Abstract
Background
Therapeutic variability not explained by patient clinical characteristics is a potential source of avoidable morbidity and mortality. We aimed to explore regional variability in the management and mortality of patients with non-ST-segment elevation acute coronary syndromes (NSTE-ACS).
Methods and results
11,931 NSTE-ACS hospital survivors enrolled in two prospective registries: EPICOR [5625 patients, 555 hospitals, 20 countries in Europe (E) and Latin America (LA), September 2010–March 2011] and EPICOR Asia (6306 patients, 218 hospitals, 8 countries, June 2011–May 2012) were compared among eight pre-defined regions: Northern E (NE), Southern E (SE), Eastern E (EE); Latin America (LA); China (CN), India (IN), South-East Asia (SA), and South Korea, Hong Kong and Singapore (KS). Patient characteristics differed between regions: mean age (lowest 59 years, IN; highest 65.9 years, SE), diabetes (21.4% NE; 35.5% IN) and smoking (32% NE; 62% IN). Variations in dual antiplatelet therapy at discharge (lowest 83.1%, IN; highest 97.5%, SA), coronary angiography (53.9% SA; 90.6% KS), percutaneous coronary intervention (35.8% SA; 78.6% KS) and coronary artery bypass graft (0.7% KS; 5.7% NE) were observed. Unadjusted 2-year mortality ranged between 3.8% in KS and 11.7% in SE. Two-year, risk-adjusted mortality rates ranged between 5.1% (95% confidence interval 2.9–7.3%) in KS to 10.5% (8.3–12.7%) in LA.
Conclusion
Wide regional variations in patient features, hospital care, coronary revascularization and post-discharge mortality are present among patients hospitalized for NSTE-ACS. Focused regional interventions to improve the quality of care for NSTE-ACS patients are still needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Variations in hospital and post-discharge mortality related to the quality of hospital care have been described for patients with non-ST-segment elevation acute coronary syndromes (NSTE-ACS) [1,2,3,4]. The increase in the use of coronary angiography and revascularization in these patients, for instance, seems to explain part of the reduction in 6-month mortality observed in the United Kingdom (UK) during recent years [5]. Despite this fact, wide regional variations in hospital care of these patients have been described at national and international levels, including medical therapies and invasive strategy [6,7,8,9,10,11,12]. We aimed to better understand the relationship between different geographic patterns in hospital care of patients with NSTE-ACS in general and the rates of use of coronary revascularization in particular, and the risk of death after hospital discharge.
Methods
In total, 23,490 patients with non-fatal NSTE-ACS were enrolled between September 2010 and March 2011 from 555 hospitals in 20 countries across Europe and Latin America (LA) (EPICOR [long-tErm follow-uP of antithrombotic management patterns In acute CORonary syndrome patients], NCT01171404, n = 10,568), and between June 2011 and May 2012 from 219 hospitals across eight countries in Asia (EPICOR Asia, NCT01361386, n = 12,922). The protocol and case record form of both studies were almost identical and their rationale and designs have been described elsewhere [13, 14]. The current study is a pre-defined secondary objective of both studies. Of these patients, only those with NSTE-ACS were included in the present analysis; 5625 from EPICOR and 6306 from EPICOR Asia.
Definitions used in EPICOR have been presented elsewhere [13, 14]. Diagnosis of NSTE-ACS included non-ST-segment elevation myocardial infarction (diagnosis based on the presence of chest pain or discomfort, lack of persistent ST-segment elevation, left bundle branch block or intraventricular conduction disturbances, and elevation of cardiac biomarkers (creatinine kinase-isoenzyme MB and troponins) with at least one value above the 99th percentile of the upper reference limit), and unstable angina (diagnosis based on the presence of angina symptoms at rest or on minimal exercise, and transient ST-T changes, with no significant increase in biomarkers of necrosis but objective evidence of ischemia by non-invasive imaging or significant coronary stenosis on angiography). An invasive management was defined as the realization of at least a diagnostic coronary angiography during index hospitalization with or without further coronary revascularization.
Eight geographical regions were defined for regional analyses (Fig. 1): Southern Europe (SE) (France, Greece, Italy and Spain), Northern Europe (NE) (Belgium, Denmark, Finland, Germany, Luxembourg, The Netherlands, Norway, and UK), Eastern Europe (EE) (Poland, Romania, Slovenia and Turkey), Latin America (LA) (Argentina, Brazil, Mexico and Venezuela), China (CN), India (IN), South-East Asia (SA) (Malaysia, Vietnam and Thailand) and South Korea, Hong Kong and Singapore (KS) [15]. Supplementary Table S1 shows the number of patients enrolled per country and region.
Statistical analysis
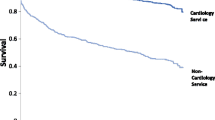
Continuous parameters are mostly presented as mean (SD) and regions are compared using one-way analysis of variance. Ordinal and continuous highly skewed distributed variables are presented by median and inter-quartile range, and regions are compared using the nonparametric Kruskal–Wallis test. Categorical data are expressed as percentages and compared between regions using Chi-square tests. Cumulative probability of all-cause post-discharge mortality by region was plotted using the Kaplan–Meier method.
We used a Poisson regression model to estimate 2-year mortality rates for each region. Poisson regression modelling is used for count outcomes during a given interval of time (i.e., number of deaths in 2-year follow-up) and provides an estimation of incidence rates. In this study, we obtained both crude and adjusted estimates of 2-year mortality for each region. The latter was adjusted for 16 known predictors of 2-year mortality in the overall study population, which were obtained from the same cohort in our EPICOR 2-year risk [16] and were (ranked by the strength of its association with 2-year mortality): older age (fitted as continuous), low left ventricular ejection fraction (≥ 40, 39–30 and < 30%), lack of coronary revascularization or reperfusion therapy during hospitalization, elevated serum creatinine at admission (fitted as continuous if ≥ 1.2 mg/dL), poor EuroQol Five Dimensions score (0, 1, ≥ 2), low hemoglobin at admission (≥ 13, 12–11 and < 11 g/dL), previous cardiac disease, previous chronic obstructive pulmonary disease, elevated blood glucose at admission (fitted as continuous if ≥ 140 mg/dL), diuretics prescribed at discharge, male sex, lower educational level (no formal, primary, secondary, university), aldosterone inhibitor prescribed at discharge, body mass index < 20 kg/m2, in-hospital cardiac complications, and Killip class (I, II and III–IV). To allow for missing values for each co-variate, multiple imputation was used, as described in the EPICOR 2-year mortality risk score publication [16], which included the Von Hippel method of transformation then imputation for continuous variables [17].
All probability (p) values were 2-sided and values of < 0.05 were considered as statistically significant. All statistical analyses were performed using STATA software, version 13.1 (Stata Corp, College Station, TX, USA). GraphPad Prism version 6.00 (GraphPad Software, La Jolla California) was used to produce the figures.
Results
The study cohort comprised a total of 11,931 consecutive NSTE-ACS patients who survived to hospital discharge. Supplementary Fig. 1 depicts the distribution of patients across the eight regions. Substantial differences in patient baseline profiles across regions were observed (Table 1; Fig. 1). Mean patient age ranged between 59.0 years (IN) and 65.9 years (SE) and the proportion of men between 66.2% in SA and 79.1% in IN. The prevalence of risk factors also varied by region, with current smoking ranging between 32.0% (NE) and 62.0% (IN), and diabetes between 21.4% (NE) and 35.5% (IN). Although Killip class I was more frequently reported in E and LA compared with the Asian regions, the rate of missing values for this parameter among the latter was high (CN 70.4%, IN 46.9%, KS 44.3%, SA 31.9%).
There were also regional differences in the characteristics of the participating hospitals where these patients were treated (Supplementary Table S2). In general, a higher proportion of Asian participants were initially admitted to hospitals with catheterization laboratory facilities compared to E and LA patients. The percentage of on-site cardiac surgery was also higher in Asian and LA enrolling hospitals compared to E. Many centers had a coronary or intensive care unit, ranging from 87.9% (SA) to 100% in IN and KS.
In-hospital management
Medication prescription patterns at discharge (Table 2) differed between regions. Dual antiplatelet therapy was prescribed at discharge in most patients in each region, ranging between 77.5% (IN) and 89.7% (SA), with aspirin and clopidogrel used in the majority of cases. Prescription of statins at discharge was high, between 80.4% in KS and 93.3% in CN. IN showed the lowest prescription rates for beta-blockers (58.0%) and angiotensin converting enzyme inhibitors (45.1%) and EE the highest (91.3% and 82.7%, respectively).
Assessment of left ventricular ejection fraction before discharge was not universal, ranging from 51.6% in IN to 84.8% in SE (Supplementary Table S2). The proportion of patients with severely depressed left ventricular ejection fraction also varied, being the lowest in CN (3.1%) and the highest in SA (12.8%).
An invasive strategy was employed in a majority of patients but ranged between 53.9% in SA and 90.6% in KS. Coronary revascularization before discharge basically followed the same trend (Supplementary Table S2, Fig. 1), ranging between 38.6% in SA and 79.3% in KS. The type of revascularization also differed but less importantly. The majority of patients (58.7%) were treated with percutaneous coronary angioplasty (between 35.1% in LA and 78.6% in KS) and 2.4% (from 0.7% in KS to 5.7% in NE) underwent surgical revascularization. The median length of hospital stay was 6 days (4–10 days) but varied widely between the 3 days observed in IN and 9 days in CN.
Post-discharge mortality risk
After discharge, 81 patients (0.7%) died by any cause during the first 30 days and 684 within the first 2 years, so the all-cause, 2-year post-discharge mortality risk was 5.7% (95% confidence interval [CI], 5.3–6.2%), ranging between 3.8% in KS and 11.7% in SA (Fig. 2, Supplementary Table S3). After comprehensive adjustment for baseline characteristics, comorbidities and therapies employed in hospital with a validated model (http://www.acsrisk.org/) [16], differences between regions in adjusted all-cause, 2-year mortality risk remained significant (p < 0.001) (Fig. 2, Supplementary Table S3), with the lowest rate observed in KS (5.1%; 95% CI, 2.9–7.3%) and the highest in LA (10.5%; 95% CI, 8.3–12.7%) (Fig. 3).
Unadjusted and risk-adjusted, 2-year, all-cause mortality rate by region. Two-year mortality risk adjusted for: age, sex, body mass index, Killip class; creatinine, hemoglobin, and blood glucose at admission; left ventricular ejection fraction; in-hospital cardiac complications; coronary revascularization; quality of life; prior cardiac disease or chronic obstructive pulmonary disease; educational level; diuretics or aldosterone inhibitors prescribed at discharge
Discussion
The present study, evaluating a large geographic area from the world, shows an important variability in the hospital management of NSTE-ACS patients, which is not explained only by differences in the clinical profile of the patients, and is associated with differences as high as twofold between some regions in post-discharge adjusted survival.
Important regional variations were described in medical therapy for acute coronary syndrome several years ago [7, 8, 11, 12, 18]. Our study shows that, although some general progression has occurred, important regional differences in the management of NSTE-ACS persist worldwide. The rates in the use of dual antiplatelet therapy, statins, and angiotensin converting enzyme inhibitors is higher than previously described, and the variability is lower. However, very important differences in the use of an invasive strategy and coronary revascularization during initial hospitalization remain. This seems to be relevant as regions with the highest rate of use of evidence-based therapies—medications and coronary revascularization—show the lowest rate of 2-year mortality, while regions with higher rates of medical management show higher 2-year mortality rates.
Although previous studies performed by us [6, 16] and others [5, 19] showed that early revascularization is associated with a significantly lower post-discharge mortality risk in NSTE-ACS patients even after adjustment for confounders, and the current results of the study are consistent with these studies, our results also point out that other factors matter. Indeed, after extensive adjustment for baseline characteristics and treatments, there still are significant residual regional differences in mortality risk. Whether this is due to uncontrolled intrinsic patient differences, other differences in management or unmeasured confounders needs further study. We speculate that the regional differences observed in a number of performance measures, such as use of dual antiplatelet therapy, statins, or other drugs, and the use of an invasive strategy and coronary revascularization, which have been described as quality indicators [20], and validated as prognostic markers [2, 3], may be a reflection of wider differences in the quality of care provided by the different healthcare systems. The influence of limited health resources in poor performing countries also needs to be considered.
One interesting observation from our study is the discrepancy between the immediate availability of coronary angiography (i.e., proportion of patients admitted to centers with a catheterization laboratory facility) and the actual access to treatment. The extreme examples are NE with the lowest proportion of hospitals with an on-site catheterization laboratory or on-site cardiac surgery on one hand and the highest levels of coronary angiography, percutaneous coronary intervention and coronary artery bypass graft, as well as with the lowest 2-year adjusted mortality rates on the other hand. On the opposite side, a number of regions, mostly from Asia, where only hospitals with a catheterization laboratory facility participated in the registry, showed much lower rates of coronary angiography or revascularization and also some of the highest post-discharge mortality rates. This discrepancy highlights that quality of care is not only a matter of availability of resources but also depends on knowledge of guidelines and application of its recommendations, organization of care, including effective referral systems from secondary centers to tertiary centers with full coronary revascularization facilities, and issues related to social security coverage and/or need for reimbursement for procedures. Therefore, revascularization rates are probably not the only cause for the better survival of patients with NSTE-ACS in some regions but rather a surrogate for a higher quality of the healthcare system. This comprises factors such as other issues related to acute care, quality of revascularization, post-discharge compliance with lifestyle changes, secondary prevention therapies or cardiac rehabilitation. In fact, a number of other critical issues related to access of care must be considered when such different healthcare systems are compared, including public insurance coverage, public versus private health, reimbursement for procedures (i.e., coronary angiography and/or revascularization), devices (i.e., coronary stents) or drugs (i.e., secondary prevention drugs). Local healthcare authorities should be aware of this fact [21, 22].
Our results have also implications for research, emphasizing the importance of having diverse regional representation in randomized clinical trials towards testing therapies or strategies for NSTE-ACS patients; results may be modulated by local practice patterns as evident from a number of trials. There is also the need to try and reasonably standardize treatment practice across regions to avoid excessive confounding associated with regional variation in clinical practice and outcomes.
Several limitations should be considered in this study. (1) It is not possible to rule out the possibility that differences in post-discharge mortality may be explained in part by differences in hospital mortality (i.e., initial survival of higher risk patients may translate into higher post-discharge mortality) but interestingly, the regions with highest baseline risk did not show the highest post-discharge mortality rate. (2) The lack of information on the cause of death precludes the inference of a potential mechanism for a survival advantage. (3) There might be unexplored variability both within and between countries, rather than regions. (4) While both registries were designed to recruit representative patients from centers also representative of the type of hospitals (i.e., tertiary) within each country, regional differences in center characteristics suggests that some bias in regard to the type of hospitals recruiting patients from EPICOR and EPICOR Asia may play a role. Hence, some caution is needed to extrapolate our findings since these centers might not be fully representative of the reality of each country. (5) Despite its wide representation, this is not a global study as important regions are not represented. However, it is likely that similar findings would have been found had more regions been included in the study.
In conclusion, important geographic variations in patient features, initial medical care, coronary revascularization and post-discharge mortality are present among patients hospitalized for NSTE-ACS, which remain after extensive adjustment for confounders. More research is needed to define the best opportunities to improve the quality of care for these patients at each healthcare system.
References
Peterson ED, Roe MT, Mulgund J, DeLong ER, Lytle BL et al (2006) Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA 295(16):1912–1920
Bebb O, Hall M, Fox KAA, Dondo TB, Timmis A et al (2017) Performance of hospitals according to the ESC ACCA quality indicators and 30-day mortality for acute myocardial infarction: national cohort study using the United Kingdom Myocardial Ischaemia National Audit Project (MINAP) register. Eur Heart J 38(13):974–982
Schiele F, Gale CP, Simon T, Fox KAA, Bueno H, et al. (2017) Assessment of quality indicators for acute myocardial infarction in the FAST-MI (French Registry of Acute ST-Elevation or Non-ST-Elevation Myocardial Infarction) registries. Circ Cardiovasc Qual Outcomes 10(6):pii: e003336
Bueno H, Sinnaeve P, Annemans L, Danchin N, Licour M et al (2016) Opportunities for improvement in anti-thrombotic therapy and other strategies for the management of acute coronary syndromes: Insights from EPICOR, an international study of current practice patterns. Eur Heart J Acute Cardiovasc Care 5(1):3–12
Hall M, Dondo TB, Yan AT, Goodman SG, Bueno H et al (2016) Association of clinical factors and therapeutic strategies with improvements in survival following non-ST-elevation myocardial infarction, 2003–2013. JAMA 316(10):1073–1082
Bueno H, Pocock S, Medina J, Annemans L, Danchin N et al. (2017) Heterogeneity in medically managed patients with non-ST-segment elevation acute coronary syndromes. Rev Esp Cardiol. pii:S1885-585:30454–30456
Puymirat E, Battler A, Birkhead J, Bueno H, Clemmensen P et al (2013) Euro Heart Survey 2009 Snapshot: regional variations in presentation and management of patients with AMI in 47 countries. Eur Heart J Acute Cardiovasc Care 2(4):359–370
Mandelzweig L, Battler A, Boyko V, Bueno H, Danchin N et al (2006) The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J 27(19):2285–2293
Budaj A, Brieger D, Steg PG, Goodman SG, Dabbous OH et al (2003) Global patterns of use of antithrombotic and antiplatelet therapies in patients with acute coronary syndromes: Insights from the Global Registry of Acute Coronary Events (GRACE). Am Heart J 146(6):999–1006
Fox KA, Goodman SG, Klein W, Brieger D, Steg PG et al (2002) Management of acute coronary syndromes. Variations in practice and outcome; findings from the Global Registry of Acute Coronary Events (GRACE). Eur Heart J 23(15):1177–1189
Fox KA, Goodman S, Bigonzi F, Le Louer V, Cohen M (2000) Inter-regional differences and outcome in unstable angina; analysis of the international ESSENCE trial. Efficacy and safety of subcutaneous enoxaparin in non-Q-wave coronary events. Eur Heart J 21(17):1433–1439
Boersma E, Pieper KS, Steyerberg EW, Wilcox RG, Chang WC et al (2000) Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation. Results from an international trial of 9461 patients. PURSUIT Investigators Circulation 101(22):2557–2567
Bueno H, Danchin N, Tafalla M, Bernaud C, Annemans L et al (2013) EPICOR (long-tErm follow-up of antithrombotic management Patterns In acute CORonary syndrome patients) study: Rationale, design, and baseline characteristics. Am Heart J 165(1):8–14
Huo Y, Lee SW, Sawhney JP, Kim HS, Krittayaphong R et al (2015) Rationale, design, and baseline characteristics of the EPICOR Asia Study (Long-tErm follow-uP of antithrombotic management patterns In Acute CORonary Syndrome patients in Asia). Clin Cardiol 38(9):511–519
Rossello X, Huo Y, Pocock S, Van de Werf F, Chin CT et al (2017) Global geographical variations in ST-segment elevation myocardial infarction management and post-discharge mortality. Int J Cardiol 245:27–34
Pocock SJ, Huo Y, Van de Werf F, Newsome S, Chin CT et al. (2017) Predicting two-year mortality from discharge after acute coronary syndrome: an internationally-based risk score. Eur Heart J Acute Cardiovasc Care 2048872617719638 (epub ahead of print)
Von Hippel PT (2009) How to impute interactions, squares, and other transformed variables. Sociol Methodol 39:265–291
O’Connor GT, Quinton HB, Traven ND, Ramunno LD, Dodds TA et al (1999) Geographic variation in the treatment of acute myocardial infarction: the Cooperative Cardiovascular Project. JAMA 281(7):627–633
Feldman L, Steg PG, Amsallem M, Puymirat E, Sorbets E et al (2017) Editor’s choice-medically managed patients with non-ST-elevation acute myocardial infarction have heterogeneous outcomes, based on performance of angiography and extent of coronary artery disease. Eur Heart J Acute Cardiovasc Care 6(3):262–271
Schiele F, Gale CP, Bonnefoy E, Capuano F, Claeys MJ et al (2017) Quality indicators for acute myocardial infarction: a position paper of the Acute Cardiovascular Care Association. Eur Heart J Acute Cardiovasc Care 6(1):34–59
Chan MY, Du X, Eccleston D, Ma C, Mohanan PP et al (2016) Acute coronary syndrome in the Asia-Pacific region. Int J Cardiol 202:861–869
Huo Y, Thompson P, Buddhari W, Ge J, Harding S et al (2015) Challenges and solutions in medically managed ACS in the Asia-Pacific region: expert recommendations from the Asia-Pacific ACS Medical Management Working Group. Int J Cardiol 183:63–75
Acknowledgements
Editorial support was provided by Carl V Felton PhD of Prime (Knutsford, Cheshire, UK), supported by AstraZeneca. Ultimate responsibility for opinions, conclusions, and data interpretation lies with the author. X.R. has received support from the SEC-CNIC CARDIOJOVEN fellowship program.
Funding
EPICOR and EPICOR Asia are funded by AstraZeneca. Being a non-interventional study, no drugs were supplied or funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H.B. has received consulting fees from Abbott, AstraZeneca, Bayer, BMS, Novartis and Pfizer; speaking fees from AstraZeneca, Bayer, BMS-Pfizer, Ferrer, Novartis, Servier and MEDSCAPE-the heart.org; and fees for research activities from AstraZeneca, BMS, Janssen, Novartis; S.P. has received research funding from AstraZeneca. F.v.d.W. has received consulting fees and research grants from Boehringer Ingelheim and Merck, and consulting fees from Roche, Sanofi-Aventis, AstraZeneca, and The Medicines Company. C.T.C. has received research support from Eli Lilly, honoraria from Medtronic, and has been a consultant or advisory board member for AstraZeneca. N.D. has received consulting or speaking fees from AstraZeneca, BMS, Boehringer-Ingelheim, GSK, MSD-Schering Plough, Novartis, Pierre Fabre, Pfizer, Roche, Sanofi-Aventis, Servier, Takeda, and The Medicines Company. J.M. and A.V. are employees of AstraZeneca. X.R., S.W-L.L. and Y.H. have nothing to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bueno, H., Rossello, X., Pocock, S. et al. Regional variations in hospital management and post-discharge mortality in patients with non-ST-segment elevation acute coronary syndrome. Clin Res Cardiol 107, 836–844 (2018). https://doi.org/10.1007/s00392-018-1254-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-018-1254-y