumors have been lumped together under a single diagnosis. There is increasing evidence from multiple studies that the poor clinical outcome of IDHwt AA III is a result of a considerable proportion of unrecognized glioblastomas (GBM) in this group [2, 4, 22, 26]. Such evidence is based on an overlap of distinct molecular lesions in IDHwt AA III and GBM and on similar clinical courses. It remains to be tested how many IDHwt A II or IDHwt AA III cannot be allotted to other tumor entities by molecular analyses.
Frequency of IDH1 and IDH2 mutations in WHO 2007 classified and graded astrocytomas
Upon recognition of IDH mutations in a series of GBM, predominantly secondary GBM [16], several studies demonstrated IDH1 or IDH2 mutations in A II and AA III. The percentages of IDH mutations given for A II ranged from 59 to 90 % and those for AA III from 52 to 78 % [1, 5–7, 25, 28]. Interestingly, the frequency of IDH mutations in all studies was higher in A II than in AA III.
Aim and design of the study
The present study was designed to interrogate the hypothesis that the group of IDHwt astrocytoma is in fact composed of distinctive pathobiological entities. A series of 160 adult IDHwt A II or IDHwt AA III was analyzed for molecular parameters consistent with other brain tumor entities. The overall survival (OS) of these subgroups was compared to that of the brain tumor entity in question.
Materials and methods
Tissue collection
For the Heidelberg series, paraffin blocks containing tissue of adult patients (18 years of age and older) with IDHwt A II or AA III were collected from the archives of Neuropathology departments of Universities of Heidelberg, Münster and Zürich, the UCL Institute of Neurology (08/H0716/16) and from the German Glioma Network (GGN). Tumors with 1p/19q co-deletion were excluded. One reference set was extracted from a recently published series by the TCGA (n = 231) [2]. Therefore, the results here are in part based upon data generated by the TCGA Research Network: http://cancergenome.nih.gov/.
Determination of copy number alterations and G-CIMP phenotype by 450k array analysis
The Illumina Infinium HumanMethylation450 BeadChip (450k) array was used to determine the DNA methylation status of 482,421 CpG sites (Illumina, San Diego, USA) according to the manufacturer’s instructions at the Genomics and Proteomics Core Facility of the DKFZ. The array data was used to calculate a low-resolution copy number profile (CNP) as previously described [21]. Further, the data were analyzed as previously described to allot the tumors to either a G-CIMP or a non-G-CIMP cluster [27].
IDH1/IDH2, H3F3A and TERT promoter mutation analyses
Primer design for sequencing was based on accession numbers NM_005896 for IDH1, NM_002168 for IDH2 and NM_002107.4 for H3F3A (http://www.ncbi.nlm.nih.gov). Primers for IDH1: forward 5′-TGATGAGAAGAGGGTTGAGGA-3′; reverse 5′-GCAAAATCACATTATTGCCAAC-3′ and for IDH2: forward 5′-CTCCACCCTGGCCTACCT-3′; reverse 5′-GCTGCAGTGGGACCACTATT-3′.PCR and sequencing were performed as previously described [5]. Primers for H3F3A: forward 5′-CATGGCTCGTACAAAGCAGA-3′; reverse 5′-CAAGAGAGACTTTGTCCCATTTTT-3′. PCR and sequencing were performed as previously described [20]. A 163 bp fragment of the TERT promoter region spanning the hotspot mutations at positions 1,295,228 and 1,295,250 was amplified using GoTaq G2 Hot Start Polymerase (Promega, Madison, USA) and the primers hTERT-short-for 5′-CAGCGCTGCCTGAAACTC-3′ and hTERT-short-rev, 5′-GTCCTGCCCCTTCACCTT-3′ as previously described [9]. Sequences were determined using a semi-automated sequencer (ABI 3100 Genetic Analyzer, Applied Biosystems, Foster City) and Sequence Pilot version 3.1 software (JSI-Medisys, Kippenheim, Germany).
Immunohistochemistry
Immunohistochemistry was conducted on 4 µm thick formalin-fixed, paraffin-embedded (FFPE) tissue sections mounted on StarFrost Advanced Adhesive slides (Engelbrecht, Kassel, Germany) followed by drying at 80 °C for 15 min. Immunohistochemistry was performed on a BenchMark Ultra immunostainer (Ventana Medical Systems, Tucson, AZ, USA). Sections were stained with anti-IDH1-R132H antibody H09 (Dianova, Hamburg, Germany) as previously described [3]. ATRX immunohistochemistry was performed as previously described [19]. In brief, after deparaffinization, slides were pretreated at 95 °C in Cell Conditioning 1 buffer (Ventana) for 90 min. The sections were incubated with primary antibody HPA001906 (Sigma-Aldrich, St. Louis, MO, USA) diluted 1:200 for 2 h. Standard Ventana signal amplification was used. For BRAFV600E staining V600E-specific clone VE1 was used. After pretreatment with cell conditioner 1 (pH 8) for 64 min, sections were incubated with VE1 hybridoma supernatant (monoclonal, dilution 1:5) at 37 °C for 32 min. Antibody incubation was followed by OptiView HQ Universal Linker for 12 min, incubation with OptiView HRP Multimer for 12 min, and signal amplification including the Ventana OptiView Amplification Kit (Ventana, catalogue number 760-099).
Statistics
The Kaplan–Meier plots and log-rank were conducted by JMP statistics software (version 9.0.0; SAS Institute, Cary, NC, USA). The 450k data was processed with the Bioconductor package minfi (version 1.12). For the unsupervised hierarchical clustering only CpGs with a standard deviation (SD) greater than 0.2 across the beta values were selected. The samples were clustered with Ward’s linkage method and the pairwise similarity was calculated using the Euclidean distance. For the hierarchical clustering of the CpGs average linkage and the Euclidian distance were applied. R version 3.1.3 and Bioconductor version 3.0 were used.
Results and discussion
Study and reference groups
To compare tumors diagnosed as IDHwt astrocytoma with other entities, a study and a reference set were formed. The study set contained 160 IDHwt astrocytomas with 40 being diagnosed as diffuse A II and 120 as AA III. The reference set contained 132 IDH mutated (IDHmut) astrocytomas, 100 IDHwt GBM and 21 H3F3A mutated gliomas (GBM-H3-K27 and GBM-H3-G34). All tumors of both study and reference groups were subjected to 450k methylation analysis and low-resolution copy number profiles were calculated from the methylation data. For comparison of OS a TCGA control cohort of 105 IDHmut anaplastic astrocytomas was used.
Molecular hallmark lesions in IDHmut and IDHwt astrocytic tumors of the reference cohort associate with distinct methylation patterns
Unsupervised hierarchical clustering of the tumors in the reference set revealed two main methylation clusters perfectly matching the IDH status (suppl. Fig. 1). Given the dominant hypermethylation phenotype of IDHmut tumors [14, 23] we then re-clustered the IDHwt tumors separately to achieve a more refined differentiation (suppl. Fig. 2).
The IDHwt tumors segregated into two main clusters. One of these clusters was composed only of GBM cases which again formed two subclusters reminiscent of the “mesenchymal” and “classic” methylation groups [21]. The second main cluster was enriched for H3F3A-mutant cases. The G34 and K27 mutant cases formed homogenous subclusters within this cluster confirming the reported distinctiveness of methylation profiles associated with both mutations [21]. A third subcluster composed of GBM cases reminiscent of the previously reported “RTK1” methylation cluster was also present [21]. Of note, two of the GBM reference cases formed a small subcluster adjacent to the H3F3A-K27 mutant cluster. Both cases were sequenced and found to be wild type for H3F3A.
In line with previous reports, [8] TERT promoter mutations were found in 88 % of all GBM cases irrespective of the methylation cluster but in only 2/132 (1 %) IDHmut cases and in none of the H3F3A mutant cases. TERT mutation is therefore considered a hallmark lesion for GBM. Analysis of CNPs confirmed 7p gain/10q loss to be highly characteristic for GBMs. In 88 % of such cases the whole chromosomes were affected. 7p gain/10q loss was present in 75 % of cases in the GBM cluster and in 20 % of GBM-H3-G34 but absent in all IDHmut and GBM-H3-K27 cases. EGFR amplification was detected in 38 % of GBMs but in only 1/132 IDHmut cases. EGFR amplification was differently distributed between the various GBM methylation groups with the highest frequency in the “classic” cluster. The combination of loss of the entire arm 10q combined with partial or complete losses on 13q and 14q was recognized as a distinct pattern present in 20 % of GBM but was absent in other groups. Therefore, 7p gain/10q loss, EGFR amplification and the combination of loss of the entire arm 10q combined with losses on 13q and 14q were also considered hallmark lesions for GBM. At least one of these hallmark alterations was present in 96 % of GBM cases. The distribution of molecular lesions in the reference sets is given in suppl. Table 1. Typical examples for CNPs are provided in Fig. 1.
From top to bottom: a typical copy number profile of GBM with gain of 7, loss of 10, CDKN2A deletion and EGFR amplification; b CNP of GBM-H3-K27 with co-gain of MDM2/CDK4 and 17q gain; c CNP of a MID-HGG with a deletion on 3q and a 17q gain; d typical profile of ganglioglioma with several whole chromosomal gains
H3F3A mutated gliomas exhibit morphological features of both, GBM and AA III. Clinically the presence or absence of necrosis has not been shown to be of prognostic relevance, and the clinical course of these patients is similar to those with GBM. For these reasons we pooled these tumors under the provisional designation GBM H3F3A mutated (GBM-H3). GBM-H3 frequently showed loss of chromosomal material or complex alterations on 3q (48 %) and frequently was accompanied by gain of 17q (33 %). In GBM-H3-K27 there was frequently a gain (45 %) or occasionally an amplification of MDM2 (9 %), often with a co-gain of CDK4 (45 %), a feature shared with a minority of GBMs (9 %) but virtually absent in all other cases. Interestingly, the two H3F3A wild type GBM reference cases clustering adjacent to H3F3A-K27 mutant GBM lacked conventional GBM hallmark alterations and exhibited CNP reminiscent to H3F3A mutant GBMs.
ATRX loss was present in 96 % of IDHmut astrocytomas, in 5/5 GBM-H3-G34, in 5/6 GBM-H3-K27, but only in 3/94 (3 %) GBM. A compilation of the alterations in the respective reference sets is provided in supplementary Table 1.
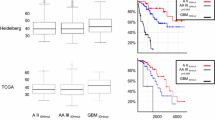
Establishing “integrated” diagnoses for IDH wild type astrocytomas and comparison with clinical outcomes
For the analysis of the study set, composed exclusively of IDHwt astrocytomas we used the same clustering strategy as for the reference set. First, the IDHwt astrocytomas were clustered with the reference set to identify possible cases with a G-CIMP phenotype. Two tumors (1 %) exhibited a G-CIMP phenotype and mapped to the IDHmut cluster despite showing IDH1/2 wild type sequences in Sanger sequencing and were provisionally designated astrocytoma-IDH-like. The remaining cases were then re-clustered without the IDHmut reference set. Based on the distribution of the molecular findings, the IDHwt astrocytoma set could be subdivided in four major groups (Fig. 2a). OS of the four groups is given in Fig. 3a.
Molecular profiling of non-CIMP IDHwt astrocytomas and GBM and GBM-H3 reference cases. The dendrogram depicts the results of unsupervised hierarchical clustering of methylation levels of the top 18856 most variant probes (SD > 0.20). The row “Tumor series” indicates study cases in red and reference cases in white. Diagnoses of reference cases were set prior to analysis and remained unchanged. Integrated diagnosis of study cases are indicated by different colors: GBM glioblastoma (gray), GBM-H3-G34 glioblastoma H3F3A-G34 mutated (green), GBM-H3-K27 glioblastoma H3F3A-K27 mutated (yellow), MID-HGG midline high grade glioma (light yellow), other (blue). For each sample associated results of TERT and H3F3A hotspot sequencing, ATRX immunohistochemistry and selected chromosomal copy number variants are indicated: black indicated presence of the alteration, white indicates absence of the alteration, gray indicates unknown status
Survival of patients: a overview over survival of the four IDHwt groups compared with AIII-IDHmut; b survival of patients with integrated diagnoses of GBM (left) or GBM-H2F3A-K27-mut (right) compared with patients diagnosed with IDHmut anaplastic astrocytoma; c survival of patients of the MID-HGG group compared with GBM and GBM-H3-K27 (left) and AIII-IDHmut (right)
All tumors were assessed for distinct molecular lesions. The integrated diagnosis of GBM was assigned to 124/160 (78 %) tumors. 115 tumors segregated to a GBM cluster and showed at least one of the GBM hallmark alterations TERT promoter mutation, 7p gain/10q loss, EGFR amplification or combined 10q/13q/14q deletion. Additional 6 tumors segregated to the GBM cluster and showed complex CNPs with gains and losses involving several chromosomes or gene amplifications. Therefore, these tumors were also considered to be GBMs. Two additional cases that clustered adjacent to GBM-H3-K27 cases but showed TERT promoter mutations were classified as GBMs. A single case which clustered together with GBM-H3-G34 cases but was H3F3A wild type and showed a complex CNP with EGFR amplification was also classified as GBM.
Accounting for 78 % of cases this was by far the most numerous group. Median survival in this group was 19.4 months—very well matching survival seen in GBM patients and thus further justifying the diagnosis of GBM. Presence or absence of TERT promoter mutations did not affect survival in this group.
15 (9 %) tumors exhibited a methylation profile typical of H3F3A mutated GBM and indeed harbored hotspot mutations; 12 were GBM-H3-K27 and three GBM-H3-G34. This group of 15 patients predominantly containing H3F3A-K27 mutations exhibited a median survival of 16.9 months matching the observation of very poor clinical courses in pediatric glioma with H3F3A-K27 mutations [21, 24]. Comparison of OS of this group with that of a control cohort of IDHmut astrocytoma is shown in Fig. 3b. H3F3A mutations were highly associated with loss of nuclear expression of ATRX (8/11 cases, 73 %) which further emphasizes that this group represents a clearly defined GBM. Likewise, the lack of TERT mutations further separates GBM-H3 from classical GBM.
Thirteen tumors (8 %) with a distinct methylation profile clustering adjacent to GBM-H3-K27 lacked H3F3A mutations. These tumors did not exhibit the hallmark alterations of GBM but showed complex CNP with overlaps to both G34 and K27 H3F3A mutant GBMs. This group was enriched for tumors of midline localization and has not previously been described. The median survival of 54.7 months may indicate a more favorable course than that of GBM patients, and, therefore this group may qualify as a second astrocytoma subgroup apart from IDHmut astrocytoma (Fig. 3c). Since OS still is shorter than that of IDHmut astrocytoma, we suggest that grouping with malignant astrocytic tumors may be appropriate (Fig. 3c). Therefore, this tumor group was provisionally termed ‘midline high grade glioma’ (MID-HGG).
6/160 (5 %) cases assigned to a common subcluster within the large GBM cluster lacked all hallmark alterations and demonstrated a CNP that was either completely balanced or showed only minor chromosomal alterations or trisomies. These cases were considered to most likely comprise an assortment of other lower grade neuroepithelial tumors. Case 3276 exhibited a CNP with several whole chromosomal gains including chromosomes 5 and 7. This pattern is typical for low grade glioneuronal tumors and is absent in diffuse astrocytomas [17]. Furthermore, this case harbored a BRAFV600E mutation strongly suggestive of ganglioglioma [10]. Case 68924 showed a similar CNP with trisomies of chromosomes 5, 7 and 20. Histologic re-evaluation demonstrated an Alcian blue-positive tumor matrix and an astrocytic as well as an oligodendroglial appearance of the tumor cells. Even though “floating neurons” were not found in this small biopsy a dysembryoplastic neuroepithelial tumor (DNT) seems the most likely diagnosis. A similar histological constellation was present in case 72220 which exhibited a completely balanced CNP. Similarly, case 72274 did not show any chromosomal aberrations and histological re-evaluation revealed an atypical ganglion cell component in this tumor consistent with ganglioglioma. Histological re-evaluation of case 49164 revealed tumor areas with bipolar tumor cells and Rosenthal fibers suggestive of pilocytic astrocytoma. Case 50133 had a unique methylation profile and a copy number profile showing gain of chromosome 12 and losses of chromosomes 13 and 22q. Histological re-evaluation revealed an overall low but perivascular accentuated GFAP expression and a “dot-like” EMA expression. It was concluded that this spinal tumor should be re-diagnosed as ependymoma.
Thus, molecular analyses completely resolved this group of morphologically diagnosed IDHwt astrocytomas into established entities. A compilation on the molecular alterations of IDHwt astrocytomas is provided in Table 1. The data for each individual tumor are listed in suppl. Table 2. The changes from the initial WHO diagnosis to an integrated diagnosis are shown in Fig. 4.
Changes from initial WHO to integrated diagnosis in 160 patients with IDHwt astrocytoma. Width of bars indicates relative proportions of the initial tumor groups. A II diffuse astrocytoma WHO grade II, AA III anaplastic astrocytoma WHO grade III, GBM glioblastoma, GBM-H3 glioblastoma H3F3A mutated, MID-HGG midline high grade glioma
In conclusion, these data demonstrate that 139/160 (87 %) of IDHwt astrocytomas on molecular and clinical grounds are indistinguishable from GBM or GBM-H3. Interestingly, upon separation of GBM from GBM-H3, the latter having the least favorable prognosis, the presence of TERT mutations in the GBM group did not influence survival (suppl. Fig. 3). 6/160 tumors were misdiagnosed other lower grade gliomas. Most interestingly, a group of 13 tumors emerged with a distinct methylation profile most similar to GBM-H3-K27 and enriched for midline tumors but lacked a H3F3A mutation. This group showed a trend towards better survival than GBMs.
Implication for future diagnostic approach to diffuse and anaplastic astrocytomas
In-depth genome wide molecular genetic analysis is available only in few diagnostic institutions. Even more common analysis methods, such as fluorescent in situ hybridization or gene sequencing are not affordable to all departments and access to immunohistochemistry can be limited in countries with emerging markets. That said, even with the absence of immunohistochemical and molecular genetic analyses tumors must be classifiable to provide a basis for therapy. In a recent meeting under sponsorship of the International Society of Neuropathology (ISN) held in Haarlem, the Netherlands, the consensus “ISN-Haarlem” guidelines were developed [13]. One notable proposition was the introduction of a “not otherwise specified” (NOS) category for tumors which could not be analyzed by IHC and/or molecular genetics in a desired way. While this is an important and pragmatic approach, it must be made very clear that the diagnoses of astrocytoma NOS, of astrocytoma IDHmut and of astrocytoma IDHwt refer to patients with very different characteristics: The diagnosis astrocytoma NOS inevitably will contain IDHmut astrocytomas and a considerable proportion of GBM, and less frequently other tumor entities as well as some oligodendrogliomas. The IDHmut astrocytoma group can be expected to be quite homogenous, however will contain some oligodendrogliomas which do require 1p/19 analysis for exclusion. Most problematic is the group of IDHwt astrocytomas because, as we show in this study, this set contains a variety of entities with defined molecular patterns. In the present series, 83 % of IDHwt astrocytomas exhibited clear molecular and clinical traits of GBM or GBM-H3. Related to this group are astrocytomas negatively scoring with the IDH1-R132H specific antibody. Because no more than 10 % of all IDH mutations in diffuse glioma are other than the IDH1-R132H type, this group can be expected to consist predominantly of GBM or GBM-H3. A schematic summary of this concept problem is given in Fig. 5.
Different sets of tumors are included in the classification categories of astrocytoma NOS, IDHmut, IDHwt, and IDH1-R132H-IHC-negative. From left to right: Astrocytoma NOS includes different tumors with the histopathological features of astrocytomas (left). Astrocytoma IDHmut constitutes a homogenous group (middle left), astrocytoma IDHwt (middle right) is a mixed bag with different tumors excluding astrocytoma IDHmut and astrocytoma IDH1-R132H-IHC-negative (right panel) is similar but contains those astrocytomas and oligodendrogliomas with rare IDH1 and IDH2 mutations. Size of boxes approximates the incidence in % and varies between institutions. PA pilocytic astrocytoma, DNT dysembryoplastic neuroepithelial tumor, GG ganglioglioma, PXA pleomorphic xanthoastrocytoma, O oligodendroglioma
Astrocytoma NOS is reserved for cases in which molecular characterization is not available. Most cases in which the IDH-R132H mutation has been excluded by immunohistochemistry, but which have not been sequenced for rare mutations, will be IDHwt and thus are best separated from the NOS designation.
The diagnosis of IDHmut astrocytoma can be considered to define a molecular and clinical homogenous entity. In fact, recent evidence points to only minor differences in clinical characteristics between patients with IDHmut diffuse A II and A III [2, 15, 18, 22]. We strongly recommend to use every possibility to come to this diagnosis by IHC with IDH1-R132H specific antibodies and, if required by sequencing exons 4 of IDH1 and IDH2.
In the face of the steadily increasing number of molecular parameters of potential diagnostic relevance, neuropathological practice must aim at reducing additional assays to the necessary. In our experience, a feasible approach further refined from a previous report [19] towards the diagnosis of diffuse gliomas starts with the analysis of ATRX and IDH1-R132H (H09) immunohistochemistry. A large group consisting of astrocytomas exhibiting nuclear ATRX loss and positively staining with IDH1-R132H antibody does not require further analysis. Tumors with nuclear ATRX loss and lack of H09 binding need to be sequenced for rare IDH mutations and H3F3A mutations: IDH mutations render these tumors astrocytoma H3F3A mutations place them into the GBM-H3 group. IDHmut tumors with nuclear ATRX expression require testing for the complete loss of 1p/19q. All tumors with 1p/19q co-deletion represent oligodendrogliomas. This will also identify those IDHmut astrocytomas lacking both ATRX mutations and 1p/19q co-deletions. Further, all tumors of proven IDHwt need not be tested for 1p/19q co-deletion, as the latter alteration in practice always is associated with IDH mutations [11, 19, 29]. IDHwt tumors most likely represent GBM or misinterpreted other low grade glial or glioneuronal lesions. If diagnostically necessary, the analysis of TERT promoter mutations is helpful in distinguishing between these groups with TERT mutations exclusively present in the GBM group. The MID-HGG group currently cannot be distinguished without methylation profiling. A flow diagram of a possible approach is provided in Fig. 6.
Diagnostic approach to tumors with diffuse astrocytic morphology starting with IDH1-R132H and ATRX immunohistochemistry. Following this diagnostic algorithm, an integrated diagnosis can be obtained with reduced involvement of molecular analyses. The MID-HGG group currently cannot be distinguished without methylation profiling. While the assessment of TERT promoter mutations is not required for distinguishing between distinct groups of malignant glioma (GBM, GBM-H3, MID-HGG), it may be helpful in separating IDHwt GBM from other IDHwt lower grade tumors
Conclusions
Our data demonstrate that approximately 80 % of IDHwt astrocytomas in fact represent underdiagnosed GBM or GBM-H3 and a smaller fraction represents misclassified lower grade tumors such as pilocytic astrocytomas, pleomorphic astrocytomas, DNTs or gangliogliomas. A further 8 % of the IDHwt astrocytomas emerge as a new midline high grade glioma subset.
References
Balss J, Meyer J, Mueller W, Korshunov A, Hartmann C, von Deimling A (2008) Analysis of the IDH1 codon 132 mutation in brain tumors. Acta Neuropathol 116:597–602
Cancer Genome Atlas Research Network (2015) Comprehensive, integrative genomic analysis of diffuse lower-grade gliomas. N Engl J Med. doi:10.1056/NEJMoa1402121
Capper D, Weißert S, Balss J et al (2010) Characterization of R132H mutation specific IDH1 Antibody binding in brain tumors. Brain Pathol 20:245–254
Hartmann C, Hentschel B, Wick W et al (2010) Patients with IDH1 wild type anaplastic astrocytomas exhibit worse prognosis than IDH1 mutated glioblastomas and IDH1 mutation status accounts for the unfavorable prognostic effect of higher age: implications for classification of gliomas. Acta Neuropathol 120:707–718
Hartmann C, Meyer J, Balss J et al (2009) Type and frequency of IDH1 and IDH2 mutations are related to astrocytic and oligodendroglial differentiation and age: a study of 1010 diffuse gliomas. Acta Neuropathol 118:469–474
Horbinski C (2013) What do we know about IDH1/2 mutations so far, and how do we use it? Acta Neuropathol 125:621–636
Ichimura K, Pearson DM, Kocialkowski S, Backlund LM, Chan R, Jones DT, Collins VP (2009) IDH1 mutations are present in the majority of common adult gliomas but are rare in primary glioblastomas. Neuro Oncol 11:341–347
Killela PJ, Reitman ZJ, Jiao Y et al (2013) TERT promoter mutations occur frequently in gliomas and a subset of tumors derived from cells with low rates of self-renewal. Proc Natl Acad Sci 110:6021–6026
Koelsche C, Sahm F, Capper D et al (2013) Distribution of TERT promoter mutations in pediatric and adult tumors of the nervous system. Acta Neuropathol 126:907–915
Koelsche C, Wöhrer A, Jeibmann A, Schittenhelm J, Schindler G, Preusser M, Lasitschka F, von Deimling A, Capper D (2013) Mutant BRAF V600E protein in ganglioglioma is predominantly expressed by neuronal tumor cells. Acta Neuropathol 125:891–900
Labussiere M, Idbaih A, Wang XW et al (2010) All the 1p19q codeleted gliomas are mutated on IDH1 or IDH2. Neurology 74:1886–1890
Louis D, Ohgaki H, Wiestler O, Cavenee W (2007) World Health Organization classification of tumours of the central nervous system. In: Bosman F, Jaffe E, Lakhani S, Ohgaki H (eds) World Health Organization Classification of Tumours, 4th edn. IARC, Lyon
Louis DN, Perry A, Burger P et al (2014) International Society of Neuropathology—Haarlem consensus guidelines for nervous system tumor classification and grading. Brain Pathol 24:429–435. doi:10.1111/bpa.12171
Noushmehr H, Weisenberger DJ, Diefes K et al (2010) Identification of a CpG island methylator phenotype that defines a distinct subgroup of glioma. Cancer Cell 17:510–522
Olar A, Wani KM, Alfaro-Munoz KD et al (2015) IDH mutation status and role of WHO grade and mitotic index in overall survival in grade II-III diffuse gliomas. Acta Neuropathol 129:585–596
Parsons DW, Jones S, Zhang X et al (2008) An integrated genomic analysis of human glioblastoma multiforme. Science 321:1807–1812
Prabowo AS, van Thuijl HF, Scheinin I et al (2015) Landscape of chromosomal copy number aberrations in gangliogliomas and dysembryoplastic neuroepithelial tumours. Neuropathol Appl Neurobiol. doi:10.1111/nan.12235
Reuss DE, Mamatjan Y, Schrimpf D et al (2015) IDH mutant diffuse and anaplastic astrocytomas have similar age at presentation and little difference in survival: a grading problem for WHO. Acta Neuropathol 129:867–873
Reuss DE, Sahm F, Schrimpf D et al (2015) ATRX and IDH1-R132H immunohistochemistry with subsequent copy number analysis and IDH sequencing as a basis for an “integrated” diagnostic approach for adult astrocytoma, oligodendroglioma and glioblastoma. Acta Neuropathol 129:133–146
Schwartzentruber J, Korshunov A, Liu X et al (2012) Driver mutations in histone H3.3 and chromatin remodelling genes in pediatric glioblastoma. Nature 482:226–231
Sturm D, Witt H, Hovestadt V et al (2012) Hotspot mutations in H3F3A and IDH1 define distinct epigenetic and biological subgroups of glioblastoma. Cancer Cell 22:425–437
Suzuki H, Aoki K, Chiba K et al (2015) Mutational landscape and clonal architecture in grade II and III gliomas. Nat Genet 47:458–468. doi:10.1038/ng.3273
Turcan S, Rohle D, Goenka A et al (2012) IDH1 mutation is sufficient to establish the glioma hypermethylator phenotype. Nature 483:479–483
Venneti S, Santi M, Felicella MM et al (2014) A sensitive and specific histopathologic prognostic marker for H3F3A K27M mutant pediatric glioblastomas. Acta Neuropathol 128:743–753
Watanabe T, Nobusawa S, Kleihues P, Ohgaki H (2009) IDH1 mutations are early events in the development of astrocytomas and oligodendrogliomas. Am J Pathol 174:653–656
Weller M, Weber RG, Willscher E et al (2015) Molecular classification of diffuse cerebral WHO grade II/III gliomas using genome- and transcriptome-wide profiling improves stratification of prognostically distinct patient groups. Acta Neuropathol 129:679–693
Wiestler B, Capper D, Sill M et al (2014) Integrated DNA methylation and copy-number profiling identify three clinically and biologically relevant groups of anaplastic glioma. Acta Neuropathol 128:561–571
Yan H, Parsons DW, Jin G et al (2009) IDH1 and IDH2 mutations in gliomas. N Engl J Med 360:765–773
Yip S, Butterfield YS, Morozova O et al (2012) Concurrent CIC mutations, IDH mutations, and 1p/19q loss distinguish oligodendrogliomas from other cancers. J Pathol 226:7–16
Acknowledgments
Part of this work was undertaken at UCLH/UCL which received funding from NIHR. We thank Maria Fernanda Ruiz, Kerstin Lindenberg, Viktoria Zeller for technical assistance. FS is a fellow of the Medical Faculty Heidelberg Physician-Scientist Program. Supported by the Bundesministerium für Bildung und Forschung (BMBF) program SYS-GLIO and the German Cancer Net (DKTK) joint funding project “Next generation molecular diagnostics of malignant gliomas”.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
401_2015_1454_MOESM5_ESM.xlsx
Supplementary material 5 (XLSX 26 kb) Supplementary Table 2: Molecular alterations in 160 patients with IDHwt astrocytoma
Rights and permissions
About this article
Cite this article
Reuss, D.E., Kratz, A., Sahm, F. et al. Adult IDH wild type astrocytomas biologically and clinically resolve into other tumor entities. Acta Neuropathol 130, 407–417 (2015). https://doi.org/10.1007/s00401-015-1454-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-015-1454-8