Abstract
Purpose
Circular staplers for colorectal anastomoses significantly ameliorated post-operative outcomes after rectal resection. The more recent three-row technology was conceived to improve anastomotic resistance and, thus, lower the incidence of anastomotic complications. The aim of this study was to evaluate potential advantages of three-row circular staplers (Three-CS) on anastomotic leakage (AL), stenosis (AS), and hemorrhage (AH) rates after rectal resection as compared to two-row circular staplers (Two-CS).
Methods
All rectal resections for rectal cancer between 2016 and 2021 were retrospectively included. Patients were classified according to the circular stapler employed in Two-CS and Three-CS cohorts. AL, AS, and AH rates were compared between the two populations. Additionally, the prognostic role of the type of circular stapler on AL onset was evaluated.
Results
Three-hundred and seventy-five patients underwent a rectal resection with an end-to-end anastomosis during the study period: 197 constituted the Two-CS group and 178 the Three-CS cohort. AL rate was 6.7%, significantly higher in the Two-CS group (19–9.6%) as compared to the Three-CS cohort (6–3.4%) (p = 0.01). No difference was noted in terms of AL severity. Although not statistically significant, a lower incidence rate of AL was evidenced even in the subset of patients with low rectal cancers (4.5% vs 12.5% in the two-row cohort; p = 0.33). At the multivariate analysis, Two-CS was a negative prognostic factor for AL onset (OR: 2.63; p = 0.03). No difference was noted between the two groups in terms of AS and AH.
Conclusion
Three-row CSs significantly decrease the rate of AL after rectal resection. Further multicenter controlled trials are still needed to confirm the advantages of three-row CSs on anastomotic complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although the improvement of peri-operative care protocols and the centralization of the surgical treatment in high-volume centers have slightly decreased the rate of post-operative complications after colorectal surgery, morbidity rate still ranges between 17 and 35% [1, 2]. Anastomotic leakage (AL), hemorrhage (AH), and anastomotic stenosis (AS) represent the most-feared adverse events, with a reported incidence rate of 1–26% [3], 2.3–6% [4], and 0.5–5%, respectively [5]. Among them, AL is recognized as the most serious complication, with a reported associated mortality incidence of 6.8% and detrimental long-term consequences, namely increased risk of cancer recurrence, decreased long-term survival, and reduced quality of life [6, 7].
In order to guarantee the safest method of reconstruction and, thus, reduce the potential onset of complications following colorectal surgery, the recent decades of research have been focusing on the different techniques of reconstruction and on the introduction of innovative devices.
Since the 1980s, the double stapling technique (DST) has become the standard method of reconstruction after rectal resection [8]. It is a mechanical anastomosis consisting in the transection of the rectum with a linear stapler and the anastomosis creation with a circular stapler introduced transanally. The spreading of the DST allowed surgeons to perform safer, reproducible, and easier colorectal anastomoses, increasing the sphincter-preservation rate and significantly decreasing the surgical time [9,10,11,12]. In this context, the advancement of circular stapling devices has given a significant contribution to the amelioration of clinical outcomes after DST. The main aim of the circular stapler technology is to achieve an appropriate tissue apposition avoiding, at the same time, tissue damage and ischemia [13]. Majority of circular staplers are currently characterized by two rows of staples, aimed to guarantee a high anastomotic resistance with reduced tissue damage. Nevertheless, technological advancements brought to the more recent introduction of the Tri-staple™ Technology (tri-EEA™) (Medtronic, Mansfield, MA, USA), based on three staple lines, conceived to guarantee a higher resistance of the anastomotic site with less stress on tissue as compared to the two-row circular staplers.
Despite these hypothetical advantages of the Tri-staple™ Technology, no evidence is currently present in the literature on the comparison between the two-row (Two-CS) and three-row circular staplers (Three-CS) in the clinical setting after rectal resection.
The aim of this single-center retrospective case–control study is, thus, to compare the two surgical devices firstly in terms of post-operative AL incidence. Secondary aims were the comparison between the two technologies also in terms of AS and AH.
Materials and methods
Patient selection and data extraction
After Institution Review Board (IRB) and Ethical Committee approvals (Protocol Number 6499/22; ID:4762), all patients who underwent a curative rectal resection for malignant disease at the Digestive Surgery Unit of the Fondazione Policlinico Agostino Gemelli IRCCS of Rome between January 2016 and August 2021 were retrospectively included in the study.
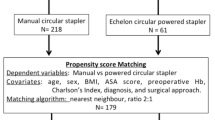
Only patients who underwent rectal resection for a histologically proven adenocarcinoma with an end-to-end reconstruction were enrolled for analysis, independently of the type of surgical approach employed (open, laparoscopic, or robot-assisted). Patients aged < 18 years, with previous history of colorectal surgery, with emergent operations, and with missing data or lost at follow-up were excluded from analysis. Similarly, the use of powered circular staplers (ECHELON CIRCULAR™ Powered Stapler—ECP, Ethicon Endo-Surgery, Inc., Cincinnati, OH, USA) was defined as an exclusion criterion, due to the different technologies in comparison to manual circular staplers.
Thus, surgical procedures were categorized, and outcomes compared, according to the manual circular stapler employed. Specifically, the two-row circular stapler (Two-CS group) (ETHICON™ Circular Stapler—ECP, Ethicon Endo-Surgery, Inc., Cincinnati, OH, USA, or Medtronic DST Series EEA—Medtronic, Mansfield, MA, USA) was used in all the procedures performed from January 2016 to December 2018. Conversely, since the introduction of the Tri-staple™ Technology in 2018, patients underwent a colorectal anastomosis using a three-row circular stapler (Three-CS group) (Medtronic, Mansfield, MA, USA).
All the data of interest were collected from prospectively maintained databases. Demographic and clinical characteristics included sex, age, body mass index (BMI), the American Society of Anesthesiologists (ASA) score, and tumor location. Tumor location was classified according to the distance from the anal verge into high rectum (10 to 15 cm from the anal verge), middle rectum (5 to 10 cm from the anal verge), and low rectum (< 5 cm from the anal verge).
Operative time (time between skin incision and skin closure), estimated intraoperative blood loss (EBL), and conversion rate were also considered for the comparative analysis.
Post-operative complications were defined as any deviation from the conventional post-operative clinical course and categorized according to the Clavien-Dindo classification [14]. Mortality was also recorded and defined as any death occurring within 30 days after surgery or during hospitalization. Further data on the post-operative course, namely time to first flatus and length of stay (LOS), were also included for the study purpose.
TNM classification (AJCC Cancer Staging System, 8th edition) was used for histopathological classification and staging.
Anastomotic leakage, anastomotic hemorrhage, and anastomotic stenosis definitions
According to the International Study Group of Rectal Cancer (ISREC) [15], AL was defined as a defect to the integrity of the intestinal wall of the anastomotic site, resulting in communication between the intraluminal and extraluminal compartments of the abdomen. AL was also classified according to severity: grade A was defined as only radiological evidence of a leak, without any treatment required; grade B as a leak that requires either antibiotics or a percutaneous drain; grade C as a symptomatic anastomotic leak that requires reoperation. Diagnosis was based on the clinical presence of symptoms (i.e., fever) and/or apparent signs of dehiscence (such as emission of gas, pus, or feces from the pelvic drain) leading to a radiologic examination (i.e., computed tomography (CT) scan or contrast enema) for leakage confirmation.
AH was defined as two or more episodes of rectal bleeding with a contemporary reduction of at least 2 g/dL of hemoglobin, requiring an endoscopic exploration [16].
AS was defined as the inability to pass a 12-mm scope through the anastomosis as well as reduction of at least 2/3 of the lumen diameter at the colonoscopy and/or double contrast barium enema performed at the routine follow-up or before in case of referred symptoms for stenosis [17].
Selection for neoadjuvant treatment and surgical technique
Preoperative staging included complete colonoscopy, whole-body CT scan, and pelvic magnetic resonance imaging (MRI). All cases were discussed at the multidisciplinary meeting and neoadjuvant treatment was prescribed in case of preoperative radiological evidence of node-positive or extramural disease. In these patients, radiological imaging was then repeated before surgery to evaluate tumor response.
All surgical procedures were performed by two senior surgeons with an extensive experience in colorectal surgery, according to standardized surgical steps as previously reported [18, 19]. A mechanical bowel preparation was prescribed and performed 2 days before surgery in all cases. The choice of the operative approach (open, laparoscopic, or robot-assisted) was at the discretion of the operating surgeon. There was no change in terms of antibiotics use and post-operative management during the whole study period.
In case of upper rectum lesion, a partial mesorectal excision (PME) was performed up to 5 cm below the tumor. Conversely, a total mesorectal excision (TME) with dissection at least 1 cm below the lesion was carried out for middle and low rectum tumors.
DST (Knight-Griffen technique) was employed in all cases [20]. The distal section of the rectum was performed with a linear three-line stapler. The proximal colon was freed circumferentially from pericolic fat along 1.5–2 cm. Then, a prolene 2/0 running suture was performed at 5–6 mm from the proximal border in order to anchor the anvil in the proximal stump of the colon. The first assistant introduced the circular stapler (Two- or Three-CS) from the anus. The instrument was then advanced, with the handle directed upwards since it reached the stapled line. At this point, the assistant opened the integrated trocar of the stapler anchoring the anvil. During this procedure, the surgeon was able to guide the first assistant and verify the correct position of the trocar inside the anvil, in order to avoid any damage of nearby structures (mesentery, vagina, small bowel loops). Once the trocar was correctly anchoring the anvil, the circular stapler was closed until its pointer was in the control zone. The stapler was then fired and the end-to-end anastomosis was, thus, performed (Fig. 1). The stapler was, then, opened counterclockwise and gently extracted from the anus. At this point, a hydro-pneumatic test was performed to evaluate the integrity of the anastomosis. Specifically, air was insufflated transanally using a catheter with the anastomosis under irrigation. In case of positive hydro-pneumatic test, reinforcing sutures were placed and an ileostomy was created.
Indications to ileostomy creation
Ileostomy was performed in all cases of positive hydro-pneumatic test, in case of neoadjuvant treatment as well as for tumor location into the low rectum.
Follow-up
Patients were followed-up every 6 months after surgery for the first year and then annually. A thoraco-abdominal CT scan and pelvic MRI were prescribed every year for the first 5 years. Similarly, a routine colonoscopy was prescribed 1 year after surgery or before in case of symptoms.
Study outcomes
The primary endpoint of the study was to compare the Two-CS and Three-CS study cohorts in terms of AL incidence rate.
The secondary endpoint was a further comparison between the two groups in terms of AS and AH. In addition, a comparative analysis was also conducted with regard to the intraoperative (namely operative time, EBL, intraoperative complications) and post-operative outcomes (time to first flatus, post-operative complications, LOS).
Statistical analysis
Categorical variables were presented as numbers and percentages, while continuous variables were presented as median and quartile rank (QR). Categorical variables were statistically compared using the chi-square test, while the Mann–Whitney U test was used for comparing continuous variables. The significance level was set at 0.05, two sided. Variables significant at univariate analysis for AL onset were then entered into a logistic regression model to identify independent predictors. Results were expressed as odds ratio (OR) with 95% confidence interval (CI). All data were analyzed by SPSS v25® (IBM, IL, USA).
Results
From January 2016 and August 2021, 375 patients underwent a curative rectal resection with a mechanical end-to-end reconstruction at the Digestive Surgery Unit of the Fondazione Policlinico Universitario Agostino Gemelli IRCCS of Rome. One-hundred and ninety-seven procedures (52.5%) were performed using the two-row circular stapler (Two-CS cohort), while the three-row circular stapler (Three-CS cohort) was employed in the remaining 178 procedures (47.5%). Demographic and clinical characteristics of the patients are shown in Table 1. There were no differences in patient characteristics and tumor location, while neoadjuvant therapy was more frequently prescribed in the Two-CS group (p = 0.03). The surgical approach significantly differed between the two study populations, with a higher percentage of minimally invasive procedures in the Three-CS group (170–95.5%) as compared to the Two-CS cohort (141–71.5%) (p < 0.0001). However, no difference was noted in terms of surgery duration, intraoperative blood loss, conversion rate, positivity of the hydro-pneumatic test, and diverting ostomy rate.
Post-operative clinical course (Table 2) was uneventful for the majority of patients, and severe post-operative complications (Clavien-Dindo grades III–IV) presented a similar incidence between the two groups (9.1% and 7.3% for the Two-CS and Three-CS cohorts, respectively; p = 0.28). Anastomotic complications, namely AS, AH, and AS, occurred in 8.5% of patients (32 out of 375). The overall incidence of AL was 6.7% (25 patients). Of them, 9 patients (36%) required reoperation and thus classified as grade C, and 8 patients (32%) needed a percutaneous drainage placement (grade B ALs), while the remaining 8 cases (32%) were successfully treated conservatively through antibiotics administration (grade A ALs). Notably, AL was equally evidenced in patients with and without an ileostomy performed during rectal resection (11–44% and 14–56%, respectively; p = 0.32). None of the patients with a positive hydro-pneumatic test developed AL post-operatively. Patients who developed an AL presented a significantly more prolonged median LOS (19 (9–26) vs 6 (4–8); p < 0.0001). In relation to the type of circular stapler used, a significantly higher incidence rate of AL was evidenced in case of Two-CS (19–9.6%) as compared to Three-CS (6–3.4%) (p = 0.01). However, no difference was noted between the two cohorts in terms of AL severity (p = 0.2), although a higher rate of grade C ALs was evidenced in the Three-CS group (4–66.7% vs 5–26.3% in the Two-CS population).
As a whole, AH and AS were documented in 1.3% (5 patients) and 0.5% (2 patients) of the population, and no difference was evidenced in terms of incidence rate according to the type of circular stapler employed (p = 0.73 and p = 0.94 for AH and AS, respectively).
All cases of AH occurred during hospitalization after a mean time of 65.2 ± 23.4 h from surgery and were successfully treated endoscopically. Both cases of AS were endoscopically diagnosed for referred persistent symptoms of constipation. Colonoscopy was performed after a mean time of 26.5 ± 3.3 days after surgery and AS treated by endoscopic dilation.
As a whole, surgical complications lead to reoperation in 18 cases (4.8%), with similar incidence rates between the two study groups (p = 0.23). Reoperation was performed due to bowel occlusion in 5 cases, small bowel perforation in 2 cases, and post-operative hemorrhage in 2 patients due to spleen injury. A grade C AL was the cause of reoperation in the remaining 9 patients. One patient of the Two-CS group died post-operatively due to septic complications after reoperation for a grade C AL. No patient who had a diverting ileostomy performed at the time of rectal resection needed reoperation for AL. Median length of hospital stay was longer in the Two-CS cohort than in the Three-CS cohort (p < 0.0001).
Predictive factor analysis for AL incidence
As shown in Table 3, at the univariate analysis, AL onset was significantly associated to a BMI ≥ 25 (p = 0.05), to tumor lesions located in the middle/low rectum (p < 0.0001), and to the Two-CS (p = 0.01). At the multivariate analysis, only tumor location in the middle/low rectum (p = 0.002) and Two-CS (p = 0.03) were recognized as independent prognostic factors, with an OR of 4 [95% CI: 1.64–9.87] and 2.63 [1.07–6.46], respectively.
AL, AS, and AH evaluation in low rectal tumors
A subanalysis was additionally conducted only on patients with low rectal cancers, widely recognized as a negative prognostic factor for AL onset, in relation to their deep location in the pelvis that makes anastomosis more challenging to perform. Out of 46 patients, 24 (52.2%) had anastomosis performed with a Two-CS while the Three-CS was employed in the remaining 22 cases (47.8%) (p = 0.95). As a whole, AL onset was post-operatively evidenced in 4 patients (8.7%). Of note, although not statistically different, a higher percentage of AL was documented in the Two-CS cohort (3–12.5%) as compared to the Three-CS population (1–4.5%) (p = 0.33). No AS and AH were evidenced in this same subset of patients.
Discussion
In the present study, we analyzed the impact of the type of circular stapler employed for anastomotic fashioning on surgical outcomes after rectal resection. Specifically, the aim was to compare the two- and three-row circular staplers in terms of AL, AS, and AH rates. With the limitation of the retrospective study design, we demonstrated significant advantages in terms of AL incidence when the Three-CS was employed, while the type of circular stapler did not show any influence on AL severity. Furthermore, the two devices were comparable for AH and AS rate.
These results derive from the recent advances in surgical techniques and from the introduction of novel surgical devices that progressively ameliorated post-operative outcomes after colorectal surgery. In this regard, a significant contribution was firstly given by the wide spread of DST [8, 20]. The use of linear stapler for rectal resection and circular stapler introduced transanally for creation of anastomoses has demonstrated to increase sphincter-preserving procedures, reducing, at the same time, the incidence rate of anastomotic complications and surgery duration [9,10,11]. Although several comparative studies are present in the literature on DST vs handsewing anastomosis creation, no report is currently present on the comparison among the different technologies of the circular staplers.
Circular staplers have evolved over time, and the Tri-staple™ Technology was introduced in 2018. The main goal was to guarantee more secure anastomoses allowing, at the same time, an adequate perfusion of the anastomotic stumps as compared to the two-row devices. Three-CSs provide three rows of staples that vary in height. The innermost row is composed by the shortest staples, with the aim of providing the greatest occlusion and barrier to AL. The remaining rows (intermediate and the most external ones) are incrementally higher in order to further strengthen the closure, reducing, at the same time, pressure on tissues, leading to a more facilitated blood supply through microvasculature. This balance between occlusion, hemostasis, and favorable blood supply should hypothetically reflect on lower incidence of anastomotic complications in comparison to the Two-CSs. According to our results, this is particularly true for AL onset. The incidence of AL after colorectal surgery in previous reports ranges between 1 and 26% according to the definition used and to tumor location [3]. A recent report on the validation of the ISREC AL grading on 746 patients documented an AL incidence rate of 7.5%, which is not dissimilar to the 6.6% reported in our experience [21]. When patients were stratified according to the type of circular stapler employed, the Three-CS demonstrated a significantly lower association with AL onset (3.4%) as compared to the two-row technology (9.6%) (p = 0.01). A more than 6% absolute difference in AL rate inevitably makes the choice of stapler crucial for the patient, the operating surgeon, and the healthcare. Indeed, other than the relevant long-term consequences due to AL manifestation, namely higher rate of local recurrence, impaired quality of life, and related mortality rate up to 6.8% [6, 7], AL onset leads to overspending in healthcare estimated at approximately 20,000 dollars per patient [22].
Interestingly, although not statistically different, the use of the Tri-staple™ Technology was associated to a more severe grade of AL. Specifically, 4 out of 6 ALs (66.7%) of the Three-CS group were classified as grade C in comparison to 5 out of 19 (26.3%) of the Two-CS cohort. This likely finds a justification into the clinico-demographic characteristics of patients. For instance, all 4 patients of the Three-CS population presented a BMI > 25 kg/m2, and a low rectum adenocarcinoma, both characteristics that made them more prone to develop more severe ALs [23,24,25].
Furthermore, in order to specifically evaluate the prognostic role of the circular stapler on AL onset, we conducted a multivariate analysis. As expected, BMI > 25 kg/m2 and tumor location in the middle/low rectum were confirmed as independent prognostic factors, in line with the majority of reports present in the literature [23,24,25]. Of note, the use of the Two-CSs was recognized as an independent negative prognostic feature, with an OR of 2.63 [1.07–6.46] (p = 0.03).
As further analysis, we evaluated the potential influencing role of circular staplers specifically on low rectal resections. Indeed, tumor location deep in the pelvis is widely recognized as a negative prognostic feature for AL development, and, despite the recent technological advances, its incidence rate is still reported up to 36% [26]. According to the current literature, the introduction of circular staplers significantly simplified ultra-low and low anastomoses formation, thus increasing the rate of sphincter-preserving procedures [12]. However, their potential influencing role of AL incidence rate is still a matter of debate. Overlooking our data, we documented an AL rate of 8.7% (4 out 46 patients). Interestingly, a tendency toward a higher rate of AL was evidenced in the case of Two-CS (3–12.5%) as compared to the Three-CS (1–4.5%). Despite this relevant decrease in the case of three-row technology employment, the difference was not statistically significant, probably due to the low sample size of patients with low rectal tumors.
AS is recognized as another fearful complication of rectal resections. Although the physiopathology of AS is not yet fully understood, tissue ischemia, AL, inflammation, and radiotherapy have been associated to its potential development [27,28,29]. Similarly, diverting ostomies seem to increase the AS rate, probably due to the lack of dilation by fecal stream [30,31,32]. Interestingly, the use of stapler suturing has been related to higher risk of AS, currently comprised between 0 and 30%, independently of the size of the circular stapler diameter [33, 34]. It has been hypothesized that the use of staplers may induce an overactive inflammation, leading to the formation of a stricture [35]. Other authors proposed mucosal gaps and necrosis areas of the stapled anastomosis as main causes of an increased risk of anastomotic stenosis due to their healing by secondary intention [33]. Despite these premises, as a whole, we reported AS only in 2 out of 375 patients (0.5%), with similar incidence rates between the Two- and Three-CS cohorts (p = 0.23). This would imply that the type of circular stapler does not play any influencing role on anastomotic stricture formation after rectal resection. However, given the low rate of AS after colorectal surgery, a larger sample size of patients is needed in order to draw solid conclusions.
With regard to AH onset, its incidence rate after rectal resection varies between 2.3 and 6% and constitutes a clinical emergency in approximately 1% of cases [36]. As compared to the handsewn technique, the use of staplers has been associated to a 2.7% higher risk of AH [37]. Indeed, a previous report on the preliminary evaluation of safety and feasibility of the circular stapler reported an AH incidence rate of 4.2% [38]. However, both the two- and three-row devices have been conceived to apply a proper compression on tissues in order to appropriately balance adequate perfusion and hemostasis. This brought to a significant drop in AH incidence with the introduction of more recent devices. As compared to these data, we noted a more than 3% reduction of AH rate with the more recent Two- and Three-CSs, hypothetically confirming the advantages of the novel devices as compared to the initial ones. Interestingly, no difference was noted between the two technologies in terms of hemorrhage events (p = 0.73), and, notably, all hemorrhagic episodes were successfully treated endoscopically.
Our study presents some limitations. First, its retrospective design could have led to possible selection biases. Second, due to the low incidence of anastomotic complications we encountered, the sample size may be not sufficient to draw definitive conclusions. Third, the lower rate of tumors located in the upper rectum in the Two-CS group (although not statistically different as compared to the Three-CS cohort; p = 0.13) and the more frequent neoadjuvant treatment in this same cohort of patients may constitute a further bias of the study. On the counterpart, we presented, for the first time in the literature, a comparative study on surgical outcomes according to the circular stapler technology employed. Indeed, although in a preliminary setting, the more recent Tri-staple™ Technology seems to be associated to a lower incidence of AL, potentially leading to significant advantages both in terms of short-term and long-term outcomes. Moreover, the monocentric study design has permitted to rely on standardized procedures, thus limiting the potential biases due to technical inhomogeneity.
In conclusion, our retrospective comparative analysis has shown the potential positive impact of the Tri-staple™ Technology in reducing AL rate after rectal resection even for low rectal tumors, while maintaining similar rates of AS and AH in comparison to Two-CSs. Nevertheless, the need for multicenter controlled trials is implicit, together with a more homogeneous distribution of patients’ characteristics between the study groups (i.e., tumor location, neoadjuvant treatment), to obtain stronger evidences to further confirm the potential positive contribution of the Tri-staple™ Technology on clinical outcomes.
References
Angelucci GP, Sinibaldi G, Orsaria P, Arcudi C, Colizza S (2013) Morbidity and mortality after colorectal surgery for cancer. Surg Sci 4(11):520–524
Alves A, Panis Y, Mathieu P, Mantion G, Kwiatkowski F, Slim K, Association Francaise de C (2005) Postoperative mortality and morbidity in French patients undergoing colorectal surgery: results of a prospective multicenter study. Arch Surg 140:278–283, discussion 284
Paun BC, Cassie S, MacLean AR, Dixon E, Buie WD (2010) Postoperative complications following surgery for rectal cancer. Ann Surg 251:807–818
Sartori A, De Luca M, Fiscon V, Frego M, group Csw, Portale G, (2019) Retrospective multicenter study of post-operative stenosis after stapled colorectal anastomosis. Updates Surg 71:539–542
Clifford RE, Fowler H, Govindarajah N, Vimalachandran D, Sutton PA (2019) Early anastomotic complications in colorectal surgery: a systematic review of techniques for endoscopic salvage. Surg Endosc 33:1049–1065
Walker KG, Bell SW, Rickard MJ, Mehanna D, Dent OF, Chapuis PH, Bokey EL (2004) Anastomotic leakage is predictive of diminished survival after potentially curative resection for colorectal cancer. Ann Surg 240:255–259
McArdle CS, McMillan DC, Hole DJ (2005) Impact of anastomotic leakage on long-term survival of patients undergoing curative resection for colorectal cancer. Br J Surg 92:1150–1154
Knight CD, Griffen FD (1980) An improved technique for low anterior resection of the rectum using the EEA stapler. Surgery 88:710–714
Heald RJ, Leicester RJ (1981) The low stapled anastomosis. Dis Colon Rectum 24:437–444
Hansen O, Schwenk W, Hucke HP, Stock W (1996) Colorectal stapled anastomoses experiences and results. Dis Colon Rectum 39:30–36
Chassin JL, Rifkind KM, Turner JW (1984) Errors and pitfalls in stapling gastrointestinal tract anastomoses. Surg Clin North Am 64:441–459
Fleshman JW, Smallwood N (2015) Current concepts in rectal cancer. Clin Colon Rectal Surg 28:5–11
Mery CM, Shafi BM, Binyamin G, Morton JM, Gertner M (2008) Profiling surgical staplers: effect of staple height, buttress, and overlap on staple line failure. Surg Obes Relat Dis 4:416–422
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, Holm T, Wong WD, Tiret E, Moriya Y, Laurberg S, den Dulk M, van de Velde C, Buchler MW (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 147:339–351
Serur A, Rhee R, Ramjist J (2020) Current nonoperative therapeutic interventions for lower gastrointestinal hemorrhage. Clin Colon Rectal Surg 33:22–27
Kraenzler A, Maggiori L, Pittet O, Alyami MS, AlDJ P, Panis Y (2017) Anastomotic stenosis after coloanal, colorectal and ileoanal anastomosis: what is the best management? Colorectal Dis 19:O90–O96
Alfieri S, Di Miceli D, Menghi R, Cina C, Fiorillo C, Prioli F, Rosa F, Doglietto GB, Quero G (2018) Single-docking full robotic surgery for rectal cancer: a single-center experience. Surg Innov 25:258–266
Fiorillo C, Quero G, Menghi R, Cina C, Laterza V, De Sio D, Longo F, Alfieri S (2021) Robotic rectal resection: oncologic outcomes. Updates Surg 73:1081–1091
Griffen FD, Knight CD Sr, Knight CD Jr (1992) Results of the double stapling procedure in pelvic surgery. World J Surg 16:866–871
Kulu Y, Ulrich A, Bruckner T, Contin P, Welsch T, Rahbari NN, Buchler MW, Weitz J, International Study Group of Rectal C (2013) Validation of the International Study Group of Rectal Cancer definition and severity grading of anastomotic leakage. Surgery 153:753-761
Hashemi L, Mukherjee N, Morseon M, Sirkar R (2012) Economic impact of anastomotic leaks in colectomy procedures in the USA: 2005–2009. SAGES 2012 Meeting, San Diego, CA, United States
Komen N, Dijk JW, Lalmahomed Z, Klop K, Hop W, Kleinrensink GJ, Jeekel H, Ruud Schouten W, Lange JF (2009) After-hours colorectal surgery: a risk factor for anastomotic leakage. Int J Colorectal Dis 24:789–795
Lipska MA, Bissett IP, Parry BR, Merrie AE (2006) Anastomotic leakage after lower gastrointestinal anastomosis: men are at a higher risk. ANZ J Surg 76:579–585
Platell C, Barwood N, Dorfmann G, Makin G (2007) The incidence of anastomotic leaks in patients undergoing colorectal surgery. Colorectal Dis 9:71–79
Caulfield H, Hyman NH (2013) Anastomotic leak after low anterior resection: a spectrum of clinical entities. JAMA Surg 148:177–182
Senagore A, Milsom JW, Walshaw RK, Dunstan R, Mazier WP, Chaudry IH (1990) Intramural pH: a quantitative measurement for predicting colorectal anastomotic healing. Dis Colon Rectum 33:175–179
Orsay CP, Bass EM, Firfer B, Ramakrishnan V, Abcarian H (1995) Blood flow in colon anastomotic stricture formation. Dis Colon Rectum 38:202–206
Chung RS, Hitch DC, Armstrong DN (1988) The role of tissue ischemia in the pathogenesis of anastomotic stricture. Surgery 104:824–829
Waxman BP, Ramsay AH (1986) The effect of stapler diameter and proximal colostomy on narrowing at experimental circular stapled large bowel anastomoses. Aust N Z J Surg 56:797–801
Virgilio C, Cosentino S, Favara C, Russo V, Russo A (1995) Endoscopic treatment of postoperative colonic strictures using an achalasia dilator: short-term and long-term results. Endoscopy 27:219–222
Graffner H, Fredlund P, Olsson SA, Oscarson J, Petersson BG (1983) Protective colostomy in low anterior resection of the rectum using the EEA stapling instrument. A randomized study Dis Colon Rectum 26:87–90
MacRae HM, McLeod RS (1998) Handsewn vs. stapled anastomoses in colon and rectal surgery: a meta-analysis. Dis Colon Rectum 41:180–189
Luchtefeld MA, Milsom JW, Senagore A, Surrell JA, Mazier WP (1989) Colorectal anastomotic stenosis. Results of a survey of the ASCRS membership. Dis Colon Rectum 32:733–736
Dziki AJ, Duncan MD, Harmon JW, Saini N, Malthaner RA, Trad KS, Fernicola MT, Hakki F, Ugarte RM (1991) Advantages of handsewn over stapled bowel anastomosis. Dis Colon Rectum 34:442–448
Hoedema RE, Luchtefeld MA (2005) The management of lower gastrointestinal hemorrhage. Dis Colon Rectum 48:2010–2024
Lustosa SA, Matos D, Atallah AN, Castro AA (2001) Stapled versus handsewn methods for colorectal anastomosis surgery. Cochrane Database Syst Rev:CD003144
Kyzer S, Gordon PH (1992) Experience with the use of the circular stapler in rectal surgery. Dis Colon Rectum 35:696–706
Funding
This study was funded by Medtronic, Mansfield, MA, USA (reference number: ERP-2021–12921). Compensation was received by the Fondazione Policlinico Universitario Agostino Gemelli IRCCS of Rome. The authors did not receive any compensation. The Fondazione Policlinico Universitario Agostino Gemelli IRCCS of Rome did not receive any discount for stapling devices from Medtronic.
Author information
Authors and Affiliations
Contributions
Conceptualization: Giuseppe Quero, Claudio Fiorillo. Methodology: Vito Laterza; Davide De Sio, Giuseppe Massimiani. Formal analysis and investigation: Chiara Lucinato, Carlo Alberto Schena, Roberta Menghi. Writing—original draft preparation: Giuseppe Quero, Fausto Rosa. Writing—review and editing: Sergio Alfieri, Vincenzo Tondolo. Supervision: Sergio Alfieri, Valerio Papa.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of the Fondazione Policlinico Universitario Agostino Gemelli IRCCS of Rome (Protocol Number 6499/22; ID:4762).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Quero, G., Fiorillo, C., Menghi, R. et al. Preliminary evaluation of two-row versus three-row circular staplers for colorectal anastomosis after rectal resection: a single-center retrospective analysis. Int J Colorectal Dis 37, 2501–2510 (2022). https://doi.org/10.1007/s00384-022-04283-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04283-8