Abstract
Purpose
Low vitamin D status is a global problem and has been associated with reduced skeletal and cardiometabolic health. However, evidence in young children is lacking. We, therefore, aimed to characterise vitamin D status in toddlers, identify its determinants, and explore if vitamin D status was associated with bone mineralisation and lipid profile.
Methods
We used cross-sectional data from 3-year-old children (n = 323) living in Denmark (latitude: 55°N). Bone mineralisation (n = 108) was measured by DXA. Blood samples were analysed for serum 25-hydroxyvitamin D (s-25(OH)D) by LC–MS/MS, triacylglycerol, and total, low- and high density lipoprotein cholesterol.
Results
Mean ± SD s-25(OH)D was 69 ± 23 nmol/L, but varied with season. During winter, 38% had inadequate s-25(OH)D (< 50 nmol), whereof 15% had deficiency (< 30 nmol/L); these numbers were only 7 and 1% during summer. In terms of status determinants, supplement use (66% were users) was associated with s-25(OH)D (P < 0.001), whereas dietary vitamin D intake (median [25–75th percentile] of 1.3 [0.9–1.9] µg/d), sex, parental education, BMI, and physical activity were not. There were no associations between s-25(OH)D and blood lipids or bone measurements, using either unadjusted or adjusted regression models.
Conclusion
More than 1/3 of Danish toddlers had inadequate vitamin D intake during winter, but acceptable mean vitamin D status. In addition to season, supplement use was the main determinant of vitamin D status, which was, however, not associated with bone mineralisation or lipid profile. The results support recommendations of vitamin D supplements during winter at northern latitudes, but potential health effects need further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D has received much attention during the last decade due to widespread vitamin D deficiency globally and its association with both skeletal and extra-skeletal health [1,2,3]. Early childhood is a vulnerable period of profound growth and development during which maintenance of sufficient vitamin D status may be particularly important for health outcomes later in life. However, evidence on the prevalence and predictors of low vitamin D status, as well as its effects on health, is lacking in young children.
The prevalence of vitamin D insufficiency, defined as serum 25-hydroxyvitamin D (s-25(OH)D) < 50 nmol/L, has been reported to be as high as 20–70% in children and adolescents living at northern latitudes [1, 4,5,6,7,8,9,10]. Yet, this is not well described in toddlers, but has been reported to be around 20–30% among 2- to 6-year-olds living in Denmark, Sweden, and Ireland across seasons, but with a much higher prevalence during winter than summer months [11,12,13]. Since vitamin D occur naturally in only few foods, vitamin D intakes are low in most countries worldwide [3], especially in those with limited fortification, such as Denmark [14, 15]. All European countries recommend vitamin D supplementation during infancy [3], but until December 2020, supplements were not recommended in the Nordic countries past the first 2 years of life [14].
Identification of determinants of vitamin D status is important for preventing low vitamin D status. Aside from sun exposure [4, 10, 13, 16,17,18,19,20,21] and dietary vitamin D intake [6, 13, 16, 18,19,20, 22], age [10, 18,19,20], body mass index (BMI) [22, 23], and time spend on physical activity (PA) [4, 19, 20] have previously been associated with vitamin D status in children. Most of the existing literature is, however, based on children above 4 years of age, whereas determinants of vitamin D status in toddlers are not well characterised.
Vitamin D is important for optimal bone mineralisation via effects on intestinal absorption of calcium [3]. Some [5, 7, 24, 25] but not all studies [8, 9, 21, 26] in children have shown a positive association between s-25(OH)D and measures of bone mineralisation. Further, we recently found that vitamin D supplementation during winter increased bone mineralisation in 6- to 8-year-old Danish children [27]. Apart from bone, vitamin D receptors are also located in cells of the cardiovascular and immune system [3], and in children, s-25(OH)D has been associated with a more favourable blood lipid profile [28,29,30,31,32], although not consistently [33]. In our previous study in 6- to 8-year-olds, vitamin D supplementation reduced low-density lipoprotein cholesterol (LDL-C) [34], but other studies showed no effects on blood lipids [35, 36] or even increased LDL-C [37]. Thus, evidence on vitamin D and health-related outcomes in children is conflicting, and we lack studies in the younger age groups.
Thus, the aims of the present cross-sectional study were to (1) characterise vitamin D status as reflected by s-25(OH)D in 3-year-old Danish children, (2) identify determinants of vitamin D status at this age, and (3) explore possible associations between vitamin D status and bone mineralisation as well as lipid profile in these children. We hypothesised that there would be seasonal differences in vitamin D status, and that any associations between vitamin D intake and use of supplements, respectively, and vitamin D status would differ according to season. Further, we hypothesised that vitamin D status would be positively associated with measures of bone mineralisation and with a more favourable blood lipid profile. In order to base this on a considerable and broad sample of Danish toddlers, we pooled data from two cohorts that included children of mothers with mainly normal weight and obesity, respectively, that were examined using similar protocols and across all seasons. Secondarily, we explored whether any of the results were cohort-specific.
Methods
Study design and population
The study included children from two Danish child cohorts, SKOT-I [38] and SKOT-II [39]. The overall aim of both cohorts was to describe how complementary feeding influences growth and later disease risk, and inclusion criteria were term singletons aged 9 months ± 2 weeks without illnesses known to affect diet or growth and living in Copenhagen or Frederiksberg (latitude: 55oN). In SKOT-I, infants were recruited from the National Danish Civil Registry [38]. In SKOT-II, infants were recruited among pregnant women participating in the intervention study ‘Treatment of Obese Pregnant Women’ at Hvidovre Hospital (Hvidovre, Denmark) [40], and thus had a pre-pregnancy BMI > 30 kg/m2. The two cohorts followed the same measurement protocol and together represent a wide range of maternal weight statuses and social classes [39]. SKOT-I was conducted from April 2007 to October 2010 and SKOT-II from January 2011 to March 2015. The studies were conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures were approved by the Committees on Biomedical Research Ethics for the Capital Region of Denmark (SKOT-I: H-KF-2007-0003; SKOT-II: H-3-2010-122). Written informed consent was obtained from all custody holders of the children.
In SKOT-I and SKOT-II, respectively, 329 and 183 infants were enrolled, and examinations took place at age 9, 18, and 36 months. The present study uses cross-sectional data from the 3-year examination and includes only children with available s-25(OH)D, corresponding to 67% (n = 220) and 56% (n = 103) of the children in the original SKOT-I and SKOT-II cohorts, respectively. Bone outcomes were only measured in SKOT-I (n = 108).
Background information and season
Parental education was obtained from an interview at the 36-month visit, defined as the highest completed education by any parent, and categorised as short (ranging from ≤ lower secondary education to short higher education < 3 years), medium (3–4 years), or long (> 4 years). We considered children’s skin pigmentation due to its influence on dermal vitamin D synthesis; however, this was only registered for those with a dual-energy X-ray absorptiometry (DXA) scan (n = 166), where 98% were characterised as “white”. Season of examination was categorised as spring (March–May), summer (June–August), autumn (September–November), and winter (December–February). As vitamin D was not a focus of the cohorts at their planning stages, there were no data on use of sunscreen, time spend outdoor, or sunny vacations. Almost all children (94% of children in SKOT-I and all in SKOT-II) had access to own or shared garden or court, so this was not meaningful to include in the analyses.
Dietary intake and use of supplements
Dietary vitamin D intake was assessed from 7-day (SKOT-I) or 4-day (SKOT-II) validated, pre-coded dietary records [41]. The intake was calculated by the National Food Institute, Technical University of Denmark, using the GIES software (version 1.000 d; National Food Institute, Søborg, Denmark), which uses data from the Danish food composition database [42]. Parents further recorded time and content of the child’s last meal before the examination visit, from which energy and macronutrient intake was calculated. Frequency of supplement use was obtained from interview at the visit, and since the majority of multivitamins in Denmark contain vitamin D, multivitamins were categorised as vitamin D containing supplements along with vitamin D drops and vitamin D tablets. Use of vitamin D supplements was categorised as “yes” when the frequency was ≥ 1/week, and as “no” when < 1/week. Data regarding the dose of vitamin D supplied by the supplementation was not available and thus total vitamin D intake could not be estimated.
Physical activity
As previously described [43, 44], time spend on PA was measured during 7 days and nights by tri-axis accelerometer (Actigraph GT3X), which was placed on the right hip by an elastic waistband. Parents were instructed only to take it off when the child was showering or swimming and to note any non-wear time. The data was analysed using the Actilife software version 6.4.5 (Actigraph, Pensacola, Florida) and expressed as mean counts per minute (CPM) per day from at least four valid days (> 8 h wear time). Data were available from 197 and 79 children from SKOT-I and SKOT-II, respectively.
Anthropometry and body composition
Measurements of anthropometrics and body composition are described in detail elsewhere [45, 46]. In brief, body weight was measured once without clothes to the nearest 0.1 kg using a Tanita WB-100MA digital scale (Tanita, Amsterdam, Netherlands). Height was measured in triplicate to the nearest 0.1 cm using a 235 Heightronic Digital Stadiometer (Quick Medical and Measurement Concepts, USA) and the mean was used in the analyses. BMI was calculated as weight divided by height squared, and age- and sex-specific z-scores were calculated by using the software WHO Anthro 2005 [45].
Fat mass and fat free mass were obtained by bioelectrical impedance using a Quantum III (RJL Systems, USA). Measurements were performed twice and mean resistance values used in the equation to predict fat free mass. Because equations for children in early childhood was scarce, the equation was developed in SKOT-I and validated by cross-referencing with DXA data, as previously described [46]. Data from bioelectrical impedance was chosen over estimates derived from DXA in the present study because DXA scans were only performed in SKOT-I [45]. Fat mass index (FMI) and fat free mass index (FFMI) were calculated as fat mass and fat free mass, respectively, divided by height squared.
Bone mineralisation
Bone mineral content (BMC), bone area (BA), and bone mineral density (BMD) were obtained in SKOT-I using a Lunar Prodigy Advance with enCore software version 12.3 (GE Healthcare, USA). Whole body and regional measures were obtained and total body less head (TBLH) calculated as the sum of arms, legs, and trunk. Results were available from 166 children. Due to their young age, some children shifted position during the scan, which was categorised as “perfect scan”, “good scan with minor irregularities”, “scan with several irregularities”, or “useless scan” [45]. Only “perfect” (n = 74) and “good” (n = 34) scans were included in the present study.
Blood sampling and analyses
As previously described [38], 5 mL venous blood samples were drawn from the forearm in lithium-heparinized tubes after an average ± SD of 2.9 ± 0.7 h of fasting. Time since and composition of the last meal were recorded. Serum triacylglycerol and total (total-C), high-density lipoprotein cholesterol (HDL-C), and LDL-C were analysed using a Pentra 400 (HORIBA ABX) with intra- and inter-assay CV < 4 and ≤ 2%, respectively. Serum 25(OH)D were analysed by LC–MS/MS at University College Cork, Ireland, as described elsewhere [47]. Total s-25(OH)D was calculated as the sum of s-25(OH)D2 and 25(OH)D3, and the intra- and inter-assay CVs for both metabolites were < 5 and < 6%, respectively. Vitamin D sufficiency, insufficiency and deficiency were defined as s-25(OH)D ≥ 50 nmol/L, < 50 and ≥ 30 nmol/L, and < 30 nmol/L, respectively, as suggested by the IOM [48].
Statistical analyses
Data are presented as mean ± SD, median [25–75th percentile], or n (%), as appropriate. All analyses were carried out in Stata version 16.1 and P < 0.05 was considered statistically significant. Differences between cohorts and between included and excluded children were tested with Pearson’s chi-squared test, two-sample t-test, or Wilcoxon rank-sum test.
To identify determinants of vitamin D status, we performed ANCOVA of s-25(OH)D as a function of potential explanatory variables. These were sex (male/female), parental education (short/medium/long), BMI z-score, weight category (under-/normal-/overweight and obesity), FMI, FFMI, season of blood sampling (summer/autumn/winter/spring), dietary vitamin D intake, use of vitamin D supplements (yes/no), and PA. Further, we assessed whether interactions with season existed within the associations between s-25(OH)D and vitamin D intake (season × intake) and supplement use (season × supplements), as has been reported by others [13, 49, 50]. First, these potential determinants were tested one at a time with cohort as a fixed effect and s-25(OH)D as the outcome variable. Then, sex, parental education, FMI, FFMI, season, vitamin D intake, use of supplements, and PA were all introduced in the same, mutually adjusted model. Finally, we explored whether associations were cohort-specific by including determinant × cohort for all potential determinants in the mutually adjusted model, and stratified the analyses by cohort if the interaction term was significant. Since all but two children were recorded as “white”, and since all children were 3.0 ± 0.1 years old, we did not evaluate skin pigmentation or age as determinants.
To explore associations between s-25(OH)D and bone mineralisation as well as blood lipids, we ran linear regression models with the outcomes as dependent variables and s-25(OH)D as explanatory. The crude models included cohort as a fixed factor, and all adjusted models included sex, parental education, and PA, which were pre-specified potential confounders. Additional data-specific potential confounders were included in the relevant models when these were associated with both s-25(OH)D and the outcome in the ANCOVAs described above. As season was associated with both s-25(OH)D and BMC, BMD, and HDL, all adjusted models were adjusted for season. Due to short fasting before blood sampling, blood lipids were further adjusted for fat content (gramme) of last meal, and BMI z-score was investigated as a mediator in the blood lipid models. Bone outcomes were analysed both with and without size-adjustment for height, weight, and BA (BMC only), as recommended by Prentice et al. [51]. Finally, the interaction term s-25(OH)D × cohort was included in each adjusted model to assess whether associations were cohort specific. Model assumptions were checked using residual and Q–Q plots, and plasma triacylglycerol was log-transformed to fulfil these.
Results
Children’s characteristics
The 323 children included in the present study had slightly higher PA compared to those not included (1316 vs 1242 CPM/d, P = 0.040), but did not differ in age, sex, parental education, vitamin D intake or supplement use, anthropometrics, body composition or bone measures (P > 0.1). The included children had a mean ± SD age of 3.0 ± 0.1 years, with an equal number of boys and girls (Table 1), and examinations were evenly distributed among the four seasons (Table 2). Children in SKOT-II had parents with lower parental education level, as previously reported [39], and had higher weight, BMI z-score [52], and FMI, as well as lower total-C than children in SKOT-I (Supplemental Table 1).
Vitamin D intake and status
The children had a very low dietary vitamin D intake (Table 2), which was slightly higher in SKOT-I (1.3 [1.0–2.0] µg/d) than SKOT-II (1.0 [0.8–1.7] µg/d) (P = 0.003). Fewer than 1% of the children had dietary vitamin D intakes reaching the recommended intake of 10 µg/d, but 66% received vitamin D supplements at least once per week, with no difference between the cohorts (65% and 70% in SKOT-I and SKOT-II, respectively, P = 0.34). Mean ± SD s-25(OH)D was 68.6 ± 23.0 nmol/L, and the majority of the children had s-25(OH)D ≥ 50 nmol/L, whereas only 5% (n = 17) had values < 30 nmol/L (Table 2). As expected, there were substantial seasonal differences, as vitamin D status was highest during summer, lower during autumn and spring, and lowest during winter. The prevalence of s-25(OH)D ≥ 50 and < 30 nmol/L, respectively, were 93 and 1% during summer and 62% and 15% during winter (Table 2). Four children who all received supplements and were measured during summer (n = 3) or spring (n = 1) had high s-25(OH)D ≥ 125 nmol/L, of which one had a very high value of 190 nmol/L.
Determinants of vitamin D status
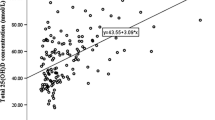
Apart from season of examination, use of vitamin D supplements was positively associated with s-25(OH)D in both the crude and mutually adjusted models (Table 3). Also, most (82%) of the cases of vitamin D deficiency (s-25(OH)D < 30 nmol/L) were found among children that did not receive supplements, comprising 13% of the unsupplemented group. Supplement users had higher s-25(OH)D than non-users regardless of season (Pseason×supplements = 0.13) (Supplemental Figure 1). However, whereas 80% of the supplement users had s-25(OH)D ≥ 50 nmol/L during winter, sufficiency was only found in 23% of the children who did not receive supplements at this time of year. During summer, the corresponding numbers were 97 and 86%. Sex, parental education, BMI, body composition, and PA were not associated with s-25(OH)D, nor was dietary vitamin D intake (Table 3), and this did not depend on season (Pseason×intake = 0.44). Compared to children with normal weight, those with overweight and obesity had lower s-25(OH)D in the crude model (P = 0.019), but this association disappeared after adjustment for sex, parental education, season, vitamin D intake, use of supplements, and PA (P = 0.98) (data not shown). Cohort-specific associations were seen for FMI (PFMI×cohort = 0.029) and PA (PPA×cohort = 0.039), due to an inverse association between FMI and s-25(OH)D and an indication of a positive association between PA and s-25(OH)D, respectively, in SKOT-II only (Supplemental Table 2).
Associations between vitamin D status and bone mineralisation and blood lipids
None of the bone outcomes or blood lipids were associated with s-25(OH)D, neither in the crude nor adjusted regression models (Table 4), and there were no cohort-specific associations (data not shown).
Discussion
In this population of toddlers living at 55°N and measured across the year, 81% had sufficient vitamin D status, whereas only 14 and 5% had insufficiency and deficiency. Season and supplement use were important determinants of s-25(OH)D, which was more than 20 nmol/L higher during summer than winter and among supplement users than non-users, and this was also reflected in the prevalence of deficiency. FMI was a negative determinant of s-25(OH)D in the cohort of children with obese mothers. Nevertheless, vitamin D status was not associated with bone health or blood lipids in the toddlers.
The finding of noteworthy seasonal differences in vitamin D status was likely due to fluctuations in sun-induced dermal vitamin D synthesis. This is in line with observations in other paediatric populations [6, 10, 17,18,19,20,21,22, 53], including pre-school children in Denmark, Sweden, and Ireland [11,12,13]. This indicates that deficiencies may be overlooked when vitamin D status is evaluated as a mean across the year, and should instead, or at least, be evaluated during the vitamin D winter. We hypothesised that the importance of supplement use for vitamin D status would depend on season, but even during summer months, s-25(OH)D was higher in those receiving supplements, thus supporting the new Danish recommendation of year-round supplementation to toddlers [54]. On the contrary, supplementation during summer may lead to high levels of vitamin D [55], and s-25(OH)D > 125 nmol/L was seen in four children in the present study, although this was not likely caused by the typical supplementation dose of just 10 µg/day. Further, there appeared to be larger differences between supplement users and non-users in the prevalence of deficiency and insufficiency during winter/spring than during summer/autumn, which has also been shown in previous studies among children [11, 13, 49, 50]. Thus, the results underline the importance of vitamin D supplements being particularly important for maintaining vitamin D sufficiency during the vitamin D winter at these northern latitudes, i.e. during October to March when negligible amounts of vitamin D is synthesised in the skin [1].
Our finding of a mean s-25(OH)D of 69 nmol/L and 19% having insufficiency or deficiency corresponds well with findings in other paediatric populations below the age of 6 years [2, 11, 13, 16,17,18, 22, 35, 53, 56, 57], although a lower proportion may have insufficiency at lower latitudes [2, 16, 22]. In older children, s-25(OH)D is generally lower and the prevalence of insufficiency higher [2, 5,6,7,8,9,10,11, 19, 20, 32, 50, 53, 57]. This may be due to less time spent outdoor as well as fewer supplement users among the older age groups [11, 58], as use of vitamin D supplements has been shown to be a major determinant of vitamin D status both in the present and in most observational studies and supplementation trials in children [13, 16, 19, 20, 22, 59, 60]. In our population, 2/3 of the children received vitamin D supplements, which shows that many Danish parents continued supplementing their children past the age of 2 years despite no official recommendation to do so at that time. In contrast, dietary vitamin D intake was not associated with s-25(OH)D, probably because of the low intake [4, 19, 20], which may in part be due to the fact that food fortification is rare in Denmark. In e.g. Ireland, Finland, and Canada, milk and/or other foods are commonly fortified with vitamin D, and intake of fortified milk is a major determinant of children's vitamin D status in these countries [6, 13, 22], together with season and supplement use [13, 22].
Although body composition was not a determinant of vitamin D status in the overall population, higher FMI was linked to lower s-25(OH)D in SKOT-II, where the children had higher FMI and BMI Z-score than in SKOT-I. This may indicate that adipose tissue affects vitamin D status only above a certain amount of fat mass and supports the speculated depot effect or sequestration of vitamin D in adipose tissue [61]. In line with this, a recent review in adults showed the strongest association between measures of adiposity and s-25(OH)D in persons with obesity [61]. Further, a cross-sectional analysis in Dutch children showed a 1.03 (1.01, 1.05) higher OR of s-25(OH)D < 50 nmol/L for each kg/m2 higher maternal BMI [10], and although we did not have information on maternal BMI at 3 years, the cohort-specific finding for FMI could perhaps be linked to maternal BMI. Socioeconomic differences between the cohorts could also play a role for s-25(OH)D, but we tried to minimise this potential confounding by adjusting for parental education. Vitamin D status has been shown to be higher in more physically active children [4, 6, 19, 20], but this may be due to more time spend outdoor and not PA per se, as these are usually difficult to distinguish. Time spend outdoor has indeed been related to vitamin D status in some [10, 22], although not all [4, 18] studies in pre-school and school-children. Yet, it is unclear why PA was only associated with s-25(OH)D in SKOT-II.
To our knowledge, there is no reference data for bone-related outcomes in this young age group, and it is difficult to relate DXA numbers to those of previous studies, when these are not comparable regarding both age group, type of DXA scanner, and reporting of TBLH results. However, as the included children were healthy, we expect them to have numbers within the normal range for their age group. Due to vitamin D’s known effects on calcium homeostasis [3], we hypothesised that vitamin D status would be associated with measures of bone mineralisation, as seen in some previous studies among children at different ages, who has measurements performed throughout the year or during winter [5, 7, 24, 25]. However, bone mineralisation was not associated with vitamin D status in the present study, which may be due to the year-round cross-sectional design and the low proportion (5%) of children with s-25(OH)D < 30 nmol/L, above which calcium absorption is considered sufficient by the IOM and risk of rickets is minimal [48]. Although this prevalence was higher during winter, the lower s-25(OH)D during winter may not result in health consequences when the period of deficiency is short and sufficiency is restored during summer. Further, there may be a lag from changes in vitamin D status to changes in bone mineralisation due to the rate of bone growth, and the cross-sectional design may therefore not be optimal to investigate this association. Finally, any potential haltering in bone mineralisation that may be induced during winter may be counteracted during summer. However, in a strict winter design, we recently found smaller increases in bone mineralisation of the whole body and lumbar spine when s-25(OH)D decreased during winter compared to when it was upheld among 6- to 8-year-olds [27]. Although some trials showed higher bone mineralisation after vitamin D supplementation [62, 63], the lack of association in the present study are in line with the results of other observational studies [8, 9, 21, 26] and trials [64,65,66,67,68,69,70] across the year or during winter in children of different age groups.
Vitamin D status was not associated with blood lipids in the present study. This is in contrast with our group’s previous finding that s-25(OH)D was inversely associated with total-C, HDL-C, and triacylglycerol in SKOT-I at 9 months of age [28]. However, these results were not adjusted for parental education. Comparable associations were reported in some other child populations [29,30,31], and in our recent trial, vitamin D supplementation of 20 ug/d reduced LDL-C compared to placebo [34]. Vitamin D may affect blood lipids by increasing catabolism and/or decreasing synthesis of cholesterol upon activation of the vitamin D receptor, as has been shown in rodents [71, 72]. However, numerous observational studies [33, 73, 74] and randomised trials [35,36,37] has not been able to link vitamin D and blood lipids in children and it is possible that vitamin D may not be a major regulator of blood lipids at normal blood lipid concentrations.
Strengths of our study include the investigation of determinants and associations in a broad study population of toddlers, which gave a considerable sample size and represented the general population better than either cohort alone. Further, s-25(OH)D was analysed by certified LC–MS/MS [47] and bone outcomes by DXA, which are considered the gold standard methods for assessing vitamin D status as well as BMC and areal BMD in children [75], respectively. Although parents with long education were somewhat over-represented compared to national numbers [76], all education levels were represented, and the analyses were carefully adjusted for potential confounders. Limitations of our study include the low number of acceptable DXA scans, which may have resulted in false negative findings. Further, blood samples were collected after a short fasting period, which introduces meal-dependent variation in the blood lipids. However, non-fasting mainly affects plasma triacylglycerol, not LDL and HDL cholesterol, and a longer fasting period would have been practically and ethically difficult in this age group. We had no data on current growth or growth spurts, which are likely to affect DXA results, but we conducted size-adjusted analyses. It would have been valuable to have had information about dose of supplementation and children's sun behaviour, intake of ultra-processed foods, and structured physical activity, but such data were not considered during the time of data collection, and the latter is rare in Denmark in this age group.
In conclusion, in this population of Danish toddlers, the prevalence of year-round vitamin D deficiency and insufficiency, respectively, was only 5% and 14%, but these numbers were twice as high during winter and much lower during summer. Besides season of examination, use of vitamin D supplements was a strong determinant of vitamin D status in the total population, and FMI a negative determinant in the cohort of children with obese mothers. These findings support recommendations of vitamin D supplements especially during winter in order to maintain sufficient vitamin D status among young children living at northern latitudes. However, vitamin D status was not associated with measures of bone mineralisation or blood lipids, so the clinical significance needs further investigation in randomised trials among children below 5 years of age.
Availability of data and materials
Upon request, the research data can be shared with editors and reviewers in a de-identified form for verification of the research results.
References
Cashman KD, Dowling KG, Škrabáková Z et al (2016) Vitamin D deficiency in Europe: pandemic? Am J Clin Nutr 103:1033–1044. https://doi.org/10.3945/ajcn.115.120873
Herrick KA, Storandt RJ, Afful J et al (2019) Vitamin D status in the United States, 2011–2014. Am J Clin Nutr 110:150–157. https://doi.org/10.1093/ajcn/nqz037
Braegger C, Campoy C, Colomb V et al (2013) Vitamin D in the healthy European paediatric population. J Pediatr Gastroenterol Nutr 56:692–701. https://doi.org/10.1097/MPG.0b013e31828f3c05
Mortensen C, Mølgaard C, Hauger H et al (2018) Sun behaviour and physical activity associated with autumn vitamin D status in 4–8-year-old Danish children. Public Health Nutr 21:3158–3167. https://doi.org/10.1017/S1368980018002094
Rønne MS, Heidemann M, Lylloff L et al (2019) Bone mass development in childhood and its association with physical activity and vitamin D levels The CHAMPS-Study DK. Calcif Tissue Int 104:1–13. https://doi.org/10.1007/s00223-018-0466-5
Soininen S, Eloranta A-M, Lindi V et al (2016) Determinants of serum 25-hydroxyvitamin D concentration in Finnish children: the physical activity and nutrition in children (PANIC) study. Br J Nutr 115:1080–1091. https://doi.org/10.1017/S0007114515005292
Pekkinen M, Viljakainen H, Saarnio E et al (2012) Vitamin D is a major determinant of bone mineral density at school age. PLoS ONE 7:e40090. https://doi.org/10.1371/journal.pone.0040090
Hauksson HH, Hrafnkelsson H, Magnusson KT et al (2016) Vitamin D status of Icelandic children and its influence on bone accrual. J Bone Miner Metab 34:580–586. https://doi.org/10.1007/s00774-015-0704-0
Videhult FK, Öhlund I, Hernell O, West CE (2016) Body mass but not vitamin D status is associated with bone mineral content and density in young school children in northern Sweden. Food Nutr Res. https://doi.org/10.3402/fnr.v60.30045
Voortman T, van den Hooven EH, Heijboer AC et al (2015) Vitamin D deficiency in school-age children is associated with sociodemographic and lifestyle factors. J Nutr 145:791–798. https://doi.org/10.3945/jn.114.208280
Hansen L, Tjønneland A, Køster B et al (2018) Vitamin D status and seasonal variation among Danish children and adults: a descriptive study. Nutrients 10:1801. https://doi.org/10.3390/nu10111801
Öhlund I, Silfverdal S-A, Hernell O, Lind T (2013) Serum 25-hydroxyvitamin D levels in preschool-age children in northern Sweden are inadequate after summer and diminish further during winter. J Pediatr Gastroenterol Nutr 56:551–555. https://doi.org/10.1097/MPG.0b013e3182838e5b
ní Chaoimh C, McCarthy EK, Hourihane JO et al (2018) Low vitamin D deficiency in Irish toddlers despite northerly latitude and a high prevalence of inadequate intakes. Eur J Nutr 57:783–794. https://doi.org/10.1007/s00394-016-1368-9
Nordic Council of Ministers (2014) Vitamin D. Nordic nutrition recommendations integrating nutrition and physical activity, 5th edn. norden, Copenhagen, pp 349–384
Pedersen AN, Christensen T, Matthiessen J et al (2015) Dietary habits in Denmark 2011–2013. Main results. DTU Fødevareinstituttet, Afdeling for Ernæring, Søborg
El Hayek J, Pham TT, Finch S et al (2013) Vitamin D status in Montréal preschoolers is satisfactory despite low vitamin D intake. J Nutr 143:154–160. https://doi.org/10.3945/jn.112.169144
Zhou SJ, Skeaff M, Makrides M, Gibson R (2015) Vitamin D status and its predictors among pre-school children in Adelaide. J Paediatr Child Health 51:614–619. https://doi.org/10.1111/jpc.12770
Carpenter TO, Herreros F, Zhang JH et al (2012) Demographic, dietary, and biochemical determinants of vitamin D status in inner-city children. Am J Clin Nutr 95:137–146. https://doi.org/10.3945/ajcn.111.018721
Absoud M, Cummins C, Lim MJ et al (2011) Prevalence and predictors of vitamin d insufficiency in children: a great Britain population based study. PLoS ONE 6:e22179. https://doi.org/10.1371/journal.pone.0022179
Petersen RA, Damsgaard CT, Dalskov S-M et al (2016) Vitamin D status and its determinants during autumn in children at northern latitudes: a cross-sectional analysis from the optimal well-being, development and health for Danish children through a healthy new Nordic diet (OPUS) school meal study. Br J Nutr 115:239–250. https://doi.org/10.1017/S000711451500433X
Stein EM, Laing EM, Hall DB et al (2006) Serum 25-hydroxyvitamin D concentrations in girls aged 4–8 y living in the southeastern United States. Am J Clin Nutr 83:75–81. https://doi.org/10.1093/ajcn/83.1.75
Maguire JL, Birken CS, Khovratovich M et al (2013) Modifiable determinants of serum 25-hydroxyvitamin D status in early childhood: opportunities for prevention. JAMA Pediatr 167:230. https://doi.org/10.1001/2013.jamapediatrics.226
Rodríguez-Rodríguez E, Navia-Lombán B, López-Sobaler AM, Ortega RM (2010) Associations between abdominal fat and body mass index on vitamin D status in a group of Spanish schoolchildren. Eur J Clin Nutr 64:461–467. https://doi.org/10.1038/ejcn.2010.26
Hazell TJ, Pham TT, Jean-Philippe S et al (2015) Vitamin D status is associated with bone mineral density and bone mineral content in preschool-aged children. J Clin Densitom Off J Int Soc Clin Densitom 18:60–67. https://doi.org/10.1016/j.jocd.2014.04.121
Constable AM, Vlachopoulos D, Barker AR et al (2021) The independent and interactive associations of physical activity intensity and vitamin D status with bone mineral density in prepubertal children: the PANIC Study. Osteoporos Int. https://doi.org/10.1007/s00198-021-05872-z
White Z, White S, Dalvie T et al (2019) Bone health, body composition, and vitamin D status of black preadolescent children in South Africa. Nutrients 11:1243. https://doi.org/10.3390/nu11061243
Stounbjerg NG, Thams L, Hansen M et al (2021) Effects of vitamin D and high dairy protein intake on bone mineralization and linear growth in 6 to 8-year-old children: the D-pro randomized trial. Am J Clin Nutr 114:1971–1985. https://doi.org/10.1093/ajcn/nqab286
Arnberg K, Østergård M, Madsen AL et al (2011) Associations between vitamin D status in infants and blood lipids, body mass index and waist circumference. Acta Paediatr 100:1244–1248. https://doi.org/10.1111/j.1651-2227.2011.02273.x
Birken CS, Lebovic G, Anderson LN et al (2015) Association between Vitamin D and circulating lipids in early childhood. PLoS ONE 10:e0131938. https://doi.org/10.1371/journal.pone.0131938
Pacifico L, Anania C, Osborn JF et al (2011) Low 25(OH)D3 levels are associated with total adiposity, metabolic syndrome, and hypertension in Caucasian children and adolescents. Eur J Endocrinol 165:603–611. https://doi.org/10.1530/EJE-11-0545
Petersen RA, Dalskov S-M, Sørensen LB et al (2015) Vitamin D status is associated with cardiometabolic markers in 8–11-year-old children, independently of body fat and physical activity. Br J Nutr 114:1647–1655. https://doi.org/10.1017/S0007114515003372
Rodríguez-Rodríguez E, Ortega RM, González-Rodríguez LG et al (2011) Vitamin D deficiency is an independent predictor of elevated triglycerides in Spanish school children. Eur J Nutr 50:373–378. https://doi.org/10.1007/s00394-010-0145-4
Dolinsky DH, Armstrong S, Mangarelli C, Kemper AR (2013) The association between vitamin D and cardiometabolic risk factors in children: a systematic review. Clin Pediatr (Phila) 52:210–223. https://doi.org/10.1177/0009922812470742
Thams L, Stounbjerg NG, Hvid LG et al (2022) Effects of high dairy protein intake and vitamin D supplementation on body composition and cardiometabolic markers in 6–8-y-old children—the D-pro trial. Am J Clin Nutr. https://doi.org/10.1093/ajcn/nqab424
Öhlund I, Lind T, Hernell O et al (2020) Vitamin D status and cardiometabolic risk markers in young Swedish children: a double-blind randomized clinical trial comparing different doses of vitamin D supplements. Am J Clin Nutr 111:779–786. https://doi.org/10.1093/ajcn/nqaa031
Rajakumar K, Moore CG, Khalid AT et al (2020) Effect of vitamin D3 supplementation on vascular and metabolic health of vitamin D–deficient overweight and obese children: a randomized clinical trial. Am J Clin Nutr 111:757–768. https://doi.org/10.1093/ajcn/nqz340
Hauger H, Laursen RP, Ritz C et al (2020) Effects of vitamin D supplementation on cardiometabolic outcomes in children and adolescents: a systematic review and meta-analysis of randomized controlled trials. Eur J Nutr 59:873–884. https://doi.org/10.1007/s00394-019-02150-x
Madsen AL, Schack-Nielsen L, Larnkjær A et al (2010) Determinants of blood glucose and insulin in healthy 9-month-old term Danish infants; the SKOT cohort. Diabet Med 27:1350–1357. https://doi.org/10.1111/j.1464-5491.2010.03134.x
Andersen LBB, Pipper CB, Trolle E et al (2015) Maternal obesity and offspring dietary patterns at 9 months of age. Eur J Clin Nutr 69:668–675. https://doi.org/10.1038/ejcn.2014.258
Renault KM, Nørgaard K, Nilas L et al (2014) The treatment of obese pregnant women (TOP) study: a randomized controlled trial of the effect of physical activity intervention assessed by pedometer with or without dietary intervention in obese pregnant women. Am J Obstet Gynecol 210:134.e1–9. https://doi.org/10.1016/j.ajog.2013.09.029
Gondolf UH, Tetens I, Hills AP et al (2012) Validation of a pre-coded food record for infants and young children. Eur J Clin Nutr 66:91–96. https://doi.org/10.1038/ejcn.2011.133
Fødevaredata (frida.fooddata.dk) (2019) version 4, 2019. In: Fødevareinstituttet Dan. Tek. Univ. https://frida.fooddata.dk/. Accessed 30 Apr 2019
Møller NC, Christensen LB, Mølgaard C et al (2017) Descriptive analysis of preschool physical activity and sedentary behaviors–a cross sectional study of 3-year-olds nested in the SKOT cohort. BMC Public Health 17:613. https://doi.org/10.1186/s12889-017-4521-3
Schnurr TM, Viitasalo A, Eloranta A-M et al (2018) Genetic predisposition to adiposity is associated with increased objectively assessed sedentary time in young children. Int J Obes 42:111–114. https://doi.org/10.1038/ijo.2017.235
Jensen SM, Mølgaard C, Ejlerskov KT et al (2012) Validity of anthropometric measurements to assess body composition, including muscle mass, in 3-year-old children from the SKOT cohort. Matern Child Nutr 11:398–408. https://doi.org/10.1111/mcn.12013
Ejlerskov KT, Jensen SM, Christensen LB et al (2014) Prediction of fat-free body mass from bioelectrical impedance and anthropometry among 3-year-old children using DXA. Sci Rep. https://doi.org/10.1038/srep03889
Cashman KD, Kiely M, Kinsella M et al (2013) Evaluation of Vitamin D Standardization Program protocols for standardizing serum 25-hydroxyvitamin D data: a case study of the program’s potential for national nutrition and health surveys. Am J Clin Nutr 97:1235–1242. https://doi.org/10.3945/ajcn.112.057182
Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium (2011) Dietary reference intakes for adequacy: calcium and vitamin D. In: Ross AC, Taylor CL, Yaktine AL, Valle HBD (eds) Dietary reference intakes for calcium and vitamin D. National Academies Press, Washington, DC
Davies PSW, Bates CJ, Cole TJ et al (1999) Vitamin D: seasonal and regional differences in preschool children in Great Britain. Eur J Clin Nutr 53:195–198. https://doi.org/10.1038/sj.ejcn.1600697
Thorisdottir B, Gunnarsdottir I, Steingrimsdottir L et al (2016) Vitamin D intake and status in 6-year-old Icelandic children followed up from infancy. Nutrients. https://doi.org/10.3390/nu8020075
Prentice A, Parsons TJ, Cole TJ (1994) Uncritical use of bone mineral density in absorptiometry may lead to size-related artifacts in the identification of bone mineral determinants. Am J Clin Nutr 60:837–842. https://doi.org/10.1093/ajcn/60.6.837
Madsen MTB, Biltoft-Jensen AP, Trolle E et al (2022) Wholegrain intake, growth and metabolic markers in Danish infants and toddlers: a longitudinal study. Eur J Nutr. https://doi.org/10.1007/s00394-022-02902-2
Bates B, Lennox A, Prentice A et al (2014) National diet and nutrition survey results from years 1, 2, 3 and 4 (combined) of the rolling programme (2008/2009–2011/2012). Public Health England Food Standards Agency, London, UK
Fødevarestyrelsen D-vitamin (2022) In: ALT OM KOST. https://altomkost.dk/fakta/naeringsindhold-i-maden/d-vitamin/. Accessed 7 Jan 2022
Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium (2011) Tolerable upper intake levels: calcium and vitamin D. In: Ross AC, Taylor CL, Yaktine AL, Valle HBD (eds) Dietary reference intakes for calcium and vitamin D. National Academies Press, Washington, DC
Rabenberg M, Scheidt-Nave C, Busch MA et al (2018) Implications of standardization of serum 25-hydroxyvitamin D data for the evaluation of vitamin D status in Germany, including a temporal analysis. BMC Public Health 18:845. https://doi.org/10.1186/s12889-018-5769-y
Mansbach JM, Ginde AA, Camargo CA (2009) Serum 25-Hydroxyvitamin D levels among US children aged 1 to 11 years: do children need more vitamin D? Pediatrics 124:1404–1410. https://doi.org/10.1542/peds.2008-2041
Kyttälä P, Erkkola M, Kronberg-Kippilä C et al (2010) Food consumption and nutrient intake in Finnish 1–6-year-old children. Public Health Nutr 13:947–956. https://doi.org/10.1017/S136898001000114X
Lamberg-Allardt C, Brustad M, Meyer HE, Steingrimsdottir L (2013) Vitamin D–a systematic literature review for the of the 5th edition Nordic nutrition recommendations. Food Nutr Res 57:22671. https://doi.org/10.3402/fnr.v57i0.22671
Brett NR, Gharibeh N, Weiler HA (2018) Effect of vitamin D supplementation, food fortification, or bolus injection on vitamin d status in children aged 2–18 years: a meta-analysis. Adv Nutr 9:454–464. https://doi.org/10.1093/advances/nmy012
Karampela I, Sakelliou A, Vallianou N et al (2021) Vitamin D and obesity: current evidence and controversies. Curr Obes Rep 10:162–180. https://doi.org/10.1007/s13679-021-00433-1
Viljakainen HT, Natri A-M, Kärkkäinen M et al (2006) A positive dose-response effect of vitamin d supplementation on site-specific bone mineral augmentation in adolescent girls: a double-blinded randomized placebo-controlled 1-year intervention. J Bone Miner Res 21:836–844. https://doi.org/10.1359/jbmr.060302
El-Hajj Fuleihan G, Nabulsi M, Tamim H et al (2006) Effect of vitamin D replacement on musculoskeletal parameters in school children: a randomized controlled trial. J Clin Endocrinol Metab 91:405–412. https://doi.org/10.1210/jc.2005-1436
Du X, Zhu K, Trube A et al (2004) School-milk intervention trial enhances growth and bone mineral accretion in Chinese girls aged 10–12 years in Beijing. Br J Nutr 92:159–168. https://doi.org/10.1079/BJN20041118
El-Hajj Fuleihan G, Vieth R (2007) Vitamin D insufficiency and musculoskeletal health in children and adolescents. Int Congr Ser 1297:91–108. https://doi.org/10.1016/j.ics.2006.09.019
Cheng S, Lyytikäinen A, Kröger H et al (2005) Effects of calcium, dairy product, and vitamin D supplementation on bone mass accrual and body composition in 10–12-y-old girls: a 2-y randomized trial. Am J Clin Nutr 82:1115–1126. https://doi.org/10.1093/ajcn/82.5.1115
Andersen R, Mølgaard C, Skovgaard LT et al (2008) Effect of vitamin D supplementation on bone and vitamin D status among Pakistani immigrants in Denmark: a randomised double-blinded placebo-controlled intervention study. Br J Nutr 100:197–207. https://doi.org/10.1017/S000711450789430X
Mølgaard C, Larnkjær A, Cashman KD et al (2010) Does vitamin D supplementation of healthy Danish Caucasian girls affect bone turnover and bone mineralization? Bone 46:432–439. https://doi.org/10.1016/j.bone.2009.08.056
Brett NR, Parks CA, Lavery P et al (2018) Vitamin D status and functional health outcomes in children aged 2–8 y: a 6-mo vitamin D randomized controlled trial. Am J Clin Nutr 107:355–364. https://doi.org/10.1093/ajcn/nqx062
Åkeson PK, Åkesson KE, Lind T et al (2018) Vitamin D intervention and bone: a randomized clinical trial in fair and dark-skinned children at northern latitudes. J Pediatr Gastroenterol Nutr 67:388–394. https://doi.org/10.1097/MPG.0000000000002031
Gonzalez FJ, Moschetta A (2014) Potential role of the vitamin D receptor in control of cholesterol levels. Gastroenterology 146:899–902. https://doi.org/10.1053/j.gastro.2014.02.022
Li S, He Y, Lin S et al (2016) Increase of circulating cholesterol in vitamin D deficiency is linked to reduced vitamin D receptor activity via the Insig-2/SREBP-2 pathway. Mol Nutr Food Res 60:798–809. https://doi.org/10.1002/mnfr.201500425
Hauger H, Mølgaard C, Mortensen C et al (2018) Winter cholecalciferol supplementation at 55°N has no effect on markers of cardiometabolic risk in healthy children aged 4–8 years. J Nutr 148:1261–1268. https://doi.org/10.1093/jn/nxy080
Smith TJ, Tripkovic L, Hauger H et al (2018) Winter cholecalciferol supplementation at 51°N Has no effect on markers of cardiometabolic risk in healthy adolescents aged 14–18 years. J Nutr 148:1269–1275. https://doi.org/10.1093/jn/nxy079
ISCD (2019) 2019 ISCD official pediatric positions: skeletal health assessment in children from infancy to adolescence. The International Society for Clinical Densitometry, Connecticut, USA
Danmarks Statistik Befolkningens højst fuldførte uddannelse (2022) In: Dan. Stat. https://www.dst.dk/da/Statistik/emner/uddannelse-og-forskning/befolkningens-uddannelsesstatus/befolkningens-hoejst-fuldfoerte-uddannelse. Accessed 14 Feb 2022
Acknowledgements
We thank the participating children, families, and project staff of the SKOT cohorts.
Funding
The SKOT-I cohort was funded by The Directorate for Food, Fisheries and Agri Business as part of the project “Complementary and young child feeding–impact on short and long term development and health.” The SKOT-II cohort was supported by grants from the Aase and Ejnar Danielsens Foundation and the Augustinus Foundation to KFM. The work also received support from Arla Food for Health.
Author information
Authors and Affiliations
Contributions
NGS formulated the research questions, analysed the data, interpreted the findings, and wrote the paper; CM interpreted the findings; KDC analysed and interpreted s-25(OH) D; KFM designed the study and interpreted the findings; CTD formulated the research questions, interpreted the findings, and helped revise the manuscript. All authors reviewed, provided input to, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The studies were conducted in accordance with the Declaration of Helsinki and approved by The Committees on Biomedical Research Ethics for the Capital Region of Denmark: SKOT I: H-KF-2007–0003; SKOT II: H-3–2010-122.
Informed consent
Written informed consent was obtained from all custody holders of the children.
Study registration
The studies were registered at clinicaltrials.gov as NCT02170428 and NCT02377973.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stounbjerg, N.G., Mølgaard, C., Cashman, K.D. et al. Vitamin D status of 3-year-old children in Denmark: determinants and associations with bone mineralisation and blood lipids. Eur J Nutr 62, 1441–1451 (2023). https://doi.org/10.1007/s00394-023-03084-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-023-03084-1