Abstract
Purpose
Outcomes of fundoplication in children.
Methods
In this monocentric retrospective study, chart review was performed on children who underwent fundoplication between 2006 and 2013. Outcomes were defined as the need for redo fundoplication and recommencement of anti-reflux medication (ARM) at 6-month follow-up.
Results
119 patients underwent fundoplication with a mean age of 4.76 years and 55.5 % of these were male. At 6-month follow-up, 21 (17.6 %) required redo fundoplication and 64 (53.8 %) were recommenced on ARM. Post-operative complications occurred in 50 (42.2 %) of children; 30 % of those with complications had surgery at less than 1 year of age, and 36 % had an associated comorbid condition. Neither being under the age of one nor associated comorbidity was significantly associated with a poor outcome. Concurrent gastrostomy was associated with a higher risk of being back on ARM at 6-month follow-up (p = 0.003). Neither gastrointestinal or respiratory symptoms pre-surgery nor abnormal pre-operative investigations including pH monitoring and endoscopy were predictive of poor outcome post-fundoplication.
Conclusion
Although fundoplication has a role in the treatment of severe GORD in children, the majority of children in this study needed to restart their anti-reflux medications within 6 months of surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Gastroesophageal reflux (GOR) is a normal physiological process that usually happens after eating in healthy infants, children, young people and adults. In contrast, gastroesophageal reflux disease (GORD) occurs when the effect of GOR leads to symptoms and/or complications severe enough to merit medical treatment.
Medical treatment of GORD usually involves acid suppression therapy [proton pump inhibitors (PPI) or H2 receptor antagonists (H2RA)], as well as supplemental enteral feeding if weight gain is an issue.
Fundoplication is currently recommended for the management of severe GORD where medical treatment has been unsuccessful, or feeding regimens to manage GORD prove impractical [1]. Fundoplication surgically prevents GOR by correcting hiatal herniation, lengthening the intra-abdominal portion of the oesophagus, tightening the crura and increasing the pressure at the lower oesophageal sphincter [2]. It is highly effective therapy for carefully selected patients with chronic GORD when performed by an experienced surgeon [3].
Clinical guidelines are well established to aid clinicians diagnose, investigate and medically treat GORD; however, current guidelines do not define ‘unsuccessful medical therapy’, nor do they provide guidance on timing of surgical intervention, or patient selection. They do, however, suggest performing an upper GI endoscopy with oesophageal biopsies and a contrast study for children before deciding whether to offer fundoplication, and encourage clinicians to consider performing other investigations such as pH/impedance monitoring ± manometry as part of their pre-operative workup [1].
There are few studies in the medical literature assessing outcomes of fundoplication in paediatric GORD. Those that exist are focused on comparing surgical techniques.
Aims
The purpose of this study was to look at outcomes of fundoplication at a tertiary children’s hospital. Variables looked at included patient selection and post-fundoplication complications. As a secondary aim, we also looked for any pre-operative predictive factors that could assist in patient selection and improved outcomes post-fundoplication.
Methods
This was a monocentric retrospective study based on chart review. Patients from our institution aged between zero and 18 who underwent fundoplication between 2006 and 2013 were included. Sydney Children’s Hospital is a major tertiary teaching hospital, with five surgeons performing fundoplications during this 7-year period. Medical records of the 119 patients who met the inclusion criterion were reviewed. Patients were excluded if they were lost to follow-up by 6-month post-fundoplication. During the process of data collection, the data were de-identified to ensure privacy of participants and reduce risk of bias.
The following information was recorded:
-
1.
Demographics (age and sex).
-
2.
Comorbidities [neurological impairment (NI), repaired oesophageal atresia/trachea-oesophageal fistulas (OA/TOF) and cystic fibrosis (CF)]. Neurological impairment was defined as static or progressive, central and/or peripheral neurological diagnoses associated with functional and/or intellectual impairment (e.g. cerebral palsy, trisomy 21, and global developmental delay).
-
3.
Use of anti-reflux medications [PPI, H2RA and prokinetic agents (erythromycin or domperidone)].
-
4.
Gastrointestinal symptoms. Gastrointestinal symptoms of GORD were defined as persistent regurgitation/vomiting, epigastric pain and/or irritability, feeding difficulties including refusal and failure to thrive [4, 5].
-
5.
Respiratory symptoms. Respiratory symptoms were defined as chronic or nocturnal cough, recurrent aspiration/recurrent chest infections, cyanotic episodes, apparent life threatening events (ALTE), stridor and otitis media [6].
-
6.
Pre-operative investigations (pH probe, endoscopy, pepsin assay as a marker or reflux microaspiration and gastric emptying study).
-
7.
Surgical technique (open vs laparoscopic).
-
8.
Concurrent procedures (insertion of a gastrostomy or pyloroplasty) at time of fundoplication.
-
9.
Post-fundoplication complications (gagging/retching, dumping syndrome, gas bloat and dysphagia).
-
10.
Hospitalisations in the 12-month pre- and post-fundoplication.
-
11.
Outcomes were defined as the need for redo fundoplication, and or recommencement of anti-reflux medications (ARM) at 6-month follow-up post-surgery.
Statistical analysis was completed using SPSS v17.0 for Windows (descriptive statistics and univariate binary logistic regression analysis) and Graph Pad (Chi-squared tables, Fisher’s exact and Wilcoxon’s tests).
We isolated each variable in the collected data and ran univariate binary logistic regression analysis, with the aim of identifying any significant individual pre-operative factor which impacted either outcome.
Approval for this study was obtained from the Human Research Ethics Committee at Sydney Children’s Hospital, Randwick (LNR/13/SCHN/42).
Results
Patient demographics
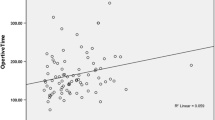
A total of 119 patients underwent fundoplication, with a mean age of 4.76 years (SD 4.76) (Fig. 1) and 55.5 % male gender. 9 (7.6 %) patients underwent open fundoplication, the majority (110, 92.4 %) of fundoplications were performed laparoscopically. 29 (24.4 %) children had a comorbid condition [20 (16.8 %) NI, 7 (5.9 %) OA/TOF and 2 (1.7 %) CF]; there were no patients with two or more comorbidities. Anti-reflux medications were used pre-operatively in all patients [99 (83.2 %) PPI, 53 (44.5 %) H2RA, and prokinetic agents 43 (36.1 %)]. 74 (62.2 %) children were on more than one medication; PPI and H2RA 48 (40.3 %) or PPI and prokinetic 43 (36.1 %).
Indications for fundoplication
Persistent regurgitation/vomiting was the most common gastrointestinal symptom (67, 56.3 %), followed by epigastric pain and/or irritability (55, 46.2 %) and feeding difficulties including refusal (27, 22.7 %). The two most commonly reported respiratory symptoms were recurrent chest infections/recurrent aspiration (46, 38.6 %) and nocturnal cough (22, 18.5 %).
Surgical technique
Surgeons in our centre routinely perform 360 degree Nissen fundoplication. All fundoplications in our study were performed with this technique. 9 (7.6 %) procedures were the open fundoplications, the rest (110, 92.4 %) were performed laparoscopically. Open fundoplications had a lower rate of redo (0 %, p = 0.0001) but higher rate of ARM recommencement (88.9 %, p = 0.01). All surgeons performing laparoscopic fundoplication had more than 10 years’ experience in this field.
Outcomes post-fundoplication
At 6-month follow-up, 21 (17.6 %) children required redo fundoplication, and 2 of these (1.7 %) required more than 1 redo fundoplication. 64 (53.8 %) patients were recommenced on anti-reflux medication. 62 (52 %) were symptom free. In the subgroup of 23 (19.3 %) infants <1 year of age who underwent fundoplication, 3 (13 %) had redo fundoplication and 15 (65.2 %) needed ARM within 6-month post-surgery. Being under the age of 1 was not significantly associated with either outcome. Gender was not significantly associated with either outcome. In children with NI, 4 (21 %) had redo fundoplication and 10 (52.6 %) were recommenced on ARM. There was no statistically significant correlation between presence of comorbidity and either outcome, even when looking specifically at the NI or OA/TOF cohorts. Even the subgroup of patients who were both under the age of 1 and had associated comorbidity did not have a significantly higher need for redo fundoplication or need to recommence ARM at 6-month follow-up.
The univariate analysis identified no variable [age, gender, individual comorbidities and symptomatology (gastrointestinal or respiratory)] which was statistically significant (p < 0.05) for either outcomes. However, there was a trend towards significance with one of the pre-operative symptoms—nocturnal cough (p = 0.06). Chronic cough (including nocturnal cough), however, was not predictive of either outcome.
Results of pre-operative investigations and their influence on outcome post-fundoplication are shown in Table 1. There was no statistically significant correlation between the presence of abnormal results in any of the pre-operative investigations and either of the outcomes post-fundoplication.
Effect of concurrent surgery on fundoplication outcomes
38 (31.9 %) patients underwent a gastrostomy with their fundoplication, whilst 10 (8.4 %) had a pyloroplasty performed with their fundoplication. Of the 38 patients who underwent concurrent gastrostomy, 28 (73.7 %) were back on ARM at 6-month follow-up (p = 0.003). Concurrent pyloroplasty did not significantly affect recommencement of ARM. Neither procedure was related to redo fundoplication. Having a pyloroplasty significantly increased the risk of post-procedure dumping syndrome (p = 0.02).
Post-fundoplication complications
50 children (42.2 %) had complications post-fundoplication: gagging or retching not present prior to fundoplication (39, 32.8 %), dumping syndrome (5, 4.2 %), gas bloat (7, 5.9 %) and dysphagia (5, 4.2 %). 15 (30 %) children with complications post-fundoplication had surgery at less than 1 year of age, and 18 (36 %) also had an associated comorbid condition. Children with a comorbidity and/or <1 year did not have a significantly higher complication rate. Having an abnormal gastric emptying study did not correlate with increased risk of post-procedure gagging/retching or gas bloat.
Hospitalisations
In the 12 months prior to fundoplication, the total number of hospitalisations across the 119 patients in this study was 222. In the 12 months post-operatively, there were 168 hospitalisations. The mean total number of hospitalisations per patient was 4.4 (SD 3.8), with a reduction of 1.9 (SD 2.4) admissions per patient pre-operatively to 1.5 (SD 1.9) post-operatively (p = 0.05). In children with neurological impairment (69), the mean number of hospitalisations per patient was 3.6 (SD 3.0), with a 27.5 % reduction (p = 0.17) in hospitalisations post-fundoplication (40–29).
Table 2 contains the complete table of descriptive statistics.
Discussion
The NASPGHAN/ESPGHAN guidelines [7] for evaluation and treatment of paediatric gastroesophageal reflux disease state that fundoplication usually eliminates reflux [8] and is indicated in children with confirmed GORD who have failed optimal medical therapy, who are dependent on medical therapy over a prolonged period of time, who are significantly non-adherent with medical therapy, or who have life threatening complications of GORD. Although the guidelines list prolonged dependence on medical therapy as one of the indications for fundoplication in children, in the paediatric literature, there have not been many studies looking at outcomes post-fundoplication in the short- and long-term especially with special reference to the need for restarting anti-reflux medication and need for redo surgery and the pre-operative predictive factors influencing the post-operative outcomes.
At 6-month follow-up in our study, 21 (17.6 %) of children required a redo fundoplication and 64 (53.8 %) were back on anti-reflux medications. 62 (52 %) were symptom free. Gilger et al. [9] conducted a retrospective review of 198 children (78 % of whom had comorbidities) who underwent fundoplication over a 3-year period in Houston Texas and found that at 2-month follow-up post-surgery 63 % of children had received evaluation and treatment for symptoms suggestive of recurrent reflux despite fundoplication. Other paediatric studies have showed varying rates for the outcomes examined in our study (Table 3). Our study is the first of this type in Australia. Our redo rate was higher than Esposito [10], Mattioli [11] and Diaz [12] over a shorter period of time. This could be because we had a larger number of children with comorbidities in our cohort, compared to their study populations (excluding Diaz). The recommencement rate of ARM in our study was again higher in our study compared to Esposito, but was lower than that in Lee et al’s study [13], which also had a significant proportion of NI patients in their cohort.
None of the children who had open fundoplication in our study required redo, but the sample size was small (9 of 119). Larger studies are needed to substantiate this finding. Other studies in the literature comparing open to laparoscopic fundoplication have focused on the peri-operative period, but not need for redo fundoplication or recommencement of ARM [14, 15].
In the adult literature, there are four large RCTs (Anvari 2006, LOTUS 2008, Mahon 2005 and REFLUX 2008) comparing medical to surgical management of GORD, reviewed in Wileman et al.’s [16] 2010 Cochrane review. The reoperation rate at 12-month follow-up across these papers was low—0 to 3.7 %. Victorzon et al. [17] assessed the symptomatic outcome of fundoplication in 135 adults in Scandinavia by questionnaire at a mean follow-up of 25 months (range 6–82) and found 87 % were free of reflux symptoms, and 84 % were without any medication. Grant et al. [18] randomised 810 adult patients to medical or surgical management of GORD in the REFLUX trial, by 12 months after surgery 14 % in the surgical group were taking ARM. We feel it is important to consider the higher incidence of need for restarting anti-reflux medication and need for redo surgery in the paediatric data when comparing to the adult data, when making decisions on need for fundoplication in children with GORD.
Anti-reflux surgery has been shown to highly benefit neurologically impaired children, mainly due to the improvement in nutrition and respiratory problems [19]. However, other studies have suggested significant failure rates post-fundoplication in this patient base, with one study [20, 21] finding more than twice the complication rate, 3 times the morbidity rate and 4 times the anti-reflux surgery reoperation rate in children with NI, within a mean follow-up of only 1.6 years. Better results of GORD control in children with NI have been recorded with jejunal or gastrostomy feeds and concurrent PPI treatment [17]. Martinez et al. [22] reviewed the cases of 198 children with NI and found a 25 % redo rate, and return of symptoms in 71 %. Martinez concluded that recognition of recurrent GER after anti-reflux surgery in children with NI required a high index of suspicion, with repeated testing over time, and use of more than one test. The largest combined hospital study of 7467 paediatric patients by Fonkalsrud et al. [23] showed need for redo fundoplication in 3.6 % of neurologically normal (NN) children and 11.8 % of children with NI. Rothenberg et al. [24] in his study of 1048 children who had laparoscopic fundoplication showed a reflux recurrence rate of 4 % overall and 6 % in the NI group, and 6 % in those under the age of 1 year. Spillane et al. [25] did a retrospective review of 103 patients at our institution looking at outcomes of fundoplication found a failure rate of 7.5 % and a long-term mortality rate of 7.8 %; the group most at risk of mortality and morbidity was the neurologically impaired. Our redo rate in this study was higher at 17.6 % compared to Fonkalsrud’s study but lower than that in Martinez’s study. Interestingly, we did not show a significantly higher need for redo fundoplication in the NI population unlike Martinez [22]. However, our similar rate of redo in normal and NI patients was similar to Rothenberg’s results. In our study, there were no comorbidities (including NI, OA/TOF or CF) which were associated with a poor outcome. Our result is similar to that of Strecker-McGraw et al. [19] who also found that in their cohort there was no significantly increased probability of immediate post-operative failure in patients with NI, OA/TOF or gastric emptying abnormalities. Given the higher incidence of complicated GORD in the population with associated comorbidities like NI, OA/TOF and CF we feel that this is important new information to consider when making decision regarding the need for fundoplication in this population.
Leung et al. [26] compared the outcomes of laparoscopic fundoplication in 86 infants under 12 months of age and children over 12 months of age. They did not find a difference in outcomes or complication rates; nor did our study. Our study cohort was larger than Leung’s. Esposito et al. [27] reviewed the cases of 36 infants under the age of 12 months who underwent fundoplication, with a redo rate of 11.1 % and recommencement of ARM in only 1 (2.8 %) baby. Kubiak et al. [28] found a fundoplication redo rate of 24 % in a cohort of 66 infants babies less than 4 months of age. Both Leung and Kubiak did not look at recommencement of ARM in their cohorts. Our redo rate of 13 % was slightly higher than Esposito’s but lower than Kubiak’s. The main difference was the significantly higher percentage (65 %) of infants who were recommenced on anti-reflux medication in our study compared to Esposito. Esposito’s cohort had half the number of neurologically impaired infants than our study (8.3 vs 16.8 %) but more infants with OA (14 vs 5.9 %). Given the varying results of outcomes post-fundoplication in infancy in these studies it is important to take these factors into consideration whilst making a decision on need for anti-reflux surgery in young infants.
Respiratory symptoms established to have been caused by GORD are often the main indicators for fundoplication, with studies finding 92 % of children had improved respiratory symptoms after surgery, when they had previously failed medical therapy [6]. Although there was no significant difference in outcomes post-fundoplication when comparing GI to respiratory symptomatology as the pre-operative indication for surgery, nocturnal cough was the only respiratory symptom which was predictive of redo fundoplication in our study. However, as nocturnal cough can be due to not only GOR but also potentially asthma or sinusitis with post-nasal drip, and none of the patients in this study with nocturnal cough had impedance pH testing to confirm symptom association between nocturnal cough and reflux episodes, it is difficult to categorically state whether the nocturnal cough was secondary to reflux recurrence post-fundoplication. Although coughing might put pressure on the fundal wrap and lead to reflux recurrence, our finding that nocturnal cough as a potential risk factor for fundoplication failure needs to be corroborated with larger prospective studies where reflux recurrence post-fundoplication is documented not only based on symptomatology but also with objective measures including pH-impedance testing.
Niebisch and Peters [29] said in 2012 that pre-operative investigations are advantageous to post-operative outcomes as they highlight any underlying anatomic and physiologic abnormalities and reconfirm a diagnosis of GORD, which aids in assuring a high probability of symptomatic relief post-surgery. Anvari et al. [30] demonstrated a link between abnormal pH result and good outcome post-fundoplication in adults; however, they looked at reflux control and symptom resolution, not need to restart ARM or need for reoperation. Broeders et al. [31] found high supine acid exposure as an independent predictor of surgical re-intervention (p = 0.006) in adults. Although in our study outcomes of pre-operative investigations were not useful in prognostication of outcome, our study was limited by low numbers of pre-operative investigations actually performed. An ideal prospective cohort study would involve pre-operative investigations (endoscopy and pH/impedance testing) performed on all patients.
The definition of failure with reflux recurrence post-fundoplication varies between studies looking at outcomes of fundoplication. It has been based on patient satisfaction levels, quality of Life (QOL) scores, results of investigations (barium meal, pH/impedance testing, endoscopy) and reoperation rates. Gilger [9], Lee [13] and Lord’s [32] studies relied on need to recommence ARM, as did our study. Other studies which have used a more objective measure of reflux recurrence post-fundoplication have shown that relying on symptoms alone or ARM usage is unreliable and overestimates reflux recurrence as ARMs might have been recommenced to treat dyspeptic symptoms. Strecker-McGraw et al. [19] did a retrospective review of 385 children who underwent fundoplication and then had extended oesophageal pH study within the first 12 post-operative weeks. Strecker-McGraw found that only 5 (36 %) of the 14 children with persisting symptoms suggestive of GERD had actually had immediate post-operative failure of their operation. Lord et al. [32] did a similar study of 86 adult patients who had symptoms following Nissen fundoplication that were sufficient to merit evaluation with 24-h distal oesophageal pH monitoring. 37 patients (43 %) in Lord’s study were taking acid suppression medications after fundoplication, but only 24 % (9 of 37) of those taking acid suppression medications had abnormal oesophageal acid exposure on the 24-h pH study. In adults, Broeders et al. [33] showed that of 26.4 % of patients were on ARM at 10 years post-fundoplication, only 35 % of those on ARM had abnormal pH-impedance results. Hence we should not rely on symptoms alone when diagnosing reflux recurrence post-fundoplication before recommencing ARM or deciding on need for a redo fundoplication. A more objective measure of recurrent reflux post-fundoplication could also have potentially had an effect on pre-operative prognostic factors and outcomes (need for restarting ARM and need for redo surgery) post-fundoplication. At the same time, under reporting of symptoms could also have resulted in lack of significance as only if the patient came to see the doctor as part of scheduled follow-up and told him about the symptom/complication would it have been recorded. This shortcoming could be avoided by large prospective studies with scheduled follow-up included and a standardised reflux symptom questionnaire in addition to objectively documenting reflux recurrence with pH-impedance and endoscopy in symptomatic post-fundoplication.
In our study, concurrent gastrostomy insertion was a significant predictor of ARM recommencement post-fundoplication. It is possible that the children who needed a concurrent gastrostomy with the fundoplication had more severe reflux. This needs to be corroborated with larger prospective studies.
As the majority (53.8 %) of children in this study needed to restart their anti-reflux medications within 6 months of surgery, parents should be aware that fundoplication is unlikely to allow their child to remain off anti-reflux medications in the long term. We therefore feel fundoplication should be reserved for patients with poorly controlled reflux as documented by oesophagitis on biopsy/abnormal acid reflux index or symptom association on treatment as shown in pH/impedance testing, recurrent chest infections/ALTE which have been proven to be secondary to GORD, and not routinely performed on patients to get them off long-term ARM. In addition, we feel it is also important to ensure that patients were on therapeutic doses before they were labelled as ‘failing medical therapy’. If the decision to proceed with fundoplication is made, parents need to be aware that there is a 50 % chance that their child will be back on ARM at 6 months. This is very different to the adult data where only 14 % of patients undergoing fundoplication were back on ARM at follow-up [16].
The main limitations of this study are the fact that it was a retrospective study where our data were limited by clinician’s documentation. Outcomes post-fundoplication were based on ARM recommencement and redo fundoplication at 6-month post-fundoplication. However, not all the patients had reflux recurrence objectively measured with contrast studies, pH-impedance testing and endoscopy before ARM were recommenced or a decision was made to proceed with a redo fundoplication. This needs to be addressed in future studies looking at outcomes post-fundoplication. Another limitation of our study was that post-operative complication data was only based on development of chronic new symptoms post-fundoplication. It would be important to also record data on acute post-operative complications after fundoplication including wound infection, wound dehiscence, bleeding, splenic laceration, perforation (oesophageal, gastric, pericardial and pleural), vagal injury, atelectasis or pneumonia and protracted ileus. The data presented in this study are from a single centre and consequently the outcomes described are limited to that seen at our hospital, and generalizability is limited.
The findings in this study are significant as there are no previous similar Australian studies looking at outcomes of fundoplication in children. This monocentric study is also important given the relatively large number of patients (119). We attempted to minimise selection bias in our study by including all patients in whom fundoplication was performed during a defined time period. This is also one of the few paediatric studies to look at outcomes post-fundoplication with respect to need to restart anti-reflux medications and need for redo surgery and incidence of complications. This is also the only paediatric study to look at effect of fundoplication on need for hospitalisation post-surgery. Although our hospitalisation data was based on primary diagnosis only, and hence is potentially confounded by patients with multiple reasons for admission and hospital coding processes. Future work in this area is important from a health economics point of view. It would also be important in future studies to assess improvement in quality of life of the patient and family post-fundoplication, and we are planning on assessing this in a future prospective study.
Overall, this study revealed that a significant proportion of children need either a redo fundoplication or go back on anti-reflux medications by 6-month post-fundoplication. This finding is similar to previous paediatric data, but worse than outcomes in the adult literature. It is important therefore that paediatric practice and decision making in GORD not be influenced by adult outcomes and that parents be made aware of this when being counselled about management options for severe GORD. Our study also showed that the outcomes of fundoplication in young children under the age of one and in children with significant comorbidities including those with neurological impairment were not significantly worse when compared to older children and or children without comorbidities. Hence where indicated for severe GORD fundoplication should still be considered in these patient groups. Future prospective studies are needed to continue looking at outcomes of paediatric fundoplication for GORD and to optimise patient selection.
References
NICE Guideline (2014) Gastro-oesophageal reflux disease in children and young people DRAFT NICE guideline. www.nice.org.uk. Accessed June 2015
Di Lorenzo C, Orenstein S (2002) Fundoplication: friend or foe? J Pediatr Gastroenterol Nutr 34(2):117–124
Katz P, Gerson L, Vela M (2013) Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol 108(3):308–328
Blanco F, Davenport K, Kane T (2012) Pediatric gastroesophageal reflux disease. Surg Clin N Am 92(3):541–558
Carroll M, Jacobson K (2012) Gastroesophageal reflux disease in children and adolescents. Pediatric Drugs 14(2):79–89
Norrashidah A, Henry R (2002) Fundoplication in children with gastro-oesophageal reflux disease. J Paediatr Child Health 38(2):156–159
NASPGHAN, ESPGHAN Guideline (2009) Pediatric gastroesophageal reflux clinical practice guideline. J Paediatric Gastroenterol Nutr 49(4):498–547
Berquist W, Fonkalsrud E, Ament M (1981) Effectiveness of Nissen fundoplication for gastroesophageal reflux in children as measured by 24-hour intraesophageal pH monitoring. J Paediatric Surg 16:872–875
Gilger M, Yeh C, Chiang J, Dietrich C, Brandt M, El-Serag H (2004) Outcomes of surgical fundoplication in children. Clin Gastroenterol Hepatol 2(11):978–984
Esposito C, Montupet P, van Der Zee D, Settimi A, Paye-Jaouen A, Centonze A, Bax NK (2006) Long-term outcome of laparoscopic Nissen, Toupet, and Thal antireflux procedures for neurologically normal children with gastroesophageal reflux disease. Surg Endosc 20(6):855–858
Mattioli G, Esposito C, Lima M, Garzi A, Montinaro L, Cobellis G, Mastoianni L, Aceti MG, Falchetti D, Repetto P, Pini Prato A, Leggio S, Torri F, Ruggeri G, Settimi A, Messina M, Martino A, Amici G, Riccipetitoni G, Jasonni V (2002) Italian multicenter survey on laparoscopic treatment of gastro-esophageal reflux disease in children. Surg Endosc 16(12):1666–1668
Diaz D, Gibbons T, Heiss K, Wulkan M, Ricketts R, Gold B (2005) Antireflux surgery outcomes in pediatric gastroesophageal reflux disease. Am J Gastroenterol 100(8):1844–1852
Lee S, Sydorak R, Chiu V, Hsu J, Applebaum H, Haigh P (2008) Long-term antireflux medication use following pediatric Nissen fundoplication. Arch Surg 143(9):873–876
McHoney M, Wade A, Eaton S, Howard R, Kiely E, Drake D, Curry J, Pierro A (2011) Clinical outcome of a randomized controlled blinded trial of open versus laparoscopic Nissen fundoplication in infants and children. Ann Surg 254(2):209–216
Papandria D, Goldstein S, Salazar J, Cox J, McIltrot K, Stewart F, Arnold M, Abdullah F, Colombani P (2014) A randomized trial of laparoscopic versus open Nissen fundoplication in children under two years of age. J Pediatr Surg 50(2):267–271
Wileman S, McCann S, Grant A, Krukowski Z, Bruce J (2010) Medical versus surgical management for gasto-oesophageal reflux disease (GORD) in adults (Review). Cochrane Database Syst Rev 3:CD003243
Victorzon M, Tolonen P (2003) Symptomatic outcome of laparoscopic fundoplication, using a minimal dissection technique. Scand J Surg 92(2):138–143
Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, Macran S, Kilonzo M, Vale L, Francis J, Mowat A, Krukowski Z, Heading R, Thursz M, Russell I, Campbell M (2008) The effectiveness and cost-effectiveness of minimal access surgery amongst people with gastro-oesophageal reflux disease—a UK collaborative study. The REFLUX trial. Health Technol Assess 12(31):1–181
Strecker-McGraw M, Lorenz M, Hendrickson M, Jolley S, Tunell W (1998) Persistent gastroesophageal reflux disease after antireflux surgery in children: I. Immediate postoperative evaluation using extended esophageal pH monitoring. J Pediatr Surg 33(11):1623–1627
Hassall E (2005) Decisions in diagnosing and managing chronic gastooesosphageal reflux disease in children. J Paediatr 146:S3–S12
Pearl R, Robie D, Ein S, Shandling B, Wesson D, Superina R et al (1990) Complications of gastroesophageal antireflux surgery in neurologically impaired versus neurologically normal children. J Pediatr Surg 25:1169–1173
Martinez D, Ginn-Pease M, Caniano D (1992) Sequelae of antireflux surgery in profoundly disabled children. J Pediatr Surg 27(2):267–271
Fonkalsrud E, Ashcraft K, Coran A, Ellis D, Grosfeld J, Tunell W, Weber T (1998) Surgical treatment of gastroesophageal reflux in children: a combined hospital study of 7467 patients. Paediatrics 101(3 Pt 1):419–422
Rothenberg S (2005) The first decade’s experience with laparoscopic Nissen fundoplication in infants and children. J Paediatr Surg 40(1):142–146 (discussion 147)
Spillane A, Currie B, Shi E (1996) Fundoplication in children: experience with 106 cases. Aust N Z J Surg 66(11):753–756
Leung L, Wong C, Chung P, Wong K, Tam P (2015) Laparoscopic Nissen fundoplication for gastro-oesophageal reflux disease in infants. Pediatr Surg Int 31(1):83–88
Esposito C, Montupet P, Reinberg O (2001) Laparoscopic surgery for gastroesophageal reflux disease during the first year of life. J Pediatr Surg 36(5):715–717
Kubiak R, Spitz L, Kiely E, Drake D, Pierro A (1999) Effectiveness of fundoplication in early infancy. J Pediatr Surg 34(2):295–299
Niebisch S, Peters J (2012) Update on fundoplication for the treatment of GERD. Curr Gastroenterol Rep 14(3):189–196
Anvari M, Allen C, Marshall J, Armstrong D, Goeree R, Ungar W, Goldsmith C (2006) A randomized controlled trial of laparoscopic nissen fundoplication versus proton pump inhibitors for treatment of patients with chronic gastroesophageal reflux disease: one-year follow-up. Surg Innov 13(4):238–249
Broeders J, Roks D, Draaisma W, Vlek A, Hazebroek E, Broeders I, Smout A (2011) Predictors of objectively identified recurrent reflux after primary Nissen fundoplication. Br J Surg 98(5):673–679
Lord R, Kaminski A, Oberg S, Bowrey D, Hagen J, DeMeester S, Sillin L, Peters J, Crookes P, DeMeester T (2002) Absence of gastroesophageal reflux disease in a majority of patients taking acid suppression medications after Nissen fundoplication. J Gastrointest Surg 6(1):3–9
Broeders J, Rijnhart-de Jong H, Draaisma W, Bredenoord A, Smout A, Gooszen H (2009) Ten-year outcome of laparoscopic and conventional nissen fundoplication: randomized clinical trial. Ann Surg 250(5):698–706
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Pascoe, E., Falvey, T., Jiwane, A. et al. Outcomes of fundoplication for paediatric gastroesophageal reflux disease. Pediatr Surg Int 32, 353–361 (2016). https://doi.org/10.1007/s00383-015-3843-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-015-3843-4