Abstract
Anastomotic stenosis after colorectal surgery is usually considered low-rate complication and often is under-reported in most studies. Few data are available on management strategies. The aim of the study was to assess the prevalence of stenosis after stapled colorectal anastomosis, performed either in elective or emergent setting, for benign or malignant disease, and to evaluate treatment profiles. This retrospective study was a survey conducted in a large Italian North-Eastern area including three regions (Triveneto), over a 12-month period (January–December 2015). Patients’ characteristics and surgical technique details were recorded, along with data on the prevalence of stenosis and its treatment. Patients with mid or low rectal resection and/or neoadjuvant chemo-radio therapy and/or diverting stoma were excluded. The study was promoted by the Italian Association of Hospital Surgeons (ACOI) and the Society of Surgeons of the Triveneto Region. Twenty-eight surgical units were enrolled in the survey, accounting for over 1400 patients studied. Fifty percent of the units performed laparoscopically > 70% of the colorectal resections and 7.5% of the procedures were emergent. Less than 60% of the units planned regular endoscopic follow-up after colorectal resection. Anastomotic stricture was recorded in 2% of the patients; 88% of the stenoses were diagnosed within 6 months from surgery. Only one anastomotic stricture required re-do surgery. The CANSAS study confirms that colorectal anastomotic stenosis is low-rate—but still present—complication. Treatment strategies vary according to surgeons’ and endoscopists’ preferences. Commonly endoscopic dilatation is preferred, but re-do surgery is required in some cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anastomotic benign stenosis is an infrequent complication following colorectal resection. It is usually under-reported in the literature, with prevalence ranging from 3 to 30%, and its pathophysiologic mechanisms are not entirely understood [1,2,3,4,5,6]. Neoadjuvant chemo-radiotherapy, anastomotic leakage, diverting stoma and the presence of a stapled rather than a hand-sewn anastomosis have all been claimed as risk factors for stenosis [7,8,9]. The treatment of choice for stenosis following stapled colorectal anastomosis is endoscopic dilatation. Usually repeated sessions with balloon dilators of different calibers or laser incisions are required to treat the stenosis. Surgery (re-do anastomosis) is reserved to those-few-cases who do not fully respond to endoscopic therapy [10,11,12,13,14].
The aim of the CANSAS (Colorectal ANastomotic Stenosis After Surgery) survey was to retrospectively assess the prevalence of anastomotic stenosis after colorectal stapled resections, performed either in elective or emergent setting, and evaluate treatment profiles.
Materials and methods
Study design
This multicenter retrospective observational study was conducted in a large Italian North-Eastern area of about 7.2 million inhabitants, including three regions (Veneto, Friuli Venezia Giulia e Trentino Alto Adige), over a 12-month period (January–December 2015) and it was promoted by the Italian Association of Hospital Surgeons (ACOI) and the Society of Surgeons of the Triveneto Region.
All patients with colorectal stapled anastomosis (left hemicolectomy and rectal anterior resection with partial mesorectal resection) were included. Patients with mid–low rectal resection undergoing total mesorectal resection, along with patients receiving neoadjuvant chemo-radiotherapy and/or diverting stoma were excluded. Follow-up endoscopic data were updated at June 2017. The coordinator of each participating center collected the data and compiled the study form. The collected data included patients characteristics (age, gender) and surgical technique details (laparotomy vs laparoscopy, emergent vs elective procedure, splenic flexure mobilization, low or high vascular ligation), along with data on endoscopic follow-up and on the prevalence of stenosis and details of its treatment. For the purpose of the survey, stenosis was not defined but under specific evaluation of the surveyed surgeons.
The study was conducted according to the Helsinki Declaration and patients gave their consent to have their data collected for scientific purposes. The study was approved by the local Ethics Committee.
Statistical analysis
Continuous data were expressed as median and interquartile range (IQR).
Results
Twenty-eight of the 49 surgical units (57.1%) contacted in the Triveneto Italian North-Eastern area, replied to the invitation letter and fully completed the survey. The total number of patients included in the study was 1404 (682 M and 722 F). Twenty-three of 28 units (82.1%) operated > 25 patients in the study period. The vast majority of the operations were done for either cancer (812 patients, 57.8%), diverticular disease (338, 24.1%), or endometriosis (226, 16.1%), with few patients operated for inflammatory bowel disease (20, 1.4%) or other reasons (e.g., trauma, 8, 0.6%). Fourteen (50%) units performed laparoscopically > 70% of the colorectal resections; 7.5% of the procedures were emergent (median). Take down of the splenic flexure was performed on a routine basis in 78.5% (22/28) of the centers; the inferior mesenteric artery was routinely sectioned at its origin in 1/3 (32.2%, 9/28) of the centers, while in 2/3 this was performed only for cancer patients. In all but one center the length of the resected fixed specimen was (median) either < 25 cm (13/28, 46.4%) or 25–35 cm (14/28, 50%), in all but one center, reporting resected specimens of > 35 cm. Fifteen of 28 (53.6%) units planned regular endoscopic controls after colorectal resection, with either rigid rectoscopy or colonoscopy at 3, 6 or 12 months after surgery.
A stenosis was recorded in 28/1404 (2%) patients. The stenosis was diagnosed within 3 months from surgery in 19 patients (60.7%), between 3 and 6 months in 8 (28.6%) and after 6 months in 3 (10.7%). Anastomotic stricture accounted for < 5% of patients in 25/28 (89.3%) surgical units (no cases in 16 of these 25) and > 5% in 3/28 (10.7%).
Endoscopic dilatation was commonly used in cases requiring treatment in all the surgical units reporting stenosis, but in one case re-do surgery was required (1/28 stenoses, 3.5%).
Discussion
Benign anastomotic stricture following stapled colorectal resection for either malignant or benign disease is a well-known but poorly defined complication. There is no clear definition of what is stricture nor when and how to evaluate it. It is considered a narrowing that prevents a ‘normal’ passage of the stools. But what is ‘normal’ passage still remains ambiguous. Several thresholds in caliber have been proposed in the past: the inability to pass a 12-mm scope through the anastomosis, the reduction of at least 2/3 of the diameter, etc., [14,15,16]. Excluding regular endoscopic follow-up of patients operated for malignant disease, a colorectal anastomosis done for other diseases may not undergo endoscopic evaluation for months or years except in symptomatic patients. All these reasons contribute to explain the difficulty of assessing the true rate of colonic or colorectal anastomotic stricture. As a result, most surgeons are reluctant to report their data on stenosis and are not convinced of the opportunity to have their patients (including those with benign disease) routinely evaluated with postoperative endoscopy for stricture assessment. Furthermore, when stenoses are found, not all are symptomatic or require treatment, and in some cases they may improve spontaneously over time [2].
A large mail survey was conducted in 1989 from the American Society of Colorectal Surgeons, but from 1034 members only 110 (roughly 10%) replied and reported a total number of 123 patients with intestinal anastomotic stenosis, anywhere in the large bowel, mostly in the sigmoid colon or rectum and two-thirds of these were stapled anastomoses [1]. The very low rate of responses of this survey confirmed the idea that anastomotic stenosis after colorectal surgery is not a subject of great interest amongst surgeons and that most surgeons are reluctant to follow-up endoscopically their patients. We decided to assess the prevalence of anastomotic stricture in a large Italian North-Eastern area, with over 7.2 millions inhabitants, that we deem representative of the whole Italian country. Over 1400 patients were retrospectively enrolled in the study, with a prevalence of stenosis of 2%. We considered a 12 months of endoscopic follow-up adequate to assess the real prevalence of stenosis of stapled colorectal anastomosis, irrespective of the oncologic follow-up which was already set for cancer patients, allowing for both benign and malignant patients to have the same interval of post-operative evaluation.
An important issue when dealing with stenosis after surgery is the timing of this complication. In our survey nearly 90% of all the anastomotic stenoses were reported within 6 months from surgery. We are aware in fact that stenosis may improve spontaneously from one endoscopic examination to another and that most of the stenoses will present up to 6 months after surgery [2]. That’s why, after this retrospective CANSAS I study, we decided to start a prospective multicenter study for a proper assessment of colorectal anastomosis, the CANSAS II, including symptomatic and repeated endoscopic evaluation carried out at 1–3–6 months after surgery.
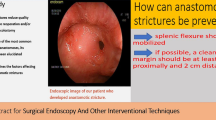
Amongst the risk factors for anastomotic stenosis, the presence of a tension-free anastomosis has been recalled. It is important to have sufficient length of proximal colon to avoid tension of the suture line. This can be achieved by freeing the left colon with takedown of the splenic flexure and by dividing the IMA (inferior mesenteric artery) at its origin from the aorta, rather than after the emergence of the left colic artery. In our study in nearly 80% of the centers the take down of the splenic flexure was performed on a routine basis and in 1/3 of the centers the inferior mesenteric artery was routinely sectioned at its origin, while in 2/3 this was performed for cancer patients only. As a result, in 50% of the centers a median length of 25–35 cm of colon could be resected and in the remainders this was < 25 cm. It was not the aim of this study to assess the predisposing factors of stenosis. We are just reporting the common attitude of surgeons with some of the technical aspects that might be evoked when addressing the problem of anastomotic benign stenosis.
Most symptomatic strictures are commonly treated with a variable number of endoscopic dilatations, according to the symptomatic relief and endoscopic confirm that a large anastomotic lumen has been achieved. Several techniques have been developed, including the use of steroid injection, electrocautery, photoablation, although usually a balloon or pneumatic dilator is enough to accomplish the result [10,11,12,13]. Surgery with redo anastomosis is reserved for cases refractory to endoscopic treatment or long segment strictures [14,15,16,17]. Even though the reoperations are reported as more difficult with long operative times, blood loss and long post-operative stay, the procedure is usually feasible and safe [5]. In our survey most of the centers reporting cases of stenosis treated these patients with endoscopic dilatations. Reoperation was necessary only in one case of stenosis reported (3.5% of the 28 stenosis of our survey). A survey of ASCRS (American College of Surgeons Society) members in 1981, older than the one previously quoted, 315 stenoses were identified after 3594 stapled anastomosis and only 4% of these stenosis required surgical intervention.
The aim of this study was to assess the prevalence of anastomotic stenosis after colorectal resection with mechanical staple device and not to ascertain the causes or predictive factors of such stenosis. In order to define the effect of patient’s related factors (age, gender, comorbidities) or surgery’s related factors (smaller/larger cartridge used for the anastomosis, splenic flexure mobilization, low or high vascular ligation, anastomotic leak, etc.,) we have started a prospective study, already mentioned above. Despite this being beyond the aims of the study, however, we observed that cases of stenosis were reported both from centers with and without routine section of the IMA at its origin in all cases and in centers with and without routine takedown of the splenic flexure.
This study has some limitations that need to be considered when reading the results. First, the retrospective nature of the study affects at least in part the completeness of data, in fact not all the surgical units had their data prospectively collected in an electronic database with follow-up information easily updated before the analysis, avoiding loss of data. Second, there was no unique definition of ‘stenosis’ and this was left to the discretion of each surgical unit involved in the study. However, this was not unexpected by our survey and actually this was one of the reasons to justify the next prospective study with a common definition of ‘stenosis’.
The strengths of the study include a picture of a large Italian area (probably representative of the full nation) with regard to the prevalence of ‘stenosis’ after colonic resection and the treatments in use, at the moment, to solve this complication. Nearly 60% of the contacted surgical units replied to the invitation letter and fully completed the survey. This was well above the 10% of the US survey, dated back in the early 1980s. Further, the 12-month follow-up period is quite long and sufficient to detect virtually all the stenoses which will develop after surgery.
Conclusions
In conclusion, this study confirms that colorectal anastomotic stenosis is a low-rate—but still present—complication and should be kept in mind, with endoscopic follow-up, not only symptomatic one, advised both for malignant and benign disease. Treatment strategies vary according to surgeons’ and endoscopists’ preferences, with endoscopic dilatation commonly the preferred one, although re-do surgery might be required in some cases.
References
Luchtefeld MA, Milsom JW, Senagore A, Surrell JA, Mazier WP (1989) Colorectal anastomotic stenosis. Results of a survey of the ASCRS membership. Dis Colon Rectum 32:733–736
Bannura GC, Cumsille MA, Barrera AE, Contreras JP, Melo CL, Soto DC (2004) Predictive factors of stenosis after stapled colorectal anastomosis: prospective analysis of 179 consecutive patients. World J Surg 28:921–925
Polese L, Vecchiato M, Frigo AC, Sarzo G, Cadrobbi R, Rizzato R, Bressan A, Merigliano S (2012) Risk factors for colorectal anastomotic stenoses and their impact on quality of life: what are the lessons to learn? Colorectal Dis 14:e124–e128. https://doi.org/10.1111/j.1463-1318.2011.02819
Ambrosetti P, Francis K, De Peyer R, Frossard J-L (2008) Colorectal anastomotic stenosis after elective laparoscopic sigmoidectomy for diverticular disease: a prospective evaluation of 68 patients. Dis Colon Rectum 51:1345–1349
Hiranyakas A, Da Silva G, Denoya P, Shawki S, Wexner SD (2013) Colorectal anastomotic stricture: is it associated with inadequate colonic mobilization? Tech Coloproctol 17:371–375
Davis B, Rivadeneira D (2013) Complications of colorectal anastomoses. Leaks, strictures and bleeding. Surg Clin N Am 93:61–87
Pahlman I, Glimelius B, Frykholm G (1989) Ischaemic strictures in patients treated with a low anterior resection and perioperative radiotherapy for rectal carcinoma. Br J Surg 76:605–606
Waxman BP, Ramsay AH (1986) The effect of stapler diameter and proximal colostomy on narrowing at experimental circular stapled large bowel anastomosis. Aust N Z J Surg 56:797–801
Matos D, Atallah AN, Castro AA, Lustosa S (2001) Stapled versus handsewn methods for colorectal anastomosis surgery. Cochrane Database Syst Rev 3:CD003144
Di Giorgio P, De Luca L, Rivellini G, Sorrentino E, D’Amore E, De Luca B (2004) Endoscopic dilatation of benign colorectal anastomotic stricture after low anterior resection: a prospective comparison study of two balloon types. Gastrointest Endosc 60:347–350
Forshaw MJ, Maphosa G, Sankararajah D, Parker MC, Stewart M (2006) Endoscopic alternatives in managing anastomotic strictures of the colon and rectum. Tech Coloproctol 10:21–27
Brandimarte G, Tursi A, Gasbarrini G (2000) Endoscopic treatment of benign anastomotic colorectal stenosis with electrocautery. Endoscopy 32:461–463
Suchan KL, Muldner A, Manegold BC (2003) Endoscopic treatment of postoperative colorectal anastomotic strictures. Surg Endosc 17:1110–1113
Schlegel RD, Dehni N, Parc R, Caplin S, Tiret E (2001) Results of reoperations in colorectal anastomotic strictures. Dis Colon Rectum 44:1464–1468
Fasth S, Hedlund H, Svaninger G, Hulten L (1982) Autosuture of low colorectal anastomosis. Acta Chir Scand 148:535–539
Fegiz G (1983) ANgelini L, Bezzi M. Rectal cancer: restorative surgery with EEA stapling device. Int Surg 6:13–18
Swenson O, Idriss FS (1966) Excision of rectal stricture with end-to-end anastomosis. Arch Surg 93:54–58
Acknowledgements
Collaborators of the CANSAS study working group (Colorectal ANastomotic Stenosis After Surgery). S Vigna, A Mazzeo, D Coco, F Agresta, E Finotti, M Antoniutti, S Carnio, A Elio, M Brunelli, G Ruffo, E Bertocchi, D Parini, L Losacco, F Poli, G Santoro, M Massani, C Ruffolo, E Cian, L Zanatta, M Genna, A Ballarin, M Rebonato, M Fontana, G Moretto, H Impellizzeri, R Merenda, G Margani, S Merigliano, N Baldan, P Ubiali, A Braini, A Balani, M Kosuta, A Infantino, G Giacomel, G Armatura, S Patauner, N de Manzini, S Palmisano, M Sorrentino, M Brizzolari, C Belluco, M Olivieri, E Lauro, G Scudo, P Valduga, A Brolese, G Pignata, J Andreucetti, A Caruso, F Zappalà.
Funding
There was no funding source for this paper.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Drs. Alberto Sartori, Maurizio De Luca, Valentino Fiscon, Mauro Frego, the CANSAS study working group and Giuseppe Portale have no conflict of interest to disclose.
Ethical approval
The study was conducted according to the Helsinki Declaration. The study was approved by the local Ethics Committee.
Informed consent
Patients gave their consent to have their data collected for scientific purposes.
Additional information
Collaborators of the CANSAS study working group (Colorectal ANastomotic Stenosis After Surgery) are given in the acknowledgements section.
Rights and permissions
About this article
Cite this article
Sartori, A., De Luca, M., Fiscon, V. et al. Retrospective multicenter study of post-operative stenosis after stapled colorectal anastomosis. Updates Surg 71, 539–542 (2019). https://doi.org/10.1007/s13304-018-0575-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-018-0575-8