Abstract
Background
Malignant colonic obstruction is commonly treated surgically. Colonic stents are a therapeutic option for palliation or used as a bridge to surgery or chemotherapy.
Objective
The aim of the study was to evaluate the clinical success rate of stenting as a bridge to one-step surgery, chemotherapy, or as a palliative measure.
Design
This was a retrospective observational study.
Settings
The study was conducted at a university-affiliated tertiary referral center.
Patients and interventions
From 2007 to 2014, 45 patients with malignant colonic obstruction were referred for stent insertion.
Main outcome measures
Patients were grouped according to three pre-defined treatment goals: group 1: restorative one-step procedure without an ostomy, group 2: completion of scheduled chemotherapy before surgery, and group 3: palliation without surgical intervention.
Results
Group 1 included 11 patients. Three patients (27.3 %) met the treatment goal of one-step surgery. Eight patients (72.7 %) did not reach the primary goal due to stent insertion failure (four patients), stent-related complications (two patients), and failure to perform a one-step surgery after successful stent insertion (two patients). Group 2 included 12 patients. Chemotherapy was successfully completed prior to surgery in six patients (50 %). Six patients (50 %) did not achieve treatment goal due to stent insertion failure (two patients), stent migration (two patients), stent-related perforation (one patient), and mortality (one patient). Group 3 included 20 patients. Long-term palliation without surgical intervention was achieved in eight patients (40 %). Stent insertion failed in seven patients (35 %). Five patients (25 %) needed urgent surgery due to stent complications (three migrations and two perforations).
Limitations
The study was limited by its retrospective nature and small sample size.
Conclusions
This study demonstrates only a modest success rate of colonic stents in the treatment of malignant colonic obstruction. Although colonic stenting seems to be an effective method of relieving colonic obstruction, high failure rates limits its applicability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colonic obstruction due to colorectal cancer is a common clinical emergency with significant morbidity and mortality unless treated properly [1, 2]. Until two decades ago, the treatment for distal colonic or rectal tumors presented with acute obstructions was emergent surgery. However, emergent surgical interventions often require formation of a stoma, which is associated with considerable morbidity and a negative effect on quality of life [1, 2]. In search for a less invasive and less morbid treatment, colonic stent insertion was suggested as a mean for acute decompression in the early 1990s [3, 4]. Baron et al. [5] outlined two main indications for colonic stenting: The first as a bridge to surgery (BTS), thus increasing the chance for a one-step procedure with primary anastomosis. The second indication is palliation for patients who are inoperable or poor candidates for surgical intervention.
Although many studies examined stent insertion as a bridge to surgery and as palliation in incurable disease, much less data exists on stenting as a bridge to chemotherapy (BTC). In other words, the use of temporary decompression will allow systemic treatment as a first step until curative surgical capability is achieved. Colonic stenting during chemotherapy was reported in several studies aiming to assess long-term complications [6, 7], but not as part of a short course therapy as a first step before curative surgery.
The aim of the present study was to evaluate clinical success in three groups of patients according to pre-defined therapeutic goals: BTS as a bridge to one-step surgery, BTC as a bridge to chemotherapy, and P as a palliative measure. The innovation of the study lies within the BTC group. We evaluated whether colonic stenting and short course chemotherapy could be accomplished as scheduled, as a first step treatment before operating on patients with limited, potentially curable, metastatic disease.
Materials and methods
Patients
A retrospective analysis was done on all patients who presented with colonic obstruction and underwent insertion of a self-expanding metallic stent between January 2007 and May 2014. Institutional review board approval was obtained. Patients included in the study presented a left colonic or rectal obstruction with clinical signs including constipation, vomiting, abdominal pain, and abdominal distention, along with a radiological study determining the location of the obstruction. Patient demographics, clinical data, and follow-up medical and surgical treatment after stent insertion were analyzed. Patients were divided into three groups according to treatment goal: group 1, BTS; group 2, BTC; and group 3, P. Technical success rate, clinical outcome, and complications were recorded. Patients were followed up until an elective curative surgery was performed, a clinical stent-related complication that required emergent surgery occurred, or until patients’ death.
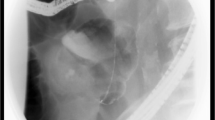
Procedure
All stent insertions were performed with a Boston Scientific Wallflex™, using a guide wire under fluoroscopy with a maximum length of 12 cm and a diameter of up to 22 mm. When the stricture would not allow passage of the stent introducer system, dilation was performed by using 8 or 10-mm through-the-scope (TTS) balloons. All stents were introduced by a senior and certified gastroenterologist after consent from the patients or their legal guardians.
Definitions and outcome
Patients were defined as success when reaching the pre-defined treatment goals. In the BTS group, success was defined as a restorative one-step procedure without colostomy. In the BTC group, a success was defined when the planned chemotherapy regimen was completed. In the P group, success was defined as relief of acute obstruction without surgical intervention until the latest follow-up. Stent complications were classified as obstruction/migration, perforation, and mortality.
Results
Stent insertion for colonic or rectal obstruction was attempted in a total of 45 patients; 43 patients had adequate follow-up. Patient demographics, tumor location, complications, and grouping are outlined in Table 1. Stent insertion succeeded in 32 out of the total 45 candidates (71.1 % technical success rate). In 13 patients, insertion failed (28.9 %), determining the need for a surgical resolution. Ten out of 13 patients were immediately operated; in 8 of them, a stoma was created, and in the other two a one-step procedure was feasible. Three patients were not operated immediately following failure of stent insertion. One patient was operated a month later due to colonic perforation and an ileostomy was performed. The second patient died before surgical treatment was attempted. The third patient refused surgical treatment and was referred to palliative care. Stent obstruction/migration occurred in seven patients (15.5 %) and perforation in three patients (6.7 %). Overall, stent complication rate was 22.2 %. Patients’ data was further analyzed according to the three pre-defined treatment goals: BTS, BTC, and P (Table 1).
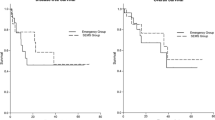
The BTS group included 11 patients. In this group, primary treatment goal was achieved in only 3 patients (27.2 %). The other eight patients (72.8 %) did not achieve the primary goal. Stent insertion failed in four patients (36.4 %). When stent insertion succeeded, the stent migrated in two patients and restoration of bowel continuity was not achieved in two patients (Table 2). One-step procedure rate was similar when comparing successful stent insertions and unsuccessful stent insertions (2/4 vs. 3/7 P = 0.8). In patients after successful stenting, the mean time to one-step procedure was 21.6 days (range 11–29 days). When one-step procedure failed, mean time to surgery was 38.7 days (range 29–63 days) (P = 0.08).
The BTC group included 12 patients who underwent stent insertion to enable systemic chemotherapy prior to surgery. Six patients (50 %) received systemic chemotherapy prior to surgery as planned. Six patients failed because of stent insertion failure, stent complications, and mortality (Table 3). Mean time to stent complication was 50 days (range 23–109 days). This group included seven patients who were referred by their attending physicians for a semi-elective procedure. All had technical success upon insertion. However, four of the seven patients (57 %) needed emergency surgical treatment during chemotherapy, due to stent complications, including stent perforation and migration.
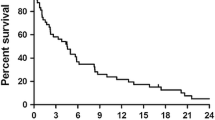
The P group included 20 patients who required stent insertion for palliation. In eight patients (40 %), long-term palliation was achieved after successful stenting, of which two patients needed re-stenting. In seven patients, stenting failed, four of them were operated on, while the other three refused surgery. Surgical intervention was performed due to failure of stent insertion in four patients, stent obstruction/migration in three patients, and stent-related perforation in two patients (Table 4).
Discussion
This study demonstrated limited success rates of stenting in achieving three pre-defined treatment goals of malignant colonic obstruction—BTS, BTC, and palliation. Previous studies included only two indications for the role of stents in the treatment of malignant colonic obstruction; BTS and palliation. Early publications concluded that colonic stenting is a feasible and safe therapeutic option. However, recent, large-scale prospective trials have cast doubt on the promising results shown in the past [8].
First comparative studies regarding stenting as a BTS were published in the beginning of the 2000s. Martinez-Santos et al. [9] compared patients treated with stent versus patients treated surgically, demonstrating a lower mortality and lower need for colostomy in the stented group. Obstruction was relieved in 95 % of the patients. The rate of severe complications was 12 % in the stented group while 41 % in the surgery group. Nevertheless, a meta-analysis of randomized clinical trials comparing stents as a BTS versus emergency surgery showed a technical success rate of only 70 % and a clinical and silent perforation rate as high as 20 % [8]. Kavanagh et al. [10] found that despite a high rate of technical success in selected patients with colonic obstruction, stenting had no impact on stoma rates. In a randomized clinical trial by Van Hooft et al. [11], stenting was associated with increased 30-day morbidity when compared to emergency surgery. In another prospective randomized, controlled trial, technical failure rate was as high as 53 % and perforation rate 7 % [12]. Moreover, some studies suggest worse oncological long-term outcome in patients with stent insertion compared to immediate surgery [13]. Our experience with colonic stenting as a BTS showed similar success and complication rates of stent insertion, when compared to recent meta-analysis. Success to achieve treatment goal was low (27 %), and there was no difference in stoma rates between successful and non-successful stenting. Moreover, when taking into account the reported association between adverse oncological results with the use of stenting, it is unreasonable to prioritize a one-step operation over oncological results. Quality of life issues are important but should be considered against oncological results. Therefore, stenting should generally be avoided. Nevertheless, elderly patients with curable disease, but with a low life expectancy, may benefit from a stenting approach. This group of patients may benefit on a quality of life aspect if a stoma is avoided. This recommendation pertains to recently published European guidelines [14].
In patients with incurable colorectal cancer (P group), early reports demonstrated good results with stenting when compared to surgery [14–16]. Lee et al. [17] compared stent insertion versus surgery for palliation. Stent insertion success rate was 95 %, and the complication rate was 15 %. In another comparative study of the palliative group, the rate of stent perforation was 6 %, and there was no difference in survival rates between the stenting and surgery groups (13.7 vs. 11.4 months, respectively) [18]. However, other studies [19] indicated a higher stent-related morbidity rate (38 %), and high perforation and stent-related mortality rates (13 %). Moreover, a prospective randomized controlled trial by Van Hooft et al. [11] comparing the use of stents to surgery had to be terminated prematurely because of high perforation rates (40 %). Our experience regarding palliative treatment with colonic stents suggests that the majority of colonic stents introduced for palliation fail to give patients long-term palliation. Nonetheless, often no other therapeutic options for relief are applicable. Therefore, although there is a high failure rate, stents should be considered in the severely ill patient with a short life expectancy or in the patient with disseminated peritoneal spread and a hostile abdomen.
Stenting to enable chemotherapy before surgery (BTC) in patients with potentially curable metastatic disease has not been addressed directly in the literature. Fernandez-Esparrach et al. [7] concluded that stenting should be avoided in patients with curable malignant disease because of long-term complications of the stent. Reports on the relationship between a higher risk of perforation and treatment with bevacizumab have limited the therapeutic regimens available for patients with malignant disease [6, 19–21]. In this study, the stent failed during chemotherapy in 40 % of patients. Therefore, stent insertion interfered with the planned regimen of chemotherapy. We suggest performing a stoma for bowel decompression, so as to enable the full chemotherapy regimen to be given without interruption. Another question that needs to be addressed is in regards to the long-term oncological outcome. It would not be reasonable to make an effort to comply with a chemotherapeutic regimen if the means for accomplishing it (i.e., stenting) has an adverse oncological effect. A multicenter comparative study of survival and oncological outcomes in stented versus diverted patients will clarify this conflict.
The limitation of our study lies within its retrospective design and limited number of patients. Therefore, results reported should be interpreted with caution. Nevertheless, the study results are in line with data from current literature and confirm the poor success rate of colonic stents in treatment of colonic obstruction. Moreover, other studies demonstrated worse oncologic results with the use of stents in malignant colonic obstruction. Therefore, in the potentially curable patient, stenting should be avoided.
Conclusions
This study confirms the results from current literature that although colonic stenting seems to be effective for relieving malignant colonic obstruction, high failure rates to achieve pre-defined treatment goals makes its applicability limited. Stent insertion should be considered for end-stage patients with short life expectancy and in selected patients. However, its routine as a BTS or BTC should be avoided.
References
Sagar J (2011) Colorectal stents for the management of malignant colonic obstructions. Cochrane Database Syst Rev 11
Breitenstein S et al (2007) Systematic evaluation of surgical strategies for acute malignant left-sided colonic obstruction. Br J Surg 94(12):1451–1460
Mainar A et al (1996) Colorectal obstruction: treatment with metallic stents. Radiology 198(3):761–764
Tejero E et al (1994) New procedure for the treatment of colorectal neoplastic obstructions. Dis Colon Rectum 37(11):1158–1159
Baron TH et al (1998) Expandable metal stents for the treatment of colonic obstruction: techniques and outcomes. Gastrointest Endosc 47(3):277–286
Cennamo V et al (2009) Does stent placement for advanced colon cancer increase the risk of perforation during bevacizumab-based therapy? Clin Gastroenterol Hepatol 7(11):1174–1176
Fernandez-Esparrach G et al (2010) Severe complications limit long-term clinical success of self-expanding metal stents in patients with obstructive colorectal cancer. Am J Gastroenterol 105(5):1087–1093
Tan CJ, Dasari BV, Gardiner K (2012) Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Br J Surg 99(4):469–476
Martinez-Santos C et al (2002) Self-expandable stent before elective surgery vs. emergency surgery for the treatment of malignant colorectal obstructions: comparison of primary anastomosis and morbidity rates. Dis Colon Rectum 45(3):401–406
Kavanagh DO et al (2013) A comparative study of short- and medium-term outcomes comparing emergent surgery and stenting as a bridge to surgery in patients with acute malignant colonic obstruction. Dis Colon Rectum 56(4):433–440
van Hooft JE et al (2007) Colonic stenting as bridge to surgery versus emergency surgery for management of acute left-sided malignant colonic obstruction: a multicenter randomized trial (Stent-in 2 study). BMC Surg 7:12
Pirlet IA et al (2011) Emergency preoperative stenting versus surgery for acute left-sided malignant colonic obstruction: a multicenter randomized controlled trial. Surg Endosc 25(6):1814–1821
Sabbagh C et al (2013) Is stenting as “a bridge to surgery” an oncologically safe strategy for the management of acute, left-sided, malignant, colonic obstruction? A comparative study with a propensity score analysis. Ann Surg 258(1):107–115
Faragher IG, Chaitowitz IM, Stupart DA (2008) Long-term results of palliative stenting or surgery for incurable obstructing colon cancer. Colorectal Dis 10(7):668–672
Jung MK et al (2010) Factors associated with the long-term outcome of a self-expandable colon stent used for palliation of malignant colorectal obstruction. Surg Endosc 24(3):525–530
Vemulapalli R et al (2010) A comparison of palliative stenting or emergent surgery for obstructing incurable colon cancer. Dig Dis Sci 55(6):1732–1737
Lee HJ et al (2011) Long-term outcome of palliative therapy for malignant colorectal obstruction in patients with unresectable metastatic colorectal cancers: endoscopic stenting versus surgery. Gastrointest Endosc 73(3):535–542
Karoui M et al (2007) Stents for palliation of obstructive metastatic colon cancer: impact on management and chemotherapy administration. Arch Surg 142(7):619–623, discussion 623
Fuccio L, Cennamo V (2010) Bevacizumab-based therapy and complication risk after colonic stent placement: is it time for a warning? Gastrointest Endosc 72(6):1330, author reply 1330-2
Small AJ, Coelho-Prabhu N, Baron TH (2010) Endoscopic placement of self-expandable metal stents for malignant colonic obstruction: long-term outcomes and complication factors. Gastrointest Endosc 71(3):560–572
van Halsema EE et al (2014) Perforation in colorectal stenting: a meta-analysis and a search for risk factors. Gastrointest Endosc 79(6):970–82.e7, quiz 983.e2, 983.e5
Acknowledgments
The authors thank Moshe Rubin, M.D. for his assistance and valuable comments.
Author information
Authors and Affiliations
Corresponding author
Additional information
Nir Horesh and Joseph Dux contributed equally to this work.
Rights and permissions
About this article
Cite this article
Horesh, N., Dux, J.Y., Nadler, M. et al. Stenting in malignant colonic obstruction—is it a real therapeutic option?. Int J Colorectal Dis 31, 131–135 (2016). https://doi.org/10.1007/s00384-015-2375-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2375-7