Abstract
Background
Sudden cardiac death (SCD) is an important cause of death in patients with left-ventricular systolic dysfunction (LVSD). Mineralocorticoid receptor antagonists (MRAs) may attenuate this risk. We aimed to assess the impact of MRAs on SCD in patients with LVSD.
Methods
A fixed-effect meta-analysis at individual patient-level was performed using 11,032 patients recruited in three placebo-controlled randomized trials: Randomized Aldactone Evaluation Study (RALES), Eplerenone Post Acute Myocardial Infarction Heart Failure Efficacy and Survival Study (EPHESUS), and Eplerenone in Mild Patients Hospitalization and Survival Study in Heart Failure (EMPHASIS-HF). Treatment effect was determined using a Cox proportional hazards model stratified by study.
Results
Patients receiving MRAs were at lower risk of SCD compared with placebo-treated patients after a mean follow-up of 18 months (HR 0.77, 95% CI 0.66–0.89). This effect was consistent across trials and did not change substantially after adjustment for 14 baseline co-variates. Moreover, the benefits of MRAs were consistent across study subgroups, except for a greater effect in those < 65 years old and those using beta-blockers. Using stratified analyses, we also found a consistent effect in relevant subsets of patient defined by heart failure cause, NYHA class or LVEF ≤ 35%.
Conclusions
MRAs reduce the risk for SCD by 23% in patients with heart failure and LVSD. In these patients, the use of MRAs, on top of other evidence-based medications, should be optimized. It might be useful to re-assess the benefit of implantable cardiac defibrillator (ICD) placement, as ICD treatment effect was evaluated in trials enrolling patients not receiving MRAs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with symptomatic heart failure (HF) and left-ventricular systolic dysfunction (LVSD) are at high risk for sudden cardiac death (SCD). Over the last 2 decades, the sequential introduction of evidence-based medications, such as beta-blockers [1], angiotensin-converting enzyme inhibitors (ACEIs) [2], angiotensin-receptor blockers (ARBs), and more recently, sacubitril/valsartan, a angiotensin-receptor-neprilysin inhibitor (ARNI) [3], has paralleled a decline in the rate of SCD [4]. In this new context, the cost-effectiveness of some interventions reducing SCD is currently under intense debate. Recently, the Danish Study to Assess the Efficacy of ICDs in Patients with Nonischemic Systolic Heart Failure on Mortality (DANISH) trial has cast doubt on the benefit of implantable cardiac defibrillators (ICDs) when added to contemporary optimal medical therapy in patients with non-ischemic systolic HF [5]. In the light of this evolving clinical scenario, it seems imperative to collate and review the evidence that mineralocorticoid receptor antagonist (MRAs) prevents SCD in patients with HF and LVSD, especially as there is evidence that these agents continue to be underused in routine practice.
The current guidelines already recommend MRAs in patients with symptomatic HF and LVSD [6, 7]. Based on the Randomized Aldactone Evaluation Study (RALES) [8] and the Eplerenone in Mild Patients Hospitalization and Survival Study in Heart Failure (EMPHASIS-HF) [9] trials, MRAs are recommended in patients in New York Heart Association (NYHA) class II–IV and left-ventricular ejection fraction (LVEF) ≤ 35%. Based on the Eplerenone Post Acute Myocardial Infarction Heart Failure Efficacy and Survival Study (EPHESUS) trial, MRAs are also recommended in post-myocardial infarction patients with LVEF ≤ 40% and symptomatic HF or a history of diabetes, unless contraindicated [10]. Despite this evidence, MRAs are particularly underprescribed in patients with HF [11,12,13], thus potentially providing room for further improvement in SCD prevention by simply increasing its use. There are solid biological grounds to hypothesise that MRAs can decrease the rate of SCD. This rationale is based on their ability to prevent electrical remodelling [14], improve ventricular remodelling enhancing the effect provided by either ACEIs or ARBs [15], and decrease the substrate for arrhythmias by diminishing the effect of aldosterone, norepinephrine, and cortisol in the heart [16, 17].
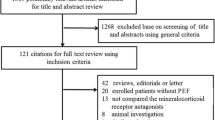
To assess whether MRAs decrease the risk of SCD in patients with symptomatic HF and LVSD, we performed a meta-analysis at individual patient level using data from three large randomized clinical trials (RCTs): RALES, EPHESUS, and EMPHASIS-HF. The aim of this meta-analysis was to estimate the overall effect of MRAs on SCD, as well as to evaluate whether this benefit was consistent across patient subgroups. Further emphasis was put to demonstrate the efficacy of MRAs in relevant subsets of patients with clinical implications, such as those differing in the cause of HF, NYHA functional class, and LVEF.
Methods
Study design, setting, and participants
Each individual RCT was conducted in accordance with the Declaration of Helsinki and approved by site ethics committees. All participants gave written informed consent to participate in the RCTs.
Table 1 depicts the main study design features for each trial, such as treatment being tested (spironolactone or eplerenone) and its regime, the entry criteria, the primary endpoint, and the mean follow-up.
Study outcomes
Major clinical outcomes were centrally adjudicated by endpoint committees and defined by the conventional criteria (definitions have been published in the respective studies) [8,9,10]. In this study, we analysed SCD, which was consistently defined across trials (Table S1).
Statistical analysis
A fixed-effect model for a one-stage individual patient data meta-analysis was conducted based on the assumption that the underlying treatment effect was similar in the three studies and that the main reason for variation in the estimates between studies was sampling error [18].
Baseline clinical characteristics of patients were either summarised by treatment group or by study with means and SD for continuous variables, with frequencies and percentages for categorical variables, and hazard ratios (HRs) with their 95% confidence interval (95% CI) for treatment effect estimates. Incidence rates for MRA and placebo, as well as incidence rates ratios were also estimated for each trial and for the overall pooled sample. Time-to-first-event curves for SCD were obtained for each trial and for the pooled data using the Kaplan–Meier method and compared using the log-rank test. Univariate Cox proportional hazards’ modelling was used to explore the association of the intervention and SCD for each trial. A Cox model stratified by study was used to obtain the overall HR for this individual patient meta-analysis (assuming equal effects across strata but with a baseline hazard unique to each study) [19]. To obtain an adjusted estimate of the effect of MRA and test for consistency across trials, an adjusted model using the set of harmonized co-variates was built for each trial as well as for the stratified model (complete case analysis). The variables for this multivariate model were chosen according to their clinical relevance or historical association with the outcome in the previous studies [2, 4, 20], and were MRA, age, male gender, systolic blood pressure (SBP), diabetes, hypertension, atrial fibrillation, nonischemic cause, NYHA class III–IV, LVEF, potassium, estimated glomerular filtration rate, digoxin, ACE inhibitors, and beta-blocker treatment. Subgroup analyses for SCD were performed with a Cox model stratified by study, with terms for treatment, subgroup, and interaction between treatment and subgroup. A trend test for interaction was used for age. Further stratified analyses were performed in clinically relevant patient subsets with meaningful implications: cause of HF, NYHA class, and LVEF.
To identify the variation of treatment effect estimates between trials over and above of the variation expected by chance alone (statistical heterogeneity), visual inspection of individual effect sizes and overall effect size estimations and their 95% CI were used. Moreover, the distribution of baseline characteristics of patients across trials was also evaluated. Heterogeneity was tested using a two degree of freedom Wald test of the overall interaction study x treatment.
All statistical analyses were performed using the STATA/SE software, version 15.1 (Stata Corp, College Station, TX, USA).
Results
Baseline characteristics
Individual patient data from the three randomised trials (RALES, EPHESUS, and EMPHASIS-HF) were available for 11,032 subjects. Of them, 5505 patients were randomly assigned to MRA (822 received spironolactone and 4684 received eplerenone) and 5527 were assigned to placebo. The mean follow-up was 18 months, although each RCT had originally a different follow-up duration (Table 1). Baseline clinical features, medical history, and medications at randomisation according to randomised intervention (pooled across the three trials) are shown in Table 2, and were well matched between both groups. Baseline clinical characteristics by trial are detailed in Table S2.
Treatment effect
Summary estimates for SCD occurring up to 50 months after randomisation in the three pooled trials are shown in Fig. 1. The overall unadjusted HR (95% CI) was 0.77 (0.66–0.89) and there was a consistent treatment effect across trials, although in EMPHASIS-HF, the smallest trial, the confidence intervals around the point estimate for the treatment effect were broader. Cumulative time-to-first-event curves for patients randomly assigned to MRA vs placebo from the individual trial data are depicted in Fig. 2, and the overall and by-trial incidence rate ratios are shown in Table S3. The contribution of reduced risk of SCD to the overall reduction of all-cause mortality was consistent across the three trials (Table S4).
Forest plot with crude and adjusted HRs for SCD. Adjusted HRs are plotted in this figure, although both unadjusted and adjusted HR are reported in the right side. Model adjusted for gender, systolic blood pressure, diabetes, hypertension, atrial fibrillation, nonischemic cause, NYHA class III–IV, LVEF, potassium, estimated glomerular filtration rate digoxin, ACEI or ARB, and beta-blockers
Adjusted treatment effect
After adjustment for baseline co-variates, the treatment effect remained consistent across the three trials: the HR (95% CI) was 0.70 (0.53–0.94) for RALES, 0.80 (0.64–1.00) for EPHESUS, and 0.74 (0.52–1.05) for EMPHASIS-HF (Fig. 1 and Table S5). In the same vein, the multivariable analysis demonstrated evidence of an overall MRA effect for SCD, HR (95% CI) of 0.76 (0.65, 0.89), P = 0.001 (Fig. 1).
Subgroup and stratified analysis
The consistency of the treatment effect was assessed among 13 subgroups. The effect in each subgroup was analysed with the use of a Cox proportional hazards model stratified by study, without adjustment for co-variates. There was some evidence for two treatment-by-subgroup interactions: age showed a linear relationship (P = 0.04 for interaction) (< 65 years. patients had the highest treatment effect) and the concomitant use of beta-blocker showed a synergistic effect (interaction P value 0.01). Differences between beta-blocker and nonbeta-blocker users are illustrated in Table S6. Briefly, MRAs were well randomized between patients with and without beta-blockers (around 50% use in both groups, P = 0.89). However, patients receiving beta-blockers were younger, in lower NYHA functional class and had higher LVEF. They had also higher percentage of ACEI/ARB, aspirin and statin prescriptions, and lower percentages of diuretics and digoxin use. The remaining interaction tests demonstrated a consistent treatment effect across subgroups (Fig. 3). Importantly, the effect of MRAs to prevent SCD was similar between patients from ischemic and nonischemic causes: unadjusted HR (95% CI) were 0.77 (0.65–0.90) and 0.76 (0.51–1.12), respectively. We also found a consistent effect between patients in NYHA class I–II (HR of 0.76, 95% CI 0.62–0.93) and III–IV (HR of 0.78, 95% CI 0.61–0.99). In the subset of patients who had higher LVEF, the rate of SCD was substantially lower than in the other two groups with poorer LVEF and the small number of sudden deaths in patients with a higher LVEF did not allow robust testing of the effect of MRA treatment on SCD in this subgroup. Results regarding MRA effect consistency in patients with different HF cause, NYHA class, and LVEF are displayed in Fig. 3, but further details can be found in the stratified analyses as displayed in Table S7.
Statistical heterogeneity
The individual effect size for each trial and overall effect size estimations and their 95% CI depicted in Fig. 1 already suggest the lack of substantial statistical heterogeneity. The distributions of baseline characteristics of patients across trials that can influence MRA effect were also evaluated in the supplemental material. To further investigate the variation of treatment effect estimates between trials, the Wald test of the overall interaction study x treatment suggested a lack of interaction (P = 0.834), therefore, supporting the hypothesis of little heterogeneity.
Discussion
In this meta-analysis at individual patient-level including 11,302 subjects with symptomatic HF and LVSD, we found that patients receiving MRAs had 23% lower risk of SCD compared with placebo-treated. Importantly, this effect was consistent across trials and the overall result did not change substantially after adjustment for baseline co-variates. Moreover, the benefits of MRAs were consistent across study subgroups, except for a greater effect in those < 65 years old and those using beta-blockers.
In this study, subjects randomized to receive an MRA had a risk reduction for SCD of more than 20% across the RCTs. Of note, there was a chronological decline in the incidence rate of SCD from RALES to EMPHASIS-HF, which is consistent with recent findings illustrating a reduction of SCD rates over time [4]. There were, however, other differences between trials that may be justified by their different underlying population. In accordance with the previous reports from the VALsartan In Acute myocardial iNfarcTion (VALIANT) trial [21], the increased risk of SCD in post-myocardial infarction (EPHESUS population) was higher in the first 3 months, whilst, for RALES and EMPHASIS-HF, the risk was quite linear. There is a gap in incidence rates between RALES and EMPHASIS-HF that can be explained by the functional severity of the underlying study population (patients with NYHA class III–IV vs II, respectively) as well as by the differences in percentages of concomitant medications between trials (i.e., beta-blockers were used in ~ 10% of patients in RALES, whilst they were used in ~ 85% of patients in EMPHASIS-HF). In any case, despite the absolute difference in rates has been declining over time, the incidence rate ratio has been constant over the same period, suggesting that MRAs are useful to prevent SCD in a broad-spectrum of patients and despite contemporaneous concurrent background therapy. Notably, the overall effect of MRA on preventing SCD did not change substantially after adjustment for baseline co-variates.
The magnitude of SCD reduction using MRA described in our study is in accordance with two previous meta-analyses, which used aggregated data in exceedingly heterogeneous populations [17, 22]. Bapoje et al. included small clinical trials assessing surrogate or soft clinical endpoints (i.e., LV function and exercise tolerance) in patients with LVEF < 45% [17], whilst Le et al. also included patients with preserved LVEF [22]. Using a relatively homogenous population of patients with HF and LVSD, our pooled data set was a unique opportunity to assess the robustness of our findings in clinically relevant subsets of patients.
In the subgroup analyses, the benefits of MRAs were consistent across patient subsets, except for age and beta-blockers’ use. Younger patients benefit more from MRAs, and the most likely explanation of this finding is competing causes of nonsudden and noncardiac death in elderly patients. In the case of beta-blockers’ use, MRAs appeared to have a synergistic effect when administered simultaneously (35% reduction of SCD), whilst a little effect was observed in those not taking beta-blockers. This finding may, as well, be confounded by indication and because patients not taking beta-blockers had a higher risk profile for SCD, also with competing causes of nonsudden and noncardiac death. Although the treatment randomization covers potential confounders by indication, one has to take into account that beta-blockers’ use can change over time during the follow-up period and we lacked information which could allow for a time-updated analysis. In any case, beta-blocker therapy is guideline IA indication in HFrEF, and MRAs are indicated on top of beta-blockers, maximizing the clinical benefit, including on SCD.
In the stratified analyses, the value of MRA to prevent SCD was robustly demonstrated across strata of relevant patient subsets. MRAs showed to similarly prevent SCD in both ischemic and nonischemic HF patients. This is particularly relevant in the light of the results of the DANISH trial and the controversy that it raised about the role of ICD therapy in nonischemic patients taking the standard-of-care medication. Evidence for the benefit of an ICD comes from older studies in which patients were not receiving contemporary background medical therapy, such as the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) trial, which evaluated ICD and amiodarone therapies and found similar benefit in ICD placement among patients with HF from ischemic or nonischemic causes [23]. In our analyses, MRAs were of clear benefit in nonischemic patients in whom the benefit of an ICD is now less certain.
The benefit of MRAs was also similar in patients with NYHA functional class I–II symptoms compared to those in NYHA functional class III–IV. This finding is particularly relevant in patients with mild-to-moderate functional class, as they constitute a large proportion of HF patients in clinical practice and they are more likely to die from SCD than from worsening HF [1, 3]. For LVEF, which is one of the most powerful predictors of SCD [21] and is a major component of guideline-based indications for receiving primary prevention ICD among patients with symptomatic HF [6, 7], the effect of MRA was similar in patients with a LVEF ≤ 30% and in those with an LVEF 31–35%. Because of the small number of sudden deaths in patients with an LVEF higher than 35%, we could not evaluate the effect of MRA therapy on SCD in these individuals. Moreover, all of these patients came from one trial (EPHESUS).
The incremental reduction of more than 20% in SCD using MRA treatment relative to placebo-control has clear clinical implications. Although several therapies have proven to reduce SCD in symptomatic patients with LVSD, their implementation in clinical practice is still suboptimal. In this context, MRAs are a particularly underused medication in patients with heart failure [12]—i.e., in the Aliskiren Trial to Minimize Outcomes in Patients with Heart Failure (ATMOSPHERE) trial, MRA was taken by less of the 38% of the study population [24]. It is a further cause for concern the fact that some patients are not receiving guideline-recommended medical therapy at the time of ICD implantation. In a 2011 registry, 25.7% of the first-time ICD recipients were reported as not receiving optimal medical therapy at the time of device implantation, despite no documented treatment contraindication [25]. In an attempt to quantify the potential survival benefits that could result if guideline-recommended therapies were universally applied to all eligible patients with HF in the US [26], Fonarow et al. showed that the largest potential benefits in terms of lives saved would result from improving the use of MRAs. Overall, it seems reasonable to believe that a substantial number of SCD might be avoided by optimal implementation of MRAs. However, caution should be taken when interpreting our results, as we lack information on the use of ICDs in RALES and EPHESUS and only a limited number of patients in EMPHASIS-HF received an ICD.
At the time when the effectiveness of ICDs might be questioned due to changes in contemporary background medical therapy and the declining risk of SCD [4, 5], our data reinforce the need to fully utilize the existing treatment armamentarium in HF patients with LVSD. Given the rate of under prescription of MRAs, the poor cost-effectiveness of ICD therapy in primary prevention [27], the complications with these devices [28], and limited access to them in some settings, it seems imperative to first improve the implementation of MRAs and other evidence-based therapies and then re-assess the benefit of ICD placement as ICD treatment effect was assessed in patients which were not treated with MRA. Importantly, the relative efficacy of MRAs on SCD was consistent across HF severity and presentations, and to the consistent relative risk reduction in all-cause mortality across trials, which should be contrasted with the lack of efficacy of ICD in patients with severely symptomatic HF (NYHA class IV) and early after myocardial infarction. In any case, MRAs and ICDs prevent SCD through different therapeutic pathways, and thus, their combination may offer additive effect. MRAs also improve symptoms and reduce hospital admissions which ICDs do not [29]. Future research should also focus on assessing whether the use of MRAs, on top of beta-blockers and ACEI/ARB, may prevent adequate ICD shocks in patients with HF and LVSD.
There are several underlying mechanisms potentially explaining the substantial reduction in the risk of SCD with MRAs in patients with symptomatic HF and LVSD described in this meta-analysis. In animal models, the pharmacologic suppression of the renin–angiotensin–aldosterone axis attenuates HF-related ventricular electric remodelling and, thus, lowers the threshold for tachyarrhythmias [30]. There is also evidence that MRAs block the effect of aldosterone on select calcium and potassium cellular currents, prolonging the ventricular action potential duration and reducing vulnerability to ventricular arrhythmias [14, 16]. In addition, aldosterone antagonism can enhance the effect of either ACEI or ARBs on ventricular remodelling [15], as well as decrease the substrate for ventricular arrhythmias by attenuating the effects on fibrosis of norepinephrine and cortisol in cardiomyocytes [16, 17]. Raising serum potassium concentration through reduced urinary potassium loss, thereby reducing the risk of hypokalemia and its associated arrhythmic risk, has been postulated as an alternative mechanism [20, 31]. In a retrospective study of the Studies of Left-Ventricular Dysfunction (SOLVD) trial, the use of potassium-sparing diuretics attenuated the higher risk of arrhythmic death associated with use of potassium-losing sparing diuretics [32]. One study has also shown the evidence of a ~ threefold increased mortality risk in patient with HF and hypokalemia [33] and another meta-analysis has reported that the use of MRAs significantly prevents the occurrence of hypokalemia [34]. Further research is needed to assess whether the underlying protective mechanism to avoid SCDs is through the increase of potassium levels—i.e., using mediation analysis and assessing a variety of clinical outcomes.
Limitations
This study should be viewed in the context of its limitations. In this meta-analysis, we did not include all randomized clinical trials assessing the impact of MRAs on SCD, although our study population represents > 95% of the patients included in RCTs assessing MRA in HF patients with LVSD [17]. Our analysis at individual patient-level allowed co-variate adjustment, subgroup analyses, and stratified assessments. Caution should also be exercised when extrapolating our results to patients with renal impairment: the RCTs under evaluation excluded patients with moderate-to-severe renal dysfunction and hyperkalemia. RALES and EPHESUS trials excluded patients with serum creatinine > 2.5 mg/dL, whilst EMPHASIS-HF excluded patients with estimated glomerular filtration rate < 30 mL/min per 1.73 m2. Subjects with baseline serum potassium concentration > 5 mEq/L were also excluded from the three RCTs. Therefore, while MRAs reduce the risk of SCD, they can also, paradoxically, induce fatal cardiac arrhythmia by causing hyperkalemia. However, with careful monitoring, the risk of hyperkalemia is not increased, as shown in the trials and in a Scottish population-based longitudinal study [35]. In addition, the use of concomitant use of nonabsorbed potassium binders, such as patiromer, might be considered in patients with chronic kidney disease who were receiving MRAs and who had hyperkalemia [36]. Finally, our results are based on the assumption that both spironolactone and eplerenone provide the same treatment effect. Although spironolactone and eplerenone differ in their molecular structure, pharmacokinetics, and pharmacodynamics, it is generally believed that the benefits of different MRAs represent a ‘class effect’ [37]. ICD use was not reported in RALES and EPHESUS, but these devices were not in routine use at the time that these trials were randomized, and ICDs were implanted in only around 13% of patients in EMPHASIS-HF.
Conclusions
In this meta-analysis using data at individual patient level, we found that MRA treatment leads to a 23% reduction in the risk of SCD in symptomatic HF patients with LVSD, compared with placebo. Importantly, this effect was consistent across trials and did not change substantially after adjustment for baseline co-variates. Using stratified analyses, we showed a consistent effect of MRAs in patient with different HF cause, NYHA functional class, and LVEF ≤ 35%.
References
MERIT-HF-Investigators (1999) Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL randomised intervention trial in congestive heart failure (MERIT-HF). Lancet 353:2001–2007
Domanski MJ, Exner DV, Borkowf CB et al (1999) Effect of angiotensin converting enzyme inhibition on sudden cardiac death in patients following acute myocardial infarction. A meta-analysis of randomized clinical trials. J Am Coll Cardiol 33:598–604
Desai AS, McMurray JJV, Packer M et al (2015) Effect of the angiotensin-receptor-neprilysin inhibitor LCZ696 compared with enalapril on mode of death in heart failure patients. Eur Heart J 36:1990–1997. https://doi.org/10.1093/eurheartj/ehv186
Shen L, Jhund PS, Petrie MC et al (2017) Declining risk of sudden death in heart failure. N Engl J Med 377:41–51. https://doi.org/10.1056/NEJMoa1609758
Køber L, Thune JJ, Nielsen JC et al (2016) Defibrillator implantation in patients with nonischemic systolic heart failure. N Engl J Med 375:1221–1230. https://doi.org/10.1056/NEJMoa1608029
Ponikowski P, Voors AA, Anker SD et al (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37:2129–2200. https://doi.org/10.1093/eurheartj/ehw128
Yancy CW, Jessup M, Bozkurt B et al (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 62:e147–e239. https://doi.org/10.1016/j.jacc.2013.05.019
Pitt B, Zannad F, Remme WJ et al (1999) The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med 341:709–717. https://doi.org/10.1056/NEJM199909023411001
Zannad F, McMurray JJV, Krum H et al (2011) Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med 364:11–21. https://doi.org/10.1056/NEJMoa1009492
Pitt B, Remme W, Zannad F et al (2003) Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 348:1309–1321. https://doi.org/10.1056/NEJMoa030207
Bossard M, Binbraik Y, Beygui F et al (2018) Mineralocorticoid receptor antagonists in patients with acute myocardial infarction—a systematic review and meta-analysis of randomized trials. Am Heart J 195:60–69. https://doi.org/10.1016/j.ahj.2017.09.010
Guglin M, Awad KE, Polavaram L, Vankayala H (2007) Aldosterone antagonists: the most underutilized class of heart failure medications. Am J Cardiovasc Drugs 7:75–79
Bistola V, Simitsis P, Farmakis D et al (2018) Association of mineralocorticoid receptor antagonist use and in-hospital outcomes in patients with acute heart failure. Clin Res Cardiol 107:76–86. https://doi.org/10.1007/s00392-017-1161-7
Perrier E, Kerfant B-G, Lalevee N et al (2004) Mineralocorticoid receptor antagonism prevents the electrical remodeling that precedes cellular hypertrophy after myocardial infarction. Circulation 110:776–783. https://doi.org/10.1161/01.CIR.0000138973.55605.38
Pitt B (1995) “Escape” of aldosterone production in patients with left ventricular dysfunction treated with an angiotensin converting enzyme inhibitor: implications for therapy. Cardiovasc drugs Ther 9:145–149
Ouvrard-Pascaud A, Sainte-Marie Y, Bénitah J-P et al (2005) Conditional mineralocorticoid receptor expression in the heart leads to life-threatening arrhythmias. Circulation 111:3025–3033. https://doi.org/10.1161/CIRCULATIONAHA.104.503706
Bapoje SR, Bahia A, Hokanson JE et al (2013) Effects of mineralocorticoid receptor antagonists on the risk of sudden cardiac death in patients with left ventricular systolic dysfunction: a meta-analysis of randomized controlled trials. Circ Heart Fail 6:166–173. https://doi.org/10.1161/CIRCHEARTFAILURE.112.000003
da Costa BR, Jüni P (2014) Systematic reviews and meta-analyses of randomized trials: principles and pitfalls. Eur Heart J 41:3336–3345. https://doi.org/10.1093/eurheartj/ehu424
Riley RD, Lambert PC, Abo-Zaid G (2010) Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ 340:c221
Rossignol P, Girerd N, Bakris G et al (2017) Impact of eplerenone on cardiovascular outcomes in heart failure patients with hypokalaemia. Eur J Heart Fail 19:792–799. https://doi.org/10.1002/ejhf.688
Solomon SD, Zelenkofske S, McMurray JJV et al (2005) Sudden death in patients with myocardial infarction and left ventricular dysfunction, heart failure, or both. N Engl J Med 352:2581–2588. https://doi.org/10.1056/NEJMoa043938
Le H-H, El-Khatib C, Mombled M et al (2016) Impact of aldosterone antagonists on sudden cardiac death prevention in heart failure and post-myocardial infarction patients: a systematic review and meta-analysis of randomized controlled trials. PLoS One 11:e0145958. https://doi.org/10.1371/journal.pone.0145958
Bardy GH, Lee KL, Mark DB et al (2005) Amiodarone or an implantable cardioverter–defibrillator for congestive heart failure. N Engl J Med 352:225–237. https://doi.org/10.1056/NEJMoa043399
McMurray JJV, Krum H, Abraham WT et al (2016) Aliskiren, enalapril, or aliskiren and enalapril in heart failure. N Engl J Med 374:1521–1532. https://doi.org/10.1056/NEJMoa1514859
Miller AL, Wang Y, Curtis J et al (2012) Optimal medical therapy use among patients receiving implantable cardioverter/defibrillators: insights from the National Cardiovascular Data Registry. Arch Intern Med 172:64–67. https://doi.org/10.1001/archinternmed.2011.466
Fonarow GC, Yancy CW, Hernandez AF et al (2011) Potential impact of optimal implementation of evidence-based heart failure therapies on mortality. Am Heart J 161:1024–1030. https://doi.org/10.1016/j.ahj.2011.01.027
Sanders GD, Hlatky MA, Owens DK (2005) Cost-effectiveness of implantable cardioverter–defibrillators. N Engl J Med 353:1471–1480. https://doi.org/10.1056/NEJMsa051989
Moss AJ, Zareba W, Hall WJ et al (2002) Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 346:877–883. https://doi.org/10.1056/NEJMoa013474
Stanek EJ, Oates MB, McGhan WF et al (2000) Preferences for treatment outcomes in patients with heart failure: symptoms versus survival. J Card Fail 6:225–232. https://doi.org/10.1054/jcaf.2000.9503
Stambler BS, Laurita KR, Shroff SC et al (2009) Aldosterone blockade attenuates development of an electrophysiological substrate associated with ventricular tachyarrhythmias in heart failure. Heart Rhythm 6:776–783. https://doi.org/10.1016/j.hrthm.2009.02.005
Ferreira JP, Girerd N, Medeiros PB et al (2016) Spot urine sodium excretion as prognostic marker in acutely decompensated heart failure: the spironolactone effect. Clin Res Cardiol 105:489–507. https://doi.org/10.1007/s00392-015-0945-x
Cooper HA, Dries DL, Davis CE et al (1999) Diuretics and risk of arrhythmic death in patients with left ventricular dysfunction. Circulation 100:1311–1315
Aldahl M, Jensen A-SC, Davidsen L et al (2017) Associations of serum potassium levels with mortality in chronic heart failure patients. Eur Heart J 38:2890–2896. https://doi.org/10.1093/eurheartj/ehx460
Vukadinović D, Lavall D, Vukadinović AN et al (2017) True rate of mineralocorticoid receptor antagonists-related hyperkalemia in placebo-controlled trials: a meta-analysis. Am Heart J 188:99–108. https://doi.org/10.1016/j.ahj.2017.03.011
Wei L, Struthers AD, Fahey T et al (2010) Spironolactone use and renal toxicity: population based longitudinal analysis. BMJ 340:c1768–c1768. https://doi.org/10.1136/bmj.c1768
Weir MR, Bakris GL, Bushinsky DA et al (2015) Patiromer in patients with kidney disease and hyperkalemia receiving RAAS inhibitors. N Engl J Med 372:211–221. https://doi.org/10.1056/NEJMoa1410853
Iqbal J, Parviz Y, Pitt B et al (2014) Selection of a mineralocorticoid receptor antagonist for patients with hypertension or heart failure. Eur J Heart Fail 16:143–150. https://doi.org/10.1111/ejhf.31
Funding
Dr Rossello has received support from SEC-CNIC CARDIOJOVEN Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
XR, CA, SJP, and DJVV have nothing to declare. JMcM reports conflicts of interest from Roche Pharmaceuticals, during the conduct of the study; other from Novartis, Cardiorentis, Amgen Oxford University/Bayer, GlaxoSmithKline, Theracos, Abbvie, DalCor, Pfizer, Merck, AstraZeneca Bristol Myers Squibb (BMS), Kidney Research UK (KRUK)/Kings College Hospital, London/Vifor-Fresenius Pharma, outside the submitted work. BP reports personal fees from Bayer, personal fees from KDP pharmaceuticals, and personal fees from Astrazeneca, outside the submitted work; In addition, BP has a patent site-specific delivery of eplerenone to the myocardium pending to university of Michigan. Faiez Zannad received honoraria and/or travel fees for participation in clinical trial committees and meetings/presentations from Amgen, AstraZeneca, Bayer, Boehringer, Boston Scientific, GE Healthcare, CVRx, Relypsa/Vifor-Fresenius, J&J, Pfizer, Novartis, Quantum Genomics, Resmed, Takeda, and received honoraria and/or travel fees for participation in advisory boards from BMS, KBP BioSciences, Livanova, NovoNordisk, Roche, ZS Pharma.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rossello, X., Ariti, C., Pocock, S.J. et al. Impact of mineralocorticoid receptor antagonists on the risk of sudden cardiac death in patients with heart failure and left-ventricular systolic dysfunction: an individual patient-level meta-analysis of three randomized-controlled trials. Clin Res Cardiol 108, 477–486 (2019). https://doi.org/10.1007/s00392-018-1378-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-018-1378-0