Abstract
Cyclic GMP-dependent protein kinase (PKG) is a serine-threonine kinase that mediates the cardioprotective effect of ischemic and pharmacologic preconditioning. Since hydrogen sulfide (H2S) has been implicated in mediating the cardioprotective effects of the cGMP modulators tadalafil and cinaciguat, we tested the hypothesis that myocardial gene therapy with PKG exerts cardioprotection against ischemia/reperfusion (I/R) injury through a mechanism involving H2S. Adult rat cardiomyocytes were infected with adenoviral vector encoding PKGIα or inactive mutant PKGIαK390A (K390A) for 24 h. Necrosis and apoptosis (n = 6/group) were determined after 90 min of simulated ischemia and 1 or 18 h of reoxygenation, respectively. To study the effect of PKGIα in vivo, mice received intramyocardial injections of adenoviral PKGIα or K390A. Four days later, the hearts were subjected to 30 min of ischemia followed by reperfusion for 24 h. The inhibitor of H2S-producing enzyme, cystathionine-γ-lyase (CSE), dl-propargylglycine (PAG, 50 mg/kg, ip) was given 30 min before ischemia. PKGIα overexpression induced CSE expression, whereas cystathionine-β-synthase (CBS) and 3-mercaptopyruvate sulfurtransferase expression was not changed. PKGIα overexpression increased H2S in the heart and cardiomyocytes in relation to control and PKGIαK390A. Moreover, PAG abolished protection with PKGIα in vitro by increasing necrosis (35.2 ± 1.7 %, P < 0.05) and apoptosis (23.5 ± 1.8 %, P < 0.05) as compared to PKGIα-overexpressing cells (necrosis: 17.2 ± 0.9 % and apoptosis: 13.2 ± 0.8 %). In vivo, PKGIα overexpression reduced infarct size and preserved left ventricular fractional shortening as compared with K390A (P < 0.05) and PAG abolished the cardioprotective effect of PKGIα. The protective effect of myocardial gene therapy with PKGIα against I/R injury is mediated through a mechanism involving H2S signaling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cyclic GMP-dependent protein kinase (PKG)Iα and PKGIß are major mediators of cGMP signaling in the cardiovascular system. Two PKG genes have been identified in mammalian cells encoding for PKG type I (including α- and ß- splice variants) and PKG type II [18]. In particular, the PKGIα isozyme is mainly found in lung, heart, platelets, and cerebellum while the Iβ form is highly expressed with Iα in smooth muscle, including uterus, vessels, intestine, and trachea [22, 25]. Several cardioprotective strategies including ischemic preconditioning, nitric oxide (NO), and ANP/BNP have been shown to ischemia/reperfusion (I/R) injury through PKG [28, 30, 37]. In addition, the importance of restoring PKG signaling with selective phosphodiesterase-5 (PDE5) inhibitors [9, 12, 29, 30, 47] has been shown to be protective against several pathologies [23, 34]. At the cellular level, PKGIα overexpression in isolated primary cardiomyocytes protected against cell death caused by simulated ischemia and reoxygenation (SI/RO) [14]. PKGIα overexpression triggered a number of signaling events, which involved the opening of mitochondrial KATP channels, phosphorylation of Akt, MAPKs including ERK and JNK, increased the expression of nitric oxide synthase (NOS) and Bcl-2 leading to reduction in necrosis and apoptosis in cardiomyocytes. However, considering the diverse population of cells in the heart, it is not known whether in vivo gene transfer of PKGIα would also salvage the intact myocardium following I/R injury.
A number of recent studies have shown that H2S protects the heart through anti-apoptotic, anti-inflammatory, antioxidant, and mitochondrial actions of H2S [35, 39]. H2S is one of the gasotransmitters (similar to NO and CO), which is produced enzymatically in the cardiovascular system. Cystathionine-β-synthase (CBS), cystathionine-γ-lyase (CSE), and 3-mercaptopyruvate sulfurtransferase (3-MST) are the key enzymes responsible for the endogenous production of H2S in mammalian cells and tissues. Both CBS and CSE enzymes are pyridoxal-5-phosphate-dependent and use l-cysteine as the main substrate [36]. Although other enzymes can catalyze the production of H2S [17], CBS seems to be the main H2S-forming enzyme in the central nervous system, whereas CSE is important for H2S generation in the cardiovascular system including the heart [19]. We demonstrated that protection against myocardial I/R injury with the long-acting PDE5 inhibitor, tadalafil, was dependent upon PKG [41]. In these studies, the protective effect of tadalafil was abolished by treatment with a CSE inhibitor, dl-propargylglycine (PAG), as well as in CSE-knockout mice, suggesting a definite role of endogenous H2S in cardioprotection. Similarly, reduction of infarct size following treatment with NO-independent soluble guanylate cyclase (sGC) activator, Cinaciguat, was associated with increased expression of CSE and augmented levels of H2S in the heart [42]. These studies provided evidence that cGMP-generating drugs with consequent activation of PKG produced therapeutic levels of H2S. Nevertheless, considering the confounding or potentially off-target and non-specific effects of pharmacological generators of cGMP, it is critical to further evaluate the direct role of PKG in H2S generation and demonstrate its protective effects against I/R injury in vivo. Therefore, the first goal of the current investigation was to show whether myocardial gene therapy with PKGIα overexpression reduces infarct size and improves cardiac function following I/R injury. A second goal was to examine whether H2S is one of the critical gasotransmitters involved in reducing cardiomyocyte death in vitro and myocardial injury in vivo following PKGIα overexpression. Our results provide evidence that overexpression of PKGIα protects against I/R injury through CSE-dependent generation of H2S in the heart as well as adult cardiomyocytes.
Materials and methods
Animals
Adult male out-bred CD-1 mice were purchased from Charles River Laboratories International, Inc. (Wilmington, MA); the body weight ranged from 30 to 34 g. Adult male Wistar rats (300 g) were purchased from Harlan Sprague–Dawley, Inc. (Indianapolis, IN). All animal experiments were conducted under the guidelines on humane use and care of laboratory animals for biomedical research published by National Institutes of Health (No. 85-23, revised 1996).
Drugs and chemicals
Triphenyltetrazolium chloride (TTC) and dl-propargylglycine (PAG) were purchased from Sigma-Aldrich (St. Louis, MO). PKG and CSE antibodies were purchased from Santa Cruz. KT5823 (Cat # 420321) was purchased from Calbiochem (La Jolla, CA). Adenoviral vectors to overexpress PKG were obtained from Dr. Suzanne M. Lohmann (Institut für Klinische Biochemie und Pathobiochemie, Medizinische Universitätsklinik, Würzburg, Germany), which were amplified and maintained in our laboratory.
Adult primary cardiomyocyte preparation and overexpression of PKG-Iα protocol
Ventricular cardiomyocytes were isolated using an enzymatic technique as previously reported [14]. The freshly isolated cardiomyocytes were plated with Medium 199 containing 2 mM L-carnitine, 5 mM creatine, 5 mM taurine, 5 mM glucose, 0.1 μM insulin, and 1 % penicillin–streptomycin. After 1 h of plating, the myocytes were infected with adenoviral vectors containing hPKGIα (PKGIα) or catalytically inactive hPKGIαK390A (K390A) [14] in serum-free growth medium for 24 h. In this study, we chose adult rat primary cardiomyocytes because the stability of these cells is superior to primary mouse cardiomyocytes especially with the use of adenoviral vectors to overexpress PKGIα.
Simulated ischemia/reoxygenation protocol
After 24 h of adenoviral infection, the cells were subjected to simulated ischemia (SI) for 90 min by replacing the cell medium with an “ischemia buffer” that contained 118 mM NaCl, 24 mM NaHCO3, 1.0 mM NaH2PO4, 2.5 mM CaCl2-2H2O, 1.2 mM MgCl2, 20 mM sodium lactate, 16 mM KCl, and 10 mM 2-deoxyglucose (pH adjusted to 6.2) as reported previously [15]. The cells were incubated at 37 °C in tri-gas incubator adjusting 1–2 % O2 (monitored by the incubator sensors) and 5 % CO2 during the entire SI period. Reoxygenation (RO) was accomplished by replacing the ischemic buffer with normal cell medium under normoxic conditions. Cell necrosis and apoptosis were assessed after 1 or 18 h of RO, respectively.
Experimental groups (in vitro)
Five groups of adult primary rat cardiomyocytes were used. Cardiomyocytes isolated from 6 rat hearts were used to conduct our experiments. Then, cardiomyocytes isolated from each heart were plated in 4 wells/group for each experiment. 1- Control cardiomyocytes were prepared and 24 h later, they were subjected to SI/RO; 2- PKGIα cardiomyocytes were infected with Ad.PKGIα (1 × 105 pfu) 24 h prior to SI/RO; 3- PKGIα + PAG cardiomyocytes were infected with Ad.PKGIα 24 h prior to incubation with PAG (2 mmol/L) for 30 min before SI/RO; 4- PKGIαK390A: Cardiomyocytes were infected with catalytically inactive PKGIα (1 × 105 pfu), as control for group 2, 24 h prior to SI/RO; 5- PAG: Cardiomyocytes were prepared as in Group 1 and incubated with PAG as in Group 3 followed by SI/RO.
Assessment of necrosis and apoptosis
Trypan blue exclusion assay and lactate dehydrogenase (LDH) release into the medium were used to assess cell necrosis [15]. Cardiomyocyte apoptosis was analyzed by TUNEL staining as reported previously [15].
Myocardial overexpression of PKG-Iα
Mice were anesthetized with the injection of pentobarbital (70 mg/kg ip), intubated orotracheally and ventilated on a positive-pressure ventilator. The tidal volume was set at 0.2 ml, and the respiratory rate was adjusted to 133 cycles/min. A left thoracotomy was performed at the fourth intercostal space, and the heart was exposed by stripping the pericardium. After the heart was exposed, 1.5 × 109 pfu in 30 μl total (3 injections of 10 μl at different locations) were administered intramyocardially in the LV wall adjacent to the LAD in the prospective area at risk for experimental ischemia.
Real-time PCR
Ninety-six hours after intramyocardial injection of adenoviral vectors encoding PKG-Iα or its inactive mutant, the transcript levels of PKG were quantified by real-time PCR performed in the ABI prism 7900HT sequence detector system (Applied Biosystems, Foster City, CA) using the TaqMan® One Step PCR Master reagent kit (product number 4309169). All of the samples were processed in triplicates according to the manufacturers' recommended conditions. The cycling conditions were as follows: 48 °C for 30 min, 95 °C for 10 min, 40 cycles of 95 °C for 15 s and 60 °C for 1 min. The cycle threshold was determined to provide the optimal standard curve values (0.98–1.0). The primers used for PKG were as follows: forward, 5′-TGGTCACTAGGAATTCTGATGTATGAG-3′ and reverse, 5′-TGATATTGTAGGTTTTCATTGGATCTG-3′ and the TaqMan probe was as follows: 5′-TCTGACTGGCAGCCCACCTTTCTCA-3′. The probes and primers were designed using the Primer Express® 2.0 version and synthesized in the Nucleic Acid Research Facilities of Virginia Commonwealth University. The probes were labeled in the 5′ end with FAM (6-carboxyfluorescein) and in the 3′ end with TAMRA (6-carboxytetramethylrhodamine). Ribosomal RNA (18S rRNA) from the predeveloped TaqMan Assay Reagents (product number 4310893E) was used as an endogenous control.
Western blot analysis
Total soluble protein was extracted from the whole heart tissue with RIPA buffer. The homogenate was centrifuged at 14,000×g for 15 min under 4 °C and the supernatant was recovered. 50 μg of protein from each sample was separated by SDS-PAGE and transferred onto nitrocellulose membrane [16]. The membrane was incubated with primary antibody for each of the respective proteins, i.e., PKG and actin, GAPDH (goat polyclonal, 1:1000 dilution), CSE, CBS, and 3-MST (mouse monoclonal 1:500 dilution) (Santa Cruz Biotechnology). The membrane was washed and incubated with horseradish peroxidase-conjugated secondary antibody (1:2000 dilution, 1 h at room temperature). The blots were developed using a chemiluminescent system (ECL Plus; Amersham Biosciences). The densitometric analysis for the corresponding PKG, CSE, CBS, 3-MST, actin, and GAPDH bands was done using ImageJ software.
Myocardial infarction protocol
The methodology of myocardial infarction was described previously [40]. In brief, 96 h after intramyocardial injection of PKGIα or K390A viral vectors, the left descending coronary artery was identified and occluded for 30 min by a 7.0 silk ligature that was placed around it and a small piece of polyethylene tubing (PE10) that was positioned on top of it. After coronary artery occlusion for 30 min, reperfusion was established by removing the PE10 tube that was compressing the coronary artery. After reperfusion, the air was expelled from the chest and the animals were extubated and then received analgesia (buprenorphine SR LAB; 0.1 mg/kg; sc, which last for 72 h) and antibiotic (Gentamicin; 0.7 mg/kg; IM).
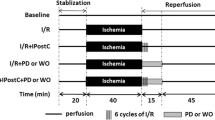
Experimental groups (in vivo)
Eight groups were used. 1- PBS (Control) Each mouse received 30 µl of PBS (3 intramyocardial injections of 10 μl in the prospective area at risk for ischemia) 96 h prior to I/R; 2- PKGIα Mice received intramyocardial injections of Ad.PKGIα (1.5 × 109 pfu; 3 injections of 10 µl in the prospective area at risk for ischemia) 96 h prior to I/R; 3- Ad.PKGIα + PAG Ad.PKGIα was administered as in group 2 and PAG (50 mg/kg, ip) was injected 30 min prior to ischemia; 4- PKGIαK390A Catalytically inactive Ad.PKG-Iα was injected as in group 2; 5- PAG PAG was administered as in group 3; 6- PKGIα + KT5823 Ad.PKGIα was administered as in group 2 and KT5823 (PKG inhibitor, 1 mg/kg, ip) was injected 5 min prior to reperfusion; 7- KT5823 KT5823 (1 mg/kg, ip) was injected 5 min prior to reperfusion. 8- Sham Mice were subjected to a left thoracotomy without coronary artery ligation as a control for the surgical procedure (the animals in this group received no treatment until sampling of the heart). In all groups, infarct size was measured 24 h after I/R. Prior to sacrifice, left ventricular (LV) function was analyzed using echocardiography. Six to eight mice in each group were used for infarct size assessment and for functional analysis using echocardiography. The detailed experimental protocol is shown in Fig. 1. Three additional mice in groups 2 and 4 were used for measurement of myocardial H2S concentration at 96 h after infection and compared to group 8.
Infarct size assessment
As described previously [40], after 24 h of reperfusion, the heart was quickly removed and mounted on a Langendorff apparatus. The coronary arteries were perfused with 0.9 % NaCl containing 2.5 mM CaCl2. After the blood was washed out, ~1 ml of 10 % Phthalo blue dye was injected as a bolus into the aorta until most of the heart turned blue. The heart was perfused with saline to wash out the excess Phthalo blue. Finally, the heart was removed, frozen, and cut into 8–10 transverse slices from apex to base of equal thickness (~1 mm). The slices were then incubated in 10 % TTC in isotonic phosphate buffer (pH 7.4) at room temperature for 30 min. The areas of infarcted tissue, the risk zone, and the whole left ventricle were determined by computer morphometry using a Bioquant imaging software.
Measurement of H2S in cardiomyocytes and heart tissue
Isolated cardiomyocytes were lysed and passaged through a syringe after adding 500 µl of 100 mM potassium phosphate buffer (pH 7.4). For the intact heart, the tissue was homogenized in 1 mL of 100 mM potassium phosphate buffer (pH 7.4). To trap H2S, 250 μL of zinc acetate (1 % wt/vol) was added to the cell or tissue homogenate followed by 30 min incubation at 37 °C. The reaction was stopped by adding 250 μL of trichloroacetic acid (10 % wt/vol) to the assay mixture and incubated for 60 min at 37 °C before centrifugation at 14,000g for 10 min. H2S concentration of the supernatants was measured using a highly specific H2S sensor connected to a single channel analyzer (Apollo 1000, WPI, Sarasota, FL) and was calculated using a calibration curve of NaHS standards. Protein concentration was measured spectrophotometrically at 595 nm. The results were calculated as μM/mg of protein [45].
Echocardiography
Echocardiography was performed using the Vevo770™ imaging system (VisualSonics Inc., Toronto, Canada) prior to surgery (baseline) and 24 h after surgery prior to sacrificing the animal. Pentobarbital (30 mg/kg; ip) was used for anesthesia and the procedure was carried out as previously described [40] to measure LV end-diastolic diameter (LVEDD) and end-systolic diameter (LVESD). LV fractional shortening (FS) was calculated as (LVEDD − LVESD)/LVEDD × 100.
Statistics
All measurements are expressed as group mean ± SE. The data were analyzed by unpaired t test between 2 groups or one-way ANOVA among 3 or more groups where normal distribution was justified according to the Kolmogorov–Smirnov test. If a significant value of F was obtained in ANOVA, the Student–Newman–Keuls post hoc test was further used for pair-wise comparisons. For data sets with n ≤ 3, non-parametric testing using Kruskal–Wallis test was used. P < 0.05 was considered significant.
Results
Cardioprotection with PKGIα overexpression in vivo: role of H2S
A total of 106 mice for in vivo studies were used. Twenty-four hours following I/R injury, 7 out of 8 (88 %) mice survived with in vivo intraventricular injection of Ad.PKGIα as compared to 6 out of 10 (60 %) with injection of inactive mutant PKGIαK390A. CSE inhibition with PAG in mice treated with Ad.PKGIα reduced survival to 60 % following I/R. PAG administration in mice injected with Ad.PKGIαK390A had no adverse effects on survival as compared with PBS control. PKG inhibition with KT5823 at the onset of reperfusion in mice treated with Ad.PKGIα also reduced survival to 60 % following I/R, which was similar to survival in the control group that received KT5823 at reperfusion. The survival rate was 100 % in sham-operated mice.
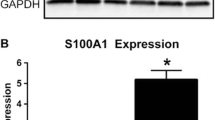
Ad.PKGIα and Ad.PKGIαK390A injections in the LV increased expression of PKGIα mRNA and protein as compared with the hearts injected with vehicle (Fig. 2). Overexpression of PKGIα also induced CSE expression without altering the expression of CBS or 3-MST in the heart as compared to control and PKGIαK390A as shown in Fig. 3. Moreover myocardial H2S level was increased 8-Fold with PKGIα overexpression as compared to sham and PKGIαK390A (P < 0.01, Fig. 4a).
PKG-Iα overexpression increased myocardial CSE protein expression as compared to control and K390A mutant groups (P < 0.05). This corroborates the increase in cardiac H2S levels observed with PKG-Iα overexpression in the heart. PKG-Iα overexpression had no effect on the expression profiles of CBS and 3-MST
H2S tissue levels assessed in hearts harvested 96 h after intramyocardial injection of Ad.PKG-Iα or Ad.PKG-IαK390A (a) and cardiomyocytes at 24 h after infection with Ad.PKG-Iα or Ad.PKG-IαK390A (b). Note that Ad.PKG-Iα caused an increase in H2S compared with control and K390A mutant groups (P < 0.01) in both cases
Myocardial infarct size (% of risk area, mean ± SEM) was reduced from 37.5 ± 2.2 in PBS control to 14.1 ± 1.4 with PKGIα overexpression following 30 min of ischemia and 24 h of reperfusion (P < 0.05, Fig. 5a, b). PKG-IαK390A mutant had no effect on infarct size (37.3 ± 3.6, P > 0.05 vs. control). The infarct-limiting effect of PKGIα overexpression was abolished with PAG (45.2 ± 2.2, P < 0.05 vs. PKGIα). Treatment with PAG alone resulted in infarct size similar to control. PKG inhibition with KT5823 at the onset of reperfusion caused partial blockade of the infarct-sparing effect of PKGIα overexpression (27.5 ± 4.4, P < 0.05 vs. control and PKGIα). Treatment with KT5823 alone at reperfusion resulted in infarct size similar to control. The risk areas (% LV) were not different between the groups (Fig. 5c). Sham-operated mice did not exhibit any infarction (not shown).
a Representative heart sections stained with phthalo blue to demarcate the non-risk area and TTC to identify viable tissue. b Myocardial infarct size (% of RA) measured 24 h post-MI in the various groups. Note that intramyocardial injection of adenoviral constructs encoding for PKG-Iα exhibited a smaller infarct size following I/R compared to mutant K390A or control groups. PAG abolished the protection observed with PKG-Iα overexpression whereas KT5823 caused partial blockade of the infarct-sparing effect of PKG-Iα overexpression. c The area-at-risk, expressed as percent of the left ventricle, was similar in all groups
Figure 6 shows results of M-mode echocardiography from baseline and I/R in the various treatment groups 24 h following I/R injury. None of the groups showed significant LV dilatation at 24 h (Fig. 6a). However, PKGIα overexpression decreased LV end-systolic diameter (LVESD: 2.5 ± 0.1 mm, Fig. 6b) and preserved fractional shortening (FS: 32 ± 1.1 %, Fig. 6c) as compared to I/R control (LVESD: 3.0 ± 0.2 mm and FS: 19 ± 3 %, respectively; P < 0.05) and mutant K390A (LVESD: 3.1 ± 0.1 mm and FS: 19 ± 1 %, respectively; P < 0.05). PAG and KT5823 abolished the protective effect of PKGIα on cardiac contractility (P < 0.05). Baseline LVESD and FS were 2.0 ± 0.1 mm and 44 ± 2 %, respectively.
Representative M-mode images illustrating the preservation of LV contractility with PKG gene therapy compared with other groups. LV end-diastolic diameter (a), end-systolic diameter (b), and fractional shortening (c) measured in the various treatment groups. Although there was no marked dilatation at 24 h post-MI in all groups, PKG-Iα overexpression prevented the increase in LV end-systolic diameter seen in the other groups and preserved fractional shortening
PKG-Iα overexpression protects against ischemia/reoxygenation injury in cardiomyocytes
Infection with adenoviral PKGIα in cardiomyocytes caused 4.9-Fold increase in H2S concentration as compared to control and PKGIαK390A mutant (P < 0.05, Fig. 4b). The percentage of trypan blue-positive cardiomyocytes decreased with PKGIα overexpression to 17.2 ± 0.9 % as compared with SI-RO controls (37.1 ± 1.8 %) or PKGIαK390A mutant overexpression (38.0 ± 2.0 %, n = 6; P < 0.05). Incubation with PAG abolished the protective effect of PKGIα as evidenced by increased necrosis (35.2 ± 1.7 %, Fig. 7a). Similarly, PKG1α overexpression attenuated the release of LDH following SI/RO. PKGIαK390A control did not exert any protective effects as shown by elevated LDH release (Fig. 7b).
Necrosis assessed by trypan blue staining (a) and LDH release (b) as well as apoptosis assessed by TUNEL (c) following SI/RO in primary adult rat cardiomyocytes demonstrating a decrease in cell death with PKG-Iα overexpression compared to control and K390A mutant groups. PAG blocked the protective effect of PKG overexpression
PKGIα overexpression also decreased apoptosis in cardiomyocytes following SI/RO. The percentage of TUNEL-positive nuclei was lower with PKGIα (13.2 ± 0.8 %, P < 0.05) as compared to the non-treated control group (26.9 ± 2.8 %) and PKGIαK390A mutant (25.9 ± 1.9 %) as shown in Fig. 7c.
Discussion
Our results show that direct overexpression of PKGIα in the intact heart and adult cardiomyocytes protected against I/R injury. Such protective effect of PKGIα gene therapy was associated with significant increase in the levels of H2S. Inhibition of CSE with PAG abolished the cardioprotective effect of PKGIα, likely by decreasing H2S levels both in cardiomyocytes as well as intact heart. These results suggest that H2S is an important mediator of the cardioprotective effect of PKGIα.
There has been considerable interest in studying the role of the NO-cGMP-PKG pathway in protection of the heart against I/R injury [11, 21, 30, 38]. Inhibition of cGMP-specific PDE5 with the selective potent inhibitors, sildenafil (Viagra), vardenafil (Levitra), and tadalafil (Cialis), induced protective effects against I/R injury in the heart [33, 41, 43] and adult cardiomyocytes [13, 15]. These drugs inhibit the enzymatic hydrolysis of cGMP, which in turn maintains its tissue accumulation, leading to downstream protective mechanisms involving activation of PKG and opening of mitoKATP channels [33, 43]. Recently, we also demonstrated that the NO-independent sGC activator, cinaciguat, induced PKG-dependent generation of H2S from CSE in the mouse heart [42]. In addition, several studies have demonstrated the cardioprotective effects of PKG modulation or activation prior to I/R injury or at the time of reperfusion [3, 6, 10, 32]. The benefits of PKG were not restricted to I/R injury since gene transfer of PKGIβ was shown to enhance the antihypertrophic effects of NO in neonatal rat cardiomyocytes [48]. However, a recent study demonstrated that deletion of PKGI in cardiomyocytes did not amplify cardiac hypertrophy secondary to isoproterenol or trans-aortic constriction in vivo [31]. We tested the effect of pharmacologic inhibition of PKG with KT5823 at the time of reperfusion in our study and our results demonstrate that KT5823 partially blocked the infarct-sparing effect of PKG gene therapy, but completely abolished the preservation in LV function at 24 h following I/R injury. This may be due to several reasons, including late pharmacologic inhibition of PKG (96 h after gene transfer) that may not block signaling pathways that have been already initiated. Another reason may be the half-life and duration of KT5823 in the system, which is too short when compared to adenoviral gene transfer. Finally, side effects of pharmacologic inhibition cannot be ruled out, which may affect function more than infarct sparing in this model.
H2S protects cardiomyocytes by increasing cell viability and improving cell function, and also attenuating I/R injury in isolated-perfused hearts [50, 51]. Moreover, NaHS (H2S donor), given at reperfusion and then daily for 7 days following ischemia protected against the structural and functional deterioration of the heart by attenuating oxidative stress and mitochondrial dysfunction [7]. We previously showed that the long-acting PDE5 inhibitor, tadalafil, reduced infarct size after I/R injury and attenuated LV dysfunction through PKG-dependent generation of H2S [41]. The infarct-sparing effect of tadalafil was abolished by the CSE inhibitor, PAG, as well as in CSE-knockout mice in these studies. Interestingly, the current study provides direct evidence that PKG is the central enzyme in the cGMP signaling cascade that is responsible for protection against I/R injury in vitro and in vivo, independent of pharmacological agents such as PDE5 inhibitors or GC activators, which may have off-target protective effects secondary to PKG activation. Although we have previously demonstrated that PKG overexpression protects primary cardiomyocytes against SI/RO [14], the current study highlights the role of H2S in mediating this cytoprotective effect. Our results showed increase in H2S levels in cardiomyocytes overexpressing PKGIα, but not its inactive mutant form and also demonstrated that CSE inhibition abolished the cytoprotective effects of gene therapy with PKG in cardiomyocytes. This observation also paralleled our in vivo studies where the CSE enzyme in the heart appears to be targeted by PKGIα because it significantly increased H2S production and PAG was highly effective in blunting myocardial protection following I/R injury. Furthermore, myocardial overexpression of PKGIα caused significant increase in CSE protein, which was not observed in hearts overexpressing inactive PKGIαK390A. Interestingly, the expression profile of the other H2S-producing enzymes, CBS and 3-MST, was not changed by PKG overexpression. These results further support the key role that CSE-driven H2S generation plays in mediating the protective effects of PKG.
A potential role of NO in protection against SI/RO injury in cardiomyocytes following overexpression of PKGIα was suggested in our previous study [14]. A clear identification of a potential cross-talk between NO and H2S signaling in mediating the cardioprotective effects of PKGIα requires further investigation, although recent reviews have alluded to a relationship between these gaseous molecules in the context of endothelial dysfunction [1]. Akt phosphorylation was also implicated as a potential key player in PKGIα-induced protection of primary rat cardiomyocytes against SI/RO injury [14]. Interestingly, our recent study demonstrating the infarct-sparing and anti-inflammatory effects of H2S against myocardial I/R injury also revealed an increase in Akt phosphorylation with sulfide donor [46]. This possibly indicates that induction of Akt phosphorylation with PKGIα overexpression may be mediated by H2S. Further studies are warranted to explore this premise.
Exactly how PKG overexpression is associated with increased CSE is not clear from the present study although it may be related to PKG-dependent enhancement of the transcription factor Sp1. There is evidence that Sp1 plays an important role in the basal transcriptional activity of CSE enzyme [24] and regulates its gene expression in vascular smooth muscle cells [49]. PKG can phosphorylate Sp1 on serine residue(s), which results in transcriptional activation of Sp1 in human SW480 colon cancer cells [8] with consequent increase in CSE activity and possibly generation of H2S. Future studies are warranted to investigate the mechanism through which PKG induces CSE expression in the heart.
It is noteworthy that despite the cytoprotective effect of PKGIα gene therapy in primary cardiomyocytes, it is unclear from our study whether other cardiac cell types also profit from PKG overexpression and contribute to the salutary effects following I/R injury in vivo. Although we have previously shown that primary cardiomyocytes isolated from adult mice do express PDE5, recent studies have conveyed discrepant findings [31] and reported low concentrations of cGMP in these cells [20]. Therefore, identification of sGC- or particulate GC-regulated pool of cGMP as the source of cardioprotection with PKG gene therapy cannot be determined from our study. Future studies are needed to dissect the involvement of individual cell types and the regulatory source of cGMP contributing toward such protection.
Recent studies have shown that oxidant sensing and signaling by kinases play an important role in cardiovascular function [5], although other studies have indicated that cGMP-dependent activation of PKG renders it resistant to disulfide formation and therefore desensitizes PKG to oxidation [4]. This was shown to occur to a greater degree in aorta as opposed to mesenteries since aorta has higher peroxidase activity as demonstrated in the same study. Based on this information, we believe that the primary mechanism of PKG activation in the heart is cGMP-dependent, which is supported by several studies demonstrating significant increase in PKG activity with cGMP regulating drugs, including PDE-5 inhibitors and sGC activators [41, 42]. A very recent study showed that PKGIα oxidation paradoxically mediates, to a certain extent, the blood pressure-lowering effect of H2S [44]. Although this signaling pathway seems contradictory to the findings in the current study, in reality it highlights the possible interaction between the NO and H2S axes whereby NO may drive H2S generation through activation of PKG and H2S, in turn, may activate PKG through either eNOS phosphorylation leading to increased cGMP [18] or by catalyzing the formation of an activating interprotein disulfide within PKG [44]. Moreover, H2S has been proposed as a non-selective PDE inhibitor [2], which may also contribute to cGMP/PKG axis activation.
In summary, we have provided evidence that myocardial gene therapy with PKGIα protects against I/R injury by reducing infarct size and preserving LV function through H2S generation. We believe that gene therapy with PKGIα or its pharmacologic activation may share a similar signaling pathway involving generation of physiologic levels of H2S in attenuating ischemic cardiomyopathy as illustrated in Fig. 8. Although gene therapy for cardiovascular disease is not currently practiced due to concerns regarding viral delivery, the use of FDA-approved drugs that can activate PKG (such as sildenafil and tadalafil) may replace the need for such an approach. Therefore, this study serves as a proof-of-concept for the importance of PKG activators in cardioprotection with the involvement of H2S as a mediator.
References
Altaany Z, Moccia F, Munaron L, Mancardi D, Wang R (2014) Hydrogen sulfide and endothelial dysfunction: relationship with nitric oxide. Curr Med Chem 21:3646–3661. doi:10.2174/0929867321666140706142930
Bibli SI, Yang G, Zhou Z, Wang R, Topouzis S, Papapetropoulos A (2015) Role of cGMP in hydrogen sulfide signaling. Nitric Oxide 46:7–13. doi:10.1016/j.niox.2014.12.004
Bice JS, Baxter GF (2014) Postconditioning signaling in the heart: mechanisms and translatability. Br J Pharmacol. doi:10.1111/bph.12976
Burgoyne JR, Prysyazhna O, Rudyk O, Eaton P (2012) cGMP-dependent activation of protein kinase G precludes disulfide activation: implications for blood pressure control. Hypertension 60:1301–1308. doi:10.1161/HYPERTENSIONAHA.112.198754
Burgoyne JR, Oka S, Ale-Agha N, Eaton P (2013) Hydrogen peroxide sensing and signaling by protein kinases in the cardiovascular system. Antioxid Redox Signal 18:1042–1052. doi:10.1089/ars.2012.4817
Burley DS, Ferdinandy P, Baxter GF (2007) Cyclic GMP and protein kinase-G in myocardial ischaemia-reperfusion: opportunities and obstacles for survival signaling. Br J Pharmacol 152:855–869. doi:10.1038/sj.bjp.0707453
Calvert JW, Elston M, Nicholson CK, Gundewar S, Jha S, Elrod JW, Ramachandran A, Lefer DJ (2010) Genetic and pharmacologic hydrogen sulfide therapy attenuates ischemia-induced heart failure in mice. Circulation 122:11–19. doi:10.1161/CIRCULATIONAHA.109.920991
Cen B, Deguchi A, Weinstein IB (2008) Activation of protein kinase G Increases the expression of p21CIP1, p27KIP1, and histidine triad protein 1 through Sp1. Cancer Res 68:5355–5362. doi:10.1158/0008-5472.CAN-07-6869
Chau VQ, Salloum FN, Hoke NN, Abbate A, Kukreja RC (2011) Mitigation of the progression of heart failure with sildenafil involves inhibition of RhoA/Rho-kinase pathway. Am J Physiol Heart Circ Physiol 300:H2272–H2279. doi:10.1152/ajpheart.00654.2010
Cohen MV, Downey JM (2014) Signalling pathways and mechanisms of protection in pre- and postconditioning: historical perspective and lessons for the future. Br J Pharmacol. doi:10.1111/bph.12903
D’Souza SP, Yellon DM, Martin C, Schulz R, Heusch G, Onody A, Ferdinandy P, Baxter GF (2003) B-type natriuretic peptide limits infarct size in rat isolated hearts via KATP channel opening. Am J Physiol Heart Circ Physiol 284:H1592–H1600. doi:10.1152/ajpheart.00902.2002
Das A, Salloum FN, Xi L, Rao YJ, Kukreja RC (2009) ERK phosphorylation mediates sildenafil-induced myocardial protection against ischemia-reperfusion injury in mice. Am J Physiol Heart Circ Physiol 296:H1236–H1243. doi:10.1152/ajpheart.00100.2009
Das A, Salloum FN, Xi L, Rao YJ, Kukreja RC (2009) Role of ERK1/2 phosphorylation in sildenafil-induced myocardial protection against ischemia-reperfusion injury in mice. Am J Physiol Heart Circ Physiol 296:H1236–H1243. doi:10.1152/ajpheart.00100.2009
Das A, Smolenski A, Lohmann SM, Kukreja RC (2006) Cyclic GMP-dependent protein kinase Ialpha attenuates necrosis and apoptosis following ischemia/reoxygenation in adult cardiomyocyte. J Biol Chem 281:38644–38652. doi:10.1074/jbc.M606142200
Das A, Xi L, Kukreja RC (2005) Phosphodiesterase-5 inhibitor sildenafil preconditions adult cardiac myocytes against necrosis and apoptosis: essential role of nitric oxide signaling. J Biol Chem 280:12944–12955. doi:10.1074/jbc.M404706200
Das A, Xi L, Kukreja RC (2008) Protein kinase G-dependent cardioprotective mechanism of phosphodiesterase-5 inhibition involves phosphorylation of ERK and GSK3beta. J Biol Chem 283:29572–29585. doi:10.1074/jbc.M801547200
Elrod JW, Calvert JW, Morrison J, Doeller JE, Kraus DW, Tao L, Jiao X, Scalia R, Kiss L, Szabo C, Kimura H, Chow CW, Lefer DJ (2007) Hydrogen sulfide attenuates myocardial ischemia-reperfusion injury by preservation of mitochondrial function. Proc Natl Acad Sci USA 104:15560–15565. doi:10.1073/pnas.0705891104
Francis SH, Corbin JD (1999) Cyclic nucleotide-dependent protein kinases: intracellular receptors for cAMP and cGMP action. Crit Rev Clin Lab Sci 36:275–328. doi:10.1080/10408369991239213
Geng B, Yang J, Qi Y, Zhao J, Pang Y, Du J, Tang C (2004) H2S generated by heart in rat and its effects on cardiac function. Biochem Biophys Res Commun 313:362–368. doi:10.1016/j.bbrc.2003.11.130
Gotz KR, Sprenger JU, Perera RK, Steinbrecher JH, Lehnart SE, Kuhn M, Gorelik J, Balligand JL, Nikolaev VO (2014) Transgenic mice for real-time visualization of cGMP in intact adult cardiomyocytes. Circ Res 114:1235–1245. doi:10.1161/CIRCRESAHA.114.302437
Han J, Kim N, Kim E, Ho WE, Earm YE (2001) Modulation of ATP-sensitive potassium channels by cGMP-dependent protein kinase in rabbit ventricular myocytes. J Biol Chem 276:22140–22147. doi:10.1074/jbc.M010103200
Hofmann F, Ammendola A, Schlossmann J (2000) Rising behind NO: cGMP-dependent protein kinases. J Cell Sci 113:1671–1676
Hou J, Kang YJ (2012) Regression of pathological cardiac hypertrophy: signaling pathways and therapeutic targets. Pharmacol Ther 135:337–354. doi:10.1016/j.pharmthera.2012.06.006
Ishii I, Akahoshi N, Yu XN, Kobayashi Y, Namekata K, Komaki G, Kimura H (2004) Murine cystathionine gamma-lyase: complete cDNA and genomic sequesnces, promoter activity, tissue distribution and developmental expression. Biochem J 381:113–123
Keilbach A, Ruth P, Hofmann F (1992) Detection of cGMP dependent protein kinase isozymes by specific antibodies. Eur J Biochem 208:467–473. doi:10.1111/j.1432-1033.1992.tb17209.x
King AL, Polhemus DJ, Bhushan S, Otsuka H, Kondo K, Nicholson CK, Bradley JM, Islam KN, Calvert JW, Tao YX, Dugas TR, Kelley EE, Elrod JW, Huang PL, Wang R, Lefer DJ (2014) Hydrogen sulfide cytoprotective signaling is endothelial nitric oxide synthase-nitric oxide dependent. Proc Natl Acad Sci USA 111:3182–3187. doi:10.1073/pnas.1321871111
Kondo K, Bhushan S, King AL, Prabhu SD, Hamid T, Koenig S, Murohara T, Predmore BL, Gojon G Sr, Gojon G Jr, Wang R, Karusula N, Nicholson CK, Calvert JW, Lefer DJ (2013) H2S protects against pressure overload-induced heart failure via upregulation of endothelial nitric oxide synthase. Circulation 127:1116–1127. doi:10.1161/CIRCULATIONAHA.112.000855
Kukreja RC (2012) Phosphodiesterase-5 and retargeting of subcellular cGMP signaling during pathological hypertrophy. Circulation 126:916–919. doi:10.1161/CIRCULATIONAHA.112.124966
Kukreja RC, Salloum F, Das A, Ockaili R, Yin C, Bremer YA, Fisher PW, Wittkamp M, Hawkins J, Chou E, Kukreja AK, Wang X, Marwaha V, Xi L (2005) Pharmacological preconditioning with sildenafil: basic mechanisms and clinical implications. Vascul Pharmacol 42:219–232. doi:10.1016/j.vph.2005.02.010
Kukreja RC, Salloum FN, Das A (2012) Cyclic guanosine monophosphate signaling and phosphodiesterase-5 inhibitors in cardioprotection. J Am Coll Cardiol 59:1921–1927. doi:10.1016/j.jacc.2011.09.086
Lukowski R, Rybalkin SD, Loga F, Leiss V, Beavo JA, Hofmann F (2010) Cardiac hypertrophy is not amplified by deletion of cGMP-dependent protein kinase I in cardiomyocytes. Proc Natl Acad Sci USA 107:5646–5651. doi:10.1073/pnas.1001360107
Methner C, Lukowski R, Grube K, Loga F, Smith RA, Murphy MP, Hofmann F, Krieg T (2013) Protection through postconditioning or a mitochondria-targeted S-nitrosothiol is unaffected by cardiomyocyte-selective ablation of protein kinase G. Basic Res Cardiol 108:337. doi:10.1007/s00395-013-0337-1
Ockaili R, Salloum F, Hawkins J, Kukreja RC (2002) Sildenafil (Viagra) induces powerful cardioprotective effect via opening of mitochondrial K(ATP) channels in rabbits. Am J Physiol Heart Circ Physiol 283:H1263–H1269. doi:10.1152/ajpheart.00324.2002
Paulus WJ, Tschöpe C (2013) A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol 62:263–271. doi:10.1016/j.jacc.2013.02.092
Polhemus DJ, Lefer DJ (2014) Emergence of hydrogen sulfide as an endogenous gaseous signaling molecule in cardiovascular disease. Circ Res 114:730–737. doi:10.1161/CIRCRESAHA.114.300505
Pryor WA, Houk KN, Foote CS, Fukuto JM, Ignarro LJ, Squadrito GL, Davies KJ (2006) Free radical biology and medicine: it’s a gas, man! Am J Physiol Regul Integr Comp Physiol 291:R491–R511. doi:10.1152/ajpregu.00614.2005
Qin Q, Yang XM, Cui L, Critz SD, Cohen MV, Browner NC, Lincoln TM, Downey JM (2004) Exogenous NO triggers preconditioning via a cGMP- and mitoKATP-dependent mechanism. Am J Physiol Heart Circ Physiol 287:H712–H718. doi:10.1152/ajpheart.00954.2003
Rassaf T, Totzeck M, Hendgen-Cotta UB, Shiva S, Heusch G, Kelm M (2014) Circulating nitrite contributes to cardioprotection by remote ischemic preconditioning. Circ Res 114:1601–1610. doi:10.1161/CIRCRESAHA.114.303822
Salloum FN (2015) Hydrogen sulfide and cardioprotection—mechanistic insights and clinical translatability. Pharmacol Ther. doi:10.1016/j.pharmthera.2015.04.004
Salloum FN, Abbate A, Das A, Houser J, Mudrick CA, Qureshi IZ, Hoke NN, Roy SK, Brown WR, Prabhakar S, Kukreja RC (2008) Sildenafil (Viagra) attenuates ischemic cardiomyopathy and improves left ventricular function in mice. Am J Physiol Heart Circ Physiol 294:H1398–H1406. doi:10.1152/ajpheart.91438.2007
Salloum FN, Chau VQ, Hoke NN, Abbate A, Varma A, Ockaili RA, Toldo S, Kukreja RC (2009) Phosphodiesterase-5 inhibitor, tadalafil, protects against myocardial ischemia/reperfusion through protein-kinase G dependent generation of hydrogen sulfide. Circulation 120:S31–S36. doi:10.1161/CIRCULATIONAHA.108.843979
Salloum FN, Das A, Samidurai A, Hoke NN, Chau VQ, Ockaili RA, Stasch JP, Kukreja RC (2012) Cinaciguat, a novel activator of soluble guanylate cyclase, protects against ischemia/reperfusion injury: role of hydrogen sulfide. Am J Physiol Heart Circ Physiol 302:H1347–H1354. doi:10.1152/ajpheart.00544.2011
Salloum FN, Ockaili R, Wittkamp M, Marwaha VR, Kukreja RC (2006) Vardenafil: a novel type 5 phosphodiesterase inhibitor reduces myocardial infarct size following ischemia/reperfusion injury via opening of mitochondrial KATP channels in rabbits. J Mol Cell Cardiol 40:405–411. doi:10.1016/j.yjmcc.2005.10.002
Stubbert D, Prysyazhna O, Rudyk O, Scotcher J, Burgoyne JR, Eaton P (2014) Protein kinase G Iα oxidation paradoxically underlies blood pressure lowering by the reductant hydrogen sulfide. Hypertension 64:1344–1351. doi:10.1161/HYPERTENSIONAHA.114.04281
Su YW, Liang C, Jin HF, Tang XY, Han W, Chai LJ, Zhang CY, Geng B, Tang CS, Du JB (2009) Hydrogen sulfide regulates cardiac function and structure in adriamycin-induced cardiomyopathy. Circ J 73:741–749
Toldo S, Das A, Mezzaroma E, Chau VQ, Marchetti C, Durrant D, Samidurai A, Van Tassell BW, Yin C, Ockaili RA, Vigneshwar N, Mukhopadhyay ND, Kukreja RC, Abbate A, Salloum FN (2014) Induction of microRNA-21 with exogenous hydrogen sulfide attenuates myocardial ischemic and inflammatory injury in mice. Circ Cardiovasc Genet 7:311–320. doi:10.1161/CIRCGENETICS.113.000381
Varma A, Das A, Hoke NN, Durrant DE, Salloum FN, Kukreja RC (2012) Anti-inflammatory and cardioprotective effects of tadalafil in diabetic mice. PLoS One 7:e45243. doi:10.1371/journal.pone.0045243
Wollert KC, Fiedler B, Gambaryan S, Smolenski A, Heineke J, Butt E, Trautwein C, Lohmann SM, Drexler H (2002) Gene transfer of cGMP-dependent protein kinase I enhances the antihypertrophic effects of nitric oxide in cardiomyocytes. Hypertension 39:87–92
Yang G, Pei Y, Teng H, Cao Q, Wang R (2011) Specificity protein-1 as a critical regulator of human cyctathionine gamma-lyase in smooth muscle cells. J Biol Chem 286:26450–26460. doi:10.1074/jbc.M111.266643
Yong QC, Lee SW, Foo CS, Neo KL, Chen X, Bian JS (2008) Endogenous hydrogen sulphide mediates the cardioprotection induced by ischemic postconditioning. Am J Physiol Heart Circ Physiol 295:H1330–H1340. doi:10.1152/ajpheart.00244.2008
Yong QC, Pan TT, Hu LF, Bian JS (2008) Negative regulation of beta-adrenergic function by hydrogen sulphide in the rat hearts. J Mol Cell Cardiol 44:701–710. doi:10.1016/j.yjmcc.2008.01.007
Acknowledgments
The authors would like to thank Jun He, M.S. and Dr. Nitai Mukhopadhyay for performing the biostatistical analyses for this study. This study was supported in part by a grant from the American Heart Association (BGIA 0765273U) to AD, grants from the National Institutes of Health (HL51045, HL59469, and HL79424) to RCK, and grants from the American Heart Association (10SDG3770011 and 14GRNT20010003) and the Virginia Commonwealth University Presidential Research Quest Fund to FNS.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Das, A., Samidurai, A., Hoke, N.N. et al. Hydrogen sulfide mediates the cardioprotective effects of gene therapy with PKG-Iα. Basic Res Cardiol 110, 42 (2015). https://doi.org/10.1007/s00395-015-0500-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00395-015-0500-y