Abstract
This longitudinal study examined associations of bone mass with physical activity and vitamin D level over more than 6 years through puberty. A total of 663 participants (320 boys) with mean age 9.6 years at baseline (10–17 years at follow-up), underwent dual energy X-ray absorptiometry, anthropometry and blood samples for vitamin D at least twice during the study period (with three possible time-points). Physical activity was assessed using accelerometers at follow-up. A positive association was found between percent time spent at vigorous physical activity and total-body less head bone mineral content (β = 5.8, p = 0.002). The magnitude of this association increased with maturational development; thus physical activity may have a greater influence on bone mass in the more mature participants. The vitamin D levels were also positively associated with bone mass. A high degree of tracking was observed with changes in anthropometric Z scores predictive of deviation from tracking. No environmental factor predicted deviation from tracking.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prevention of bone loss and eventual osteoporosis becomes more relevant as expected life spans increase in the Western World [1]. The attainment of a higher peak bone mass may thus be important, as it could delay the onset of osteoporosis for several years [2].
High-impact physical activity, especially jumping activities, improves bone mass development in childhood and adolescence [3, 4]. Whether the effect of physical activity (PA) on bone mass development is modulated by maturational development remains under debate. Mackelvie et al. [5] and Meyer et al. [6] both examined whether pre-puberty was a more ideal time than early puberty to improve bone mass with PA and found opposite results. However, they did not include participants in late puberty. Studies including participants in late puberty [7,8,9] reported diverse results. Lappe et al. [7] and Janz et al. [8] found no overall interaction between PA and maturity on bone mass, although Lappe et al. reported an interaction between Tanner-stage and PA in a subgroup of non-black boys, and Heinonen et al. [9] reported exercise to be more beneficial for the bones in girls before menarche than after menarche.
Vitamin D also plays a pivotal role in bone health during childhood and adolescence [10]. However, a meta-analysis by Winzenberg et al. [11] found that supplementation may not necessarily improve bone mass in children with vitamin D at a sufficient level but potentially in Vitamin D deficient children. Cross-sectional studies have produced diverse results regarding the association between the vitamin D level and bone mass in children and young adults, ranging from a negative or no association [12] to a positive association [13,14,15,16]. Moreover, one group observed an association only in girls [17], another found that the association was most consistent in boys [18], and Pekkinen et al. [13] claimed that the strength of the association surpassed that of PA with bone mass. Furthermore, two studies [19, 20] reported interaction between the vitamin D level and PA in adolescence that affected bone mass. Data from longitudinal studies are sparse and equally diverse [21, 22]. Thus, much uncertainty persists regarding the relationship between vitamin D levels and bone mass.
The stability of bone mass, adjusted for age and sex, during growth is known as tracking, and is described in childhood and adolescence [4]. Two studies [23, 24] showed that PA in childhood and adolescence may be associated with positive deviation from tracking, and another study [25] showed that deviation in height growth status was associated with deviation from bone mass tracking. To our knowledge, no study has evaluated whether the vitamin D level is associated with deviation from bone mass tracking.
In this study, we thus sought to: (1) examine associations between bone mass development and maturity, PA, and vitamin D levels, as well as potential interactions; and (2) elucidate the associations of tracking over more than 6 years in bone mass with PA, and vitamin D levels, as well as their potential interaction.
Methods
Study Design
The Childhood Health Activity and Motor Performance School Study, Denmark (CHAMPS-study DK) is a longitudinal cohort study originating from a non-randomised intervention study conducted from 2008 to 2015. A population-based sample of children aged 6–11 years from 10 schools in the municipality of Svendborg was recruited at baseline in 2008. The study has been described in detail elsewhere [26]. The intervention consisted of adding 180 min physical education per week (in total 270 min per week) and was implemented at six schools in 2008 [26, 27]. These schools were matched with four control schools (with 90 min physical education per school week). The extra physical education was discontinued after grade 6, whereupon all schools continued as the control schools.
This sub-study included the oldest part of the cohort, consisting of children aged 8–11 years (2nd–4th grade) at baseline. Participants with chronic illness known to affect bone development (diabetes mellitus and bone disease) were excluded from the final analyses. Participants with metal in the body and those taller than 195 cm (the scanner limit) were excluded from tests conducted in 2015.
Dual Energy X-ray Absorptiometry
Whole-body dual energy X-ray absorptiometry (DXA) scans were performed in autumn/winter 2008/2009, autumn/winter 2010/2011 and spring 2015. All DXA-scans were conducted using the same GE Lunar Prodigy DXA scanner with enCORE software (version 15; GE Medical Systems, Madison, WI, USA) at Hans Christian Andersen Children’s Hospital, Odense University Hospital, Denmark. All scans were performed by three operators (two at each time-point) and analysed by two persons (MSR and MH). Total-body less head (TBLH) values were used for bone mineral content (BMC), areal bone mineral density (aBMD) and bone area (BA), together with whole-body percent lean mass (%LM).
During the scan, each participant was covered by a thin blanket and was wearing undergarments, stockings and a thin T-shirt. The scan depth was automatically altered based on the child’s age, height and weight.
Every morning, the reproducibility and precision of the scanner were tested with repeated scans of a phantom according to the manufacturer’s standardised operational procedures. The coefficient of variation for phantom aBMD during the whole study period was 0.27–0.33%.
Anthropometry and Sexual Maturation
Before DXA, height was measured to the nearest 0.1 cm with a portable stadiometer (SECA 213) and weight was measured to the nearest 0.1 kg on an electronic scale (SECA 861) (both SECA GmbH & Co. KG, Hamburg, Germany).
Sexual maturation was predicted using the equations provided by Moore et al. [28], with calculation of expected age at peak height velocity (APHV). The height measurement nearest in time to the predicted APHV was used for the calculation for children with repeated measurements. A continuous measure of maturity was calculated by subtracting the APHV from the participant’s chronological age (with − 1 corresponding to 1 year prior to APHV) [28].
Physical Activity
PA was assessed objectively by GT3X and GT3X+ accelerometers (ActiGraph, Pensacola, FL, USA) at four time-points [2009, 2010, 2012 (autumn/winter) and 2015 (spring)].
The accelerometers were programmed to start recording the day after distribution and were collected after at least 7 consecutive days of wear. Data from 06:00 to 23:00 (to 24:00 in 2015) were included. Participants were given written and visual instructions to wear the device on the right hip and to remove it only for aquatic activities, showering and night-time sleep. To distinguish between true and false intervals of inactivity, we interpreted all consecutive strings of 0 counts spanning ≥ 30 min as “accelerometer not worn” and these strings were removed from the data. The accelerometers were programmed to store data every 2 s (GT3X) and at 30 Hz (GT3X+). We subsequently collapsed recordings into 10 s epochs for analysis, as in previous sub-studies of the CHAMPS-study DK [29, 30]. Data were considered to be acceptable when they covered a minimum of 3 days, with at least 10 h valid recording per day after removal of non-wear time. Data outputs from the accelerometers were analysed using customised software (Propero version 1.7.4; University of Southern Denmark, Odense, Denmark). Accelerometer recordings were coded into four intensity domains using accelerometer counts per minute as sedentary (< 100), light physical activity (100–2295), moderate to vigorous physical activity (MVPA; ≥ 2296) and vigorous physical activity (VPA; ≥ 4012) with count cut-offs adapted to match the 10 s epochs. The intensity classification algorithm is based on cut-off points that showed excellent sensitivity and specificity against indirect calorimetry in an external validation sample [31]. The percentages of wear time spent in the intensity domains were used in the analysis.
In analyses of tracking, data on PA exposure from each time-point were averaged. Before the calculation of cumulative average PA exposure, data from 2009 to 2010 were averaged to avoid giving overly high weights to the first assessment rounds. For each participant, valid data from at least two of the three potential time-points (2009/2010, 2012, and 2015) were required to be included in the cumulative average.
Laboratory Analyses
Blood samples were collected between 08:00 and 12.00 and processed and stored within 4 h. The samples were kept frozen at − 80 °C, but were transferred to a − 20 °C freezer for a maximum of 2 months prior to analysis. Serum 25-hydroxy-vitamin D3 + D2 (vitamin D) was measured on a Cobas e411 device using the 25-OH-vitamin D, chemiluminescence assay (Roche Diagnostics, Basel, Switzerland) at the Department of Clinical Biochemistry, Glostrup, Rigshospitalet, Denmark. The intermediary precisions of the assay, expressed as coefficients of variation, are 10% (50 nmol/l) and 7.5% (90 nmol/l).
Vitamin D levels were measured in different seasons (autumn in 2008 and 2010, spring in 2015). To reduce the influence of seasonal variation, internal age- and sex-adjusted Z scores were calculated for post hoc analysis (as autumn measurements with generally higher vitamin D levels were from the youngest children (< 14 years) whereas spring measurements were from the oldest children (> 14 years)).
An average vitamin D level over the whole study period was calculated for each participant (only participants with at least two of three possible measurements available were included). This average vitamin D level was used only for the tracking analysis.
Statistical Analyses
p values less than 0.05 were considered to be significant, and results are presented with 95% confidence intervals (CI).
All statistical analyses are conducted using STATA/IC 14.2 software (StataCorp LP, College Station, TX, USA).
Internally derived age- and sex-adjusted Z scores were calculated for TBLH BMC, TBLH aBMD, TBLH BA, height, weight, %LM and vitamin D level.
Unpaired t tests were used to examine differences between sexes and between participants attending control and intervention schools (stratified by sex and year of DXA-scan).
Associations Between Bone Mass and Explanatory Variables
Linear mixed-effect models were fitted to examine the associations between TBLH BMC at follow-ups (2-years and last follow-up) and explanatory variables measured at follow-ups (PA and vitamin D level), adjusted for maturity, sex, size (height, TBLH BA), body composition (weight, %LM) and baseline TBLH BMC. As maturity may influence bone development differently in boys and girls, a maturity-by-sex interaction term was added to the models.
Given the high degree of collinearity between age and maturity, only maturity was used in the models.
As the study involved repeated measures on the same individuals and different schools and classes, the models were built as random intercept models with the schools, classes, and unique participant identification numbers serving as random effects.
Comparable models were built for TBLH aBMD and TBLH BA, except that TBLH BA was not included as size-adjusting variable.
After fitting the models, the STATA margins command was used to plot predicted values of TBLH BMC and PA depending on maturity and sex.
Tracking Analyses
Participants who underwent DXA-scan at baseline and in 2015 were divided into quintiles according to their respective Z scores at baseline and in 2015. The change in quintile over the follow-up time was calculated for each participant (change score), and five groups were defined based on change scores (≤ − 2, − 1, 0, 1, ≥ 2) and compared according to means of explanatory variables in each group. Differences between groups were analysed using mixed-effect models, taking into account school- and class-clustering as random effects.
A basic mixed-effect model was also built with the TBLH BMC Z score at follow-up serving as the outcome and the TBLH BMC Z score at baseline serving as the independent variable, with additional adjustment for sex, maturity, changes in Z scores of height, weight, and %LM and baseline Z score-level (for height, weight and %LM). After fitting, this model was extended to address the objectives by adding averages of explanatory variables (VPA and vitamin D level) as well as vitamin D levels measured at each time-point. The clustering of data in schools and classes was handled as random effects.
Ethical Considerations
Participating children and their parents received written information about the study together with verbal information at school meetings. Parents provided written informed consent before enrolment of their children in the study. For all children, participation was voluntary and consent could be withdrawn at any time. The CHAMPS-study DK was approved by the Regional Scientific Ethical Committee of Southern Denmark (Project IDs: S2008-0047, S-20140105).
Results
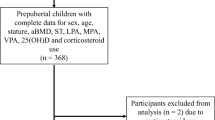
At baseline, 713 participants underwent DXA scanning. Of these, 663 participants (320 boys) underwent at least one follow-up scan (190 participants underwent DXA-scan at all three time-points), and their data were included in analyses. In total, 1516 DXA-scans were included in analyses. Three participants were excluded from final analyses due to chronic illness. Data on PA were missing for 41 participants, and data on vitamin D level were missing for 156 participants.
At baseline, the mean age was 9.6 years, equal for boys and girls. Other characteristics are shown in Table 1.
Vitamin D levels measured in the spring (2015) were generally lower than levels measured in the autumn (2008 and 2010). In 2015, 9% (n = 15) of participants were vitamin D deficient (< 30 nmol/l) and 52% (n = 88) had insufficient vitamin D (≤ 50 nmol/l)). In 2008, only 3% (n = 15) of participants had vitamin D insufficiency (≤ 50 nmol/l) (cut-off levels by Munns et al. [32]).
No significant difference in study characteristics (TBLH BMC, TBLH aBMD, TBLH BA, height, weight, %LM, vitamin D, MVPA and VPA) was detected between participants attending control and intervention schools (data not shown). Hence, intervention status was not included as a covariate in the analyses.
A high drop-out was observed during the study with the majority from the oldest participants. The 194 participants measured both at baseline and follow-up were compared on baseline Z scores for key variables with those lost to follow-up during the study. The difference in average Z scores between the two groups for girls/boys, respectively, were: height 0.04, p = 0.71/0.22, p = 0.06, weight 0.18, p = 0.11/0.26, p = 0.02, TBLH BMC 0.14, p = 0.25/0.21, p = 0.06, %LM 0.19, p = 0.09/0.17, p = 0.14, vitamin D 0.26, p = 0.05/0.22, p = 0.09.
Associations with TBLH BMC
A significant association between TBLH BMC and maturity was found in all models, and the maturity-by-sex interaction term showed an additional benefit of maturity on bone mass in boys (p < 0.001; Table 2).
Percent time spent at VPA was associated positively with TBLH BMC (in g) (βVPA = 5.8, p = 0.002). The magnitude of this positive association increased with the progression of maturational development (βinteraction-VPA-by-maturity = 1.8, p = 0.034; Fig. 1).
Percent time spent at MVPA was analysed by replacing VPA with MVPA in model 2, which showed a possible (but not significant) positive association with TBLH BMC (βMVPA = 0.18, p = 0.101).
The vitamin D level (in nmol/l) was also positively associated with TBLH BMC (βvitaminD = 0.3, p = 0.039).
Vitamin D level was replaced with vitamin D Z scores in model 3 to partly adjust for seasonality; this post hoc analysis confirmed the positive association between vitamin D and TBLH BMC (βvitaminDZ−score = 8.1, p = 0.011).
No interaction between the vitamin D level and VPA was found to be associated with TBLH BMC.
Associations with TBLH aBMD and TBLH BA
TBLH aBMD and TBLH BA were analysed with the same models (with no adjustment for TBLH BA) and with the interaction term between maturity and sex omitted, as it was not significant in any model.
Percent time at VPA was positively associated with TBLH aBMD (in g/cm2) (βVPA = 0.002, p = 0.004) and the VPA-by-maturity interaction term yielded a significant positive result (βinteraction-VPA-by-maturity = 0.0007, p = 0.039). In contrast, the vitamin D level and its interaction with VPA showed no association with TBLH aBMD.
TBLH BA (in cm2) and vitamin D levels in nmol/l were almost significantly negatively associated (βvitamin D = − 0.25, p = 0.051). VPA and its interaction with vitamin D level showed no association with TBLH BA.
Tracking of TBLH BMC
A high degree of tracking was found in comparison of baseline and follow-up TBLH BMC Z scores (Pearson correlation, R = 0.81 (CI 0.76–0.85); Fig. 2).
Table 3 shows the characteristics of the five groups according to changes in TBLH BMC Z score quintiles over more than 6 years. All groups had different changes in height- and weight Z scores compared with the reference group (no BMC quintile change; all p < 0.001). The reference group had a mean positive change in height Z score of 0.27, whereas a negative change in height Z score was observed for participants who shifted to a lower BMC quintile during the study period and a positive change in height Z score was observed for those who shifted to a higher BMC quintile. The same pattern was evident for changes in weight Z score (Table 3).
The percentage of time spent engaging in VPA in 2009, 2010, 2012 and 2015 did not differ significantly between groups (data not shown). The cumulative average of VPA, average vitamin D level and vitamin D level in 2008 and 2010 also did not differ. Vitamin D levels in 2015 were higher in participants with change scores of 1 compared with participants with no BMC quintile change.
Analysed with mixed-effect models (adjusted for baseline levels, sex and maturity) positive changes in Z scores of height, weight and %LM were associated positively with deviation from tracking with high significance for all models (Table 4).
A positive non-significant association was found for percent time spent at VPA (average over the whole period) and deviation from tracking (β = 0.04, p = 0.101).
The vitamin D levels and vitamin D Z scores averaged for the whole study period did not predict deviation from tracking of TBLH BMC and nor did vitamin D levels measured at single time-points.
Discussion
This study revealed a positive association between VPA and TBLH BMC in childhood and adolescence. This association was influenced by maturational development, with the magnitude of the regression coefficient increasing with maturity. Thus VPA may be more important for bone mass in late puberty, where the adolescents, on the other hand, may tend to be less active [33]. The vitamin D level was associated positively with TBLH BMC and, although vitamin D is an essential micronutrient regarding bone health, no interaction between VPA and the vitamin D level with bone variables was observed.
Positive changes in Z scores of height, weight and %LM were associated with positive deviation from tracking of TBLH BMC, whereas neither VPA nor the vitamin D level was found to predict deviation from tracking.
Puberty is an important period for skeletal development; approximately 40% of peak bone mass is achieved in the 4 years surrounding the peak in bone growth [4] (around 12.4 years of age in girls and 14 years of age in boys (non-African American) [34]). This period of rapid bone accrual coincides with the age of this study population (10–17 years) and may explain the association observed between maturity and TBLH BMC, dependent on sex.
The greater increase in bone mass in boys than in girls during puberty can be explained partly by larger gains in stature and body weight in boys, but developmental differences caused by sexual hormones remain after adjustment for body size. However, girls are more mature at the time for follow-up than boys although at the same chronological age, which may have influenced the results. Even examined at the same maturational stage sex-differences have also been reported by Bailey et al. [35] who found greater bone mass in boys than in girls 1 year after PHV, but the exact nature of the interaction between sex and maturity remains incompletely understood.
VPA
VPA was positively associated with TBLH BMC whereas MVPA was not associated significantly with TBLH BMC, possibly because lower-intensity exercise has a lesser osteogenic effect. Similarly, Janz et al. [8] found that VPA was associated more consistently with greater BMC than MVPA. The amount of time spent engaging in VPA and MVPA was markedly greater among boys than among girls throughout the study period, as reported by others [8, 36]. The positive association between VPA and TBLH BMC and the higher level of VPA in boys may also have contributed to the increased bone mass seen in boys compared with girls.
Of note, the association between VPA and TBLH BMC increased with maturity in 10–17-year-old children in this study. Few studies have evaluated the interaction between PA and maturational development and reported diverse results. Two studies showed no overall interaction between maturational development and PA on bone mass [7, 8], although Lappe et al. [7] found different effects of PA according to Tanner-stage in a subgroup of non-black boys. However, others reported either pre-pubertal stage [6] or early pubertal stage to be the most opportune period to improve bone mass through PA [5, 9] but with different cohorts and definitions of maturational development challenging the comparison between studies. Although Meyer et al. [6] reported the pre-pubertal period to be the most opportune period for improving bone mass through PA, they did not include participants more mature than Tanner-stage 3 and the results cannot be generalised to older adolescents. Heinonen et al. [9] included girls from Tanner-stage 1 to 5 and compared the difference in increased BMC between trainees and controls and reported a higher effect of exercise intervention in girls before menarche than after menarche at some skeletal sites.
Also different measurement methods of PA may explain some of the differences. Lappe et al. [7] found only small differences in hours of PA per week between children at different Tanner-stages (with the highest PA level at Tanner-stage 4). In contrast, in this study we observed decreasing time spent engaging in MVPA as children matured in line with other findings [8]. This finding could influence the association between PA and bone mass, as the youngest, most active children, may already have experienced a positive influence from PA on bone mass making it difficult to gain further benefits. In contrast, older children, with a generally lower level of VPA, may thereby easier gain further benefit from PA by increasing the time spent at VPA.
However, the interaction of maturity with objectively measured VPA observed in peri-pubertal children in this study needs to be evaluated further in future studies addressing this possible influence from maturational development on the association between PA and bone mass.
Vitamin D
The association of vitamin D with bone mass was small in this study (a 10 nmol/l difference in the vitamin D level predicts 3 g difference in TBLH BMC). This small difference is in accordance with the diverse findings of other studies with 2–3 years follow-up; Lehtonen-Veromaa et al. [22] reported a positive association between baseline vitamin D and increase in BMD, and Hauksson et al. [21] showed no association between vitamin D and BMC.
The observed seasonal difference in the vitamin D level aligns with that reported by Farrar et al. [37]; although 52% of participants in this study had insufficient vitamin D at the last follow-up measured in the spring, only 3% were insufficient at baseline (measured in the autumn). This percentage was markedly smaller than the 61–65% being insufficient observed by Hauksson et al. [21] among 7–9-year-old Icelandic children in autumn. Seasonality can be partly adjusted for by analysing vitamin D, age- and sex-adjusted Z scores instead of vitamin D levels, which confirmed the positive association in this study. However, the large proportion of participants having vitamin D at a sufficient level may have influenced the results, as a meta-analysis by Winzenberg et al. [11] reported that vitamin D supplementation may increase vitamin D level in children, but it seems mainly to improve bone mass in the deficient children. Therefore studies with a higher proportion of vitamin D deficient participants may be warranted.
Interaction
This study demonstrates no interaction between the vitamin D level and VPA in the assessment of bone mass in childhood and adolescence. A few cross-sectional studies have examined such interaction. Valtuena et al. [19] and Constantini et al. [20] found interactions between vitamin D and PA but with opposite effects. These studies included few participants in each group and used different bone outcomes. Our results were in line with those of Tonnesen et al. [16], who evaluated young adults (aged 19–25 years) in a cross-sectional study and found no interaction between the vitamin D level and PA with BMD. Our result may be explained by the small association between vitamin D and bone mass in healthy children, few of whom had insufficient vitamin D levels at baseline.
Tracking
A high degree of tracking was observed over more than 6 years of follow-up, with changes in Z scores of height, weight and %LM emerging as factors predicting deviation from tracking. These findings are in line with those of Kalkwarf et al. [25] who demonstrated that changes in height and weight Z scores over 3 years could predict deviation from tracking.
This study is, to the best of our knowledge, the first to evaluate tracking and PA measured with accelerometers, showing a possible positive influence of VPA on deviation from tracking. Other researchers have evaluated PA measured by questionnaires, with diverse results, but all have confirmed a high degree of tracking from childhood into adolescence.
In a 17-year follow-up study, Yang et al. [38] confirmed the high degree of tracking they had found previously [23] in children aged 8–16 years, and demonstrated that fitness capacity at the age of 8 years and self-reported sport participation at the 17-year follow-up in young adults predicted deviation from tracking in spine BMD in boys, but not in girls. Nilsen et al. [24] evaluated tracking over 2 years in Norwegian adolescents aged 15–17 years at baseline and noted some effect of self-assessed PA on total-body BMD in girls but not in boys, and not at specific skeletal sites. Baxter-Jones et al. [39] did not examine tracking directly, but reported positive effects from PA on bone mass in adolescence 1 year after peak height velocity. The benefits are reported to be maintained into young adulthood (mean age 23.1–24.2 years), but diminish over time [39]. Therefore, further research is needed to determine whether PA predicts deviation from tracking through puberty and into adulthood.
This study yielded diverse results regarding vitamin D and tracking. In 2015 a significant difference in the vitamin D level was seen between the reference group (no change in TBLH BMC Z score) and the group with a small positive change in this score. This result could indicate an association between positive deviation from tracking and a higher vitamin D level. No association was seen with greater deviation from tracking (change score ≥ 2), which could be explained by the small number of participants in that group.
In the adjusted mixed-effect model, no association between the vitamin D level and deviation from tracking was found. Hauksson et al. [21] evaluated vitamin D status according to BMC accrual in children, and found no difference in the percentage increase in BMC over 2 years between children with insufficient and sufficient levels of vitamin D. This finding corresponds well with the diverse results regarding the influence of the vitamin D level on bone mass in general, and no clear conclusion can be drawn.
Strengths and Limitations
Strengths of our study include the long follow-up period and performance of 1516 DXA-scans on 663 unique participants, although fewer participants were available for some analyses. At baseline, 90% of the invited population was included and underwent DXA-scan. Another important strength is that we used the same DXA device for all scans, with three operators and two persons analysing all scans. PA was measured using accelerometers, which has proved to be appropriate in large-scale epidemiological studies of children and adolescents [40] and is superior to subjective measures [41].
The major limitation of this study was the high drop-out rate before the last follow-up, thus our analysis of tracking may have been under-powered. However, differences in Z scores of key variables measured at baseline between participants remaining in the study and those who dropped out did not exceed 0.3, but a greater difference in age was observed with the oldest participants tending to drop-out due to logistic reasons. Furthermore, the DXA scanner had a height limit of 195 cm, which led to the exclusion of three participants.
In addition, we did not examine sun exposure or dietary sources of vitamin D or calcium. Finally, accelerometers do not directly measure weight-bearing activities.
Conclusions
In this study, we found a positive association between VPA and TBLH BMC with the association of PA on bone development being highest in the most mature children. Children and adolescents generally become less physically active as they mature. Awareness of this tendency is important; as an increase in the time spent engaging in VPA may have a greater influence on bone mass in late puberty than in early puberty.
Vitamin D was associated weakly with bone mass in this study, supporting the hypothesis that the exact level of vitamin D may have only a minor influence on the skeletal growth in healthy children and adolescents with sufficient vitamin D.
A high degree of tracking in bone mass was present from childhood to adolescence, with changes in anthropometric Z score variables found to be predictive of deviation from tracking. We did not identify any environmental factor that predicted deviation from tracking over the follow-up period, although we observed a possible association with VPA. Thus, it is important to be aware of children presenting with low bone mass as they may be at risk for osteoporosis later in life.
References
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22(3):465–475. https://doi.org/10.1359/jbmr.061113
Hernandez CJ, Beaupre GS, Carter DR (2003) A theoretical analysis of the relative influences of peak BMD, age-related bone loss and menopause on the development of osteoporosis. Osteoporos Int 14(10):843–847. https://doi.org/10.1007/s00198-003-1454-8
Gomez-Bruton A, Matute-Llorente A, Gonzalez-Aguero A, Casajus JA, Vicente-Rodriguez G (2017) Plyometric exercise and bone health in children and adolescents: a systematic review. World J Pediatr 13(2):112–121. https://doi.org/10.1007/s12519-016-0076-0
Weaver CM, Gordon CM, Janz KF, Kalkwarf HJ, Lappe JM, Lewis R, O’Karma M, Wallace TC, Zemel BS (2016) The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations. Osteoporos Int 27(4):1281–1386. https://doi.org/10.1007/s00198-015-3440-3
Mackelvie KJ, McKay HA, Khan KM, Crocker PR (2001) A school-based exercise intervention augments bone mineral accrual in early pubertal girls. J Pediatr 139(4):501–508. https://doi.org/10.1067/mpd.2001.118190
Meyer U, Romann M, Zahner L, Schindler C, Puder JJ, Kraenzlin M, Rizzoli R, Kriemler S (2011) Effect of a general school-based physical activity intervention on bone mineral content and density: a cluster-randomized controlled trial. Bone 48(4):792–797. https://doi.org/10.1016/j.bone.2010.11.018
Lappe JM, Watson P, Gilsanz V, Hangartner T, Kalkwarf HJ, Oberfield S, Shepherd J, Winer KK, Zemel B (2015) The longitudinal effects of physical activity and dietary calcium on bone mass accrual across stages of pubertal development. J Bone Miner Res 30(1):156–164. https://doi.org/10.1002/jbmr.2319
Janz KF, Letuchy EM, Francis SL, Metcalf KM, Burns TL, Levy SM (2014) Objectively measured physical activity predicts hip and spine bone mineral content in children and adolescents ages 5–15 years: iowa bone development study. Front Endocrinol (Lausanne) 5:112. https://doi.org/10.3389/fendo.2014.00112
Heinonen A, Sievanen H, Kannus P, Oja P, Pasanen M, Vuori I (2000) High-impact exercise and bones of growing girls: a 9-month controlled trial. Osteoporos Int 11(12):1010–1017. https://doi.org/10.1007/s001980070021
Saggese G, Vierucci F, Boot AM, Czech-Kowalska J, Weber G, Camargo CA Jr, Mallet E, Fanos M, Shaw NJ, Holick MF (2015) Vitamin D in childhood and adolescence: an expert position statement. Eur J Pediatr 174(5):565–576. https://doi.org/10.1007/s00431-015-2524-6
Winzenberg T, Powell S, Shaw KA, Jones G (2011) Effects of vitamin D supplementation on bone density in healthy children: systematic review and meta-analysis. BMJ 342:c7254. https://doi.org/10.1136/bmj.c7254
Stein EM, Laing EM, Hall DB, Hausman DB, Kimlin MG, Johnson MA, Modlesky CM, Wilson AR, Lewis RD (2006) Serum 25-hydroxyvitamin D concentrations in girls aged 4–8 y living in the southeastern United States. Am J Clin Nutr 83(1):75–81
Pekkinen M, Viljakainen H, Saarnio E, Lamberg-Allardt C, Makitie O (2012) Vitamin D is a major determinant of bone mineral density at school age. PLoS ONE 7(7):e40090. https://doi.org/10.1371/journal.pone.0040090
Boot AM, Krenning EP, de Muinck Keizer-Schrama SM (2011) The relation between 25-hydroxyvitamin D with peak bone mineral density and body composition in healthy young adults. J Pediatr Endocrinol Metab 24(5–6):355–360
Hazell TJ, Pham TT, Jean-Philippe S, Finch SL, El Hayek J, Vanstone CA, Agellon S, Rodd CJ, Weiler HA (2015) Vitamin D status is associated with bone mineral density and bone mineral content in preschool-aged children. J Clin Densitom 18(1):60–67. https://doi.org/10.1016/j.jocd.2014.04.121
Tonnesen R, Schwarz P, Hovind PH, Jensen LT (2016) Physical exercise associated with improved BMD independently of sex and vitamin D levels in young adults. Eur J Appl Physiol 116(7):1297–1304. https://doi.org/10.1007/s00421-016-3383-1
Cashman KD, Hill TR, Cotter AA, Boreham CA, Dubitzky W, Murray L, Strain J, Flynn A, Robson PJ, Wallace JM, Kiely M (2008) Low vitamin D status adversely affects bone health parameters in adolescents. Am J Clin Nutr 87(4):1039–1044
Joo NS, Dawson-Hughes B, Yeum KJ (2013) 25-Hydroxyvitamin D, calcium intake, and bone mineral content in adolescents and young adults: analysis of the fourth and fifth Korea National Health and Nutrition Examination Survey (KNHANES IV-2, 3, 2008–2009. 2010). J Clin Endocrinol Metab and V-1(9):3627–3636. https://doi.org/10.1210/jc.2013-1480 98 ) .
Valtuena J, Gracia-Marco L, Vicente-Rodriguez G, Gonzalez-Gross M, Huybrechts I, Rey-Lopez JP, Mouratidou T, Sioen I, Mesana MI, Martinez AE, Widhalm K, Moreno LA (2012) Vitamin D status and physical activity interact to improve bone mass in adolescents. The HELENA study. Osteoporos Int 23(8):2227–2237. https://doi.org/10.1007/s00198-011-1884-7
Constantini NW, Dubnov-Raz G, Chodick G, Rozen GS, Giladi A, Ish-Shalom S (2010) Physical activity and bone mineral density in adolescents with vitamin D deficiency. Med Sci Sports Exerc 42(4):646–650. https://doi.org/10.1249/MSS.0b013e3181bb813b
Hauksson HH, Hrafnkelsson H, Magnusson KT, Johannsson E, Sigurdsson EL (2016) Vitamin D status of Icelandic children and its influence on bone accrual. J Bone Miner Metab 34(5):580–586. https://doi.org/10.1007/s00774-015-0704-0
Lehtonen-Veromaa MK, Mottonen TT, Nuotio IO, Irjala KM, Leino AE, Viikari JS (2002) Vitamin D and attainment of peak bone mass among peripubertal Finnish girls: a 3-y prospective study. Am J Clin Nutr 76(6):1446–1453
Foley S, Quinn S, Jones G (2009) Tracking of bone mass from childhood to adolescence and factors that predict deviation from tracking. Bone 44(5):752–757. https://doi.org/10.1016/j.bone.2008.11.009
Nilsen OA, Ahmed LA, Winther A, Christoffersen T, Furberg AS, Grimnes G, Dennison E, Emaus N (2017) Changes and tracking of bone mineral density in late adolescence: the Tromso Study, Fit Futures. Arch Osteoporos 12(1):37. https://doi.org/10.1007/s11657-017-0328-1
Kalkwarf HJ, Gilsanz V, Lappe JM, Oberfield S, Shepherd JA, Hangartner TN, Huang X, Frederick MM, Winer KK, Zemel BS (2010) Tracking of bone mass and density during childhood and adolescence. J Clin Endocrinol Metab 95(4):1690–1698. https://doi.org/10.1210/jc.2009-2319
Wedderkopp N, Jespersen E, Franz C, Klakk H, Heidemann M, Christiansen C, Moller NC, Leboeuf-Yde C (2012) Study protocol. The Childhood Health, Activity, and Motor Performance School Study Denmark (The CHAMPS-study DK). BMC Pediatr 12:128. https://doi.org/10.1186/1471-2431-12-128
Heidemann M, Jespersen E, Holst R, Schou AJ, Husby S, Molgaard C, Wedderkopp N (2013) The impact on children’s bone health of a school-based physical education program and participation in leisure time sports: the Childhood Health, Activity and Motor Performance School (the CHAMPS) study, Denmark. Prev Med 57(2):87–91. https://doi.org/10.1016/j.ypmed.2013.04.015
Moore SA, McKay HA, Macdonald H, Nettlefold L, Baxter-Jones AD, Cameron N, Brasher PM (2015) Enhancing a somatic maturity prediction model. Med Sci Sports Exerc 47(8):1755–1764. https://doi.org/10.1249/mss.0000000000000588
Moller NC, Tarp J, Kamelarczyk EF, Brond JC, Klakk H, Wedderkopp N (2014) Do extra compulsory physical education lessons mean more physically active children—findings from the childhood health, activity, and motor performance school study Denmark (The CHAMPS-study DK). Int J Behav Nutr Phys Act 11:121. https://doi.org/10.1186/s12966-014-0121-0
Heidemann M, Molgaard C, Husby S, Schou AJ, Klakk H, Moller NC, Holst R, Wedderkopp N (2013) The intensity of physical activity influences bone mineral accrual in childhood: the childhood health, activity and motor performance school (the CHAMPS) study, Denmark. BMC Pediatr 13:32. https://doi.org/10.1186/1471-2431-13-32
Trost SG, Loprinzi PD, Moore R, Pfeiffer KA (2011) Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc 43(7):1360–1368. https://doi.org/10.1249/MSS.0b013e318206476e
Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, Michigami T, Tiosano D, Mughal MZ, Makitie O, Ramos-Abad L, Ward L, DiMeglio LA, Atapattu N, Cassinelli H, Braegger C, Pettifor JM, Seth A, Idris HW, Bhatia V, Fu J, Goldberg G, Savendahl L, Khadgawat R, Pludowski P, Maddock J, Hypponen E, Oduwole A, Frew E, Aguiar M, Tulchinsky T, Butler G, Hogler W (2016) Global consensus recommendations on prevention and management of nutritional rickets. Horm Res Paediatr 85(2):83–106. https://doi.org/10.1159/000443136
Pearson N, Haycraft E, J PJ, Atkin AJ (2017) Sedentary behaviour across the primary-secondary school transition: a systematic review. Prev Med 94:40–47. https://doi.org/10.1016/j.ypmed.2016.11.010
McCormack SE, Cousminer DL, Chesi A, Mitchell JA, Roy SM, Kalkwarf HJ, Lappe JM, Gilsanz V, Oberfield SE, Shepherd JA, Winer KK, Kelly A, Grant SFA, Zemel BS (2017) Association between linear growth and bone accrual in a diverse cohort of children and adolescents. JAMA Pediatr. https://doi.org/10.1001/jamapediatrics.2017.1769
Bailey DA, McKay HA, Mirwald RL, Crocker PR, Faulkner RA (1999) A six-year longitudinal study of the relationship of physical activity to bone mineral accrual in growing children: the university of Saskatchewan bone mineral accrual study. J Bone Miner Res 14(10):1672–1679. https://doi.org/10.1359/jbmr.1999.14.10.1672
Gabel L, Macdonald HM, Nettlefold L, McKay HA (2017) Physical activity, sedentary time, and bone strength from childhood to early adulthood: a mixed longitudinal HR-pQCT study. J Bone Miner Res 32(7):1525–1536. https://doi.org/10.1002/jbmr.3115
Farrar MD, Mughal MZ, Adams JE, Wilkinson J, Berry JL, Edwards L, Kift R, Marjanovic E, Vail A, Webb AR, Rhodes LE (2016) Sun exposure behavior, seasonal vitamin D deficiency, and relationship to bone health in adolescents. J Clin Endocrinol Metab 101(8):3105–3113. https://doi.org/10.1210/jc.2016-1559
Yang Y, Wu F, Winzenberg T, Jones G (2017) Tracking of areal bone mineral density from age eight to young adulthood and factors associated with deviation from tracking: a 17-yr prospective cohort study. J Bone Miner Res. https://doi.org/10.1002/jbmr.3361
Baxter-Jones AD, Kontulainen SA, Faulkner RA, Bailey DA (2008) A longitudinal study of the relationship of physical activity to bone mineral accrual from adolescence to young adulthood. Bone 43(6):1101–1107. https://doi.org/10.1016/j.bone.2008.07.245
Warren JM, Ekelund U, Besson H, Mezzani A, Geladas N, Vanhees L (2010) Assessment of physical activity - a review of methodologies with reference to epidemiological research: a report of the exercise physiology section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil 17(2):127–139. https://doi.org/10.1097/HJR.0b013e32832ed875
Janz KF, Medema-Johnson HC, Letuchy EM, Burns TL, Gilmore JM, Torner JC, Willing M, Levy SM (2008) Subjective and objective measures of physical activity in relationship to bone mineral content during late childhood: the Iowa Bone Development Study. Br J Sports Med 42(8):658–663. https://doi.org/10.1136/bjsm.2008.047779
Acknowledgements
We thank participants and schools for their participation in the Childhood Health Activity and Motor Performance School study. We gratefully acknowledge the team behind the CHAMPS-study DK consisting of numerous researchers and students participating in data collection and Mette Vogn Hviid for her contribution with the numerous DXA-scans as operator during the whole study period.
Funding
The study was supported by the Danish foundation “Tryg-fonden”, the Region of Southern Denmark, Hospital of Southern Jutland and “Kirsten og Freddy Johansens Fond”.
Author information
Authors and Affiliations
Contributions
MSR, MH, AS, JOL, SH, NW and CM designed the research and interpreted the data. MSR, MH and JT contributed to collecting data and LL and NRJ contributed to laboratory analyses. MSR and NW analysed the data and MSR prepared the first draft of the paper. All authors revised the paper critically and approved the final version. All authors agree to be accountable for the work and to ensure that any questions relating to the accuracy and integrity of the paper are investigated and properly resolved.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Rønne reports grants and personal fees from The Danish foundation “Tryg-fonden”, personal fees from The Region of Southern Denmark, personal fees from Hospital of Southern Jutland, other from Kirsten og Freddy Johansens Fond, during the conduct of the study. Dr. Lylloff and Dr Jørgensen report grants from Kirsten and Freddy Johansens Foundation, during the conduct of the study. Dr. Heidemann, Dr Schou, Dr Tarp, Dr. Laursen, Dr. Husby, Dr. Wedderkopp, and Dr. Mølgaard have nothing to disclose.
Human Rights and Informed Consent
Children and parents received written information about the study together with verbal information at school meetings. Parents provided written informed consent before enrolment in the study. For all children participation was voluntary and consent could be withdrawn at any time. The CHAMPS-study DK was approved by the Regional Scientific Ethical Committee of Southern Denmark (Project ID: S2008-0047, S-20140105).
Rights and permissions
About this article
Cite this article
Rønne, M.S., Heidemann, M., Lylloff, L. et al. Bone Mass Development in Childhood and Its Association with Physical Activity and Vitamin D Levels. The CHAMPS-Study DK. Calcif Tissue Int 104, 1–13 (2019). https://doi.org/10.1007/s00223-018-0466-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-018-0466-5