Abstract
From January 1994 to December 2004, 118 patients with recurrent gastroesophageal reflux disease (GERD) after fundoplication underwent laparoscopic redo Nissen fundoplication. The patients ranged in age from 6 months to 19 years (mean, 7 years), and weighed from 6.4 to 85 kg. Of the 118 patients, 64 had previous open fundoplications, 53 had previous laparoscopic fundoplications, and 19 had more than one previous fundoplication. All the procedures had been successfully completed laparoscopically. The average operative time was 100 min. The intraoperative complication rate was 1.1%. The average time to full feeding was 1.8 days, and the average hospital stay was 2.2 days. The postoperative complication rate was 3.6%. The wrap failure rate during an average follow-up period of 48 months was 6%. Laparoscopic redo Nissen fundoplication for a failed antireflux procedure is a safe and effective procedure. It has the same benefits as a primary laparoscopic Nissen for GERD, with low morbidity and a quicker recovery. Early follow-up evaluation suggests that the long-term outcome is superior to that associated with open redo fundoplication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Esophagogastric fundoplication is one of the most common procedures currently performed by pediatrics surgeons [5, 7, 14]. A recent report of more than 7,000 cases from seven major U.S. institutions concluded that fundoplication is a safe and effective procedure for the pediatric population [4]. Indications for antireflux procedures in this group include respiratory compromise, neurologic impairment, failure to thrive, and esophagitis and stricture formation.
Before the 1990s, fundoplications were routinely performed through a relatively large upper abdominal incision and required an extensive hospital stay and recovery period. These procedures were associated with a relatively high complication rate, especially postoperative pulmonary problems. Since the early 1990s, an increasing number of these operations have been performed laparoscopically. A number of reports in the adult and pediatric surgical literature have shown that laparoscopic fundoplications can be performed safely with lower morbidity, shorter hospital stays, and better recurrence rates during a 5 year follow-up period than achieved with traditional open surgery [1, 6, 8, 11, 15]. However both the open and laparoscopic procedures are associated with a recurrence rate of 3% to 40%.
Although significant data appear to support a preferential use of the laparoscopic approach for primary fundoplication, no study to date has evaluated a large series of redo fundoplications among children approached laparoscopically. This report describes a 10-year series of laparoscopic redo fundoplications by a single surgeon in an attempt to evaluate the safety and efficacy of this approach.
Methods
From January 1994 to December 2005, more than 1,100 patients underwent laparoscopic surgery for severe gastroesophageal reflux disease (GERD). Of these patients, 118 underwent redo laparoscopic Nissen fundoplication after a failed previous surgical fundoplication. The patients ranged in age from 6 months to 19 years (mean, 7 years) and in weight from 6.4 to 85 kg. Of the 118 patients, 65 had undergone previous open fundoplications including 52 Nissens, 12 Thals, and 1 Toupet, and 53 had undergone previous laparoscopic fundoplications including 50 Nissens, 2 Thals, and 1 Toupet. Moreover, 19 patients had undergone more than one previous fundoplication. All the patients had symptoms of GERD (78%), dysphagia (10%), food intolerance (24%), or worsening respiratory status (14%). The preoperative workup included upper gastrointestinal radiographs for all, upper endoscopy for 48 patients, and pH probe for 23 patients. Hiatal hernia was diagnosed preoperatively in 68% of the patients.
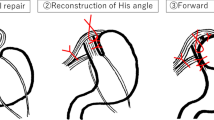
Technique
All patients referred for redo fundoplication since 1994 were approached laparoscopically. No patient was excluded. The patients were positioned in a modified dorsal lithotomy position with the surgeon positioned at the foot of the table between the patients’ legs. Four or five ports were used depending on the need for liver retraction. In many of the patients with previous open procedures, the left lobe of the liver was adherent to the anterior abdominal wall, providing adequate exposure to the hiatus without retraction. Port placement was the same as for primary cases except when a G-tube was in place requiring modification of the left-sided ports.
The procedures comprised lysis of adhesions, complete mobilization of the stomach, and takedown of the previous fundoplication. If the upper short gastric vessels had not been removed in the previous fundoplication, they were divided at this time to allow a tension-free wrap. An adequate length of intraabdominal esophagus then was reestablished, and the hiatal defect was closed. In patients with recurrent hiatal hernias, pledgeted mattress sutures were used for the crural closure. In selected cases, a diaphragmatic patch was used to relieve tension on a giant defect. A full 360° wrap then was formed with three stitches of 2-0 braided suture. The wrap was formed around an appropriate-sized bougie. Ten patients with delayed gastric emptying also underwent a formal pyloroplasty.
If the adhesions were not extensive, no nasogastric (NG) tube was left, and liquids were started in 4 to 6 h. If more dissection and mobilization were required, the NG tube was left in place overnight and removed when volumes were considered minimal. Patients were discharged when they tolerated adequate nutrition by mouth and were comfortable on oral pain medications. All the patients were followed up at 2 weeks, and then at 3 months. Upper gastrointestinal radiographs were obtained if the patients had any complaints or symptoms of recurrent reflux. All families were told to contact us immediately if any symptoms recurred.
Results
All the procedures were successfully completed laparoscopically. The operative times ranged from 35 to 195 min (mean, 100 min). The intraoperative complication rate was 1%. Four patients had enterotomies during an extensive lysis of adhesions, and all were repaired laparoscopically. The average time to full feeding was 1.8 days, and the average hospital stay was 2.2 days. The postoperative complication rate was 3.6%. There were two delayed perforations at 48 h requiring laparoscopic reexploration and gastroraphy. One patient experienced severe gagging and retching in the immediate postoperative period and an incarcerated paraesophageal hernia, which was reduced and repaired on postoperative day 4. The dysphagia rate postoperatively was 3.8%, and one patient required a single dilation 3 weeks after surgery. Ten patients with wrap breakdowns also underwent formal pyloroplasty for delayed gastric emptying, and at this writing, one recurrence has been diagnosed in this group.
The secondary wrap failure rate was 6% during an average follow-up period of 48 months. At this writing, three patients have undergone revision laparoscopically. One had an open revision by another surgeon; one is being managed medically; and one is lost to follow-up evaluation.
Discussion
Laparoscopic fundoplication has become the mainstay for the management severe GERD in both the adult and pediatric populations. A recent review of our experience during the first decade shows a low complication rate and a recurrence rate lower than 4% [12]. Both of these rates are significantly lower than the majority of reports for the open procedure.
As experience and techniques have evolved, advanced laparoscopic approaches to more difficult and complex gastric procedures have been undertaken. This includes procedures such as a Collis–Nissen for short esophagus, revision of failed fundoplications (laparoscopic or open), and repair of giant or recurrent hiatal hernias. Reports by Hunter, Anvari, Rosemurgy [10] and others [3, 9] have demonstrated that these procedures can be undertaken safely with success rates of up to 95%. There also are a few small series in the pediatric population, including those by Tan and Wulkan [13] and Espisito et al. [2], that show favorable results, as compared with open redo fundoplication. It is clear in all these studies that this group of patients receives the same benefits of quicker recovery and lower morbidity from a laparoscopic approach as those undergoing a primary fundoplication.
This report describes the largest single series of redo laparoscopic fundoplications for children in the literature to date. All the patients presented with a recurrence of their symptoms that failed conservative medical management. Many had the dysphagia and food intolerance common to patients with a hiatal hernia. Some had a worsening of their respiratory symptoms, and some had increasingly severe epigastric and abdominal pain. In each case, the symptoms were felt to be so severe that medical management was not an option. Some of the neurologically impaired patients with G-tubes and food intolerance were offered a gastrojejunostomy tube, but because of the high dislodgement rate, most of the parents requested a revision of the Nissen after a short period.
The majority of the patients (55%) had undergone a previous open fundoplication, and 30% had undergone a laparoscopic Nissen by the author. Of these failures, 29 had occurred within the first 16 months after surgery, suggesting a technical error. Moderate to large hiatal hernias had developed in 24 of these patients, with the remainder experiencing partial wrap disruption. The long-term success rate appeared to exceed 94%, and the complication rate was less than 4%. Both rates are superior to that reported for open redo fundoplication.
The most serious complications were experienced by three patients. Two of the patients experienced delayed perforations requiring reexploration, and an incarcerated paraesophageal hernia developed in a third patient after 48 h of postoperative gagging and retching. The two patients with the perforations both had undergone multiple previous procedures. Both had extensive scar tissue and hiatal hernias, and one was receiving steroids. It is likely that the stomach tissue had been partially devitalized during the previous operations, resulting in weak areas more susceptible to injury.
Delayed gastric emptying was seen on the nuclear medicine scans of 10 patients with wrap breakdowns. This group also underwent a formal pyloroplasty at the time of their revision, and there were no operative complications from this procedure, although four patients had mild dumping syndrome postoperatively. There has been one diagnosed recurrence in this group. However, it should be noted that most of the patients did not require a pyloroplsty, indicating that the potential for dumping syndrome can be avoided.
Laparoscopic revision of a failed fundoplication procedure is a technically demanding procedure, but it can be performed safely and effectively by a surgeon with advanced endoscopic skills. In general, patients who have undergone a previous open procedure present as more difficult cases because of more extensive adhesions. The majority of patients will have some form of hiatal hernia, and the key to a redo procedure is extensive mobilization of the stomach and esophagus with a tension-free hiatal and wrap repair. This technique has proved to be safe and effective, and appears to yield superior results with significantly less morbidity in this difficult group of patients.
References
Collins JB, Georgeson KE, Vicente Y, Hardin WD (1995) Comparison of open and laparoscopic gastrostomy and fundoplication in 120 patients. J Pediatr Surg 30: 1065–1071
Espisito C, Becmur F, Centon A (2003) Laparoscopic reoperation following unsuccessful antireflux surgery in childhood. Semin Laparosc Surg 9: 177–179
Floch NR, Hinder RA, Klinger PJ, Branton SA, Seelig MH, Banner T, Filipi CJ (1999) Is laparoscopic surgery for failed antireflux surgery feasible? Arch Surg 134: 733–737
Fonkalsrud EW, Ashcraft KW, Coran AG, Ellis DG, Grosfeld JL, Tunnell WP, Weber TR (1998) Surgical treatment of gastroesophageal reflux in children: a combined hospital study of 7,467 patients. Pediatrics 101: 419–422
Fonkalsrud EW, Berquist W, Vargas J, et al. (1987) Surgical treatment of gastroesophageal reflux syndrome in infants and children. Am J Surg 154: 11–18
Hinder RA, Filipi CJ, Wetscher G, Neary P, DeMeester TR, Perdikis G (1994) Laparoscopic Nissen fundoplication is an effective treatment for gastroesophageal reflux disease. Ann Surg 220: 472–481
Jolley SG, Ide Smith E, Tunnel WP (1987) Protective antireflux operation with feeding gastrostomy: experience in children. Ann Surg 201: 736–739
Longis B, Grousseau D, Alain JL, Terrier G (1996) Laparoscopic fundoplication in children: our first 30 cases. J Laparoendosc Surg 6(Suppl 1): s21–s29
Papasavas PK, Yeaney WW, Landreneau RJ (2004) Reoperative laparoscopic fundoplication for the treatment of failed fundoplication. J Thorac Cardiovasc Surg 128: 509–516
Rosemurgy AS, Arnaoutakis DJ, Thometz DP, Biaitic O, Giarelli NB, Bloomston M, Goldin SG, Albrink MH (2004) Reoperation fundoplications are effective treatment for dysphagia and recurrent gastroesophageal reflux. Am Surg 70: 1061–1087
Rothenberg SS (1997) Experience with laparoscopic Nissen fundoplication in infants and children less than 10 kg. Presented at the Society of American Gastrointestinal Endoscopic Surgeons, San Diego, CA, March 1997
Rothenberg SS (2004) First decades experience with laparoscopic fundoplication in infants and children. J Pediatr Surg 40: 142–147
Tan S, Wulkan ML (2002) Minimally invasive surgical techniques in reoperative surgery for gastroesophageal reflux disease in infants and children. Am Surg 68: 989–992
Turnage RH, Oldham KT, Coran AG, Blane LE (1989) Late results of fundoplication for gastroesphageal reflux in infants and children. Surgery 105: 457–463
Weerts JM, Dallemagne B, Hamoir E, Demarche M, Markiwicz S, Jehaes C, Lombard R, Demoulu JL, Etienne M, Ferron PE (1993) Laparoscopic Nissen fundoplication: detailed analysis of 132 patients. Surg Laparosc Endosc 3: 359–364
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rothenberg, S.S. Laparoscopic redo Nissen fundoplication in infants and children. Surg Endosc 20, 1518–1520 (2006). https://doi.org/10.1007/s00464-005-0123-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0123-8