Abstract
Background
Intracranial interdural cyst is a rare lesion. The exact pathophysiology of these cysts remains unknown.
Clinical presentation
We report an infant with interdural cyst of the tentorium cerebelli. Although the cyst mimicked an arachnoid cyst on pre- and postnatal magnetic resonance images, lateral suboccipital craniotomy revealed the cyst within the tentorium. Fenestration on the infratentorial side was performed with successful results. Histologically, the inner surface of the cyst was lined with arachnoid cells.
Conclusion
We report detailed neuroradiological, intraoperative, and histological findings, and discuss the pathophysiology of the cyst in this case.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intracranial interdural cyst is a rare lesion located within the dura mater, with only five reported cases [1,2,3,4,5]. The clinical manifestations of these cases are highly variable (Table 1), and the exact pathophysiology of intradural cysts remains unknown [2]. Three reported cases were patients with huge cysts surrounded by dura mater, two in the falcotentorium [1, 2] and one in the interhemispheric region [5]. Two cases were small cysts, one located in the superior sagittal sinus [4], and one at the foramen magnum [3]. It is hard to make a correct preoperative diagnosis of interdural cyst, even with magnetic resonance imaging (MRI) [2, 3]. We surgically treated an infant with interdural cyst of the tentorium cerebelli. On pre- and postnatal MRI, the cyst mimicked an arachnoid cyst of the posterior fossa extending to the middle fossa through the tentorial defect. We report detailed neuroradiological, intraoperative, and histological findings, and discuss the pathophysiology of the cyst.
Case report
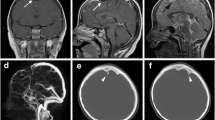
A primigravida woman with twin pregnancy was referred to us because transabdominal ultrasound examination at 30 weeks of gestation had demonstrated an intracranial cystic lesion in one of the fetuses. Prenatal MRI performed at 35 weeks revealed a cyst located in the right paracerebellar region (Fig. 1a).
(a) Prenatal magnetic resonance images (MRI) at 35 weeks of gestation. Axial view of half-Fourier acquisition single-shot turbo spin-echo image shows a cyst located in the right paracerebellar region. (b–d) Postnatal MRI at 4 days of age. Axial three-dimensional T1-weighted spoiled gradient-recalled echo (T1WI) image (b) and coronal T2-weighted image (T2WI) (c) show a cyst located at the tentorium and involving both the infra- and supratentorial regions to the same extent. The cyst demonstrates low intensity on T1WI and high intensity on T2WI. The mass effect on the adjacent cerebellum and temporal lobe is noted. On coronal gadolinium-enhanced T1WI (d) , the cyst wall and tentorium are enhanced in the same manner. (e, f) MRI on 12th day after surgery. Serial coronal T2WI (e-1, 2, 3) and T1WI (f-1, 2, 3) images reveal marked shrinkage of the cyst and decreased mass effect. The split between the dural layers is clearly demonstrated. The supratentorial side of the cyst has regained the original form of the tentorium. The opening on the infratentorial side of the cyst is delineated (e-2, f-2, white arrows). The most lateral wall of the interdural cyst is the inner wall of the transverse–sigmoid junction.
The boy was delivered by cesarean section at 35 weeks and 4 days of gestation because of twin pregnancy. He weighed 2028 g and was neurologically normal. Postnatal MRI performed on day 4 after birth demonstrated that the 20-mm cyst was located at the tentorium and involved both the infra- and supratentorial regions to the same extent (Fig. 1b,c). The cyst wall and tentorium were equally enhanced with gadolinium (Fig. 1d). Because the mass was affecting adjacent structures, cyst fenestration was indicated. Surgery was postponed until the infant reached 3 months of age and/or 5 kg, in accordance with our policy for untethering surgery for asymptomatic closed spinal dysraphism [6].
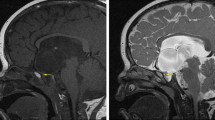
When the infant was 4 months of age and weighed 7.5 kg, right lateral suboccipital craniotomy was performed (Fig. 2a-1), after confirmation of unchanged cyst size and lack of involvement of the dural sinus on computed tomographic scan. A local bulging of the tentorium was observed in the infratentorial cistern (Fig. 2a-2, b-1). The bulge was punctured and xanthochromic fluid was aspirated. Cyst fenestration was performed (Fig. 2a-3, b-2). There was no dural defect. Because the cyst shrank, excision of the supratentorial wall was not performed.
(a) Schematic drawing and (b) microscopic view of operative findings. Right lateral suboccipital craniotomy (a-1). In the infratentorial cistern, a local bulging of the tentorium is observed, which compresses the tentorial surface of the cerebellum (a-2, b-1). The cyst wall is widely excised and cyst fenestration is performed (a-3, b-2). Through the opening, the opposite side of the inner wall is observed (b-2). (c–f) Histological findings of the cyst wall. (c) Most of the cyst wall is composed of fibrocollagenous tissue with some dilated thin-walled blood vessels, consistent with the dura. The inner cyst wall is lined with simple epithelium. (d) High-power images of the area indicated by the dotted square in (c) show that the epithelium consists of cuboidal or flattened epithelial cells. These epithelial cells are immunopositive for anti-cytokeratin (CAM 5.2) (e) and vimentin. (f). (g) Schematic drawing of pre- (g-1) and postoperative (g-2) anatomical relationships among the interdural cyst, tentorium cerebelli, cyst fenestration site, and transverse–sigmoid junction. (g-1) Interdural arachnoid cyst is located at the tentorium and involves both infra- and supratentorial regions to the same extent. The inner wall of the cyst is lined with arachnoid cells. (g-2) Postoperatively, the supratentorial side of the cyst has regained the original form of the tentorium. The opening on the infratentorial side of the cyst is seen. The most lateral wall of the interdural cyst is the inner wall of the transverse–sigmoid junction
The postoperative course was uneventful. Histologically, most of the cyst wall was composed of fibrocollagenous tissue with some dilated thin-walled blood vessels, consistent with the dura mater (Fig. 2c). The inner surface of the cyst wall was lined with simple epithelium consisting of cuboidal or flattened epithelial cells (Fig. 2c,d). These epithelial cells were immunopositive for anti-cytokeratins (CAM5.2 and AE1/AE3; Fig. 2e), vimentin (Fig. 2f) and S-100 protein, but negative for glial fibrillary acidic protein and epithelial membrane antigen. Periodic acid–Schiff and Alcian blue staining failed to reveal goblet cells. The immunohistochemical profile of the epithelial cells was not fully consistent with a specific cell type; however, it was close to that of arachnoid cells. Thus, the diagnosis of interdural arachnoid cyst was made (Fig. 2g-1).
MRI performed 12 days after surgery revealed marked shrinkage of the cyst and decreased mass effect (Fig. 1e-1, 2, 3, 1f-1, 2, 3). The split between the dural layers was clearly visible. The supratentorial side of the cyst had regained the original form of the tentorium. The opening on the infratentorial side was delineated (Fig. 1e-2, f-2). The most lateral wall of the interdural cyst was the inner wall of the transverse–sigmoid junction (Fig. 1e-1, f-1, Fig. 2g-2).
Discussion
Intracranial interdural cysts are generally thought to be of congenital origin [1, 2]. The present report describes the first documented case of interdural cyst demonstrated on both pre- and postnatal MRI, although the diagnosis at that time was arachnoid cyst.
Haymaker and Foster [1] first speculated that interdural cyst formation resulted from failure of union of the two dural layers, which occurs to enclose the venous sinus in the embryonic period, because autopsy revealed that the anterior cyst wall was formed of the dura, including the superior sagittal and transverse sinuses. Inagaki et al. [2] reported a similar case of interdural cyst at the falcotentorium. A cyst within the superior sagittal sinus has also been reported [4]. In our patient, postoperative MRI clearly revealed the split between the two dural layers. Furthermore, the most lateral wall of the interdural cyst was the inner wall of the transverse–sigmoid junction (Fig. 2g-2). These findings support the original hypothesis of Haymaker and Foster.
The most notable histological finding in our case was that the inner wall of the cyst was lined with arachnoid cells (Fig. 2g-1). It has been demonstrated that interdural cysts in the spinal canal may be caused by herniation of the arachnoid membrane through a defect in the inner layer of the dura [7, 8]. Cyst enlargement may result from the one-way valve mechanism at the neck of the cyst. In the present case, no dural defect was detected. However, a dural tear might have been too small to detect during surgery or may have spontaneously closed. The presence of xanthochromic fluid in the cyst suggests long-term isolation from the subarachnoid space. Remnant arachnoid membrane, which is normally subdivided from the same precursor as the dura but retained in the embryonic period [5, 9, 10], is another possible explanation for the presence of the arachnoid lining in the present case.
Although the optimal surgery for interdural cyst is uncertain, partial excision or fenestration of the cyst wall to create a communication with the subarachnoid space has been performed [2]. Because of the close anatomical relationship with the dural sinuses [1, 2, 5], total removal is thought to be risky and unnecessary. In the present case, we made a fenestration only on the infratentorial side of the cyst and a successful result was obtained, although further follow-up is needed.
References
Haymaker W, Foster ME (1944) Intracranial dura cysts. J Neurosurg 1:211–218
Inagaki T, Yamanouchi Y, Nishimura T, Kawamura Y, Kawamoto K (1998) Intracranial dural cyst. Childs Nerv Syst 14:69–73
Ohba S, Yoshida K, Sugiyama I, Ikeda E, Kawase T (2011) Dural cyst at the foramen magnum. Neurol Med Chir (Tokyo) 51:671–672
Ojemann JG, Moran CJ, Gokden M, Dacey RG Jr (1999) Sagittal sinus occlusion by intraluminal dural cysts. Report of two cases. J Neurosurg 91:867–870
Rao KC, Gunadi IK, Diaconis JN (1982) Interhemispheric intradural cyst. J Comput Assist Tomogr 6:1167–1171
Morioka T, Hashiguchi K, Yoshida F, Nagata S, Miyagi Y, Mihara F, Sasaki T (2007) Dynamic morphological changes in lumbosacral lipoma during the first months of life revealed by constructive interference in steady-state (CISS) MR imaging. Childs Nerv Syst 23:415–420
Done SL, Hayman LA, New PF, Davis KR, Chapman PH (1984) Interdural cyst of the lumbosacral region. Neurosurgery 14:287–294
Lee JH, Jung TG, Kim HS, Jang JS, Lee SH (2010) Symptomatic isolated lumbar interdural arachnoid cyst. Neurol Med Chir (Tokyo) 50:1035–1038
Mack J, Squier W, Eastman JT (2009) Anatomy and development of the meninges: implications for subdural collections and CSF circulation. Pediatr Radiol 39:200–210
O'Rahilly R, Muller F (1986) The meninges in human development. J Neuropathol Exp Neurol 45:588–608
Acknowledgments
We thank Drs. Nobuko Kawamura and Naoyuki Nakanami for supporting our study. We also thank Rebecca Tollefson, DVM, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Funding
This work was partly supported by the Research Foundation of Fukuoka Children’s Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent for the publication of the case report was obtained from the parents of the child.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Murakami, N., Morioka, T., Suzuki, S.O. et al. Congenital interdural arachnoid cyst of the tentorium cerebelli. Childs Nerv Syst 36, 1071–1074 (2020). https://doi.org/10.1007/s00381-019-04404-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04404-9