Abstract
Aims
Overconsumption of sugar-sweetened beverages (SSBs) is associated with an increased risk of metabolic disorders, including obesity and diabetes. However, accumulating evidence also suggests the potential negative impact of consuming nonnutritive sweeteners (NNSs) on weight and glycaemic control. The metabolic effects of sucralose, the most widely used NNS, remain controversial. This study aimed to compare the impact of intake of dietary sucralose (acceptable daily intake dose, ADI dose) and sucrose-sweetened water (at the same sweetness level) on lipid and glucose metabolism in male mice.
Materials and methods
Sucralose (0.1 mg/mL) or sucrose (60 mg/mL) was added to the drinking water of 8-week-old male C57BL/6 mice for 16 weeks, followed by oral glucose and intraperitoneal insulin tolerance tests, and measurements of bone mineral density, plasma lipids, and hormones. After the mice were sacrificed, the duodenum and ileum were used for examination of sweet taste receptors (STRs) and glucose transporters.
Results
A significant increase in fat mass was observed in the sucrose group of mice after 16 weeks of sweetened water drinking. Sucrose consumption also led to increased levels of plasma LDL, insulin, lipid deposition in the liver, and increased glucose intolerance in mice. Compared with the sucrose group, mice consuming sucralose showed much lower fat accumulation, hyperlipidaemia, liver steatosis, and glucose intolerance. In addition, the daily dose of sucralose only had a moderate effect on T1R2/3 in the intestine, without affecting glucose transporters and plasma insulin levels.
Conclusion
Compared with mice consuming sucrose-sweetened water, daily drinking of sucralose within the ADI dose had a much lower impact on glucose and lipid homeostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Emerging evidence indicates that overconsumption of sugar-sweetened beverages (SSBs) is associated with increased risks of metabolic disorders, such as obesity, hyperlipidaemia, diabetes, and other metabolic syndromes [1, 2]. Therefore, an increasing number of people have turned to nonnutritive sweeteners (NNSs) as a beneficial alternative in beverages [3]. Compared with traditional caloric sweeteners, noncaloric sweeteners undoubtedly lower the energy content of the beverages [4, 5]. Intriguingly, some studies have reported the benefits of consuming NNSs, including good glycaemic control and weight loss, whereas others have argued that NNSs can lead to counterintuitive effects, such as obesity and glucose intolerance [6,7,8,9,10,11]. Although the U.S. Food and Drug Administration (FDA) has approved six NNS products based on decades of extensive studies, the use of NNSs as sugar alternatives has been shadowed by concerns that have arisen from controversial data [5, 12]. These contradictory metabolic results come from both human and animal studies, which varied in the methods and dosing that were used [6, 13].
Dietary added sugar, mainly sucrose, corn syrup, and concentrated fruit juice, plays an important role in the epidemic of obesity worldwide [2]. Sucralose, which is structurally similar to sucrose but has three chlorine atoms replacing hydroxyl groups, was first approved in the late 1980s [13]. As one of the most commonly used NNSs in food and beverages, sucralose has been approved globally [14] based on a series of safety evaluations, such as assessments of its chemical stability, toxicity, and effects on development, growth, reproduction, and carcinogenesis [15]. Based on studies that trace the absorption, distribution, metabolism, and excretion (ADME) of sucralose in both animals and humans, very low absorption in plasma and high faecal excretion were observed, therefore, sucralose represents an ideal dietary calorie-free sugar alternative [16]. However, as the study of the gut microbiota on health has drawn much attention these days, researchers have raised the question of whether sucralose can influence overall metabolism by altering microbiota [17]. Moreover, the discovery of sweet taste receptors expressed in the gut has urged researchers to re-evaluate the potential effect of sucralose on overall glycaemic control due to its capability of activating these receptors [18]. Nevertheless, these new findings are controversial. Several studies have reported that sucralose can induce glucose intolerance by altering gut microflora [19, 20]. In contrast, subchronic studies in rodents showed that sucralose had no significant influence on microbiota populations [16], and thus further investigation is required.
As we mentioned above, accumulating studies have reported the negative metabolic impact of excessive sucrose consumption, and several recent studies have also pointed out the potential safety problem of sucralose on glycaemic control [21, 22]. However, human preference for sweet taste is initiated in infancy and spans almost all cultures [23]; therefore, people still wonder which one is the relatively healthier choice. As a high-intensity sweetener, sucralose is approximately 600 times sweeter than sucrose [16]; thus, the addition of a tiny amount of sucralose can achieve the same sweetness as sugars. However, an extremely high dose of either sucrose or sucralose, which is almost unachievable in daily intake, has been used in many in vitro and in vivo animal studies [22, 24, 25]. Therefore, data comparing the metabolic outcomes of consuming a daily dose of sucralose- or sugar-containing beverages with the same sweetness are still lacking.
Based on the no observed adverse effect level (NOAEL), the acceptable daily intake (ADI) for sucralose for the entire population is 5 mg/kg, which is also the FDA dose [13]. However, many studies that demonstrated the deleterious effects of sucrose used a very high dose (most studies used 30% w/v), which is also rarely achievable in daily uptake. In the present study, we compared the effects of daily doses of sucralose and sucrose with the same sweetness (~ 6% w/v) on glucose and lipid homeostasis in C57Bl/6 mice. We found that after 16 weeks of consuming of sucralose- or sucrose-sweetened water, sucrose consumption resulted in fat accumulation, hyperlipidaemia, and liver steatosis in mice, whereas no significant lipid alteration was observed in mice that drank sucralose. Although both sucrose and sucralose enhance sweet taste receptors T1R2 and T1R3 in the intestine, sucralose displayed lower impact on incretin levels and overall glucose tolerance.
Materials and methods
Animals
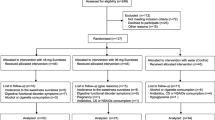
The animal experimental procedure was conducted under the Animal Ethical Board of Nanjing University (IACUC-2008017). Male C57BL/6 J mice (8 weeks old) were purchased from the Model Animal Research Centre of Nanjing University. The experimental animals were kept under standard conditions of a 12-h light/dark period in a specific pathogen-free facility. All animals were fed a normal chow diet (12%, 67.4%, and 20.6% calories from fat, carbohydrate and protein, respectively, energy 3.53 kcal/g, SWS9102, Jiangsu Xietong Pharmaceutical Bioengineering Co., Ltd.). Mice were divided into three groups at random and given water, a 0.1 mg/ml sucralose solution (cat# 69,293, Sigma–Aldrich) [19], or a 60 mg/ml sucrose solution (cat# 900,116, Sigma–Aldrich) for a 16-week duration. The body weights of these mice were measured before and after 4 weeks, 8 weeks, 12 weeks and 16 weeks of drinking the sweetened water. Mice were anaesthetized by isoflurane inhalation (3–4% induction, 1–2% maintenance), and body fat analysis was performed by a bone density imager (Ultra Focus DXA, Faxitron, USA). Isoflurane was used for anaesthetization, and mice were euthanized by cervical dislocation.
Metabolic cage assessments
To study the metabolism of the animals after 16 weeks of feeding, a metabolic cage (PhenoMaster, TSE, Germany) was used to assess the respiratory exchange ratio (RER) and total activity (XT + YT). The animals were monitored separately for 4 consecutive days, and data were collected on the last 3 days after the 1-day acclimation.
Immunohistochemistry (IHC) staining
Duodenum and ileum tissues were soaked in 4% paraformaldehyde (PFA) for 24 h. The 5-μm-thick paraffin slides were incubated with anti-T1R2 (cat# NB110-74,920, 1:200, Novus), anti-T1R3 (cat# NB100-98,792, 1:2500, Novus), anti-SGLT1 (cat# NBP2-20,338, 1:200, Novus), and anti-GLUT2 (cat# 20,436-1-AP, 1:1000, Proteintech) antibodies at 4 °C overnight. A ready-to-use high-efficiency immunohistochemistry secondary antibody kit (cat#abs957, 1:1000, Absin, Shanghai, PRC) was used to amplify the signal.
Immunofluorescence (IF) staining
Duodenum and ileum tissues were soaked in 4% paraformaldehyde (PFA) for 24 h. Tissues were cryoprotected in 15% sucrose for 1 h, incubated in 30% sucrose for 12 h, and then embedded in OCT prior to sectioning. Tissue Sects. (6 μm) were washed in PBST (0.5% Triton X-100) for three times 5 min, then followed by 10 min in PBST (1% Triton X-100) before blocking in 5% bovine serum albumin in PBST (0.5% Triton X-100) for 1 h. And then were incubated with anti-T1R2 (cat# NB110-74,920, 1:250, Novus) and anti-GLP-1 (cat# sc-514592, 1:250, Santa) or anti-GIP (cat# ab209792, 1:100, Abcam) antibodies overnight at 4 °C. All sections were incubated with species-specific secondary antibodies conjugated to Alexa Fluor dyes for 1 h (room temperature). When examining coexpression of GLP-1 and T1R2, we used secondary labels were Alexa fluor 488 (cat# A-11001, Invitrogen) and 594 (cat# A-21207, Invitrogen) streptavidin conjugates, respectively, 1:500. For GIP, we used the Donkey anti-Rabbit IgG (H + L) Highly Cross-Adsorbed Secondary Antibody, Alexa Fluor™ 488 (cat# A-21206, 1:500, Invitrogen). Finally, the sections were washed in 1 × PBST for three times 5 min, and mounted in ProLongTM Gold antifade reagent with DAPI (cat# P36935, Invitrogen). Sections were observed with a confocal microscope (Zeiss LSM880, Zeiss, Germany). ZEISS ZEN 3.6 software was used for image processing. Immunostained cells and nuclei were counted both manually and by software validation. The numbers of cells per thousand nucleated cells immunopositive for T1R2, GLP-1, and GIP were calculated. And the results shown are representative of those obtained in experiments performed in repeated five times (biological repeats) to ensure reproducibility.
Oil red O staining
The livers were collected and soaked in 4% PFA for 24 h, 15% sucrose solution for 10 min and 30% sucrose solution for 12 h. Cryostat Sects. (10 μm) were cut for Oil red O staining. Then, the lipids were stained with Oil Red O (cat# O0625, Sigma–Aldrich) for 14 min, after which the slides were rinsed twice in isopropyl alcohol for 5 s. The slides were then washed in PBS and imaged directly.
OGTT and ITT
For the OGTT, the animals were fasted for 12 h and administered glucose by gavage (2 g/kg body weight). For ITT, the animals were fasted for 6 h and then given insulin (0.75 U/kg body weight) via intraperitoneal injection. For OGTT and ITT, a blood glucose metre (Cat# 590, Yuwell, PRC) was utilized to determine the glucose level at 0, 15, 30, 60, 90, and 120 min after administration of glucose and insulin, respectively.
Metabolic index
A mouse insulin ELISA (cat# 10-1247-01, Mercodia), glucagon ELISA (cat# 10-1281-01, Mercodia), Rat/Mouse GIP (Total) 96-Well Plate (cat# EZRMGIP-55 K, Millipore, Billerica, MA, America), GLP-1 Total ELISA 96-Well Plate Assay (cat# EZGLP1T-36 K, Millipore), Mouse Haemoglobin A1c (HbA1c) Kit (cat# 80,310, Crystal Chem) and LBIS Mouse C-peptide ELISA Kit (U-type) (cat# 635-07,239, Wako) were used to measure serum hormones in mice in both fasted and refed states. Total plasma cholesterol (TC), triglycerides (TGs), LDL-cholesterol (LDL-C) and HDL-cholesterol (HDL-C) were assessed using commercial kits (Cat# A111-1, A110-1, A113-1 and A112-1, Nanjing Jiancheng Bioengineering Institute). All procedures were performed in accordance with the kit instructions and were measured on a spectrophotometer (Thermo Fisher Scientific, Waltham, MA, USA).
RNA-seq
RNA from the liver was isolated via TRIzol reagent (cat# T9424, Sigma–Aldrich). The RNA sequencing library was established via a NEBNext® Ultra™ RNA Library Preparation Tool, and the library preparation was subjected to sequencing by an Illumina NovaSeq 6000 platform by CapitalBio Technology (PRC). Fold-change screening was used to identify genes that were differentially expressed. GO enrichment was studied in the command-line software KOBAS 2.0. To statistically identify the highly enriched pathways in a batch of sequences, our team utilized the complete genome as the default background distribution. For every pathway occurring in the set of genes, our team recorded the sum of genes in the set involved in the pathway term or the GO term. A hypergeometry distribution was used to determine the p value.
Quantitative RT–PCR detection
The purified total RNA was reversed transcribed with HiScript III RT SuperMix (R323, Vazyme), and the quantitative real-time polymerase chain reaction (Q-PCR) was conducted according to the instructions provided with ChamQ Universal SYBR qPCR Master Mix (Q711, Vazyme). The reaction was first incubated at 95 °C for 5 min, followed by 40 cycles of 95 °C for 15 s, 60 °C for 30 s, and 72 °C for 30 s. After the reaction was complete, to determine the CT value, the relative level of mRNA was normalized to β-actin, and the value was calculated by the 2 – ΔΔCT method.
Statistical analysis
GraphPad Prism 7 was utilized for all statistical tests. Data were compared by one-way ANOVA, except for the body weight data, which were compared by two-way ANOVA, and multiple comparisons were conducted by Dunnett’s test. Data are shown as the mean ± SEM. P < 0.05 indicated statistical significance.
Results
Fat accumulation accelerates in mice drinking sucrose-sweetened water, rather than sucralose-sweetened water, accelerates fat accumulation in mice
Based on human and animal ADME studies, mice have been determined to be appropriate experimental models for sucralose studies, as their metabolism mimics that observed in humans [16]. Here, sucrose or sucralose was added to the drinking water of 8-week-old male C57BL/6 J mice for 16 weeks. The sucralose concentration was 0.1 mg/ml, which was equivalent to the FDA-approved ADI in humans (5 mg/kg/day) [19]. To compare sucralose with sucrose at the same sweetness level, the concentration of sucrose-containing water was 60 mg/ml (~ 6% w/v sucrose), as sucralose has a sweetness potency of about 600 times that of sucrose [16]. All mice were fed a normal chow diet (67.4% carbohydrate, 20.6% protein, 12% fat (w/w), energy 3.53 kcal/gram). Compared to the group receiving only water, the sucrose consumption group showed slightly increased body weight gain, although no statistical significance was observed (Fig. 1A). In a similar manner, compared with the water group, sucralose consumption led to slightly decreased body weight gain, also without statistical significance. As shown in Table 1, sucralose addition only led to a slight but not significant elevation in water uptake, as the food intake was comparable between the sucralose and control groups, and the total daily caloric intake was approximately 11.72 kcal and 11.83 kcal, respectively. Mice with access to the sugar-sweetened water drank more water than the control group, which might account for the slight decrease in food intake. Thus, when considering the diet and drinking water, the total daily caloric intake was approximately 0.7 kcal more. Indirect calorimetry analysis also revealed that there were no significant differences in locomotor activity or respiratory exchange ratio (RER) during the light–dark cycle among the three groups of mice, suggesting that consumption of sucrose or sucralose had no significant influence on either physical activity or the fuel being mobilized to supply energy (Fig. 1B, C). In addition, the bone mineral density (BMD) was also comparable between each group (Fig. 1D). However, compared with the water control group, the sucrose group showed markedly increased fat mass, accompanied by slightly decreased lean mass. In addition, the fat mass was comparable between the sucralose and control groups (Fig. 1E, F and Figure S1A). Overall, 16 weeks of feeding with the ADI dose of sucralose did not affect food intake or physical activity in mice, whereas compared with either the water control or the sucralose group, consumption of sucrose led to elevated body mass accumulation in mice.
Effect of sucrose (60 mg/mL) and sucralose (0.1 mg/mL) on body weight, physical activity, and fat mass in C57Bl/6 mice. A Weight measurements of the water (blue), sucrose (brown), and sucralose (orange) groups after feeding for 0, 4, 8, 12 and 16 weeks. B–C Metabolic cage analysis after 16 weeks of sweetener feeding. Exercise (XT + YT, B) and respiratory exchange rate (RER, C). D–F Body composition of mice fed water, sucrose, or sucralose for 16 weeks. The BMD (D), fat mass (E) and body fat percentage (F) of mice were measured with a bone densitometer. N = 14 mice/group for (A), 12 mice/group for (B–C), and 10 mice/group for (D–F). Data represent the mean ± SEM. **p < 0 .01, ***p < 0 .001, two-way ANOVA for (A) and one-way ANOVA for (B–F) with Dunnett’s multiple comparisons test
Hyperlipidaemia and liver steatosis are induced in mice drinking sucrose- but not sucralose-sweetened water
To further determine the impact of sucrose and sucralose on lipid metabolism, the plasma lipids were analysed. As shown in Fig. 2A, sucrose intake led to a trend towards increase in total triglycerides. Notably, although no statistical significance was observed between the sucrose and water groups, the plasma triglycerides were markedly lower in the sucralose group than in the sucrose group. In addition, plasma cholesterol analysis showed that sucrose consumption caused an approximately 54% increase in low-density lipoprotein (LDL) and moderately decreased level of high-density lipoprotein (HDL). This may explain why no significant effect on total cholesterol was observed in the sucrose group. However, no significant differences in plasma cholesterols were noted between the sucralose and water groups, indicating a lower impact of sucralose on plasma lipids. We next explored the impacts of sucrose and sucralose on liver lipid metabolism. Liver histology and Oil red O staining revealed that sucrose drinking led to a marked increase in hepatic lipids in comparison to controls. Only slightly higher lipid accumulation was observed in the sucralose group than in the water group (Fig. 2B). To further explore the potential influence of sweetened water in the liver, we conducted RNA-seq to assess the gene expression changes in the liver from mice after 16 weeks of either sucrose or sucralose administration. The expression level for each of the identified genes was normalized as the fragments per kilobase of transcript per million mapped reads (FPKM). To improve the reliability and comparability of differential expression analysis, a total of 31,135 identified genes with FPKM values > 1 in all groups were included in the analysis. Compared with the water control, 175 and 380 differentially expressed genes (DEGs) with a fold-change > 2 (FC > 2) were chosen from the sucrose and sucralose groups, respectively. Gene ontology (GO) enrichment analysis showed that among the top ten enriched GO terms, six terms were associated with the regulation of lipid metabolic processes in the sucrose group compared with the water control, suggesting a strong association between sucrose consumption and hepatic lipid derangement (Fig. 2C). In line with the previous oil-red O staining results, for the sucralose group, none of the top 10 enriched GO terms were related to lipid metabolism (Fig. 2D). As expected, the hepatic lipogenic genes, including Srebp1, Cd36, and Acc1, were markedly increased in the sucrose group but not the sucralose group (Fig. 2E, F, G). Collectively, these data indicate that compared with sucralose, consumption of sucrose-sweetened water induces hyperlipidaemia and liver steatosis in mice.
Effect of sucrose and sucralose on plasma and liver lipids. A The levels of triglycerides (TGs), total cholesterol (TC), low-density lipoprotein (LDL), and high-density lipoprotein (HDL) in fasting serum of the water (blue), sucrose (brown), and sucralose (orange) groups were measured with ELISA kits. B Representative images of Oil Red O staining of the liver; scale bar = 50 μm. C–D Gene ontology (GO) terms enriched in different biological processes (BP) of the liver in the sucrose (C) and sucralose groups (D). E–G Quantitative polymerase chain reaction (qPCR) analysis of lipid metabolism-related gene expression levels in the liver of the water (blue), sucrose (brown), and sucralose (orange) groups. N = 12 mice/group for (A), 8 mice/group for (E–G). Data represent the mean ± SEM. ****p < 0.0001, one-way ANOVA with Dunnett’s multiple comparisons test
Mice consuming sucralose developed glucose intolerance much less than those drinking sucrose
To assess glucose tolerance in the three groups of mice, oral glucose tolerance tests were performed in fasted mice. For the sucrose and sucralose groups of mice, the sweeteners were substituted with water for the period of the fasting hormones, glucose, or insulin tolerance analysis. As shown in Fig. 3A, the sucrose group showed an impaired glucose tolerance response. In line with this result, the sucrose group also exhibited impaired insulin sensitivity compared with the water group. Of note, compared with the water group, although slightly increased trends in insulin intolerance were observed in the sucralose group, no statistical significance was observed (Fig. 3A). Collectively, these data suggested that compared with sucrose-sweetened water, sucralose showed less of an impact on glucose and insulin sensitivity. In addition, 16 weeks of drinking sucrose-containing water markedly increased fasting and postprandial plasma insulin and C-peptide levels in mice, which may account for the observed unchanged fasting glucose level (Fig. 3B, C). Plasma glucagon, which is produced by pancreatic α-cells, was also analysed in the three groups of mice. Interestingly, the plasma glucagon level was drastically decreased after overnight fasting and significantly increased postprandially in the sucrose group (Fig. 3D). In addition, the fasted and fed blood glucose levels were also assessed in mice that still drank the sweetened water. As expected, compared with water controls, the caloric sucrose-sweetened liquid resulted in significantly increased blood glucose level in mice even without food intake, whereas in the fed state, only moderately elevated blood glucose level was observed. However, none of the above blood glucose alterations were observed in mice consuming sucralose (Fig. 3E). In line with these results, the blood haemoglobin A1c (Hb1AC) test showed that 16 weeks of sucrose drinking led to a marked increase in blood sugars attached to haemoglobin, while the sucralose group exhibited a similar Hb1AC level to the water group (Fig. 3F). These data indicate that sucralose-consuming mice developed much less glucose intolerance than those drinking sucrose at the same sweetness level. To further examine the influence of sucrose and sucralose on glucose metabolism in major tissues, the mRNA levels of glucose transporters 1 and 2 (Slc2a1 and Glut 2) and canonical gluconeogenic genes, including G6p and Pck1, were analysed by qRT-PCR in the livers of mice. As shown in Fig. 3G, H, I, J, compared with control mice that drank water, glucose transporters and gluconeogenic genes were significantly increased in the sucrose group, whereas no significant differences were observed in mice treated with sucralose. Taken together, these results suggest an impaired hepatic gluconeogenesis, leading to hyperglycaemia in response to glucose.
Mice consuming sucrose developed more serious glucose intolerance. A Oral glucose tolerance testing and insulin tolerance testing in water (blue), sucrose (brown), and sucralose (orange) mice after 16 weeks of treatment with AUC. B-F) The levels of insulin (B), C-peptide (C) and glucagon (D) in fasting and postprandial mice from the water (blue), sucrose (brown), and sucralose (orange) groups were measured by ELISA kits. E Fasting, only beverages (drinking water/sucrose/sucrose but no food consumption), and postprandial (drink + food) blood glucose levels of the water (blue), sucrose (brown), and sucralose (orange) groups. F The levels of glycosylated haemoglobin in the water (blue), sucrose (brown), and sucralose (orange) groups were determined by ELISA. G–J Quantitative polymerase chain reaction (qPCR) analysis of glucose metabolism-related gene expression levels in the liver of the water (blue), sucrose (brown), and sucralose (orange) groups. N = 10 mice/group for (A), 12 mice/group for (B–D & F), 15, 10, and 10 mice/group for (E), and 8 mice/group for (G–J) Data represent the mean ± SEM. *p < 0.05, **p < 0.01, one-way ANOVA with Dunnett's multiple comparisons test
Differential impact of sucrose and sucralose on glucose transporters and sweet taste receptors in the intestine
To further explain the differential responses of blood glucose between the sucrose and sucralose groups, two primary hexose transporters present in rodent small intestine, glucose transporter 2 (GLUT2) and cotransporter 1 (SGLT1), were examined in mice. To eliminate the interference from food, all mice fasted overnight, and the sweeteners were substituted with water 12 h before examination. Immunohistochemistry staining analysis revealed that the expression of GLUT2 and SGLT1, which transport dietary sugars from the intestine lumen into the absorptive enterocytes, was markedly elevated in the duodenum and ileum of mice treated with sucrose (Figure S1B). The staining for both antibodies was stronger on the lumen- side, suggesting that 16 weeks of drinking sucrose-sweetened water led to increased expression of GLUT2 and SGLT1 in the intestine (~ 1.8- and 2.2-fold, respectively), even without acute glucose stimulation. In contrast, only slightly increased GLUT2 and SGLT1 expression was observed in the duodenum or ileum of the mice administrated the ADI dose of sucralose. This is reasonable, as sucrose consumption showed a larger influence on overt glucose homeostasis than sucralose consumption (Fig. 3A). The discovery of sweet -taste receptors (STRs) has caused many debates on the glycaemic control effect of nonnutritive sweeteners (NNSs), as STRs can also be activated by NNS. To compare the impact of sucralose on STRs with sucrose at the same sweetness level, the expression levels of T1R2 and T1R3, which belong to the T1R family of C G protein-coupled receptors, were also measured in the intestines of mice. As indicated by immunochemistry staining, compared with the sucrose group, which showed a dramatically increased amount of T1R2 and T1R3 expression (~ 2-2.5-fold), only moderately elevated levels of T1R2 and T1R3 were detected in both the duodenum and ileum of sucralose group (~ 1.5-2-fold). Collectively, these results suggest that as a high-intensity sweetener, ADI-dose sucralose consumption showed a lower impact on the expression levels of T1R2/3 in the intestine than sucrose consumption, probably due to the dose being much lower than that of sucrose. Furthermore, immunofluorescence (IF) was conducted to determine the possible cell type (L cell or K cell) in which sweet receptors were increased. Considering that T1R2 and T1R3 are heteromeric taste receptors, T1R2 was examined in this study. As shown in Fig. 4, the spatial relationship between T1R2 and L cells was visualized by coimmunolabeling of T1R2- and GLP-1-positive cells in the ileum and duodenum from mice, respectively. As indicated by the numbers of cells per thousand nucleated cells immunopositive for T1R2, the ileum from mice drank sucrose showed a dramatically increased amount of T1R2 (22 ± 2), compared with the water group (7 ± 1). In addition, GLP-1-expressing L cell population coexpressing T1R2 was also significantly higher in the ileum of sucrose group (17 ± 2) than water group (4 ± 1) (Fig. 4A). Moreover, only slightly higher amount of GIP-positive cells were observed in the ileum of sucrose group (5 ± 2) than the water group (3 ± 1) (Figure S2A). While for the sucralose group of mice, moderate increased GLP-1-positive cells coexpressed T1R2 (14 ± 3), and almost unchanged level of GIP-positive cells (4 ± 1) was observed in the ileum compared with the water group. These results indicate that the majority increased amount of T1R2 may expressed in the L cells in the ileum. Similarly, the duodenal T1R2-immunopositive cells were also significantly increased in the sucrose group (50 ± 5) compared with the water group (18 ± 3). Meanwhile, the duodenal GLP-1-expressing L cell population coexpressing T1R2 was higher in the sucrose group (13 ± 2) than the water group (3 ± 1). Of note, unlike in the ileum, the increased number of duodenal T1R2-expressing cells, 31 ± 5, was much higher than that GLP-1-positive cells coexpressed T1R2 (10 ± 3) (Fig. 4B). This is reasonable as the duodenal GIP-positive K cells were also markedly increased in the sucrose group (30 ± 4) compared with the water group (10 ± 2) (Figure S2B). These data suggesting that in the duodenum, both increased L cells and K cells may contribute to the upregulated T1R2 expression in mice drank sucrose. While for the sucralose group of mice, both the detected duodenal T1R2-immunopositive L cells and K cells were significantly lower compared with those observed in the sucrose group.
Impact of sucrose and sucralose on sweet taste receptors in ileum and duodenum. A–B Representative images of the immunofluorescent staining of GLP-1 (green), T1R2 (red), and DAPI (blue) in the ileum and duodenum after 16 weeks of drinking water, sucrose, or sucralose. Scale bar = 10 μm. Data represent the mean ± SEM. *p < 0.05, **p < 0.01, one-way ANOVA with Dunnett's multiple comparisons test
Sucralose displays a lower impact on plasma incretin hormones than sucrose at the same sweetness level
The incretin hormones, including glucose-dependent insulinotropic peptide (GIP) and glucagon-like peptide-1 (GLP-1), are released from K cells and L cells in the intestine, respectively [26, 27]. The circulating concentrations of GIP and GLP-1 were measured in mice. For fasting hormone assessment, mice were fasted overnight with free access to water without sweeteners. For the sucrose group, under the fasted state, the GIP level only slightly increased; however, a significant upregulation of GLP-1 was observed. Interestingly, 2 h after refeeding, the postprandial GIP was significantly higher than that in the water group, while comparable GLP-1 levels were observed between the sucrose and water groups (Fig. 5A, B). These data suggest that sucrose consumption may have differential impacts on GIP and GLP-1 release. Given that they both stimulate insulin secretion, it was not surprising that increased plasma insulin levels were observed in mice drinking sucrose. However, for mice drinking sucralose, although slight upregulation of GIP and GLP-1 was observed in both fasted and refed states, no statistical significance was observed (Fig. 5A, B). Together, these results show that sucralose has a lower impact on plasma incretin hormones than sucrose at the same sweetness level, possibly due to fewer impacts on either glucose transporters or STRs.
The plasma incretin levels of mice treated with sucrose or sucralose. A–B The fasting and postprandial levels of GIP (A) and GLP-1 (B) in the water (blue), sucrose (brown), and sucralose (orange) groups were measured with ELISA kits. N = 13 mice/group for (A), 12 mice/group for (B). Data represent the mean ± SEM. **p < 0.01, ***p < 0 .0001, one-way ANOVA with Dunnett's multiple comparisons test
Discussion
The human appetite for sweetness is innate and universal. Unfortunately, compelling evidence has shown that consumption of either traditional nutritional sugars, such as sucrose, fructose, and concentrated fruit juice, or their nonnutritional substitutes, including aspartame and sucralose, which have become more popular, nowadays, is associated with obesity and metabolic disorders. However, the varying doses and methodologies used have led to contradictory observed effects of NNSs. The sucralose dose used in many studies is also very high, which is almost unachievable in daily intake. However, few studies have compared the metabolic outcomes of consuming NNSs (within the ADI dose) to sugar-containing beverages at the same sweetness levels. In the present study, mice were fed the FDA-approved ADI dose of sucralose for 16 weeks. By comparing its impacts on lipid and glucose metabolism with mice fed sucrose at the same sweetness level, we found that the sucralose group showed fewer impacts on adipose accumulation, dyslipidaemia, glucose intolerance, and incretin secretions.
According to the AHA suggestion, a limit of added-sugar of no more than 24 g and 36 g per day is recommended for most women and men, respectively [28]. The concentration of fructose in typical soda is equivalent to approximately 10% sucrose in the drinking liquid [29]. However, of the numerous studies that have reported the effect of sucrose on adiposity and glucose homeostasis, the sucrose dose used was very high (~ 30% w/v), which most people would never achieve during daily life. Thus, it is important to know whether daily intake of relatively high but achievable doses of sucrose can also cause the reported deleterious metabolic effects. In the present study, a much lower dose of sucrose (60 mg/ml, 6% w/v, equivalent to approximately 120 g/day for a 50 kg human), which could be consumed by a person with a “sweet tooth” during daily life, was used to explore the potential metabolic impacts. Of note, although the body weight was only slightly increased, we did observe a significant increase in fat mass in the sucrose group of mice, suggesting that daily overconsumption of sugar may indeed increase metabolic disorders, including fat accumulation, and decrease in lean mass. Previous studies have reported that consuming sugar-sweetened beverages/foods increased body adiposity, accompanied by decreased lean mass, possibly due to induced myodegeneration [30, 31]. Interestingly, our data showed similar changing pattern in fat mass and lean mass in the sucrose group of mice.
Some studies have indicated that in addition to caloric sweeteners, artificial sweeteners can also impact rodent glucose homeostasis by activating STRs in the intestine, such as inducing T1R3-dependent SGLT1 upregulation. However, these findings remain inconclusive, as other studies failed to observe the same effect on humans [13, 26, 32]. According to previous reports, natural sweeteners, including sucrose, activate STRs at approximately 100 mM, while artificial sweeteners at concentrations less than 10 mM can also lead to the activation of these STRs [33]. Here, using the ADI dose of sucralose (~ 0.25 mM) and sucrose at the same sweetness level (~ 175 mM), we showed that sucralose led to a much lower expression of STRs and of glucose transporters in the intestine. Based on the immunostaining results, for the sucrose group, we speculated that T1R2 showed the highest increase in L cells in the ileum, whereas in the duodenum, both the increased K cells and L cells may contribute to the upregulated T1R2 expression. Although a similar change was observed in the sucralose group, the increased L and K cells were found at significant lower levels than in the sucrose group, thereby leading to only moderately increased T1R2 expression. Previous studies have measured the plasma GLP-1 concentration in type 2 diabetic patients [34]. In the fasted state, GLP-1 is increased in T2DM, whereas postprandial GLP-1 secretion is drastically decreased. In line with this result, our data showed that in the fasted state, the circulating GLP-1 level was increased after 16 weeks of sucrose consumption. Surprisingly, postprandial GLP-1 levels were comparable between the sucrose and water groups of mice. These partially contradictory results may come from different metabolic circumstances. In our study, the sucrose group of mice was more likely to be in the pre-or early-diabetic state with an impaired glucose tolerance (IGT). Therefore, we postulated that under a fasting state, the increased L cells in the intestine may account for the upregulated basal GLP-1 level, thereby stimulating basal insulin secretion to maintain fasting blood glucose within the normal range. Importantly, previous reports have indicated that in T2DM, the ability of incretin cells to secrete GLP-1 is severely impaired, which results in a markedly decreased postprandial GLP-1 secretion. Therefore, it is quite possible that in our experiments, the secretion ability of the incretin cells may also be slightly impaired in the sucrose group since it is still in the IGT stage. However, as the L cells were also compensatorily increased, at this stage, the circulating GLP-1 levels were still comparable in the sucrose and control groups after a meal.
In addition, previous studies also indicated that in patients with T2DM, the initial GIP response is exaggerated compared with control subjects after a mixed meal [35]. Consistent with this observation, our data indicated that the postprandial circulating level of GIP was also increased in the sucrose of mice. While under fasted state, the trend towards an increased GIP level may result from the increased K cells in the duodenum of mice drinking sucrose. However, further studies are still urgently needed to explore the possible mechanisms of nutrient-triggered GLP-1/GIP regulation.
As the present study only explored the impact of dietary sucralose- and sucrose-sweetened water intake on lipid and glucose metabolism in male mice, it might introduce a bias, as the hormones in female mice are quite different, such as oestrogen, which is well known to have beneficial effects on metabolism, including enhancing insulin sensitivity. As both men and women consume sugar-containing or NNS currently, it is important to explore the potential impact of dietary sucralose- and sucrose-sweetened water on metabolism in female mice in future studies.
In summary, our data showed that compared with healthy mice that consume sucrose-sweetened water, daily drinking of sucralose within the ADI dose had a much lower impact on glucose and lipid homeostasis in mice. Although more investigations should be conducted, our data strongly suggest that daily overconsumption of SSBs did have a negative impact on metabolism and that the use of sucralose as a sugar alternative in daily life might be helpful in glycaemic control.
Abbreviations
- SSB:
-
Sugar-sweetened beverage
- NNS:
-
Nonnutritive sweetener
- ADI:
-
Acceptable daily intake
- STRs:
-
Sweet taste receptors
- FDA:
-
U.S. Food and Drug Administration
- ADME:
-
Absorption, distribution, metabolism, and excretion
- NOAEL:
-
No observed adverse effect level
- BMD:
-
Bone mineral density
- RER:
-
Respiratory exchange ratio
- PFA:
-
Paraformaldehyde
- GTT:
-
Glucose tolerance test
- ITT:
-
Insulin tolerance test
- TC:
-
Total plasma cholesterol
- TG:
-
Triglycerides
- LDL:
-
Low-density lipoprotein
- HDL:
-
High-density lipoprotein
- FPKM:
-
Fragments per kilobase of transcript per million mapped reads
- Hb1AC:
-
Blood haemoglobin A1c
- GLUT2:
-
Glucose transporter 2
- SGLT1:
-
Sodium/glucose cotransporter 1
- T1R2/3:
-
Taste receptor type 1 member 2/3
- GIP:
-
Glucose-dependent insulinotropic peptide
- GLP-1:
-
Glucagon-like peptide-1
- AHA:
-
American Heart Association
References
Burchfield JG, Kebede MA, Meoli CC, Stockli J, Whitworth PT, Wright AL, Hoffman NJ, Minard AY, Ma X, Krycer JR, Nelson ME, Tan SX, Yau B, Thomas KC, Wee NKY, Khor EC, Enriquez RF, Vissel B, Biden TJ, Baldock PA, Hoehn KL, Cantley J, Cooney GJ, James DE, Fazakerley DJ (2018) High dietary fat and sucrose results in an extensive and time-dependent deterioration in health of multiple physiological systems in mice. J Biol Chem 293(15):5731–5745. https://doi.org/10.1074/jbc.RA117.000808
Herman MA, Birnbaum MJ (2021) Molecular aspects of fructose metabolism and metabolic disease. Cell Metab 33(12):2329–2354. https://doi.org/10.1016/j.cmet.2021.09.010
Li XE, Lopetcharat K, Drake MA (2015) Parents’ and children’s acceptance of skim chocolate milks sweetened by monk fruit and stevia leaf extracts. J Food Sci 80(5):S1083-1092. https://doi.org/10.1111/1750-3841.12835
Gardner C, Wylie-Rosett J, Gidding SS, Steffen LM, Johnson RK, Reader D, Lichtenstein AH, American Heart association nutrition committee of the council on nutrition PA, metabolism CoAT, vascular biology CoCDitY, the American D (2012) Nonnutritive sweeteners: current use and health perspectives: a scientific statement from the American heart association and the American diabetes association. Circulation 126(4):509–519. https://doi.org/10.1161/CIR.0b013e31825c42ee
Hunter SR, Reister EJ, Cheon E, Mattes RD (2019) Low calorie sweeteners differ in their physiological effects in humans. Nutrients. https://doi.org/10.3390/nu11112717
Peters JC, Wyatt HR, Foster GD, Pan Z, Wojtanowski AC, Vander Veur SS, Herring SJ, Brill C, Hill JO (2014) The effects of water and non-nutritive sweetened beverages on weight loss during a 12-week weight loss treatment program. Obesity (Silver Spring) 22(6):1415–1421. https://doi.org/10.1002/oby.20737
Ahmad SY, Friel JK, MacKay DS (2020) The effect of the artificial sweeteners on glucose metabolism in healthy adults: a randomized, double-blinded, crossover clinical trial. Appl Physiol Nutr Metab 45(6):606–612. https://doi.org/10.1139/apnm-2019-0359
Azad MB, Abou-Setta AM, Chauhan BF, Rabbani R, Lys J, Copstein L, Mann A, Jeyaraman MM, Reid AE, Fiander M, MacKay DS, McGavock J, Wicklow B, Zarychanski R (2017) Nonnutritive sweeteners and cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials and prospective cohort studies. CMAJ 189(28):E929–E939. https://doi.org/10.1503/cmaj.161390
Lutsey PL, Steffen LM, Stevens J (2008) Dietary intake and the development of the metabolic syndrome: the atherosclerosis risk in communities study. Circulation 117(6):754–761. https://doi.org/10.1161/CIRCULATIONAHA.107.716159
Nettleton JA, Lutsey PL, Wang Y, Lima JA, Michos ED, Jacobs DR Jr (2009) Diet soda intake and risk of incident metabolic syndrome and type 2 diabetes in the multi-ethnic study of atherosclerosis (MESA). Diabetes Care 32(4):688–694. https://doi.org/10.2337/dc08-1799
Fagherazzi G, Vilier A, Saes Sartorelli D, Lajous M, Balkau B, Clavel-Chapelon F (2013) Consumption of artificially and sugar-sweetened beverages and incident type 2 diabetes in the etude epidemiologique aupres des femmes de la mutuelle generale de l’Education nationale-European prospective investigation into cancer and nutrition cohort. Am J Clin Nutr 97(3):517–523. https://doi.org/10.3945/ajcn.112.050997
Basson AR, Rodriguez-Palacios A, Cominelli F (2021) Artificial sweeteners: history and new concepts on inflammation. Front Nutr 8:746247. https://doi.org/10.3389/fnut.2021.746247
Ahmad SY, Friel JK, Mackay DS (2020) Effect of sucralose and aspartame on glucose metabolism and gut hormones. Nutr Rev 78(9):725–746. https://doi.org/10.1093/nutrit/nuz099
Meng Y, Li S, Khan J, Dai Z, Li C, Hu X, Shen Q, Xue Y (2021) Sugar- and artificially sweetened beverages consumption linked to type 2 diabetes, cardiovascular diseases, and all-cause mortality: a systematic review and dose-response meta-analysis of prospective cohort studies. Nutrients. https://doi.org/10.3390/nu13082636
Rulis AM, Levitt JA (2009) FDA’S food ingredient approval process: safety assurance based on scientific assessment. Regul Toxicol Pharmacol 53(1):20–31. https://doi.org/10.1016/j.yrtph.2008.10.003
Magnuson BA, Roberts A, Nestmann ER (2017) Critical review of the current literature on the safety of sucralose. Food Chem Toxicol 106:324–355. https://doi.org/10.1016/j.fct.2017.05.047
Plaza-Diaz J, Pastor-Villaescusa B, Rueda-Robles A, Abadia-Molina F, Ruiz-Ojeda FJ (2020) Plausible biological interactions of low- and non-calorie sweeteners with the intestinal microbiota: an update of recent studies. Nutrients. https://doi.org/10.3390/nu12041153
Jang HJ, Kokrashvili Z, Theodorakis MJ, Carlson OD, Kim BJ, Zhou J, Kim HH, Xu X, Chan SL, Juhaszova M, Bernier M, Mosinger B, Margolskee RF, Egan JM (2007) Gut-expressed gustducin and taste receptors regulate secretion of glucagon-like peptide-1. Proc Natl Acad Sci U S A 104(38):15069–15074. https://doi.org/10.1073/pnas.0706890104
Suez J, Korem T, Zeevi D, Zilberman-Schapira G, Thaiss CA, Maza O, Israeli D, Zmora N, Gilad S, Weinberger A, Kuperman Y, Harmelin A, Kolodkin-Gal I, Shapiro H, Halpern Z, Segal E, Elinav E (2014) Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 514(7521):181–186. https://doi.org/10.1038/nature13793
Uebanso T, Ohnishi A, Kitayama R, Yoshimoto A, Nakahashi M, Shimohata T, Mawatari K, Takahashi A (2017) Effects of low-dose non-caloric sweetener consumption on gut microbiota in mice. Nutrients. https://doi.org/10.3390/nu9060560
Pepino MY, Tiemann CD, Patterson BW, Wice BM, Klein S (2013) Sucralose affects glycemic and hormonal responses to an oral glucose load. Diabetes Care 36(9):2530–2535. https://doi.org/10.2337/dc12-2221
Shi Q, Zhu X, Zhou J, Chen L (2018) Low intake of digestible carbohydrates ameliorates the duodenal absorption of carbohydrates in mice with glucose metabolic disorders induced by sucralose. Food Funct 9(12):6236–6244. https://doi.org/10.1039/c8fo02029a
Kim JY, Prescott J, Kim KO (2017) Emotional responses to sweet foods according to sweet liker status. Food Qual Prefer 59:1–7. https://doi.org/10.1016/j.foodqual.2017.01.013
Glendinning JI, Hart S, Lee H, Maleh J, Ortiz G, Ryu YS, Sanchez A, Shelling S, Williams N (2020) Low-calorie sweeteners cause only limited metabolic effects in mice. Am J Physiol Regul Integr Comp Physiol 318(1):R70–R80. https://doi.org/10.1152/ajpregu.00245.2019
Shi Q, Zhu X, Deng S (2021) Sweet taste receptor expression and its activation by sucralose to regulate glucose absorption in mouse duodenum. J Food Sci 86(2):540–545. https://doi.org/10.1111/1750-3841.14586
Margolskee RF, Dyer J, Kokrashvili Z, Salmon KS, Ilegems E, Daly K, Maillet EL, Ninomiya Y, Mosinger B, Shirazi-Beechey SP (2007) T1R3 and gustducin in gut sense sugars to regulate expression of Na+-glucose cotransporter 1. Proc Natl Acad Sci U S A 104(38):15075–15080. https://doi.org/10.1073/pnas.0706678104
Kojima I, Nakagawa Y (2011) The role of the sweet taste receptor in enteroendocrine cells and pancreatic beta-cells. Diabetes Metab J 35(5):451–457. https://doi.org/10.4093/dmj.2011.35.5.451
Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, Lustig RH, Sacks F, Steffen LM, Wylie-Rosett J, American heart association nutrition committee of the council on nutrition PA, metabolism, the council on E, Prevention (2009) Dietary sugars intake and cardiovascular health: a scientific statement from the american heart association. Circulation 120(11):1011–1020. https://doi.org/10.1161/CIRCULATIONAHA.109.192627
Bomback AS, Derebail VK, Shoham DA, Anderson CA, Steffen LM, Rosamond WD, Kshirsagar AV (2010) Sugar-sweetened soda consumption, hyperuricemia, and kidney disease. Kidney Int 77(7):609–616. https://doi.org/10.1038/ki.2009.500
Jurgens H, Haass W, Castaneda TR, Schurmann A, Koebnick C, Dombrowski F, Otto B, Nawrocki AR, Scherer PE, Spranger J, Ristow M, Joost HG, Havel PJ, Tschop MH (2005) Consuming fructose-sweetened beverages increases body adiposity in mice. Obes Res 13(7):1146–1156. https://doi.org/10.1038/oby.2005.136
Lindqvist A, de la Cour CD, Stegmark A, Håkanson R, Erlanson-Albertsson C (2005) Overeating of palatable food is associated with blunted leptin and ghrelin responses. Regul Pept 130(3):123–132. https://doi.org/10.1016/j.regpep.2005.05.002
Saltiel MY, Kuhre RE, Christiansen CB, Eliasen R, Conde-Frieboes KW, Rosenkilde MM, Holst JJ (2017) Sweet taste receptor activation in the Gut is of limited importance for glucose stimulated GLP1 and GIP secretion. Nutrients. https://doi.org/10.3390/nu9040418
Li X, Staszewski L, Xu H, Durick K, Zoller M, Adler E (2002) Human receptors for sweet and umami taste. Proc Natl Acad Sci U S A 99(7):4692–4696. https://doi.org/10.1073/pnas.072090199
Toft-Nielsen M-B, Damholt MB, Madsbad S, Hilsted LM, Hughes TE, Michelsen BK, Holst JJ (2001) Determinants of the impaired secretion of glucagon-like peptide-1 in type 2 diabetic patients. J Clin Endocrinol Metab 86(8):3717–3723. https://doi.org/10.1210/jcem.86.8.7750
Vollmer K, Holst JJ, Baller B, Ellrichmann M, Nauck MA, Schmidt WE, Meier JJ (2008) Predictors of incretin concentrations in subjects with normal, impaired, and diabetic glucose tolerance. Diabetes 57(3):678–687. https://doi.org/10.2337/db07-1124
Acknowledgements
None.
Funding
This work was supported by grants from the National Natural Science Foundation of China (Nos. 31972912, 82030026, and 31771666) the Jiangsu Provincial Department of Science and Technology (No. BK20211153), and the Fundamental Research Funds for the Central Universities (No. 020814380173).
Author information
Authors and Affiliations
Contributions
Conceptualization: XJ, XW, LC and HW; investigation: XW, LC, HW, JX, ZZ, XJ, JW, HZ, YS, YT, QY and QL; writing of the manuscript: XJ, YZ, JL; funding acquisition: XJ, YZ, JL; supervision: XJ, YZ, JL.
Corresponding authors
Ethics declarations
Conflict of interest
No potential conflict of interest was reported by the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, X., Cui, L., Wang, H. et al. Impact of dietary sucralose and sucrose-sweetened water intake on lipid and glucose metabolism in male mice. Eur J Nutr 62, 199–211 (2023). https://doi.org/10.1007/s00394-022-02980-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-02980-2