Abstract
Multiple different pathological protein aggregates are frequently seen in human postmortem brains and hence mixed pathology is common. Mixed dementia on the other hand is less frequent and neuropathologically should only be diagnosed if criteria for more than one full blown disease are met. We quantitatively measured the amount of hyperphosphorylated microtubule associated tau (HP-τ), amyloid-β protein (Aβ) and α-synuclein (α-syn) in cases that were neuropathologically diagnosed as mixed Alzheimer’s disease (AD) and neocortical Lewy body disease (LBD) but clinically presented either as dementia due to AD or LBD, the latter including dementia with Lewy bodies (DLB) and Parkinson’s disease dementia (PDD). Our study group consisted of 28 cases (mean age, 76.11 SE: ±1.29 years; m:f, 17:11) of which 19 were neuropathologically diagnosed as mixed AD/DLB. Clinically, 8 mixed AD/DLB cases were diagnosed as AD (cAD), 8 as DLB (cDLB) and 3 as PDD (cPDD). In addition, we investigated cases that were both clinically and neuropathologically diagnosed as either AD (pure AD; n = 5) or DLB/neocortical LBD (pure DLB; n = 4). Sections from neocortical, limbic and subcortical areas were stained with antibodies against HP-τ, Aβ and α-syn. The area covered by immunopositivity was measured using image analysis. cAD cases had higher HP-τ loads than both cDLB and cPDD and the distribution of HP-τ in cAD was similar to the one observed in pure AD whilst cDLB showed comparatively less hippocampal HP-τ load. cPDD cases showed lower HP-τ and Aβ loads and higher α-syn loads. Here, we show that in neuropathologically mixed AD/DLB cases both the amount and the topographical distribution of pathological protein aggregates differed between distinct clinical phenotypes. Large-scale clinicopathological correlative studies using a quantitative methodology are warranted to further elucidate the neuropathological correlate of clinical symptoms in cases with mixed pathology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) and Lewy body disease (LBD) are the most prevalent neurodegenerative diseases associated with age-related dementia. Although AD and LBD have overlapping clinical features, each of these diseases has distinct clinical phenotypes, which for LBD is distinguished into cognitive (dementia with Lewy bodies, DLB) and motor (Parkinson’s disease dementia, PDD) presentations.
AD manifests clinically as impairment in memory and learning, aphasia and executive dysfunction [20, 22, 23, 39, 60], whilst core features associated with LBD (inclusive DLB and PDD) include fluctuating cognition, the presence of recurrent well-formed visual hallucinations, REM sleep behaviour disorder and extrapyramidal symptoms (EPS) [17, 57, 58, 78]. The distinction between DLB and PDD is based on the time of dementia onset in relation to EPS; in PDD, EPS precedes the onset of dementia by at least 12 months, whereas in DLB dementia is concomitant with or precedes EPS. There are no neuropathological criteria that distinguish DLB from PDD [26, 54, 57, 58, 68].
The major neuropathological features of AD include neurofibrillary tangles (NFTs) and neuropil threads (NTs) which are composed of aggregated hyperphosphorylated microtubule associated tau (HP-τ), forming intracytoplasmic inclusions (NFTs) and dendritic and axonal depositions (NTs), respectively [36, 63]. Extracellular depositions composed of amyloid-β protein (Aβ; e.g. senile plaques, fleecy amyloid) and neuritic plaques composed of both Aβ and HP-τ are also characteristic of AD [24]. The neuropathological diagnosis of LBD is based on the presence of α-synuclein (α-syn) aggregates in the form of Lewy bodies (LBs) in neuronal somata and Lewy neurites (LNs) in neuronal processes [53, 66].
Neurodegenerative diseases are neuropathologically classified according to the type and anatomical distribution of the most prevalent neuropathological lesion(s) and several internationally recognised semi-quantitative staging systems to evaluate the extent of disease progression are currently used; Braak NFT staging (I–VI) and Thal amyloid phases (1–5) are used to assess the topographical distribution of NFTs/NTs [12] and β-amyloid deposits [77], respectively, whilst Consortium to Establish a Registry for Alzheimer’s Disease (CERAD) criteria are used to score neuritic plaques (neg, A, B or C) [62]. Each ‘score’ is taken into account when determining the degree of AD neuropathologic change according to the National Association on Ageing–Alzheimer’s association (NIA-AA) criteria [36, 63]. The grading and the anatomical location of LBs and LNs are determined by Braak LB staging (I–VI) [11] and Newcastle–McKeith criteria [58], the latter distinguishing between brainstem predominant, limbic (transitional) and neocortical LBD, respectively.
However, it has been suggested that pathologies most commonly associated with a single neurodegenerative disease are often not exclusive to this particular disease [4, 42, 44, 49, 67, 69]. For example, large-scale autopsy studies revealed that between 43 and 53 % of cases exhibited pathological lesions associated with more than one neurodegenerative disease [43, 49] and the presence of such mixed pathologies increases with age [45].
The impact of multiple pathologies on the clinical phenotype of dementia has been investigated [47, 65, 71]; in particular, AD patients with concomitant Lewy body pathology showed an accelerated decline in cognition and more aggressive disease course compared to AD patients that showed AD pathology only at the postmortem examination [65, 71]. More recently, the presence of TDP-43 pathology in AD cases was associated with greater global cognitive impairment and more medial lobe atrophy compared to AD cases that were TDP-43 negative [47]. These findings suggest that multiple neurodegenerative pathologies may lower the threshold for overt clinical dementia, similar to what has been suggested for concomitant cerebrovascular pathology [40, 70].
In human postmortem brains, neuropathological hallmark lesions of more than one neurodegenerative disease are frequently seen and this is referred to as “mixed pathology” [46]. However, in such cases, one hallmark lesion is often more prevalent and considered to be the main underlying pathology causing clinical dementia, whilst additional pathologies are present to a lesser extent (e.g. DLB with additional limited AD type pathology). On the other hand, the neuropathological diagnosis of mixed dementia should be stated if the neuropathological criteria for two (or more) distinct neurodegenerative diseases are met [7, 44]. In such mixed dementia cases, the severity of each characteristic neuropathological lesion may have independently been the cause for clinical dementia.
Here, we report on a set of cases that were neuropathologically classified as mixed AD/DLB because they fulfilled neuropathological criteria for both AD (i.e. high neuropathologic change [63]) and DLB (i.e. neocortical LBD [58]). Hence, the severity of either AD or DLB pathology alone would have been sufficient to cause clinical dementia in these cases. Clinically, a proportion of these cases were diagnosed as AD, whereas others were diagnosed as DLB or PDD. Since semi-quantitative assessment according to standardised criteria [1–3] failed to show differences in the amount of pathology between clinical AD, DLB and PDD cases, we investigated whether respective differences could be detected using a quantitative methodology.
Materials and methods
Tissue preparation and neuropathological diagnosis
We searched the Newcastle Brain Tissue Resource (NBTR) for cases fulfilling neuropathological criteria for mixed AD/DLB and found 19 such cases, which were all included in this study. In total, brain tissue from 28 donors (mean age, 76.11 SE: ±1.29 years; male 17; female, 11; mixed AD/DLB, 19; pure AD 5; pure DLB 4; Table 1) was obtained from the NBTR in accordance with the approval of the joint Ethics Committee of Newcastle and North Tyneside Health Authority and following NBTR brain banking procedures. During life, patients underwent clinical assessments (by board certified Old Age Psychiatrists or Neurologists) with cognitive evaluation including Mini-Mental State Examination (MMSE) [28] and the rate of cognitive decline [65] was determined for cases with more than one MMSE score available. Clinician-assessed diagnoses of dementia subtype were made according to standard international clinical criteria for AD, DLB and PDD [26, 58–60]. Hence, AD cases did neither show core (i.e. spontaneous cognitive fluctuations, spontaneous motor Parkinsonism, complex, persistent visual hallucinations) nor suggestive (i.e. REM sleep behaviour disorder, neuroleptic sensitivity, positive dopaminergic imaging) features of LBD, respectively. After death, but blinded to neuropathological diagnoses, clinical diagnoses were reviewed by AJT (or Ian McKeith) and checked against relevant standard international clinical criteria [26, 58–60].
At autopsy the right hemisphere, brainstem and cerebellum were immersion fixed in 4 % buffered aqueous formaldehyde for 4–6 weeks.
Paraffin-embedded blocks containing frontal, temporal, parietal and occipital cortices, cingulate and hippocampus, striatum (including caudate nucleus and putamen), amygdala, midbrain and locus coeruleus were sectioned at 6 μm and mounted onto 4 % 3-aminopropyltriethoxysilane (APES)-coated glass slides.
Sections were immunostained for monoclonal antibodies against HP-τ (AT8, dilution 1:4000, Innogenetics, Ghent, Belgium) Aβ (4G8, dilution 1:15,000, 4G8, Signet Labs, Dedham, MA, USA) and α-syn (α-syn, dilution 1:200, Chemicon, Hofheim, Germany). Prior to immunostaining, antigen retrieval was performed by microwaving slides in 0.01 mL−1 citrate buffer for 10 min (AT8), pressure cooking in 0.01 mol L−1 EDTA for one and a half minutes (α-syn) or immersed for 1 h in concentrated Formic acid (4G8). Immunopositivity was detected using a MENAPATH HRP polymer detection kit (Menarini diagnostics, Berkshire, UK) with 3,3 diaminobezidine (DAB) as a chromagen and haematoxylin was used as counter stain. Tissue was subsequently dehydrated through a series of alcohols, cleared and mounted using DPX (CellPath, Powys, UK).
Independently of clinical diagnoses, all cases were subjected to a standardised neuropathological assessment. Blind to clinical diagnoses, neuropathological diagnoses were based on semi-quantitative assessment [1, 2, 81] and assigned using accepted international neuropathological criteria including neuritic Braak stages [12], Thal amyloid phases [77], CERAD scores [62], NIA-AA scores [63] and McKeith criteria [58]. Cerebral amyloid angiopathy (CAA) was scored according to the method described by Olichney and colleagues [64] and depending on the presence of capillary CAA the type of CAA was assessed [76].
19 cases fulfilled neuropathological criteria for both AD (i.e. NIA-AA: high neuropathologic change [63]) and DLB (i.e. McKeith neocortical LBD [58]). Of these neuropathologically mixed AD/DLB cases, 8 (42.1 %) were clinically diagnosed as AD (cAD), 8 (42.1 %) as DLB (cDLB) and 3 (15.8 %) as PDD (cPDD; Table 1). For comparison, we also selected cases which were neuropathologically diagnosed as AD (pure AD; n = 5) or DLB (pure DLB, n = 4). Of note, pure DLB cases showed low AD neuropathologic change [63] typical of what is seen in non-demented elderly individuals whilst pure AD cases lacked any α-syn pathology. Clinically, pure AD and pure DLB cases had been diagnosed as AD and DLB, respectively (Table 1).
CAA with capCAA was present in 9 cases whilst 15 cases showed CAA without capillary involvement. There were no differences in the type of CAA between cAD, cDLB and cPDD although there was an increased severity of CAA in cAD group with 50 % of cases having a score of 3 or 4 whilst none of the cDLB cases had a score higher than 2 (Table 1).
Quantification of protein aggregates: image analysis
Image analysis was performed using AT8, 4G8 and α-syn stained slides from frontal (Brodmann areas (BA) 9,10 and 46), temporal (BA 20, 21, 22, 41 and 42), parietal (BA 40), occipital (BA 17, 18 and 19) and cingulate (BA 24) cortices, posterior hippocampus, striatum (i.e. caudate nucleus, putamen; at the level of the amygdala), amygdala, substantia nigra (at the level of trigeminal nerve) and locus coeruleus. Of note, great care was taken to minimise any variation among cases regarding the specific topographical localisation on which analyses were performed.
Multiple adjacent single images (SI) were captured at 200× magnification using a Nikon Eclipse 90i microscope and DsFi1 camera (Nikon, Surry UK) with a fully motorised stage coupled to a PC and combined to one large image (LI) by NIS elements software (Nikon). If necessary, LI were subjected to manual setting of regions of interest (ROI; see below).
The size of measured areas depended on the assessed brain region; in each cortical region six LI were assessed and each LI encompassed a cortical strip which included all cortical layers and consisted of 8 adjacent SI forming a rectangle of 0.34 mm × 3 mm (of note, one SI measures 0.34 mm × 0.43 mm but in the final LI individual SI overlap by 0.03 mm). If necessary, ROI were set to exclude white matter and meningeal structures (Fig. 1a). It has been previously shown that densities of pathological protein aggregates (e.g. Aβ) differ between gyri and sulci [32] and therefore three gyri and three sulci were assessed per cortical region. In the hippocampus, 1 × 2 SI resulting in a rectangle of 0.34 mm × 0.8 mm was taken from hippocampal subfields CA2, CA3 and CA4 and 1 × 4 SI resulting in a rectangle of 0.34 mm × 1.54 mm was taken in CA1. If necessary, ROI were set to encompass the pyramidal cell layer only in CA1-3 whilst the entire LI of CA4 was used for analysis (Fig. 1b). In each the caudate nucleus, putamen and amygdala, three LI (0.88 mm × 1.17 mm), which were composed of 3 × 3 SI, were analysed entirely (Fig. 1c). Four SI (0.34 mm x 0.43 mm) were taken from the substantia nigra and were analysed without further setting of an ROI (Fig. 1d). One SI covering the entire locus coeruleus was used for analysis after setting an appropriate ROI to ensure that immunopositivity was measured in the locus coeruleus only (Fig. 1e).
Examples of regions of interest (ROI) delineating the area used for quantification. For assessment of cortical regions (a) 8 individual images were taken at ×200 magnification forming 1 large image (area covered: 0.34 mm × 3 mm, green rectangle) that encompassed a cortical strip including all layers of the cortex (CTX). A ROI (red rectangle) was manually applied to exclude white matter (WM—delineated by blue dotted line) and meningeal structures (a). For assessment of the hippocampus (b) 2 individual images resulting in 1 rectangular image (green rectangle, area covered: 0.34 mm × 0.8 mm) were taken at ×200 magnification in hippocampal subfields (CA2, CA3 and CA4) and 4 individual images resulting in a rectangle of 0.34 mm × 1.54 mm (green rectangle) were taken in CA1. ROI (red rectangles) were set to encompass the pyramidal cell layer only in CA1-3 whilst the entire image in CA4 was assessed. For quantification in the caudate ((c) delineated by grey dotted line), 3 areas were selected for assessment, with each area comprising of 9 individual images at ×200 magnification forming 1 large image (area covered: 0.88 mm × 1.17 mm). For quantification of the substantia nigra of the midbrain ((d) delineated by grey dotted line), four single images (area covered in one single image: 0.34 mm × 0.43 mm) were taken at ×200 magnification, and a mean of all four values was calculated for the final measurement. For the assessment of the locus coeruleus, a ROI (red line) was placed manually to ensure quantification was limited to the locus coeruleus only (e). Scale bars represent 500 μm in a–d and 100 μm in e
The measurement of immunopositivity and subsequent calculation of the percentage area covered by immunopositivity was performed as described previously [55]. Briefly, red, green and blue (RGB) thresholds that determine the pixels which are included in the binary layer used for measurement were standardised separately for each AT8, 4G8 and α-syn immunopositivity and thresholds were set at a level that was reached by immunopositive pathological structures only (except amyloid precursor protein (APP); see below). RGB intensity values are measured on a scale between 0 and 255 (see NIS elements version 3.0, user guide, 2008, Nikon, Surry UK) and were set as follows: AT8: R25-170, G27-156, B11-126; 4G8: R50-180, G20-168, B8-139, α-syn: R15-161, G7-139, B4-133. Thereby, non-specific background staining did not reach the threshold and was not included into the measurement. In addition to RGB thresholds, we set a restriction threshold for the assessment of 4G8 immunopositivity that excluded the measurement of immunopositive signals of a size below 100 μm2; this was necessary to ensure that physiological, cellular APP that is stained with 4G8 antibody was not included in the measurement. Of note, the exclusion of areas below 100 μm2 implies that pathological Aβ depositions of less than 100 μm2 were not included into the measurement. However, diffuse Aβ depositions and Aβ plaques are typically larger than 100 μm2 [24].
The amount of immunopositivity (load) was stated as the percentage of the total measured area that was covered by immunopositive signals. The respective values are expressed as HP-τ load (AT8), Aβ load (4G8) and α-syn load.
Mean frontal, temporal, parietal, occipital and cingulate loads (i.e. mean value of 6 LI loads) were calculated. Loads of individual hippocampal subfields and caudate nucleus and putamen were used to calculate a mean hippocampal and a mean striatal load, respectively. No mean values were calculated for the amygdala, substantia nigra and locus coeruleus.
APOE genotyping
Except for one cDLB case which had no frozen tissue available, all mixed AD/DLB cases underwent APOE genotyping; genomic DNA was extracted from frozen tissue taken from the left lateral cerebellum using the QIAamp DNA Mini-kit and QIAGEN EZ1 advanced XL automated system (Qiagen, Manchester, UK) according to the manufacturer’s instructions. Genotyping of APOE polymorphisms (rs429358 and rs7412) was determined by real-time PCR [18] using the 7900HT fast Real-Time PCR system (Applied Biosystems, Paisley, UK).
Statistical analysis
The Statistical Package for Social Sciences software (SPSS ver. 21) was used for statistical evaluation. Since our data were not normally distributed (Kolmogorov–Smirnov p < 0.01), we used Kruskal–Wallis to determine overall group differences and a non-parametric paired t test (Mann–Whitney U) to assess individual differences in pathological burden between clinical phenotypes. Friedman’s test with post hoc Wilcoxon signed-rank test was employed to assess differences in pathological burden between individual cortices within each clinical phenotype. Allele frequencies were calculated using the allele counting method. Hardy–Weinberg equilibrium was tested by a χ 2 goodness-of-fit test, and χ 2 was employed to assess differences in APOE allele frequencies between phenotypes.
Results
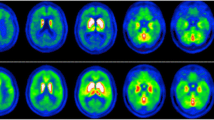
Patient demographics including clinical and neuropathological characteristics are provided in Table 1. The study cohort was subdivided according to clinical diagnoses into cAD, cDLB and cPDD. Using routine semi-quantitative scoring criteria, no significant differences in the severity of HP-τ, Aβ and α-syn were seen between cAD, cDLB and cPDD since—not surprisingly—scores were “severe” in most areas (Fig. 2; except for the three cPDD cases which showed considerably lower HP-τ in cingulate and frontal cortices).
Semi-quantitative (SQ) assessment of hyperphosphorylated tau (HP-τ), β-amyloid (Aβ) and α-synuclein (α-syn) in clinical Alzheimer’s disease (cAD) clinical dementia with Lewy bodies (cDLB) and clinical Parkinson’s disease dementia (cPDD) cases. Areas assessed were frontal (a), temporal (b), parietal (c), occipital (d), cingulate (e), hippocampus (f), striatum (g), substantia nigra (SN) (h) and locus coeruleus (LC) (i). 0 no pathology, 1 mild pathology, 2 moderate pathology, 3 severe pathology. *p < 0.05
Clinical characteristics
There were no overt differences in age of dementia onset between the clinical groups, however, the cDLB and cPDD had a shorter survival time from the onset of cognitive decline compared to the cAD group (cDLB mean 7.5 years, SE ±1.52; cPDD mean 7.33 years, SE ±2.4; cAD mean 9.38 years, SE ±1.31; p > 0.05; Table 2). The onset of dementia in pure AD cases was 8.45 years later than in cAD (pure AD, 74.2 years SE ±2.71; cAD, 65.75 years SE ±3.32; Table 2). As expected, cPDD cases had an earlier onset of EPS (mean 64.33 years, SE ±4.33) than the cDLB cases (mean 71.83 years, SE ±2.44; p > 0.05; Table 2).
cAD cases had lower final MMSE scores (mean: 6.0, SE ±3.21) compared to cDLB (mean: 8.43, SE ±3.64; p > 0.05) and cPDD (mean: 8.0, SE ±3.56; p > 0.05) as well as a higher rate of cognitive decline (mean: −7.17, SE ±2.8) compared to cDLB (mean: −3.83, SE ±0.94; p > 0.05) and cPDD (mean: −3.5, SE ±1.32; p > 0.05; Table 2).
Hyperphosphorylated tau loads
HP-τ load was higher in cAD compared to cDLB and cPDD in all regions except the frontal cortex where HP-τ load in cDLB was higher than in both cAD and cPDD (Fig. 3; Table 3). Overall significant differences were detected (Kruskal–Wallis p < 0.05) and significant respective differences were seen only in the hippocampus (p < 0.05), striatum (putamen p < 0.05) and locus coeruleus (p < 0.01) of cAD when compared to cDLB and in hippocampus (p < 0.05), striatum (putamen p < 0.05), neocortical regions (frontal, temporal and parietal; p < 0.05), striatum (putamen p < 0.05) and cingulate cortex (p < 0.05) of cAD when compared to cPDD.
Hyperphosphorylated tau (HP-τ) load differs between clinical Alzheimer’s disease (cAD) clinical dementia with Lewy bodies (cDLB) and clinical Parkinson’s disease dementia (cPDD) cases. Neurofibrillary tangles ((a) NFTs—arrow) and neuropil threads ((a) NTs—arrowhead) immunopositive for AT8 antibody were included in the quantitative assessment. The area positive for AT8 immunoreactivity is shaded red in (b). Box plots show differences in HP-τ loads between clinical phenotypes in frontal cortex (c), temporal cortex (d), parietal cortex (e), occipital cortex (f), cingulate (g), hippocampus (h), striatum (i.e. mean of caudate and putamen values) (i), amygdala (j), substantia nigra (SN) (k) and locus coeruleus (LC) (l). *p < 0.05, **p < 0.01, scale bar 20 μm, valid for a and b
In cDLB, HP-τ load was significantly higher in frontal (p < 0.05) and cingulate cortices (p < 0.05) compared to cPDD, whilst HP-τ load was significantly higher in the locus coeruleus in cPDD compared to cDLB.
When comparing HP-τ loads in limbic and cortical regions within the same clinical phenotype the cAD group showed highest HP-τ loads in the temporal cortex (mean 19.9 %, SE ±4.06), followed by hippocampus (mean 13.81 % SE ±2.58), occipital cortex (mean 13.14 %, SE ±3.68), parietal cortex (mean 12.04, SE ±2.67), cingulate gyrus (mean 10.5 %, SE ±2.7) and frontal cortex (mean 4.6 %, SE ±1.33; p > 0.05; Fig. 4a).
Scatter plots showing the hierarchical distribution of hyperphosphorylated tau (HP-τ), β-amyloid and α-synuclein (α-syn) loads of cortical and limbic regions in neuropathologically mixed AD/DLB cases which clinically either presented as Alzheimer’s disease (cAD), dementia with Lewy bodies (cDLB) or Parkinson’s disease dementia (cPDD) and in neuropathologically and clinical pure AD cases (pAD; a and b) or neuropathologically and clinical pure DLB cases (pDLB; c). cAD cases exhibited a similar pattern of HP-τ distribution to that observed pAD) cases with the temporal cortex being the most severely affected area in both, whilst the occipital cortex was the cortical region most severely affected by HP-τ in both clinical dementia with Lewy bodies (cDLB) and clinical Parkinson’s disease dementia (cPDD) (a). β-Amyloid displayed a different pattern of distribution with cAD displaying a similar hierarchical pattern of cortical distribution to pAD. This differed to that seen in cDLB and cPDD (b). The limbic regions (hippocampus and cingulate) were most affected by α-synuclein (α-syn) and the occipital cortex was least affected in all phenotypes (c)
Interestingly, cDLB and cPDD displayed a different pattern of HP-τ distribution to the one observed in cAD. In cDLB, the occipital cortex exhibited the highest HP-τ load (mean 13.06 %, SE ±3.83) followed by temporal cortex (mean 11.38 %, SE ±2.62), parietal cortex (mean 10.49 %, SE ±3.19), cingulate cortex (mean 8.45 %, SE ±2.77), hippocampus (mean 7.72 %, SE ±1.36) and frontal cortex (mean 7.51 %, SE ±2.17; p > 0.05; Fig. 4a). On the other hand, cPDD cases showed highest HP-τ loads in the hippocampus (mean 11.58 %, SE ±5.37), followed by occipital (mean 5.69 %, SE ±3.71), temporal (mean 3.49 %, SE ±2.04), parietal (mean 0.95 %, SE ±0.49), cingulate gyrus (mean 0.72 %, SE ±0.33) and frontal (mean 0.4 %, SE ±0.24; p > 0.05, Fig. 4a).
Similar to cAD, pure AD showed highest HP-τ load in the temporal cortex (mean 18.45 %, SE ±5.48), but this was followed by occipital (mean 16.44 %, SE ±4.79), parietal (mean 13.19 %, SE ±5.65) and frontal (mean 11.68 %, SE ±5.83) cortices whilst lower loads were seen in the hippocampus (mean 11.12 %, SE ±5.02) and cingulate gyrus (mean 8.46 %, SE ±3.87; p > 0.05; Fig. 4a). HP-τ load did not differ significantly between pure AD and cAD, and HP-τ loads in cDLB and cPDD were significantly lower than in pure AD in those regions that showed significantly lower loads when cDLB and cPDD were compared with cAD (see above).
β-Amyloid loads
No significant differences were seen in Aβ loads between cAD and cDLB (Fig. 5; Table 4). However, both cAD and cDLB showed significantly higher Aβ loads in the temporal cortex, and cDLB in the cingulate, when compared to cPDD (p < 0.05; Fig. 5).
β-Amyloid loads differ between clinical Alzheimer’s disease (cAD) clinical dementia with Lewy bodies (cDLB) and clinical Parkinson’s disease dementia (cPDD) in the mixed AD/DLB cohort. All β-amyloid deposits immunopositive for 4G8 antibody (a) were included in the analysis (shaded in red (b)). Restriction thresholds (see “Materials and methods” for details) were applied to include all pathological lesions in the assessment whilst excluding physiological cellular amyloid precursor protein (APP) (b—arrow). Differences in β-amyloid loads between the clinical phenotypes are illustrated in frontal cortex (c), temporal cortex (d), parietal cortex (e), occipital cortex (f), cingulate (g), hippocampus (h), striatum (i.e. mean of caudate and putamen values) (i), amygdala (j), substantia nigra (SN) (k) and locus coeruleus (LC) (l). *p < 0.05; scale bar 20 μm, valid for a and b
In cAD, Aβ loads were highest in the cingulate cortex (mean 12.58 %, SE ±2.28) followed by frontal (mean 11.38 %, SE ±1.8), parietal (mean 8.35 %, SE ±1.95), temporal (mean 8.15 %, SE ±1.09) and occipital cortices (mean 4.18 %, SE ±0.65) and hippocampus (mean 2.16 %, SE ±0.44; Fig. 4b). Overall differences between lobes were observed (Friedman’s p < 0.05). Here, cingulate, frontal, temporal and parietal Aβ loads were significantly higher than occipital Aβ load (cingulate: p < 0.01, all others: p < 0.05), whilst all cortical Aβ loads were significantly higher than hippocampal Aβ load (p < 0.05).
Aβ load in cDLB was highest in the cingulate cortex (mean 13.39 %, SE ±1.5) followed by temporal (mean 10.58 %, SE ±2.4), frontal (mean 8.89 %, SE ±1), parietal (mean 8.59 %, SE ±0.72) and occipital cortices (mean 5.87 %, SE ±0.7) and hippocampus (mean 4.45 %, SE ±1.34; Fig. 4b). In cDLB cingulate loads were significantly higher than parietal, occipital and hippocampal loads (p < 0.05). Overall differences between lobes were observed (Friedman’s p < 0.05). Temporal Aβ loads were significantly higher than hippocampal and occipital ones as were parietal compared to occipital Aβ loads, respectively (p < 0.05).
In cPDD, we found highest Aβ loads in the frontal cortex (mean 11 %, SE ±1.87) followed by cingulate (mean 7.59 %, SE ±1.01), parietal (mean 6.66, SE ±2.26), occipital (mean 4.63 %, SE ±2.06) and temporal cortices (mean 4.35 %, SE ±0.93) and hippocampus (mean 2.01 %, SE ±0.7; p < 0.05; Fig. 4b).
Like in cAD, pure AD cases showed highest Aβ load in the frontal cortex (mean 10.35 %, SE ±1.58), followed by parietal (mean 8.74 %, SE ±1.39), cingulate (mean 8.46 %, SE ±3.87), temporal (mean 6.5 %, SE ±0.74), and occipital cortices (mean 4.52 %, SE ±1.08) and hippocampus (mean 2.62 %, SE ±0.67; Fig. 4b). However, unlike cAD cases, in pure AD no significant differences in Aβ loads were observed between areas and regional Aβ loads in pure AD did not differ significantly from the ones seen in cAD, cDLB and cPDD.
α-Synuclein loads
α-Syn loads were highest in the amygdala and in the majority of areas analysed were comparable in all three mixed AD/LBD clinical phenotypes and (Fig. 6). Overall differences were seen between clinical phenotypes (Kruskal–Wallis p < 0.05). pAD cases had significantly less α-syn compared to cAD in parietal, locus coeruleus (both p < 0.05) cingulate, caudate, putamen, amygdala, substantia nigra and locus coeruleus (p < 0.01) pAD cases had lower α-syn loads compared to cDLB in the caudate, locus coeruleus (both p < 0.05), cingulate, putamen, amygdala and substantia nigra (all p < 0.01). pAD cases had lower α-syn loads compared to pDLB in cingulate, caudate, putamen substantia nigra and locus coeruleus (all p < 0.05). However, α-syn load in the striatum was significantly higher in cPDD than in cAD (p < 0.05). In addition, in cPDD α-syn load was higher in the hippocampus but lower in the substantia nigra compared to cAD and cDLB (p > 0.05; Fig. 6; Table 5).
α-Synuclein (α-syn) loads differ between clinical Alzheimer’s disease (cAD) clinical dementia with Lewy bodies (cDLB) and clinical Parkinson’s disease dementia (cPDD) in the mixed AD/DLB cohort. α-Syn pathologies inclusive of Lewy bodies ((a) LBs—arrow) and Lewy neurites ((a) LNs—arrowhead) were included in the analysis. The area positive for α-syn immunoreactivity is highlighted in red (b). Differences in α-syn loads between the clinical phenotypes are illustrated in frontal cortex (c), temporal cortex (d), parietal cortex (e), occipital cortex (f), cingulate (g), hippocampus (h), striatum (i.e. mean of caudate and putamen values) (i), amygdala (j), substantia nigra (SN) (k) and locus coeruleus (LC) (l). *p < 0.05; scale bar 20 μm, valid for a and b
With regards to cortical and limbic areas, overall differences in α-syn loads between areas were observed (Friedmans p < 0.05). In the cAD cases, α-syn load was highest in the cingulate cortex (mean 1.77 %, SE ±0.65; p < 0.05 vs frontal, parietal and occipital cortices) followed by hippocampus (mean 1.61 %, SE ±0.76; p < 0.05 vs frontal and occipital cortices), temporal (mean 0.9 %, SE ±0.4; p < 0.05 vs parietal and occipital cortices), frontal (mean 0.38 %, SE ±0.18), parietal (mean 0.33 %, SE ±0.16) and occipital cortices (mean 0.02 %, SE ±0.01; Fig. 4c).
cDLB cases showed highest cortico-limbic α-syn loads in the hippocampus (mean 1.81 %, SE ±0.72), followed by cingulate (mean 1.42 %, SE ±0.74), temporal (mean 1.01 %, SE ±0.44), parietal (mean 0.88 %, SE ±0.37), frontal (mean 0.56 %, SE ±0.34) and occipital cortices (mean 0.07 %, SE ±0.03; p < 0.05; Fig. 4c).
Cortico-limbic α-syn loads in cPDD cases were highest in cingulate cortex (mean 2.76 %, SE ±2.15), followed by hippocampus (mean 2.66 %, SE ±0.98), parietal (mean 2.02 % SE ±1.4), temporal (mean 1.28 %, SE ±0.95), occipital (mean 0.52 %, SE ±0.3) and frontal cortices (mean 0.45 %, SE ±0.32; p < 0.05; Fig. 4c).
Like cDLB, pure DLB cases showed highest cortico-limbic α-syn loads in the hippocampus (mean 2.68 %, SE ±0.67), followed by cingulate cortex (mean 2.43 %, SE ±1.67) but in pure DLB these were followed by frontal (mean 0.59 %, SE ±0.55), temporal (mean 0.12 %, SE ±0.03), parietal (mean 0.04 %, SE ±0.02) and occipital cortices (mean 0.01 %, SE ±0.00 %; p < 0.05; Fig. 4c). No significant differences were seen in α-syn loads between pure DLB and cAD, cDLB and cPDD.
APOE genotyping
APOE genotypes and allele frequencies for all cases are shown in Table 6. Two cases in the cAD group were homozygous for ε4, whilst there was one homozygous ε4 case in the cDLB group and none in the cPDD group.
The distribution of APOE allele frequency demonstrated that APOE ε4 allele frequencies were highest in the cDLB group (50 %) followed by the cAD group (43.75 %) and lowest in the cPDD group (33.33 %). Of note, none of the cases in this study had any APOE ε2 alleles.
Discussion
Using quantitative assessment to evaluate cases that neuropathologically fulfilled the criteria for both AD and DLB, we were able to detect significant differences in the amount of pathological protein aggregates between cases that clinically presented as either AD or DLB.
HP-τ load was indeed higher in cAD cases than in cDLB and cPDD cases. Moreover, we observed differences in the distribution of HP-τ load as cAD showed highest burden of HP-τ in the temporal cortex whilst in cDLB and cPDD this was highest in the occipital cortex and hippocampus, respectively. Importantly, no significant differences in HP-τ load were seen between cAD and pure AD and both showed highest HP-τ loads in the temporal cortex. However, although statistically not significant HP-τ loads in hippocampus and cingulate cortex were higher in cAD than in pure AD and this may have been influenced by concomitant α-syn pathology in cAD cases. Similarly, cingulate Aβ loads were higher in cAD than in pure AD, whilst the distribution of neocortical Aβ loads in cAD was identical to the one observed in pure AD (i.e. frontal > parietal > temporal > occipital). These findings suggest that AD pathology was the primary neurodegenerative change in cAD and represented the neuropathological correlate for the clinical AD phenotype in these cases.
On the other hand, cAD cases did show severe Lewy body pathology at postmortem examination, whilst no clinical symptoms suggestive for DLB were observed antemortem; the impact of additional pathologies on the clinical phenotype is indeed of current interest. It has been suggested that concomitant AD pathology in DLB is associated with cognitive decline [35] and concomitant TDP-43 pathology in AD exacerbates features associated with AD, i.e. greater cognitive impairment and medial temporal lobe atrophy [47], but does not associate with behavioural features frequently associated with frontotemporal lobar degeneration or amyotrophic lateral sclerosis [48], diseases in which TDP-43 inclusions are the characteristic pathological hallmark lesion. The latter is similar to our findings in cAD where co-existing Lewy body pathology did not elicit symptoms associated with DLB and PDD (i.e. visual hallucinations and Parkinsonism), whilst the mean age of disease onset in cAD cases was considerably lower (65.75 years) than the mean age of onset in our pure AD cases (74.2 years) and the mean age of AD onset reported by others [51, 82]. Likewise, the mean age of onset in cDLB (68.5 years) and cPDD (66 years) was low given that the mean age of onset in DLB is generally above 70 years [33, 51, 82]. We observed a shorter survival time in the cDLB and cPDD patients compared to cAD patients, which is in agreement with studies comparing patients with AD and DLB alone [15, 31, 72, 75]. Survival times in our entire mixed AD/DLB group were not shorter than what has been reported for AD and DLB and it has been demonstrated that survival times in AD only depend on the age of disease onset, as they progressively shorten with increasing age of onset [16, 30]. However, the rate of cognitive decline in cAD cases was considerably higher (mean: −7.17, SE ±2.8) compared to mean values of −3.5 (SE ±2.8) for AD, −3.4 (SE ±0.7) for DLB and −5.0 (SE ±0.5) for AD with varying degrees of Lewy body pathology which have been reported previously [51]. Therefore, additional Lewy body pathology in our cAD group possibly had an aggravating effect on the rate of cognitive decline.
In cDLB, we found significantly lower hippocampal HP-τ loads compared to cAD and unlike cAD and pure AD, cDLB showed considerably lower HP-τ loads in the hippocampus than in neocortical areas. This could possibly indicate that in cDLB the hippocampus was involved later in the course of disease and the spread of HP-τ may initially not have followed the typical topographical progression as indicated by Braak stages since an increase of limbic HP-τ load with increasing Braak stages has been suggested [55]. Moreover, cDLB cases showed significantly lower HP-τ loads in the locus coeruleus than did cAD cases; the locus coeruleus has been shown to be affected by HP-τ early in the course of AD (i.e. in low Braak stages) [5, 6, 13, 14] and therefore lower HP-τ loads in the locus coeruleus further suggest that in cDLB the topographical spread of HP-τ might not have followed the typical AD pattern and that AD pathology emerged later in the disease.
Aβ loads were similar in cAD and cDLB but in the majority of areas cDLB showed higher Aβ loads than cPDD, confirming previous postmortem studies [34, 41] demonstrating that DLB patients had higher striatal Aβ loads compared to PDD patients. This finding has been supported by imaging studies using Pittsburgh compound B (PiB) to image β amyloid where DLB patients exhibited higher neocortical, cingulate and striatal Aβ loads compared to PDD [25]. In addition, in our study cPDD cases showed lower HP-τ loads than cDLB in all neocortical areas as well as in cingulate and striatum, further suggesting that the amount of AD pathology is generally lower in clinical PDD than in DLB even in PDD cases that neuropathologically fulfil the criteria for AD.
α-Syn loads were highest in the amygdala and this is not surprising; moderate to severe α-syn pathology in the amygdala is frequently present in both AD and LBD as well as in non-demented controls [29, 52, 80]. Interestingly, except for the striatum where cPDD cases did show significantly higher α-syn loads than cAD cases, no significant respective differences were seen between cAD, cDLB and cPDD. Although not statistically significant, the latter group did indeed show less α-syn pathology in the substantia nigra than did cAD and cDLB. This somewhat unexpected finding might be explained by severe loss of pigmented neurons in cPDD early in the disease, resulting in less Lewy bodies, which might contribute to an overall reduction in nigral α-syn burden. When comparing α-syn loads between mixed AD/DLB cases with pure DLB cases, we found mixed AD/DLB cases to have considerably higher α-syn loads in the temporal cortex, whilst no overt differences were seen in other areas. The temporal cortex in mixed AD/DLB cases did also show highest HP-τ loads and hence HP-τ might have promoted the aggregation and accumulation of α-syn. The notion of such an interaction between HP-τ and α-syn has indeed been supported by data from transgenic animal studies [19] and human postmortem studies found co-localisation of HP-τ and α-syn [21, 38].
The APOE ε4 allele is the strongest genetic risk factor for the development of AD [56, 61, 74]. Up to 65 % of all pathologically confirmed AD cases carry at least one ε4 allele and 12–15 % are homozygous for ε4 compared to 1–3 % of healthy individuals [10, 27]. APOE ε4 has also been suggested as a risk factor for DLB [9, 79] but there is a relative lack of ε4 homozygotes in DLB compared to AD [72]. In a large clinical cohort (n = 1318), Berge and colleagues recently reported a lower APOE ε4 allele frequency in DLB (32 %) than in AD (43 %) [9]. By contrast in cases which show both AD and Lewy body pathology, APOE ε4 allele frequencies of up to 47 % have been reported [79] and the high APOE ε4 allele frequencies of 44.4 % in our mixed AD/DLB cases could at least partly explain the presence of AD pathology. Of note, none of our mixed AD/DLB cases had an APOE ε2 allele.
In conclusion, in cases that by semi-quantitative assessment showed severe degrees of both AD and Lewy body pathology and thus were neuropathologically diagnosed as mixed AD/DLB quantitative assessment revealed differences in the amount of pathological protein aggregates between different clinical phenotypes, in particular significantly higher HP-τ loads in cases with a clinical AD phenotype. Hence, our findings emphasise the important role of quantitative assessment in clinicopathological correlative studies as it is becoming increasingly clear that multiple pathological lesions frequently co-exist the brains of the ageing population [7, 8, 37, 42, 49, 50, 69, 73]. However, quantitative studies on larger cohorts are warranted to further elucidate the relative contribution of underlying neuropathological changes towards the clinical picture.
References
Alafuzoff I, Arzberger T, Al-Sarraj S, Bodi I, Bogdanovic N, Braak H, Bugiani O, Del-Tredici K, Ferrer I, Gelpi E, Giaccone G, Graeber MB, Ince P, Kamphorst W, King A, Korkolopoulou P, Kovacs GG, Larionov S, Meyronet D, Monoranu C, Parchi P, Patsouris E, Roggendorf W, Seilhean D, Tagliavini F, Stadelmann C, Streichenberger N, Thal DR, Wharton SB, Kretzschmar H (2008) Staging of neurofibrillary pathology in Alzheimer’s disease: a study of the BrainNet Europe Consortium. Brain Pathol 18:484–496
Alafuzoff I, Ince PG, Arzberger T, Al-Sarraj S, Bell J, Bodi I, Bogdanovic N, Bugiani O, Ferrer I, Gelpi E, Gentleman S, Giaccone G, Ironside JW, Kavantzas N, King A, Korkolopoulou P, Kovacs GG, Meyronet D, Monoranu C, Parchi P, Parkkinen L, Patsouris E, Roggendorf W, Rozemuller A, Stadelmann-Nessler C, Streichenberger N, Thal DR, Kretzschmar H (2009) Staging/typing of Lewy body related alpha-synuclein pathology: a study of the BrainNet Europe Consortium. Acta Neuropathol 117:635–652
Alafuzoff I, Thal DR, Arzberger T, Bogdanovic N, Al-Sarraj S, Bodi I, Boluda S, Bugiani O, Duyckaerts C, Gelpi E, Gentleman S, Giaccone G, Graeber M, Hortobagyi T, Hoftberger R, Ince P, Ironside JW, Kavantzas N, King A, Korkolopoulou P, Kovacs GG, Meyronet D, Monoranu C, Nilsson T, Parchi P, Patsouris E, Pikkarainen M, Revesz T, Rozemuller A, Seilhean D, Schulz-Schaeffer W, Streichenberger N, Wharton SB, Kretzschmar H (2009) Assessment of beta-amyloid deposits in human brain: a study of the BrainNet Europe Consortium. Acta Neuropathol 117:309–320
Armstrong RA, Lantos PL, Cairns NJ (2005) Overlap between neurodegenerative disorders. Neuropathology 25:111–124
Attems J, Thal DR, Jellinger KA (2012) The relationship between subcortical tau pathology and Alzheimer’s disease. Biochem Soc Trans 40:711–715
Attems J, Thomas A, Jellinger K (2012) Correlations between cortical and subcortical tau pathology. Neuropathol Appl Neurobiol 38:582–590
Attems J, Jellinger K (2013) Neuropathological correlates of cerebral multimorbidity. Curr Alzheimer Res 10:569–577
Attems J, Neltner JH, Nelson PT (2014) Quantitative neuropathological assessment to investigate cerebral multi-morbidity. Alzheimers Res Ther 6:85
Berge G, Sando SB, Rongve A, Aarsland D, White LR (2014) Apolipoprotein E ε2 genotype delays onset of dementia with Lewy bodies in a Norwegian cohort. J Neurol Neurosurg Psychiatry 85:1227–1231
Blacker D, Tanzi RE (1998) The genetics of Alzheimer disease: current status and future prospects. Arch Neurol 55:294–296
Braak H, Del Tredici K, Rub U, de Vos RA, Jansen Steur EN, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211
Braak H, Alafuzoff I, Arzberger T, Kretzschmar H, Del Tredici K (2006) Staging of Alzheimer disease-associated neurofibrillary pathology using paraffin sections and immunocytochemistry. Acta Neuropathol 112:389–404
Braak H, Del Tredici K (2011) The pathological process underlying Alzheimer’s disease in individuals under thirty. Acta Neuropathol 121:171–181
Braak H, Thal DR, Ghebremedhin E, Del Tredici K (2011) Stages of the pathologic process in Alzheimer disease: age categories from 1 to 100 years. J Neuropathol Exp Neurol 70:960–969
Brodaty H, Seeher K, Gibson L (2012) Dementia time to death: a systematic literature review on survival time and years of life lost in people with dementia. Int Psychogeriatr 24:1034–1045
Brookmeyer R, Corrada MM, Curriero FC, Kawas C (2002) Survival following a diagnosis of Alzheimer disease. Arch Neurol 59:1764–1767
Calderon J, Perry RJ, Erzinclioglu SW, Berrios GE, Dening TR, Hodges JR (2001) Perception, attention, and working memory are disproportionately impaired in dementia with Lewy bodies compared with Alzheimer’s disease. J Neurol Neurosurg Psychiatry 70:157–164
Calero O, Hortiguela R, Bullido MJ, Calero M (2009) Apolipoprotein E genotyping method by real time PCR, a fast and cost-effective alternative to the TaqMan and FRET assays. J Neurosci Methods 183:238–240
Clinton LK, Blurton-Jones M, Myczek K, Trojanowski JQ, LaFerla FM (2010) Synergistic Interactions between Abeta, tau, and alpha-synuclein: acceleration of neuropathology and cognitive decline. J Neurosci 30:7281–7289
Collette F, Van der Linden M, Salmon E (1999) Executive dysfunction in Alzheimer’s disease. Cortex 35:57–72
Colom-Cadena M, Gelpi E, Charif S, Belbin O, Blesa R, Marti MJ, Clarimon J, Lleo A (2013) Confluence of alpha-synuclein, tau, and beta-amyloid pathologies in dementia with Lewy bodies. J Neuropathol Exp Neurol 72:1203–1212
Cummings JL, Benson F, Hill MA, Read S (1985) Aphasia in dementia of the Alzheimer type. Neurology 35:394–397
Dubois B, Feldman HH, Jacova C, Cummings JL, Dekosky ST, Barberger-Gateau P, Delacourte A, Frisoni G, Fox NC, Galasko D, Gauthier S, Hampel H, Jicha GA, Meguro K, O’Brien J, Pasquier F, Robert P, Rossor M, Salloway S, Sarazin M, de Souza LC, Stern Y, Visser PJ, Scheltens P (2010) Revising the definition of Alzheimer’s disease: a new lexicon. Lancet Neurol 9:1118–1127
Duyckaerts C, Delatour B, Potier MC (2009) Classification and basic pathology of Alzheimer disease. Acta Neuropathol 118:5–36
Edison P, Rowe CC, Rinne JO, Ng S, Ahmed I, Kemppainen N, Villemagne VL, O’Keefe G, Nagren K, Chaudhury KR, Masters CL, Brooks DJ (2008) Amyloid load in Parkinson’s disease dementia and Lewy body dementia measured with [11C]PIB positron emission tomography. J Neurol Neurosurg Psychiatry 79:1331–1338
Emre M, Aarsland D, Brown R, Burn DJ, Duyckaerts C, Mizuno Y, Broe GA, Cummings J, Dickson DW, Gauthier S, Goldman J, Goetz C, Korczyn A, Lees A, Levy R, Litvan I, McKeith I, Olanow W, Poewe W, Quinn N, Sampaio C, Tolosa E, Dubois B (2007) Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov Disord 22:1689–1707 (quiz 1837)
Farrer LA, Cupples LA, Haines JL, Hyman B, Kukull WA, Mayeux R, Myers RH, Pericak-Vance MA, Risch N, van Duijn CM (1997) Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease: a meta-analysis, APOE and Alzheimer Disease Meta Analysis Consortium. JAMA 278:1349–1356
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Fujishiro H, Ahn TB, Frigerio R, Delle Donne A, Josephs KA, Parisi JE, Eric Ahlskog J, Dickson DW (2008) Glial cytoplasmic inclusions in neurologically normal elderly: prodromal multiple system atrophy? Acta Neuropathol 116:269–275
Ganguli M, Dodge HH, Shen C, Pandav RS, DeKosky ST (2005) Alzheimer disease and mortality: a 15-year epidemiological study. Arch Neurol 62:779–784
Garcia-Ptacek S, Farahmand B, Kareholt I, Religa D, Cuadrado ML, Eriksdotter M (2014) Mortality risk after dementia diagnosis by dementia type and underlying factors: a cohort of 15,209 patients based on the Swedish Dementia Registry. J Alzheimers Dis 41:467–477
Gentleman SM, Allsop D, Bruton CJ, Jagoe R, Polak JM, Roberts GW (1992) Quantitative differences in the deposition of beta A4 protein in the sulci and gyri of frontal and temporal isocortex in Alzheimer’s disease. Neurosci Lett 136:27–30
Gill DP, Hubbard RA, Koepsell TD, Borrie MJ, Petrella RJ, Knopman DS, Kukull WA (2013) Differences in rate of functional decline across three dementia types. Alzheimers Dement 9:S63–71
Halliday GM, Song YJ, Harding AJ (2011) Striatal beta-amyloid in dementia with Lewy bodies but not Parkinson’s disease. J Neural Transm 118:713–719
Howlett DR, Whitfield D, Johnson M, Attems J, O’Brien JT, Aarsland D, Lai MK, Lee JH, Chen C, Ballard C, Hortobagyi T, Francis PT (2014) Regional Multiple Pathology Scores are associated with cognitive decline in Lewy body dementias. Brain Pathol (Epub ahead of print)
Hyman BT, Phelps CH, Beach TG, Bigio EH, Cairns NJ, Carrillo MC, Dickson DW, Duyckaerts C, Frosch MP, Masliah E, Mirra SS, Nelson PT, Schneider JA, Thal DR, Thies B, Trojanowski JQ, Vinters HV, Montine TJ (2012) National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease. Alzheimers Dement 8:1–13
Ince PG (2001) Pathological correlates of late-onset dementia in a multicentre, community-based population in England and Wales. Neuropathology Group of the Medical Research Council Cognitive Function and Ageing Study (MRC CFAS). Lancet 357:169–175
Ishizawa T, Mattila P, Davies P, Wang D, Dickson DW (2003) Colocalization of tau and alpha-synuclein epitopes in Lewy bodies. J Neuropathol Exp Neurol 62:389–397
Jack CR Jr, Albert MS, Knopman DS, McKhann GM, Sperling RA, Carrillo MC, Thies B, Phelps CH (2011) Introduction to the recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7:257–262
Jellinger KA, Attems J (2003) Incidence of cerebrovascular lesions in Alzheimer’s disease: a postmortem study. Acta Neuropathol 105:14–17
Jellinger KA, Attems J (2006) Does striatal pathology distinguish Parkinson disease with dementia and dementia with Lewy bodies? Acta Neuropathol 112:253–260
Jellinger KA (2007) The enigma of mixed dementia. Alzheimers Dement 3:40–53
Jellinger KA (2007) The enigma of vascular cognitive disorder and vascular dementia. Acta Neuropathol 113:349–388
Jellinger KA, Attems J (2007) Neuropathological evaluation of mixed dementia. J Neurol Sci 257:80–87
Jellinger KA, Attems J (2010) Prevalence of dementia disorders in the oldest-old: an autopsy study. Acta Neuropathol 119:421–433
Jellinger KA, Attems J (2014) Challenges of multimorbidity of the aging brain: a critical update. J Neural Transm (Epub ahead of print)
Josephs KA, Whitwell JL, Weigand SD, Murray ME, Tosakulwong N, Liesinger AM, Petrucelli L, Senjem ML, Knopman DS, Boeve BF, Ivnik RJ, Smith GE, Jack CR Jr, Parisi JE, Petersen RC, Dickson DW (2014) TDP-43 is a key player in the clinical features associated with Alzheimer’s disease. Acta Neuropathol 127:811–824
Jung Y, Dickson DW, Murray ME, Whitwell JL, Knopman DS, Boeve BF, Jack CR Jr, Parisi JE, Petersen RC, Josephs KA (2014) TDP-43 in Alzheimer’s disease is not associated with clinical FTLD or Parkinsonism. J Neurol 261:1344–1348
Kovacs GG, Alafuzoff I, Al-Sarraj S, Arzberger T, Bogdanovic N, Capellari S, Ferrer I, Gelpi E, Kovari V, Kretzschmar H, Nagy Z, Parchi P, Seilhean D, Soininen H, Troakes C, Budka H (2008) Mixed brain pathologies in dementia: the BrainNet Europe Consortium Experience. Dement Geriatr Cogn Disord 26:343–350
Kovacs GG, Milenkovic I, Wohrer A, Hoftberger R, Gelpi E, Haberler C, Honigschnabl S, Reiner-Concin A, Heinzl H, Jungwirth S, Krampla W, Fischer P, Budka H (2013) Non-Alzheimer neurodegenerative pathologies and their combinations are more frequent than commonly believed in the elderly brain: a community-based autopsy series. Acta Neuropathol 126:365–384
Kraybill ML, Larson EB, Tsuang DW, Teri L, McCormick WC, Bowen JD, Kukull WA, Leverenz JB, Cherrier MM (2005) Cognitive differences in dementia patients with autopsy-verified AD, Lewy body pathology, or both. Neurology 64:2069–2073
Leverenz JB, Hamilton R, Tsuang DW, Schantz A, Vavrek D, Larson EB, Kukull WA, Lopez O, Galasko D, Masliah E, Kaye J, Woltjer R, Clark C, Trojanowski JQ, Montine TJ (2008) Empiric refinement of the pathologic assessment of Lewy-related pathology in the dementia patient. Brain Pathol 18:220–224
Lewy FH (1912) Paralysis Agitans Pathologische Anatomie. In: Lewandowski M (ed) Handbuch der Neurologie. Springer, Berlin, pp 920–933
Lippa CF, Duda JE, Grossman M, Hurtig HI, Aarsland D, Boeve BF, Brooks DJ, Dickson DW, Dubois B, Emre M, Fahn S, Farmer JM, Galasko D, Galvin JE, Goetz CG, Growdon JH, Gwinn-Hardy KA, Hardy J, Heutink P, Iwatsubo T, Kosaka K, Lee VM, Leverenz JB, Masliah E, McKeith IG, Nussbaum RL, Olanow CW, Ravina BM, Singleton AB, Tanner CM, Trojanowski JQ, Wszolek ZK (2007) DLB and PDD boundary issues: diagnosis, treatment, molecular pathology, and biomarkers. Neurology 68:812–819
Mandler M, Walker L, Santic R, Hanson P, Upadhaya AR, Colloby SJ, Morris CM, Thal DR, Thomas AJ, Schneeberger A, Attems J (2014) Pyroglutamylated amyloid-beta is associated with hyperphosphorylated tau and severity of Alzheimer’s disease. Acta Neuropathol 128:67–79
Mayeux R, Saunders AM, Shea S, Mirra S, Evans D, Roses AD, Hyman BT, Crain B, Tang MX, Phelps CH (1998) Utility of the apolipoprotein E genotype in the diagnosis of Alzheimer’s disease: Alzheimer’s Disease Centers Consortium on Apolipoprotein E and Alzheimer’s Disease. N Engl J Med 338:506–511
McKeith IG, Galasko D, Kosaka K, Perry EK, Dickson DW, Hansen LA, Salmon DP, Lowe J, Mirra SS, Byrne EJ, Lennox G, Quinn NP, Edwardson JA, Ince PG, Bergeron C, Burns A, Miller BL, Lovestone S, Collerton D, Jansen EN, Ballard C, de Vos RA, Wilcock GK, Jellinger KA, Perry RH (1996) Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the consortium on DLB international workshop. Neurology 47:1113–1124
McKeith IG, Dickson DW, Lowe J, Emre M, O’Brien JT, Feldman H, Cummings J, Duda JE, Lippa C, Perry EK, Aarsland D, Arai H, Ballard CG, Boeve B, Burn DJ, Costa D, Del Ser T, Dubois B, Galasko D, Gauthier S, Goetz CG, Gomez-Tortosa E, Halliday G, Hansen LA, Hardy J, Iwatsubo T, Kalaria RN, Kaufer D, Kenny RA, Korczyn A, Kosaka K, Lee VM, Lees A, Litvan I, Londos E, Lopez OL, Minoshima S, Mizuno Y, Molina JA, Mukaetova-Ladinska EB, Pasquier F, Perry RH, Schulz JB, Trojanowski JQ, Yamada M (2005) Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology 65:1863–1872
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM (1984) Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA work group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s disease. Neurology 34:939–944
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, Mohs RC, Morris JC, Rossor MN, Scheltens P, Carrillo MC, Thies B, Weintraub S, Phelps CH (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging–Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7:263–269
Meyer MR, Tschanz JT, Norton MC, Welsh-Bohmer KA, Steffens DC, Wyse BW, Breitner JC (1998) APOE genotype predicts when–not whether–one is predisposed to develop Alzheimer disease. Nat Genet 19:321–322
Mirra SS, Heyman A, McKeel D, Sumi SM, Crain BJ, Brownlee LM, Vogel FS, Hughes JP, van Belle G, Berg L (1991) The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). part II: standardization of the neuropathologic assessment of Alzheimer’s disease. Neurology 41:479–486
Montine T, Phelps C, Beach T, Bigio E, Cairns N, Dickson D, Duyckaerts C, Frosch M, Masliah E, Mirra S, Nelson P, Schneider J, Thal D, Trojanowski J, Vinters H, Hyman B (2012) National Institute on Aging–Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease a practical approach. Acta Neuropathologica pp 1-11
Olichney JM, Hansen LA, Hofstetter CR, Grundman M, Katzman R, Thal LJ (1995) Cerebral infarction in Alzheimer’s disease is associated with severe amyloid angiopathy and hypertension. Arch Neurol 52:702–708
Olichney JM, Galasko D, Salmon DP, Hofstetter CR, Hansen LA, Katzman R, Thal LJ (1998) Cognitive decline is faster in Lewy body variant than in Alzheimer’s disease. Neurology 51:351–357
Pollanen MS, Dickson DW, Bergeron C (1993) Pathology and biology of the Lewy body. J Neuropathol Exp Neurol 52:183–191
Rahimi J, Kovacs GG (2014) Prevalence of mixed pathologies in the aging brain. Alzheimers Res Ther 6:82
Savica R, Grossardt BR, Bower JH, Boeve BF, Ahlskog JE, Rocca WA (2013) Incidence of dementia with Lewy bodies and Parkinson disease dementia. JAMA Neurol 70:1396–1402
Schneider JA, Arvanitakis Z, Bang W, Bennett DA (2007) Mixed brain pathologies account for most dementia cases in community-dwelling older persons. Neurology 69:2197–2204
Schneider JA, Bennett DA (2010) Where vascular meets neurodegenerative disease. Stroke 41:S144–146
Serby M, Brickman AM, Haroutunian V, Purohit DP, Marin D, Lantz M, Mohs RC, Davis KL (2003) Cognitive burden and excess Lewy-body pathology in the Lewy-body variant of Alzheimer disease. Am J Geriatr Psychiatry 11:371–374
Singleton AB, Wharton A, O’Brien KK, Walker MP, McKeith IG, Ballard CG, O’Brien J, Perry RH, Ince PG, Edwardson JA, Morris CM (2002) Clinical and neuropathological correlates of apolipoprotein E genotype in dementia with Lewy bodies. Dement Geriatr Cogn Disord 14:167–175
Sonnen JA, Postupna N, Larson EB, Crane PK, Rose SE, Montine KS, Leverenz JB, Montine TJ (2010) Pathologic correlates of dementia in individuals with Lewy body disease. Brain Pathol 20:654–659
Strittmatter WJ, Saunders AM, Schmechel D, Pericak-Vance M, Enghild J, Salvesen GS, Roses AD (1993) Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. Proc Natl Acad Sci USA 90:1977–1981
Stubendorff K, Hansson O, Minthon L, Londos E (2011) Differences in survival between patients with dementia with Lewy bodies and patients with Alzheimer’s disease: measured from a fixed cognitive level. Dement Geriatr Cogn Disord 32:408–416
Thal DR, Ghebremedhin E, Rub U, Yamaguchi H, Del Tredici K, Braak H (2002) Two types of sporadic cerebral amyloid angiopathy. J Neuropathol Exp Neurol 61:282–293
Thal DR, Rub U, Orantes M, Braak H (2002) Phases of A beta-deposition in the human brain and its relevance for the development of AD. Neurology 58:1791–1800
Tiraboschi P, Salmon DP, Hansen LA, Hofstetter RC, Thal LJ, Corey-Bloom J (2006) What best differentiates Lewy body from Alzheimer’s disease in early-stage dementia? Brain 129:729–735
Tsuang DW, Wilson RK, Lopez OL, Luedecking-Zimmer EK, Leverenz JB, DeKosky ST, Kamboh MI, Hamilton RL (2005) Genetic association between the APOE*4 allele and Lewy bodies in Alzheimer disease. Neurology 64:509–513
Uchikado H, Lin WL, DeLucia MW, Dickson DW (2006) Alzheimer disease with amygdala Lewy bodies: a distinct form of alpha-synucleinopathy. J Neuropathol Exp Neurol 65:685–697
Whitfield DR, Vallortigara J, Alghamdi A, Howlett D, Hortobagyi T, Johnson M, Attems J, Newhouse S, Ballard C, Thomas AJ, O’Brien JT, Aarsland D, Francis PT (2014) Assessment of ZnT3 and PSD95 protein levels in Lewy body dementias and Alzheimer’s disease: association with cognitive impairment. Neurobiol Aging 35:2836–2844
Williams MM, Xiong C, Morris JC, Galvin JE (2006) Survival and mortality differences between dementia with Lewy bodies vs Alzheimer disease. Neurology 67:1935–1941
Acknowledgments
We are very grateful to the individuals who kindly donated their brains to the Newcastle Brain Tissue Resource. We thank Mrs Lynne Ramsay, Mrs Ros Hall and Mrs Claire Kolenda for excellent technical assistance. The research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre for Ageing and Age-related disease and the Biomedical Research Unit for Lewy body dementia based at Newcastle upon Tyne Hospitals NHS Foundation Trust and Newcastle University (R:CH/ML/0712), the views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. Tissue for this study was provided by the Newcastle Brain Tissue Resource, which is funded in part by a grant from the UK Medical Research Council (G0400074) and by Brains for Dementia research, a joint venture between Alzheimer’s Society and Alzheimer’s Research UK.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walker, L., McAleese, K.E., Thomas, A.J. et al. Neuropathologically mixed Alzheimer’s and Lewy body disease: burden of pathological protein aggregates differs between clinical phenotypes. Acta Neuropathol 129, 729–748 (2015). https://doi.org/10.1007/s00401-015-1406-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-015-1406-3