Abstract
Background
Fundoplication is considered a mainstay in the treatment of gastro-esophageal reflux. However, the literature reports significant recurrences and limited data on long-term outcome.
Aims
To evaluate our long-term outcomes of antireflux surgery in children and to assess the results of redo surgery.
Methods
We retrospectively analyzed all patients who underwent Nissen fundoplication in 8 consecutive years. Reiterative surgery was indicated only in case of symptoms and anatomical alterations. A follow-up study was carried out to analyzed outcome and patients’ Visick score assessed parents’ perspective.
Results
Overall 162 children were included for 179 procedures in total. Median age at first intervention was 43 months. Comorbidities were 119 (73 %), particularly neurological impairments (73 %). Redo surgery is equal to 14 % (25/179). Comorbidities were risk factors to Nissen failure (p = 0.04), especially children suffering neurological impairment with seizures (p = 0.034). Follow-up datasets were obtained for 111/162 = 69 % (median time: 51 months). Parents’ perspectives were excellent or good in 85 %.
Conclusions
A significant positive impact of redo Nissen intervention on the patient’s outcome was highlighted; antireflux surgery is useful and advantageous in children and their caregivers. Children with neurological impairment affected by seizures represent significant risk factors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gastro-esophageal reflux (GOR) is one of the most prevalent foregut diseases in pediatric patients. Fundoplication is considered the treatment of choice when GOR is refractory to medical therapy [1].
Despite this procedure is almost considered a mainstay in the management of GOR, the literature reports described significant morbidity and recurrences, standing at approximately 6 and 48 % [2–5].
Furthermore, the pediatric population requiring this procedure is extremely heterogeneous, including patients with neurological impairment and neuromuscular disorders that are difficult to manage under a unique treatment strategy and poorly adapted to a common assessment. Some authors described a higher incidence of recurrence in children affected by cerebral palsy and they suggested how this aspect could justify such a difference range of redo procedure [6, 7]. Generally, comorbidities and even early age at first intervention were identified as predictors of possible failure of Nissen procedure [5, 8].
Indications for surgery or abstaining from intervention, which type of antireflux surgery performed, including the esophagus-gastric disconnection, are frequent surgical discussion subjects and a source of doubt for the pediatric surgeon; this also applies to the interpretation of reported treatment failure and surgical indications that led to the redo procedure.
We retrospectively analyzed our results in managing failed antireflux surgery using the same technique by the same surgical team, in a mixed group of patients in a tertiary pediatric referral center. We hereby present a large series of data, including the long-term outcomes of antireflux surgery and tried to determine the failure rate and the mechanism of failure and to disentangle questions and controversies regarding use and safety of this procedure in recurrent disease.
Materials and methods
All patients consecutively evaluated at Gaslini Children’s Hospital who underwent Nissen fundoplication between June 2006 and June 2014 were reviewed, after formal approval of Ethical Committee.
Exclusion criteria were congenital anatomic anomalies of the esophagus (trachea-esophageal fistula and duplication) or the diaphragm (congenital diaphragmatic hernia), in order to limit fault regarding congenital anatomic alterations.
Data collected included demographic details, surgical indications, age, and weight at the time of the first intervention, the presence of comorbidities, the presence of previously placed gastrostomy, post-operative course including complications related to fundoplication, long-term outcome, and the need of re-operation.
All data were stored in a digital database according to the Personal Data Protection Act.
Surgery was indicated in children with complicated persistent primary GOR or GOR associated with other comorbidities, such as severe dysphagia with feeding intolerance, recurrent vomiting and inability to gain weight, neurologically impairment (cerebral palsy, spasticity, and seizure disorder), neuromuscular disorders (spinal muscular atrophy 1—SMA1), and severe esophagitis or Barrett esophagus. Patients with important neurologic disability were not able to walk, profoundly retarded and not able to communicate verbally.
Pre-operative evaluation included an upper gastrointestinal (GI) study to evaluate the anatomy of the esophagus, the stomach and the duodenum, the presence of reflux during the exam and/or presence of any para-esophageal herniation or malrotation, and any delay in gastric emptying.
Upper endoscopy and/or 24-h pH metering (pH-MII) were done when deemed clinically necessary.
Open or laparoscopic approach was performed with the same surgical technique previously described [9, 10].
Persistent or recurrent GOR was defined by clinical evidence of symptoms confirmed by upper GI evaluation and endoscopy and/or pH-MII monitoring when clinically required.
Reiterative surgical procedure was indicated in case of persistent symptoms and GOR associated with
-
absent or incompetent wrap;
-
migration of the wrap across the diaphragm; and
-
hiatal hernia.
Any X-ray examination was done whenever GOR symptoms recurred after surgery. Redo procedures were not offered in our series to asymptomatic patients, especially in children with cerebral palsy or neuromuscular pathologies.
Regarding the follow-up study, all patient caregivers were phone called by a physician not involved in the medical and surgical management and asked about patient’s symptoms and their quality of life. Need for pump protonic drug for a long period of time after surgery (at least 3 months), dysphagia, drooling, gas bloating, ability to vomit, dumping syndrome, frequent cough or recurrent airways infections (more than 1 episode in a year), and the good quality of life were investigated. Patients’/parents’ perspective of overall outcome was assessed according to modified Visick score (1–4: no symptoms, mild symptoms easily controlled, major symptoms not controlled, failure) [11, 12]).
In case of re-operation, data collection included: risk factors (SMA1, neurological impairment, Barrett esophagus), hiatal and wrap anatomical aspect and position, type of redo surgery, and need of diaphragmatic patch. Second outcome analysis was done in case of redo surgery.
Data were expressed as ratios, or as median and range. Differences in the frequencies of each categorical variable were evaluated by the Chi square test, or by the Fisher exact test when appropriate. A p value lower than 0.05 was considered statistically significant. Analyses were performed using Stata for Windows statistical package (release 9.0, Stata Corporation, College Station, TX). We used Bonferroni’s correction for multiple testing, when appropriate [13].
Results
In the 8-year period, 162 patients who consecutive underwent a Nissen fundoplication were included, for 179 procedures in total. Our study population comprised patients from our institution and those referred from outside institutions (8 patients).
There were 100 (62 %) males.
At the time of first intervention, median age was 43 months (range 1–290) and median weight was 11 kg (range 3–80). It is to be noticed that 34 (21 %) patients were operated before at 12 months of age (median age 9 months with range 1–12).
Overall comorbidities were 119 (73 %): 87 (73 %) neurological impairments and 32 (27 %) neuromuscular disorders.
Figure 1 describes all surgical indications that led to the intervention. Sixty-one (38 %) patients undergoing Nissen procedure with the symptom of severe dysphagia also associated with vomit; they were all affected by neurological impairment, inability to food, and gain weight.
All 162 patients underwent open (11/162 = 7 %) or laparoscopic (151/162 = 93 %) Nissen fundoplication. Concomitant gastrostomy (82 Stamm and 12 endoscopic procedures PEG) was performed in 94 (58 %) children; proximal Roux-en-Y gastrojejunal diversion in 14 (9 %) patients. Gastrostomy was previously placed in 23 (14 %) patients, all Stamm procedure except one endoscopically place. Only five patients required a gastrostomy after Nissen procedure, 2 Stamm and 3 percutaneous endoscopic gastrostomy (PEG).
There was no operation-related death during the study period. Seven (4 %) patients died for baseline disease-related cause: six children died because of cardio circulatory shock due to underlying cardiac anomaly; the other died for sepsis unrelated to the fundoplication.
Redo surgery
The median time from initial fundoplication to diagnose of first failure was 20 months (range 9–55).
Twenty-one (21/162 = 13 %) patients underwent a first redo procedure overall; 71 % (15/21) performed the first Nissen procedure at Gaslini Children’s Hospital (15/154 = 10 %) during the period of study, except one child who was operated in the same center before 2006. Median age at redo surgery was 73 months (range 12–249). Failure rate for neurologically impaired was 52 % (11/21).
During the redo surgery, we identified the surgical findings of failed fundoplication described below:
-
Herniation of the wrap into the posterior mediastinum (“slipped Nissen”) (3 patients);
-
Disruption of the wrap (9 patients); and
-
Combination of herniation and disruption (9 patients).
No tight wrap was documented in this series. The stomach was reduced in the abdomen, if herniation was present, and a redo Nissen fundoplication was performed in all cases. Nine (9/21 = 43 %) diaphragmatic patch were left in place; four (4/9 = 44 %) were absorbable prosthesis.
Overall revision “Gaslini’s surgery” failed to solve the symptoms in three (3/21 = 14 %; 3/162 = 2 %) children; after radiological confirmation, four patients required third Nissen procedure: one was referral to us by other pediatric center after two fundoplication. Three (75 %) combinations of herniation and disruption and one herniation of the wrap into the mediastinum were recorded. None had previously placed a diaphragmatic prosthesis. During the second Nissen intervention, we placed three prosthetic reinforcements, all non-absorbable.
Overall redo surgery is equal to 14 % (25/179). If we considered the “Gaslini’s redo surgery,” the incidence rate dropped to 10 % (15 + 3 = 18/179 = 10 %).
Four (12 %) children who underwent surgery before 1 year of age were re-operated; the age at intervention was deemed not statistically significant (p = 1).
Regarding the Nissen indication, the presence of Barrett’s esophagus and/or respiratory symptoms is not statistically significance associated with a higher incidence of redo surgery (p = 0.24 and p = 0.77, respectively).
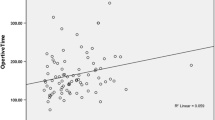
Comorbidities were risk factors to lead to Nissen fundoplication failure (p = 0.04). In particular, children suffering neurological impairment with seizures (6/21 epilepsy = 29 %; p = 0.034).
Follow-up study
The mean follow-up time was 51 months (range 7–101). Fifteen (15/111 = 13 %) patients had a follow-up study between 7 months and 1 year after the fundoplication. Complete and exhaustive follow-up data sets on long-term outcome could be obtained for 111 (111/162 = 69 %), and an informed consent was obtained from each patient. Thirteen (8 %) patients went back to their origin country and we only know that they did not perform redo surgery; other specific details were not registered because of language hindrances. The remaining 38 (23 %) patients were either not available or refused to participate.
Eighty-four (84/111 = 76 %) patients were syndromic (66 patients with cerebral palsies/neurodevelopmental delays and 18 with neuromuscular disorders); this means that 71 % (84/119) of overall syndromic and 58 % (25/43) of non-syndromic patients collaborated on the follow-up study.
Table 1 shows the symptoms present after performing Nissen fundoplication (second column) considering the presence of the same symptoms before the intervention itself (first column). Overall after surgery, 8 (8/36 = 22 %) patients who were full/partial feed orally complained of transitory dysphagia for some solid food, 10 (10/111 = 9 %) of drooling, 14 (14/111 = 13 %) of gas bloating with 79 % (11/14) who performed ventilatory support at night, 10 (10/111 = 9 %) of vomit (at least one episode after surgery). Two (2/111 = 2 %) patients experienced dumping syndrome and 20 (20/111 = 18 %) recurrent airways infections.
Proton pump inhibitors (PPI) were administrated in 44 patients (44/111 = 40 %) routinely, even after 3 months after surgery; many patients remained on PPI, although without symptoms. Patients’ and parents’ perspectives proved to be excellent (no symptoms) or good (mild occasional symptoms easily controlled) in 94 children (85 %).
Patients who underwent a redo Nissen fundoplication were compared to a group of 90 patients who underwent a single effective procedure. Table 2 shows the comparison of overall follow-up results. Male to female ratio, weight at intervention, and length of follow-up were comparable.
Among nine selected outcome parameters, none was significantly and undoubtedly interfered by repeated Nissen fundoplication.
Discussion
Nissen fundoplication procedure has changed radically the GOR management in both adults and children. However, the possibility of major complications and redo surgery still persist and it is considered a noteworthy variable according to the international literature. In order to evaluate post-operative outcomes, we must able to define the term “failure” in clinical practice; it seems puzzling and even absurd but actually there is no a uniform definition of failure antireflux surgery [14], especially if we are talking about syndromic patients. Generally, Nissen fundoplication failure is associated with post-operative complications linked to maintenance the anatomical “rebuilt,” the persistence of symptoms, the continuous use of antireflux medications, and the satisfaction and quality of life level. Besides, we must point out as not all these parameters underlying a failure: in fact, children with post-operative symptoms do not necessarily have a wrap disruption or a wrap migration. Khajanchee et al. demonstrated with an abnormal DeMeester score system that more than 20 % of children, who complained symptoms after surgery, had perfectly normal 24-h pH metering [15].
In our series, we recorded a fair number of post-operative symptoms. Kamolz et al. describe that immediately after surgery, up to 100 % of the children who underwent fundoplication suffered from temporary dysphagia and this symptom usually ablated within 3 months after surgery [16]. We found 20 % of patients, full or partial feeding by mouth, with occasional swallowing problems that we included under the heading “dysphagia,” but without any objective correlation (negative upper GI study and/or endoscopy evaluation). It has been proposed that neurologically impaired children, who represent a huge part of our population, were affected by a pre-existing gastric dysrhythmia, which could lead to retching and dysphagia itself [17]. Moreover, probably emotional/psychological factors play a pivotal role in this group of children, as already suggested by others [18].
Many authors stress about the need to investigate vomiting after an antireflux surgery [19, 20]. Historically, the 360° fundoplication was inextricably linked to vomit inability; the appearance of symptom generally implied the failure of surgery. Nine percent of our patients present at least one episode of vomit after Nissen fundoplication but the contrast studies failed to demonstrate any mechanical problem with the wrap and/or the crura. Some investigators moreover performed a subsequent ph-probe and upper GI endoscopy in these symptomatic patients without a solving problem [21]. We should attribute the symptom to the abnormal pathway of gastric emptying and the vagal nerve dysfunction that affected this group of children, considering the absence of objective radiological finding [22].
More difficult is the evaluation of neurological patients who complain drooling, especially in our population in which the symptom falls into their baseline disease. In fact, some studies do not include the sialorrhoea as symptom of provided failure [23].
In our series, a significant number of patients suffer from recurrent airways infections, more than one episode per year. We can speculate that the high number of patients could be overestimated, because more than one episode of respiratory infections per year could be happen to a healthy child without comorbidities. Moreover, Morgenthal et al. reflect on the multifactorial genesis of respiratory symptoms with regard to GOR: it is unclear what is the mechanism by which the healing from reflux symptoms does not completely eliminates also the respiratory symptom; in fact, the family is often partially unhappy with the result obtained after the fundoplication [24].
We reported a fairly large group of children that used IPP medications after surgery, although without feel reflux symptoms. The answer given by the family regarding the drug use was aspecific and little contextualized (“The general practitioner said me: Go head with the IPP some more, than we will see”). Some researchers described the lack of correlation between symptoms and use of medications, showing that the vast majority of patients were taking PPI, had a pH study with a normal distal esophagus acid exposure [25].
One of the possible risk factors that induced failure Nissen fundoplication was epilepsy, as frequently mentioned in the literature. Repeatedly, increased abdominal pressure and prolonged relaxations of the lower esophageal sphincter due to a direct vagal effect are the principle cause of herniation or disruption of the wrap [26, 27]. We also showed a significant correlation between cerebral seizures and recurrence of GOR and considering the result, we suggested to carefully investigate patients with seizures disorders even without detecting any GOR symptoms.
Regarding follow-up time and the correlation with symptoms of recurrent GOR, we are in line with Pashankar et al., who highlighted as GOR symptoms occurred 4.9 years after last fundoplication [23]. Moreover, we showed a quite low rate of complication, compared with the international literature, after Nissen fundoplication, while avoiding patient’s selection (high prevalence of neurological patients).
We ourselves said that there are some limitations in this study. First of all, the information obtained with a retrospective study could be incomplete and may be uncontrolled. Moreover, a phone follow-up study may result aspecific or not completely accurate and would be optimally performed in a prospective way. By contrast, the same surgical team carried out all surgical procedures, with only two surgeons involved and the study is entirely taken place in a tertiary pediatric referral center.
Moreover, another limitation is the possible loss of follow-up for some of our patients due to either transition of care to adult physicians and surgeons or migration of family to abroad areas.
We emphasize that, despite the countless surgical fundoplication techniques, we decided to use only 360° Nissen procedure because of consolidated learning curve and standardized skills. Regarding the esophagus-gastric disconnection, we can only expose our personal doubts about the high number of complications recorded in the literature [28] but did not provide data to support this statement.
In this retrospective study, we want to emphasize that the presence of residual symptoms after fundoplication not involve a “surgical defeat,” especially considering the level of satisfaction shown by patient’s caregivers.
To conclude, Nissen fundoplication would appear a safe and effective procedure for treating GOR in pediatric age, because of reliable outcome and reasonable number of recurrence. This study demonstrated a significant positive impact of redo Nissen intervention on the patient's outcome and the redo surgery does not particularly result in morbidity and mortality in neurologically impaired children in the hands of experienced laparoscopic surgeon. Complications leading to a redo Nissen fundoplication could be related with neurological patients affected by seizures, who represent significant risk factors. Most surgical problems are preventable by experienced surgical and medical team. Despite a quite high rate of symptomatic patients, the overall effect of surgery on quality of life is outstanding. We can comfortably say that antireflux surgery is useful and advantageous in children and their caregivers, without considering their neurological status and we can define, considering the results, that this experience is not a Nissen fundoplication failure.
References
Horgan S, Pellefrini CA (1977) Surgical treatment of gastroesophageal reflux disease. Surg Clin North Am 77:1063–1082
Rothemberg SS (2006) Laparoscopic redo Nissen fundoplication in infants and children. Surg Endosc 20:1518–1520
Wheatley M, Coran A, Wesley J et al (1991) Redo fundoplication in infants and children with recurrent gastroesophageal reflux. J Ped Surg 26:758–761
Taylor LA, Weiner T, Lacey SR et al (1994) Chronic lung disease in the leading risk factor correlating with the failure (wrap disruption) of antireflux procedures in children. J Pediatr Surg 29:161–164
Pacilli M, Eaton S, Maritsi D et al (2007) Factors predicting failure of redo Nissen fundoplication in children. Pediatr Surg Int 23:499–503
Sydorak RM, Albanese CT (2002) Laparoscopic antireflux procedures in children. Evaluating the evidence. Semin Laparosc Surg 9:133–138
Zeid MA, Kandel T, El- Shobary M et al (2004) Nissen fundoplication in infants and children: a long term clinical study. Hepatogastroenterology 51:697–700
Baerg J, Thorpe D, Bultron G et al (2013) A multicentre study of the incidence and factors associated with redo Nissen fundoplication in children. J Pediatr Surg 48:1306–1311
Mattioli G, Repetto P, Leggio S et al (2002) Laparoscopic Nissen-Rossetti fundoplicatio in children Semin Laparosc Surg 9:153–162
Mattioli G, Buffa P, Gandullia P et al (2009) Laparoscopic proximal Roux-en-Y gastrojejunal diversion in children: preliminary experience from a single center. J Laparoendosc Adv Surg Tech A 19:807–813
Visik AH (1948) A study of the failures after gastrectomy. Ann R Coll Surg Eng 3:266–284
Rijnhart-De Jong HG, Draaisma WA, Smout AJPM (2008) The Visick score: a good measure for the overall effect of antireflux surgery? Scand J Gastroenterol 43:787–793
Sankoh AJ, Huque MF, Dubey SD (1997) Some comments on frequently used multiple endpoint adjustments methods in clinical trials. Stat Med 16:2529–2542
Johnson DA (2004) Endpoints for the assessment of response to gastroesophageal reflux disease therapy—what are the appropriate measures of ‘‘success’’? Rev Gastroenterol Disord 4:118–129
Khajanchee YS, O’Rourke RW, Lockhart B et al (2002) Postoperative symptoms and failure after antireflux surgery. Arch Surg 137:1008–1014
Kamoltz T, Granderath A, Bammer T et al (2002) Dysphagia and quality of life after laparoscopic Nissen fundoplication in patients with and without prostetic reinforcement of the hiatal crura. Surg Endosc 16:572–577
Richards CA, Andrews PL, Spitz L et al (1998) Nissen fundoplication may induce gastric myoelectrical disturbance in children. J Pediatr Surg 33(12):1801–1805
Kamolz T, Granderath FA, Bammer T et al (2001) Psychological intervention influences the outcome of laparoscopic antireflux surgery in patients with stress-related symptoms of gastroesophageal reflux disease. Scand J Gastroenterol 36:800–805
Oldham K, Massey M (1998) Antireflux surgery. In: Stringer M (ed) Pediatric surgery and urology: long term outcomes. Saunders, Philadelphia, pp 189–213
Rice H, Seashore J, Touloukian R (1991) Evaluation of Nissen fundoplication in neurologically impaired children. J Pediatr Surg 26:697–701
Kimber C, Kiely EM, Spitz L (1998) The failure rate of surgery for gastro-oesophageal reflux. J Pediatr Surg 33:64–66
Jolley SG, Tunell WP, Leonard JC et al (1987) Gastric emptying in children with gastroesophageal reflux. The relationship to retching symptoms following antireflux surgery. J Pediatr Surg 22:927–930
Pashankar D, Blair GK, Israel DM (2001) Omeprazole maintenance therapy for gastroesophageal reflux disease after failure of fundoplication. J Pediatr Gastroenterol Nutr 32:145–149
Morgenthal CB, Lin E, Shane MD et al (2007) Who will fail laparoscopic Nissen fundoplicatio? Preoperative prediction of long term outcome. Surg Endosc 21:1978–1984
Lord RVN, Kaminski A, Oberg S et al (2002) Absence of gastroesophageal reflux disease in a majority of patients taking acid suppression medications after Nissen fundoplication. J Gastrointest Surg 6:3–10
Maxson RT, Harp S, Jackson RJ et al (1994) Delayed gastric emptying in neurologically impaired children with gastroesophageal reflux: the role of pyloroplasty. J Pediatr Surg 29(6):726–729
Subramaniam R, Dickson AP (2000) Long-term outcome of Boix-Ochoa and Nissen fundoplication in normal and neurologically impaired children. J Pediatr Surg 35(8):1214–1216
Danielson PD, Emmens RW (1999) Esophagogastric disconnection for gastroesophageal reflux in children with severe neurologic impairment. J Peditr Surg 34:84–87
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rossi, V., Mazzola, C., Leonelli, L. et al. Long-term outcome and need of re-operation in gastro-esophageal reflux surgery in children. Pediatr Surg Int 32, 277–283 (2016). https://doi.org/10.1007/s00383-015-3853-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-015-3853-2