Abstract
Background
Women, older patients and non-White ethnic groups experience a substantial proportion of acute coronary syndromes (ACS), although they have been historically underrepresented in ACS randomized clinical trials (RCTs). To assess the influence of sex, age and race on major adverse cardiovascular events (MACE) and on heart failure events, we studied patients with type 2 diabetes in a large post-ACS trial (EXAMINE).
Methods
Differences in baseline characteristics and the respective composite endpoint of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke (MACE) and cardiovascular death or heart failure hospitalization (HF events) were evaluated by subgroups in a cohort of post-ACS patients with diabetes, using unadjusted and adjusted Cox regression modelling.
Results
The EXAMINE trial enrolled 5380 patients with 35% aged > 65, 32% female and 27% non-White. The risk of MACE was higher in non-White compared to White patients after adjustment for potential confounding (HR = 1.35; 95% CI 1.04–1.75), but there were no significant differences by sex and age (HR = 1.03; 95% CI 0.87–1.22 for women; HR = 1.14; 95% CI 0.96–1.35 for patients ≥ 65 years). The risk of HF events was higher in non-White patients (HR = 1.56; 95% CI 1.13–2.14), and in patients aged > 65 (HR = 1.33; 95% CI 1.07–1.66) and nominally so in women (HR = 1.23; 95% CI 0.99–1.52). The additive risk of each demographic factor (women, older age and non-White race) was greater for HF events in comparison with MACE. Moreover, non-White elderly patients consistently had poorer prognosis regardless of sex.
Conclusions
Older adults, women and non-White patients with diabetes who are post-ACS are often underrepresented in RCTs. The risk for HF events was higher in older and non-White patients, with a trend towards significance in women, whereas only non-White patients (and not women and older patients) were at higher risk for MACE. Future trials should enrich enrollment of these persons at risk.
Graphic abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of both diabetes mellitus and acute coronary syndrome (ACS) represents a significant burden to individuals and health-care systems [1, 2]. Compared to people without type 2 diabetes mellitus (T2D), patients with T2D having an ACS have poor prognosis [1,2,3]. Although women, older patients and non-White ethnic groups experience a substantial proportion of ACS in the real-world setting, they have been historically underrepresented in ACS randomized clinical trials (RCTs) [4], including those exclusively enrolling patients with T2D [5,6,7,8]. Several campaigns, coalitions, and programmes [9, 10] have been initiated with the aim of improving awareness, advocacy, and research for better representativeness in clinical trials of these patient categories [11] as well as to reduce cardiovascular (CV) outcomes based on the implementation of specific recommendations [12, 13]. Although previous studies have reported age-, sex- and race differences in management and outcomes of large cohorts of post-ACS patients [4, 11], there are limited data characterizing these disparities in specific cohorts of post-ACS patients with T2D.
In the light of recent major cardiovascular outcome trials showing successful treatment effects of newer glucose-lowering agents in high-risk patients with T2D [14, 15], there is a need to understand whether there are differences in the distribution of cardiovascular outcomes according to sex, age and race. Describing clinical characteristics and CV outcomes in these underrepresented groups, using data from recent post-ACS T2D trials might help informing the design of future RCTs.
Using a cohort of post-ACS patients with T2D from the EXAMINE (examination of cardiovascular outcomes with alogliptin vs standard of care) trial [16, 17] we aimed to: (a) describe the distribution and the clinical profile of women, older and non-White patients; (b) assess differences in the rate of two composite cardiovascular outcomes by subgroups of sex, age and race; and (c) evaluate the incremental risk of cardiovascular events based on the additive effect provided by each subgroup.
Methods
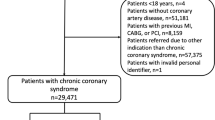
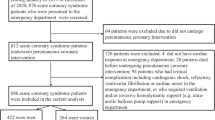
Study design
Details of the EXAMINE study (NCT00968708) design and primary findings have been previously published [16, 18]. A total of 5380 patients were randomly allocated to receive either alogliptin or placebo, administered in a double-blind fashion, in addition to standard-of-care treatment for T2D. In the overall population, alogliptin was non-inferior to placebo for the primary outcome of death from cardiovascular causes, non-fatal myocardial infarction, or non-fatal stroke [16].
The Steering Committee, consisting of academic members and three non-voting representatives of the sponsor (Takeda Development Center Americas), designed and oversaw the conduct of the trial. An independent data and safety monitoring committee monitored the trial and had access to the unblinded data. The EXAMINE trial was performed in accordance with the ethical principles contained in the Declaration of Helsinki. The appropriate national and institutional regulatory authorities and ethics committees approved the study design, and all participants provided written informed consent.
Study patients and intervention
Patients were eligible for enrolment if they had received a diagnosis of T2D, were receiving antidiabetic therapy (other than a DPP-4 inhibitor or GLP-1 analogue), and had had an ACS (either acute myocardial infarction [MI] or unstable angina requiring hospitalization) within 15–90 days before randomization. Further criteria for the diagnosis of T2D included a HbA1c level between 6.5 and 11.0% at screening, or if the antidiabetic regimen included insulin, a HbA1c concentration between 7.0 and 11.0%. Major exclusion criteria were type 1 diabetes, unstable cardiac disorders (e.g., New York Heart Association class IV heart failure, refractory angina, uncontrolled arrhythmias, critical valvular heart disease, or severe uncontrolled hypertension), and dialysis within 14 days before screening.
Institutional Review Board approval was obtained and all patients provided informed consent to participate in the trial. The EXAMINE trial was registered in ClinicalTrials.gov with the number NCT00968708.
Study outcomes
We evaluated two composite cardiovascular outcomes. The ischemic endpoint, or major adverse cardiovascular events (MACE), was a composite of CV death, nonfatal MI, or nonfatal stroke [16], whereas the heart failure endpoint (HF events) was a composite of CV death or heart failure hospitalization (HFH). Heart failure hospitalization was defined as an inpatient admission or an emergency department visit of more than 12 h with clinical manifestations of HF. An independent central adjudication committee adjudicated all the outcomes under investigation in this report (CV death, nonfatal MI, or nonfatal stroke, and HFH) [16]. The median (interquartile range) follow-up time was 1.5 (0.8, 2.1) and 1.6 (0.9, 2.1) years for each endpoint, respectively.
Statistical analysis
Differences in baseline clinical characteristics by sex, age and race were described as frequency (%) and compared using Chi-square tests for categorical data, whereas baseline continuous data were expressed as mean and standard deviation (SD) or median with interquartile range and compared using t tests or Wilcoxon rank sum tests, as appropriate.
Incidence rates for each study variable (sex, age and race) were estimated to obtain absolute risk measure using difference in rates (95% CI). Time-to-first-event curves for each outcome were obtained to compare subsets of patients by sex, age and race using the Kaplan–Meier method. Cox proportional hazards modelling was used to examine the association between cardiovascular outcomes and sex, age and race, estimating hazard ratios (HRs) and their 95% CI for each outcome. Based on previous publications [19,20,21,22], multivariate models were adjusted for sex, age, race, smoking, T2D duration, previous MI, previous HFH, previous stroke, atrial fibrillation, hypertension, systolic blood pressure, statin therapy, and study treatment (alogliptin or placebo) allocation. All models were stratified by geographic region and baseline renal function at baseline [16, 22], which assumes equal associations across strata but with a baseline hazard unique to each subset of patients [23, 24]. Data for multivariate complete case analyses were available for 5356 patients (99.6%). In addition to the main model, three extra models were conducted to adjust for some other confounders: (a) model one was adjusted by the previous set of co-variates and by the type of ACS (MI vs unstable angina requiring hospitalization) and the use percutaneous coronary intervention; (b) model two was adjusted for model one and some extra variables related to T2D treatment and co-morbidities, such as insulin and history of peripheral artery disease; and (c) model three was adjusted for model one and other secondary prevention medication, such as aspirin, beta blockers and angiotensin-converting enzyme inhibitor or angiotensin receptor blocker.
To evaluate the prognostic value of eight patient profiles based on their sex, age and race (23 = 8 combinations), we computed linear combinations of the three relevant coefficients to obtain adjusted point estimates with their 95% CI. Additionally, a risk score with one point for each demographic risk category (women, older and non-White patients) was used to evaluate the increasing risk of MACE and HF events with the increasing number of prognostic factors.
The two-tailed significance level was set at p < 0.05. STATA software version 15.1 (Stata Corp, College Station, TX, USA) was used to perform the analyses and produce most graphs.
Results
Baseline characteristics by sex, age and race
There were 1729 (32%) women, 1907 (35%) older patients and 1471 (27%) non-White patients (1089 Asian, including Indians, 216 Black and 166 from other minorities). Among them, only 1759 (33%) patients were not part of any historically underrepresented group (male, young or White). Baseline clinical features, medical history, and concomitant medications at randomisation by sex, age and race are shown in Table 1. Briefly, women were older than men (mean age 63.3 ± 9.9 vs 59.8 ± 9.7 years, p < 0.001) and were more often White (75.7% vs 71.2%, p < 0.001). They also had a longer duration of T2D with a higher percentage on insulin although no difference in HbA1c values. Women received less antiplatelet medications and statins in comparison to men, but a higher percentage were receiving diuretics. Older patients were more frequently White (76.1% vs 70.8%, p < 0.001) and had more severe T2D. Older patients received less concomitant CV medications (antiplatelet therapy, statins and beta-blockers) than younger patients, but a higher proportion were receiving diuretics as well. In comparison to White patients, non-White patients had a shorter duration of T2D and were less frequently on insulin. There was a higher percentage of non-White patients taking antiplatelet therapies and statins, but a smaller proportion of patients taking beta blockers, ACEI/ARBs and diuretics. Of note, some by-race differences in treatments might be subjected to local clinical practices (i.e., insulin is less often used in some Asian countries).
Baseline clinical biomarkers at randomisation by sex, age and race are shown in Table 2. Women, older patients and non-White patients had lower eGFRs and higher baseline BNP concentration in comparison to men, younger participants and White patients, respectively. Troponin levels were higher in male, older and non-White participants, in comparison to female, younger and White patients, respectively.
Study outcomes
Survival curves for each outcome according to sex, age and race are shown in Figs. 1 and 2. Briefly, women and older patients showed higher rates of MACE (CV death, nonfatal MI or stroke) than men and younger patients, respectively, whereas there was no significant difference between White and non-White patients. In contrast, there was a higher rate of the heart failure events (CV death or HFH) in all the traditionally underrepresented groups (women, older and non-White) compared to the more commonly represented groups. The unadjusted incidence rates and incidence rate differences for both MACE and HF events according to age, sex and race, are shown in Table 3. Of note, within the non-White patient group, the Black patient subgroup in EXAMINE had the highest risk of both MACE and heart failure hospitalization.
The association between each group and the two composite endpoints were modified after taking into account potential confounders and stratifying the model for geographic region and baseline renal function at baseline (Fig. 3). For MACE, there was no difference in adjusted risk between women and men (HR = 1.03, 95% CI 0.87–1.22, p = 0.76) nor between older and younger patients (HR = 1.14, 95% CI 0.96–1.36, p = 0.13), whereas there was a higher adjusted risk of MACE for non-White in comparison with White patients (HR = 1.35, 95% CI 1.04–1.75, p = 0.023). In contrast, for the composite of HF events, there was a nearly significant increased risk for women compared to men (HR = 1.23, 95% CI 0.99–1.52, p = 0.057), whereas there was a higher risk for older patients (HR = 1.33 95% CI 1.07–1.66, p = 0.009) and for non-White patients (HR = 1.56, 95% CI 1.13–2.14, p = 0.006). Online Resource 1 shows consistent findings using others set of co-variates for adjustment, such as type of ACS, insulin or secondary prevention medications.
Forest plot with crude and adjusted HRs for MACE (a) and HF events (b) by sex, age and race. Both unadjusted and adjusted HR are plotted in this figure. Cox proportional-hazards models were used to evaluate the time to the first occurrence of both composite outcomes among all randomly assigned patients, with stratification according to geographic region and renal function at baseline [16]. Multivariate models were adjusted for sex, age, race, smoking, diabetes duration, previous MI, previous HF hospitalization, previous stroke, atrial fibrillation, hypertension, systolic blood pressure, statin therapy, and study treatment (alogliptin or placebo) allocation, available for 5356 patients (99.6%)
Risk of events by patient profile: additive value of sex, age and race
An increasing risk of both MACE and HF events was observed with increasing number of risk factors (women, older and non-White patients) (Fig. 4). Moreover, we estimated the individualized risk for each of the eight potential patient profiles by adding the adjusted risk provided from each risk factor (Fig. 5). In comparison with a younger White male (reference group not belonging to any historically underrepresented group), the adjusted risk for MACE was increased by 58% for an older, non-White female. Similarly, for HF events, the adjusted risk was increased by 108% and by 155% in non-White older male and non-White older female vs the reference group (White younger men), respectively.
Incremental risk by patient profile based on sex, age and race. Adjusted HRs for all combinations of age, age and race are plotted in this figure. Wald tests for linear combinations using cox proportional-hazards models were used to evaluate the time to the first occurrence of both composite outcomes among all randomly assigned patients, with stratification according to geographic region and renal function at baseline [16] and adjustment for sex, age, race, smoking, diabetes duration, previous MI, previous HF hospitalization, previous stroke, atrial fibrillation, hypertension, systolic blood pressure, statin therapy, and study treatment (alogliptin or placebo) allocation. This complete case analysis was performed using 5356 patients (99.6%)
Discussion
In this new analysis from the EXAMINE trial, the risk of developing a MACE was higher in non-White compared to White patients after adjustment for potential confounding, but there were no significant differences in outcomes by sex and age. In contrast, the risk of HF events was higher in older and non-White patients, and nominally so also in women. Moreover, the additive risk of each risk factor (women, older and non-White patients) was larger for the HF endpoint in comparison to MACE. When combined, race and age had additive impact on prognosis with non-White older patients demonstrating the worst prognosis in both men and women.
Adequate demographic representation within clinical trials is critical for the generalizability of their findings [4]. Although women, older patients and racial minorities were underrepresented in the EXAMINE trial, they did have a higher percentage of representation in comparison to many of the earlier post-ACS trials. In a recent systematic review [4], the percentage of women and non-White patients in ACS trials published between 2011 and 2018 were 26.8% and 15%, respectively, whereas these percentages were higher in the EXAMINE trial (32% and 27%, respectively). In contrast, the mean age was comparable between these 460 trials and EXAMINE (62.9 vs 60.9 years). In patients with T2D and ACS from the ELIXA (Evaluation of Lixisenatide in Acute Coronary Syndrome (ELIXA) trial [25], women, older patients and racial minorities represented around 31%, 34%, and 25%, respectively, which were similar percentages to what we observed in our T2D, ACS population from the EXAMINE trial.
The issue of representativeness is relevant, because each subgroup has a different CV profile and a different incidence rates for MACE and HF events. In general, in our study, women and elderly have greater CV burden but were receiving less protective CV drugs at baseline. It is notable that the non-White patients who were primarily from Asian countries had lower CV risk clinical profiles (shorter duration of T2D and less insulin, less hypertension, lower rates of smoking and prior heart failure). Perhaps this might explain the difference in risk of both MACE and HF events within the non-White patient group, where the Asian subgroup had similar rates of events and the Black patient subgroup in EXAMINE had the highest risk of both MACE and heart failure hospitalization. Although non-White participants had higher BNP and troponin levels, and had similar levels of HbA1c, also suggesting a higher risk profile at baseline, some differences between countries as to who was receiving standard of care at baseline might also have played a role in some of our findings.
Based on our findings, reporting data according to sex, age and race in a post-ACS population of patients with T2D have revealed a higher number of subgroup differences in HF events than in MACE. In addition to the obvious clinical implications, this information might be helpful for the design of future RCTs by setting a more accurate sample size estimation as well as by selecting an adequate endpoint. In the light of our findings, the inclusion of HF events should be considered in composite outcomes for future RCTs in post-ACS T2D patients.
Describing clinical characteristics and treatment effect (subgroup analyses) by sex, age and race improves the interpretation of the findings and have the potential to eventually translate into more personalized guidelines [11]. Strong evidence already exists that T2D confers a higher excess risk of CV diseases in women than in men, with women having a 27% higher relative risk of stroke and a 44% higher relative risk of coronary heart disease compared with men [1]. Whereas it is known that older patients will have poorer outcomes than younger patients [4, 11], there is an urgent need for evidence on race-based CV outcome differences in patients with T2D [26]. Understanding by-sex, age, and race differences in terms of number and type of outcomes should be useful for clinical-decision making in light of recent trial-based evidence of new antidiabetic drugs reducing cardiovascular outcomes including the glucagon-like peptide 1 receptor agonists (GLP1-RA) and sodium–glucose cotransporter-2 inhibitors (SGLT2i) [14, 27]. Nevertheless, there is little evidence regarding differences in treatment effect by demographics due to the overall lack of statistical power of these analyses, which is enhanced by the gap in full representation of the subgroups.
In our study, the risks of CV outcomes (either MACE or HF endpoint, or both) were additive in women, older and non-White patients, despite some of the subgroups did not show statistical significance by themselves when evaluated separately. Although the incremental risk associated with aging is biologically plausible and expected, the mechanisms that underpin these sex- and race differences are not fully understood. Some of the excess risk may be the result of a disparity in the management and treatment of diabetes and ACS, to the detriment of women, and non-White patients [28, 29]. Older patients may also receive sub-optimal therapy more frequently. However, accruing evidence suggests that real biological differences might also drive these differences, particularly for sex- and age-related differences [1, 11]. Furthermore, sex-, age- and race differences are well-documented in the response to drugs {pharmacokinetics and pharmacodynamic change with body fat distribution and renal function, among many other factors [23, 30, 31] }, though there is not much evidence on the influence of these mechanisms from CV outcome trials. Importantly, there may also be differences in healthcare access and income inequality that might influence outcomes by subgroups [26, 32].
Study limitations
Our study should be considered within the context of its limitations. Our findings can be only extrapolated to patients with T2D who had a recent ACS, and the prognostic relationship with each sex-, age- and race-clinical profile may not be applicable to non-T2D patients with ACS. Furthermore, there were few non-White female patients, resulting in wide CIs around the incremental estimated risk for both younger and older patients. Some relevant data were missing, such as the type of myocardial infarction (with or without ST-segment elevation), the severity of the coronary disease, or whether some patients received fibrinolysis. We did not reported details about the type of composition of secondary prevention medications, though we adjusted the model for these factors in several ways. Moreover, some unknown residual confounding might not be addressed by our statistical approach, despite our efforts to adjust for known risk factors with the use of multivariate modelling. Nevertheless, we stratified the Cox models by geographic regions, given the well-known differences in both management and clinical outcomes in patients with ACS [33, 34].
Finally, the study was underpowered to evaluate interactions between subgroups (i.e., sex×age) as well as to use a higher cut-off value for selecting older patients. Nevertheless, this is one of the largest T2D cohorts showing the influence of sex, age and race on coronary and heart failure events in this setting.
Conclusions
There is a need to improve trial representativeness of historically underrepresented groups based on sex, age and race in registries and trials of post-ACS patients with T2D, given that they have different clinical profiles and some of them have differences in the incidence of subsequent cardiovascular outcomes. The risk of MACE was higher in non-White compared to White patients after adjustment for potential confounding, but there were no significant differences by sex and age. In contrast, the risk of HF events was higher in older and non-White patients, and nominally so for women compared to men. The additive risk of multiple risk category (women, older and non-White patients) was larger for the HF endpoint in comparison with the ischemic endpoint. These findings are clinically relevant in the light of recent evidence from major cardiovascular outcome trials showing successful treatment effects of glucose-lowering agents in high-risk patients with T2D [14, 15] and might have an impact on the design of future RCTs in post-ACS patients with T2D. Although there is no clear evidence of different treatment effects by subgroups, there are differences in rates of outcomes which might benefit some subgroups in absolute terms.
Our work adds information to the importance in enrolling older study participants, more women and ethnically diverse patients in CV clinical trials to enhance representativeness, and facilitate applicability of trial results to these under-represented groups of patients. Enrolling older, female and non-White patients may contribute to enriching the event rate in CV trials, and may decrease the trial sample size requirements.
References
Peters SAE, Huxley RR, Sattar N, Woodward M (2015) Sex differences in the excess risk of cardiovascular diseases associated with type 2 diabetes: potential explanations and clinical implications. Curr Cardiovasc Risk Rep 9:1–7. https://doi.org/10.1007/s12170-015-0462-5
Rossello X, Ferreira JP, McMurray JJ et al (2019) Editor’s choice-impact of insulin-treated diabetes on cardiovascular outcomes following high-risk myocardial infarction. Eur Hear J Acute Cardiovasc Care 8:231–241. https://doi.org/10.1177/2048872618803701
Cosentino F, Grant PJ, Aboyans V et al (2020) 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J 41:255–323. https://doi.org/10.1093/eurheartj/ehz486
Tahhan AS, Vaduganathan M, Greene SJ et al (2020) Enrollment of older patients, women, and racial/ethnic minority groups in contemporary acute coronary syndrome clinical trials: a systematic review. JAMA Cardiol 5:714–722. https://doi.org/10.1001/jamacardio.2020.0359
Scirica BM, Bhatt DL, Braunwald E et al (2013) Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med 369:1317–1326. https://doi.org/10.1056/NEJMoa1307684
Green JB, Bethel MA, Armstrong PW et al (2015) Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med 373:232–242. https://doi.org/10.1056/NEJMoa1501352
Rosenstock J, Perkovic V, Johansen OE et al (2019) Effect of linagliptin vs placebo on major cardiovascular events in adults with type 2 diabetes and high cardiovascular and renal risk: the carmelina randomized clinical trial. JAMA 321:69–79. https://doi.org/10.1001/jama.2018.18269
Rosenstock J, Kahn SE, Johansen OE et al (2019) Effect of linagliptin vs glimepiride on major adverse cardiovascular outcomes in patients with type 2 diabetes: the CAROLINA randomized clinical trial. JAMA 322:1155–1166. https://doi.org/10.1001/jama.2019.13772
Go Red for Women-American heart association. In: https://www.goredforwomen.org/en/about-go-red-for-women. https://www.goredforwomen.org/en/about-go-red-for-women. Accessed 27 Aug 2020
Women’s heart alliance. https://www.womensheartalliance.org/about/. Accessed 27 Aug 2020
Lüscher TF, Miller VM, Bairey Merz CN, Crea F (2020) Diversity is richness: why data reporting according to sex, age, and ethnicity matters. Eur Heart J 41:3117–3121. https://doi.org/10.1093/eurheartj/ehaa277
Mosca L, Benjamin EJ, Berra K et al (2011) Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American heart association. Circulation 123:1243–1262. https://doi.org/10.1161/CIR.0b013e31820faaf8
Williams B, Mancia G, Spiering W et al (2018) 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 39:3021–3104
Rossello X, Yellon DM (2017) A new era in the management of type 2 diabetes: is cardioprotection at long last a reality? Int J Cardiol 228:198–200. https://doi.org/10.1016/j.ijcard.2016.11.246
Kato ET, Silverman MG, Mosenzon O et al (2019) Effect of dapagliflozin on heart failure and mortality in type 2 diabetes mellitus. Circulation 139:2528–2536. https://doi.org/10.1161/CIRCULATIONAHA.119.040130
White WB, Cannon CP, Heller SR et al (2013) Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med 369:1327–1335. https://doi.org/10.1056/NEJMoa1305889
Zannad F, Cannon CP, Cushman WC et al (2015) Heart failure and mortality outcomes in patients with type 2 diabetes taking alogliptin versus placebo in EXAMINE: a multicentre, randomised, double-blind trial. Lancet 385:2067–2076. https://doi.org/10.1016/S0140-6736(14)62225-X
White WB, Bakris GL, Bergenstal RM et al (2011) Examination of cardiovascular outcomes with alogliptin versus standard of care in patients with type 2 diabetes mellitus and acute coronary syndrome (EXAMINE): a cardiovascular safety study of the dipeptidyl peptidase 4 inhibitor alogliptin in patients with type 2 diabetes with acute coronary syndrome. Am Heart J 162:620–626. https://doi.org/10.1016/j.ahj.2011.08.004
Hwang Y-C, Morrow DA, Cannon CP et al (2018) High-sensitivity C-reactive protein, low-density lipoprotein cholesterol and cardiovascular outcomes in patients with type 2 diabetes in the EXAMINE (examination of cardiovascular outcomes with alogliptin versus standard of care) trial. Diabetes Obes Metab 20:654–659. https://doi.org/10.1111/dom.13136
White WB, Jalil F, Cushman WC et al (2018) Average clinician-measured blood pressures and cardiovascular outcomes in patients with type 2 diabetes mellitus and ischemic heart disease in the EXAMINE trial. J Am Heart Assoc 7:e009114. https://doi.org/10.1161/JAHA.118.009114
Cavender MA, White WB, Jarolim P et al (2017) Serial measurement of high-sensitivity troponin I and cardiovascular outcomes in patients with type 2 diabetes mellitus in the EXAMINE trial (examination of cardiovascular outcomes with alogliptin versus standard of care). Circulation 135:1911–1921. https://doi.org/10.1161/CIRCULATIONAHA.116.024632
White WB, Kupfer S, Zannad F et al (2016) Cardiovascular mortality in patients with type 2 diabetes and recent acute coronary syndromes from the EXAMINE trial. Diabetes Care 39:1267–1273. https://doi.org/10.2337/dc16-0303
Rossello X, Ferreira JP, Pocock SJ et al (2020) Sex differences in mineralocorticoid receptor antagonist trials: a pooled analysis of three large clinical trials. Eur J Heart Fail 22:834–844. https://doi.org/10.1002/ejhf.1740
Rossello X, Ariti C, Pocock SJ et al (2019) Impact of mineralocorticoid receptor antagonists on the risk of sudden cardiac death in patients with heart failure and left-ventricular systolic dysfunction: an individual patient-level meta-analysis of three randomized-controlled trials. Clin Res Cardiol 108:477–486. https://doi.org/10.1007/s00392-018-1378-0
Pfeffer MA, Claggett B, Diaz R et al (2015) Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med 373:2247–2257. https://doi.org/10.1056/NEJMoa1509225
Brown AF, Gregg EW, Stevens MR et al (2005) Race, ethnicity, socioeconomic position, and quality of care for adults with diabetes enrolled in managed care: the translating research into action for diabetes (TRIAD) study. Diabetes Care 28:2864–2870. https://doi.org/10.2337/diacare.28.12.2864
Zelniker TA, Wiviott SD, Raz I et al (2019) Comparison of the effects of glucagon-like peptide receptor agonists and sodium-glucose cotransporter 2 inhibitors for prevention of major adverse cardiovascular and renal outcomes in type 2 diabetes mellitus: systematic review and meta-analysis of cardiovascular outcomes trials. Circulation 139:2022–2031. https://doi.org/10.1161/CIRCULATIONAHA.118.038868
Correa-de-Araujo R, Stevens B, Moy E et al (2006) Gender differences across racial and ethnic groups in the quality of care for acute myocardial infarction and heart failure associated with comorbidities. Women’s Health Issues 16:44–55. https://doi.org/10.1016/j.whi.2005.04.003
Correa-de-Araujo R, McDermott K, Moy E (2006) Gender differences across racial and ethnic groups in the quality of care for diabetes. Women’s Health Issues 16:56–65. https://doi.org/10.1016/j.whi.2005.08.003
Santema BT, Ouwerkerk W, Tromp J et al (2019) Identifying optimal doses of heart failure medications in men compared with women: a prospective, observational, cohort study. Lancet 394:1254–1263. https://doi.org/10.1016/s0140-6736(19)31792-1
Ferreira JP, Rossello X, Eschalier R et al (2019) MRAs in elderly HF patients: individual patient-data meta-analysis of RALES, EMPAHSIS-HF, and TOPCAT. JACC Heart Fail 7:1012–1021. https://doi.org/10.1016/j.jchf.2019.08.017
Ferreira JP, Girerd N, Rossignol P, Zannad F (2015) Geographic differences in heart failure trials. Eur J Heart Fail 17:893–905. https://doi.org/10.1002/ejhf.326
Rosselló X, Huo Y, Pocock S et al (2017) Global geographical variations in ST-segment elevation myocardial infarction management and post-discharge mortality. Int J Cardiol 245:27–34. https://doi.org/10.1016/j.ijcard.2017.07.039
Bueno H, Rossello X, Pocock S et al (2018) Regional variations in hospital management and post-discharge mortality in patients with non-ST-segment elevation acute coronary syndrome. Clin Res Cardiol 107:836–844. https://doi.org/10.1007/s00392-018-1254-y
Acknowledgements
The EXAMINE trial was funded by Takeda.
Funding
The EXAMINE trial was funded by Takeda.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
XR, JPF, FC, ZL and CM have nothing to disclose. AS has received support from the FRSQ-Junior 1 clinician scientist award, the Alberta Innovates Health Solution Clinician Scientist fellowship, the European Society of Cardiology Young Investigator research grant, and has received support from Roche Diagnostics, Astrazeneca, Boeringer-Ingelheim, Novartis, Servier, Novo-Nordisk, and the Canadian Cardiovascular Society Bayer Vascular award. Dr Ferreira has received consulting fees from Boehringer-Ingelheim. GB reports other from Merck, Novo Nordisk, Vasular Dynamics, Bayer, Ionis, Alnylam, KBP Biosciences, outside the submitted work. CPC reports in calendar years 2018–2020: (1) Research Grants from: Amgen, Boehringer-Ingelheim (BI), Bristol-Myers Squibb (BMS), Daiichi Sankyo, Janssen, Merck, Novo Nordisk, Pfizer, and (2) Consulting fees from Aegerion, Alnylam, Amarin, Amgen, Applied Therapeutics, Ascendia, BI, BMS, Corvidia, Eli Lilly, HLS Therapeutics, Innovent, Janssen, Kowa, Merck, Pfizer, Rhoshan, Sanofi. WBW reports personal fees from Takeda Millenium Pharmaceuticals, outside the submitted work. FZ reports steering committee personal fees from Applied Therapeutics, Amgen, Bayer, Boehringer, Novartis, Janssen, Cellprothera and CVRx, advisory board personal fees from, AstraZeneca, Vifor Fresenius, Cardior, Cereno pharmaceutical, Corvidia, Merck, Myokardia, NovoNordisk and Owkin, stock options at Cereno and G3Pharmaceutical, and being the founder of the Global Cardiovascular Clinical Trialist Forum.
Ethical approval
The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
Consent to participate
Informed consents were obtained from each patient.
Consent for publication
All authors agree with de publications of the present article.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rossello, X., Ferreira, J.P., Caimari, F. et al. Influence of sex, age and race on coronary and heart failure events in patients with diabetes and post-acute coronary syndrome. Clin Res Cardiol 110, 1612–1624 (2021). https://doi.org/10.1007/s00392-021-01859-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-021-01859-2