Abstract
Background
Embryonal tumor with multilayered rosettes (ETMR) is a very rare entity and has seldom been reported. It has been newly defined tumor entity included in the latest update (revised fourth edition) of WHO 2016 Classification of Tumors of the Central Nervous System which portends a uniform dismal prognosis and survival even with the best of multimodality approaches.
Illustrative case
This report documents the presentation of a 2-year-old girl with voluminous intracranial ETMR in the right parieto-occipital region. We describe clinical diagnosis, histological aspects, radiological features, and current management of this very aggressive tumor.
Conclusion
Pediatric intracranial ETMR is a highly aggressive neoplasm, and it should be considered in the differential diagnosis of pediatric brain tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Embryonal tumor with multilayered rosettes (ETMR), C19MC-altered is a very rare and a highly aggressive, malignant tumor which has been newly defined tumor entity included in the latest update (revised fourth edition) of WHO Classification of Tumors of the Central Nervous System [1].
Fewer than 100 cases of the entity have been described till now [2].
They are most commonly diagnosed in children below the age of 4 years.
Here, we present a case of brain ETMR in a 2-year-old girl. We discuss the clinical, radiological, and histopathological findings in this rare case and compare them with data in previously published cases in the literature.
Background
Historical background
ETMR was first described by Eberhart et al. in the year 2000 as a pediatric neuroblastic tumor with abundant neuropil and ependymoblastic rosettes [3]. ETMRs are highly malignant World Health Organization (WHO) grade IV [4].
It encompasses a group of three morphologically distinct embryonal tumors which were described as separate entities in the 2016 fourth edition of the WHO blue book [2] (Table 1). These include embryonal tumor with abundant neuropil and true rosettes (ETANTR), ependymoblastoma (EBL), and medulloepithelioma (MEPL).
Since this entity is known, specific molecular alterations have been identified, and authors showed amplifications at 19q13.42 using fluorescence in situ hybridization (FISH) analysis involving the C19MC; Korshunov et al. observed amplification at 19q13.42, at a high frequency of 93% the ETMRs [1, 5]. This hallmark cytogenetic feature suggested that both these tumors are a single biological entity originating from a common precursor cell [5, 6].
The basis for merging these hitherto separate tumor entities is a unique molecular signature, that is, C19MC locus amplification which is common to these entities [4].
LIN28A, a RNA binding protein, high expression is noted in ETMRs. LIN28A may directly bind mRNAs to increase production of cell cycle regulators and maintains pluripotency [7]. LIN28A increase cellular proliferation, angiogenesis, metastasis, cell death resistance, and genomic instability of cancer cells [7].
Many authors state that LIN28A is a highly specific and sensitive marker for ETMR and recommend immunohistochemical for LIN28A as a rapid and reliable tool for the routine diagnosis of these tumors, whereas there is a paucity of literature regarding immunoreactivity of LIN28A across all embryonal CNS tumors [7, 8].
Although the sex ratio may fluctuate slightly around 0.4 reported by Horwitz et al. and 0.6 reported by Picard et al. [9, 10].
Clinical presentation and imaging
Presentation varies according to involved structures. In the literature, the localization of the majority of the primitive tumor is supratentorial, the cerebellum and brain stem are affected in 30% of cases [1]. Horwitz et al. reported one patient with an ETMR localized to the spinal cord [9].
Most ETMR are radiologically misdiagnosed and/or mistaken for medulloblastoma, ependymoma, atypical teratoid/rhabdoid tumor, pilocytic astrocytoma, or pilomyxoid astrocytoma [10, 11].
On imaging, the tumors are usually a large heterogeneous solid mass at MR imaging with or without a cystic component, accompanied by relatively little edema or enhancement. These tumors restrict diffusion, indicating high cellularity [12]. Many ETMR are reported to have dural attachment as the present one [11].
Diagnosis
Histopathologically, the hallmark of embryonal tumors includes biphasic histology with the presence of multilayered true rosettes surrounded by primitive cells with high N/C ratio and abundant nuclear debris [1].
ETANTR were composed of a primitive cell component arranged in sheets and mature glial and/or neuronal component with easily appreciable background neuropil.
Scattered multilayered rosettes were also an integral component of this tumor type [13]. Ependymoblastoma (EBL) were composed of sheets of primitive cells, and frequent multilayered (ependymoblastic) rosettes and medulloepithelioma (MEPL) were composed of primitive cells arranged in papillae, tubules, and trabeculae with deposition of PAS-positive outer membrane at one of the surfaces, resembling primitive neural tube. Multilayered rosettes were also seen in these tumors [4, 13].
Immunohistochemically, the tumor cells are positive for vimentin, and the neuropil is positive for synaptophysin. MIB-1 labeling index will be very high as for all embryonal tumors [12].
Amplification of microRNA at chromosome 19q13.42 has emerged as the hallmark molecular signature for these tumors [13, 14].
Recent studies reiterate that LIN28A is a sensitive immunohistochemical marker for the diagnosis of ETMR. However, the authors also show that among CNS embryonal tumors, LIN28A is not specific to ETMRs and such immunoreactivity can also be seen in a proportion of AT/RTs. They observed that 100% of the ETMRs were LIN28A immunopositive compared to 12% of the AT/RTs [15]; it is 24.4% for Spence et al. [8] and it is 23% with Rao et al. [7].
Spence et al. highlight the fact that there are non-ETMR CNS tumors with LIN28A immunoreactivity, and the findings obtained in this study indicate that LIN28A immunopositivity with C19MC amplification does not always occur concurrently [8].
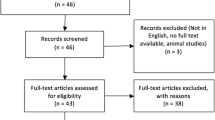
Since ETMRs are recognized as a distinct entity in the WHO 2016 classification, 63 cases have been published till now (Table 2). Immunohistochemical for LIN28A immunoreactivity was performed on 22 cases and was positive in 19 cases. We observed amplification at 19q13.42 in 90% from a total of 20 cases (Table 2).
In those cases in which molecular testing cannot be performed, the presence of multilayered rosettes is mandatory and such cases should be diagnosed as ETMR, not otherwise specified [1].
In our illustrative case, as well as in many other case reports cited here, neither LIN28 immunostaining nor C19MC amplification analysis was performed, as the facilities are not available at our center.
Management and outcomes
A standard effective and well-accepted treatment protocol for the optimal management of ETMR patients is yet to be defined. Many author recommend complete surgery resection which is critical to relieve intracranial hypertension followed by systemic chemotherapy and craniospinal radiation when appropriate [9].
Extended resection up to 1 cm in the surrounding brain, or including infiltrated tissue, is reported to improve patient outcome [19].
In this strategy, chemotherapy relies on high-dose chemotherapy which could compensate for the avoidance or dose reduction in prophylactic craniospinal irradiation. But, the effectiveness of high-dose chemotherapy on long-term survival is difficult to extrapolate from the literature due to small patient numbers [9, 23].
In more recent studies, conventional craniospinal radiotherapy, which is given after a complete surgery and high-dose chemotherapy, may contribute to improved outcomes. These findings are consistent with the experience of Horwitz et al. [9] who reported the 1-year event free survival (EFS), and overall survival (OS) rate were 36% CI 95% (23–55) and 45% CI 95% (31–64), respectively. The 2-year EFS and OS rate reported by Chi et al. were 53% and 70% [24].
In comparison, the 1-year EFS and OS rate reported by Korshunov et al. were 16% and 14%, respectively. Their treatment strategy relies only on chemotherapy and high-dose chemotherapy after surgery [25].
However, as children with ETMR are for the most of all less than 4 years old, radiotherapy potentially impairs neurocognitive function; some authors reported the feasibility and effectiveness of chemotherapy followed by conventional craniospinal radiotherapy but benefits and long-term toxicities have to be balanced [26, 27].
Exemplary case description
A 2-year-old girl presented with two episodes of seizure, multiple episodes of vomiting, and weakness of the left side of the body since 7 days.
There was no history of trauma. She was otherwise in good health and had no relevant past medical history. Salient findings on neurological examination were tightness of left limbs, ptosis, and limitation of upward gaze in the left eye. Both pupils measured 3 mm with a normal reaction to light and accommodation. Fundus examination was normal. There was no other cranial nerve deficit.
The rest of the head and neck examination was unremarkable.
Our patient’s magnetic resonance imaging (MRI) scan findings are consistent with those in previous reports; it demonstrated a 7 × 6 × 5 cm heterogeneous solid mass lesion, mass effect, and mild midline shift in the right parieto-occipital region. The tumor was hypointense on T1-weighted images, hyperintense on T2-weighted images with minimal contrast enhancement. (Fig. 1).
Preoperative magnetic resonance imaging (MRI). Axial precontrast T1-weighted images show a huge and well-circumscribed mass in the right parieto-occipital region, which is hypointense to adjacent brain in most parts (a). The cerebral falx clearly shifts to the left. Axial (b) and coronal (f) T2-weighted image shows mass with mixed signal intensity, including iso- and hyperintense signal. Apparent vascular edema is present in surrounding area. Axial postcontrast T1-weighted images show the mass with minimal inhomogeneous contrast enhancement (c). Fluid-attenuated inversion recovery sequence reveals mild hyperintensity (d) and lesion shows no diffusion restriction (e)
The imaging features were suggestive of a PNET. She underwent right parieto-occipital craniotomy with total resection. The tumor was seen gray-white, soft, friable and moderately vascular and had a poor plane of cleavage from the adjacent brain parenchyma with adherence to the dura.
Histopathological examination found a tumor with a biphasic, histological architecture characterized by a combination of hypercellular areas of small blue cells with minimal cytoplasm admixed with paucicellular neuropil areas, and numerous multilayered rosettes were found in both regions of the tumor. Immunohistochemistry showed the cells to be positive for synaptophysin, vimentin, and they are negative for cytokeratin (Fig. 2); a diagnosis of embryonal tumor with multilayered rosettes was made.
Histopathology showed a H&E × 10: biphasic histologic pattern: areas of small embryonal cells with multilayered rosettes and paucicellular fibrillar areas. b H&E × 40: multilayered rosettes consisting of pseudostratified neuroepithelium with a central round lumen. Immunohistochemistry × 40: the neuropil-like areas show positive expression for synaptophysin (c) and vimentin (d). Tumor cells are negative for cytokeratin (e)
She had an uncomplicated postoperative course with spontaneous recovery of the left oculomotor palsy 1 week after surgery that we do not have an explanation. She was sent for adjuvant chemotherapy. The girl was treated according to the medulloblastoma 2008 high-risk protocol (vincristine, cyclophosphamide, and etoposide). She has been under follow-up for the past 6 months with no evidence of recurrence.
Conclusion
Pediatric intracranial ETMR is a highly aggressive neoplasm and it should be considered in the differential diagnosis of pediatric brain tumors. In the absence of such guidelines, the role of adjuvant therapy remains unclear. Despite some case reports show long-term disease-free survival, the survival rate of patients with ETMR has been overall poor due to its highly malignant course.
Future studies should analyze clinical, radiological, biological, and prognostic results to try to better define therapeutic modalities.
References
Korshunov A, Sturm D, Ryzhova M, Hovestadt V, Gessi M, Jones DTW, Remke M, Northcott P, Perry A, Picard D, Rosenblum M, Antonelli M, Aronica E, Schüller U, Hasselblatt M, Woehrer A, Zheludkova O, Kumirova E, Puget S, Taylor MD, Giangaspero F, Peter Collins V, von Deimling A, Lichter P, Huang A, Pietsch T, Pfister SM, Kool M (2014) Embryonal tumor with abundant neuropil and true rosettes (ETANTR) , ependymoblastoma, and medulloepithelioma share molecular similarity and comprise a single clinicopathological entity. Acta Neuropathol 128(2):279–289
Edmonson CA, Weaver KJ, Kresak J, Pincus DW (2015) Embryonal tumor with multilayered rosettes of the fourth ventricle: case report. J Neurosurg Pediatr 16:579–583. https://doi.org/10.3171/2015.3.PEDS1525
Eberhart CG, Brat DJ, Cohen KJ, Burger PC (2000) Pediatric neuroblastic brain tumors containing abundant neuropil and true rosettes. Pediatr Dev Pathol 3(4):346–352
Tariq MU, Ahmad Z, Minhas MK, Memon A, Mushtaq N, Hawkins C (2017) Embryonal tumor with multilayered rosettes, C19MC-altered: report of an extremely rare malignant pediatric central nervous system neoplasm. SAGE Open Medical Case Reports 5:2050313X17745208. https://doi.org/10.1177/2050313X17745208
Nobusawa S, Yokoo H, Hirato J, Kakita A, Takahashi H, Sugino T, Tasaki K, Itoh H, Hatori T, Shimoyama Y, Nakazawa A, Nishizawa S, Kishimoto H, Matsuoka K, Nakayama M, Okura N, Nakazato Y (2012) Analysis of chromosome 19q13.42 amplification in embryonal brain tumors with ependymoblastic multilayered rosettes. Brain Pathol 22(5):689–697. https://doi.org/10.1111/j.1750-3639.2012.00574.x
Ceccom J, Bourdeaut F, Loukh N, Rigau V, Milin S, Takin R, Richer W, Uro-Coste E, Couturier J, Bertozzi AI, Delattre O, Delisle MB (2014) Embryonal tumor with multilayered rosettes: diagnostic tools update and review of the literature. Clin Neuropathol 33(1):15–22. https://doi.org/10.5414/NP300636
Rao S, Rajeswarie RT, Chickabasaviah YT, Nandeesh BN, Arivazhagan A, Santosh V (2017) LIN28A, a sensitive immunohistochemical marker for embryonal tumor with multilayered rosettes (ETMR), is also positive in a subset of atypical Teratoid/Rhabdoid tumor (AT/RT). Childs Nerv Syst 33(11):1953–1959. https://doi.org/10.1007/s00381-017-3551-6
Spence T, Sin-Chan P, Picard D, Barszczyk M, Hoss K, Lu M, Kim SK, Ra YS, Nakamura H, Fangusaro J, Hwang E, Kiehna E, Toledano H, Wang Y, Shi Q, Johnston D, Michaud J, la Spina M, Buccoliero AM, Adamek D, Camelo-Piragua S, Peter Collins V, Jones C, Kabbara N, Jurdi N, Varlet P, Perry A, Scharnhorst D, Fan X, Muraszko KM, Eberhart CG, Ng HK, Gururangan S, van Meter T, Remke M, Lafay-Cousin L, Chan JA, Sirachainan N, Pomeroy SL, Clifford SC, Gajjar A, Shago M, Halliday W, Taylor MD, Grundy R, Lau CC, Phillips J, Bouffet E, Dirks PB, Hawkins CE, Huang A (2014) CNS-PNETs with C19MC amplification and/or LIN28 expression comprise a distinct histogenetic diagnostic and therapeutic entity. Acta Neuropathol 128:291–303
Horwitz M, Dufour C, Leblond P, Bourdeaut F, Faure-Conter C, Bertozzi AI, Delisle MB, Palenzuela G, Jouvet A, Scavarda D, Vinchon M, Padovani L, Gaudart J, Branger DF, Andre N (2016) Embryonal tumors with multilayered rosettes in children: the SFCE experience. Childs Nerv Syst 32:299–305. https://doi.org/10.1007/s00381-015-2920-2
Picard D, Miller S, Hawkins CE, Bouffet E, Rogers HA, Chan TSY et al (2012) Markers of survival and metastatic potential in childhood CNS primitive neuro-ectodermal brain tumours: an integrative genomic analysis. Lancet Oncol 13(8):838–848
Frazier AA (2018) Four levels of diagnosis in the rare pediatric embryonal tumor of the CNS called embryonal tumor with multilayered rosettes. Radiographics 38(2):524. https://doi.org/10.1148/rg.2018184003
Wang B, Gogia B, Fuller GN, Ketonen LM (2018) Embryonal tumor with multilayered rosettes, C19MC-altered: clinical, pathological, and neuroimaging findings. J Neuroimaging 28:483–489. https://doi.org/10.1111/jon.12524
Govindan A, Alapatt JP (2017, 2017) Embryonal tumor with multilayered rosettes in a 3-year-old girl: case report. Turk Neurosurg. https://doi.org/10.5137/1019-5149.JTN.19621-16.0
Pfister S, Remke M, Castoldi M, Bai AHC, Muckenthaler MU, Kulozik A, von Deimling A, Pscherer A, Lichter P, Korshunov A (2009) Novel genomic amplification targeting the microRNA cluster at 19q13.42 in a pediatric embryonal tumor with abundantneuropil and true rosettes. Acta Neuropathol 117:457–464
Korshunov A, Ryzhova M, Jones DTW, Northcott PA, van Sluis P, Volckmann R, Koster J, Versteeg R, Cowdrey C, Perry A, Picard D, Rosenblum M, Giangaspero F, Aronica E, Schüller U, Hasselblatt M, Collins VP, von Deimling A, Lichter P, Huang A, Pfister SM, Kool M (2012) LIN28A immunoreactivity is a potent diagnostic marker of embryonal tumor with multilayered rosettes (ETMR). Acta Neuropathol 124:875–881
Leal Ferman L, Daigle P, Weil A, Ellezam B, Hamel P, Perreault S (2018) Embryonal tumor with multilayered rosettes presenting with intermittent third nerve palsy. Canadian Journal of Neurological Sciences / Journal Canadien Des Sciences Neurologiques 45(4):483–484. https://doi.org/10.1017/cjn.2018.23
Gupta K, Singh V, Aggarwal A, Salunke P (2018) Embryonal tumor with multilayered rosettes: diagnosis on intra-operative squash smear. Neuropathology 38(4):387–391. https://doi.org/10.1111/neup.12460
Tanaka H, Yamamoto D, Ikeda M, Morikawa M, Ueda K, Tanaka K, Sasayama T, Kohmura E (2018) Embryonal brain tumor with unknown primary lesion and massive cerebrospinal fluid dissemination: a case report. J Clin Neurosci 54:125–128
Li Q, Chen N, Ju Y (2018) Infantile medulloepithelioma in the lateral ventricle and cerebellopontine angle: two case reports. Medicine 97(20):e10751. https://doi.org/10.1097/MD.0000000000010751
Grassham CD, Rady S, Foster K, SantaCruz KS, Kuttesch JF, Maxwell JR (2018, 2018) A congenital case of ependymoblastoma: a rare and aggressive brain tumor. J Pediatr Hematol Oncol 1. https://doi.org/10.1097/MPH.0000000000001117
Shah AH, Khatib Z, Niazi T (2018) Extracranial extra-CNS spread of embryonal tumor with multilayered rosettes (ETMR): case series and systematic review. Childs Nerv Syst 34:649–654. https://doi.org/10.1007/s00381-017-3657-x
Chen SH, Ho CS, Chiu NC, Chen HJ, Lin YJ (2017) Rare brain tumor in a neonate. J Med Ultrasound 25(4):240–243. https://doi.org/10.1016/j.jmu.2017.09.004
Mozes P, Hauser P, Hortobágyi T, Benyó G, Peták I, Garami M, Cserháti A, Bartyik K, Bognár L, Nagy Z, Turányi E, Hideghéty K (2016) Evaluation of the good tumor response of embryonal tumor with abundant neuropil and true rosettes (ETANTR). J Neuro-Oncol 126:99–105. https://doi.org/10.1007/s11060-015-1938-3
Chi SN, Zimmerman MA, Yao X, Cohen KJ, Burger P, Biegel JA, Rorke-Adams LB, Fisher MJ, Janss A, Mazewski C, Goldman S, Manley PE, Bowers DC, Bendel A, Rubin J, Turner CD, Marcus KJ, Goumnerova L, Ullrich NJ, Kieran MW (2009) Intensive multimodality treatment for children with newly diagnosed CNS atypical teratoid rhabdoid tumor. J Clin Oncol 27(3):385–389. https://doi.org/10.1200/JCO.2008.18.7724
Korshunov A, Remke M, Gessi M, Ryzhova M, Hielscher T, Witt H, Tobias V, Buccoliero AM, Sardi I, Gardiman MP, Bonnin J, Scheithauer B, Kulozik AE, Witt O, Mork S, von Deimling A, Wiestler OD, Giangaspero F, Rosenblum M, Pietsch T, Lichter P, Pfister SM (2010) Focal genomic amplification at 19q13.42 comprises a powerful diagnostic marker for embryonal tumors with ependymoblastic rosettes. Acta Neuropathol 120(2):253–260
Dufour C, Delisle M-B, Geoffray A, Laplanche A, Frappaz D, Icher C et al (2014) CT-003. Tandem high-dose chemotherapy with stem cell rescue followed by risk-adapted radiation in children with high-risk cerebral primitive neuroectodermal tumor: results of the prospective sfce-trial pnet hr + 5. Neuro-Oncology 16(suppl 1):i10–i13
Padovani L, André N, Constine LS, Muracciole X (2012) Neurocognitive function after radiotherapy for paediatric brain tumours. Nat Rev Neurol 8(10):578–588
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Rights and permissions
About this article
Cite this article
Bouali, S., Zehani, A., Mahmoud, M. et al. Embryonal tumor with multilayered rosettes: illustrative case and review of the literature. Childs Nerv Syst 34, 2361–2369 (2018). https://doi.org/10.1007/s00381-018-3972-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3972-x