Abstract
Purpose
Treatment of cerebral arteriovenous malformations (AVM)—the most common cause of stroke in the pediatric population—can be challenging due to the complexity of size, morphology, and location. There is a significant risk in comparison to AVM treatment among adults. Thus, AVM treatment in the pediatric population imposes unique challenges. Recent improvements include optimized catheter techniques and better embolization materials, such as Onyx, a non-adhesive liquid embolic agent used in the adult population. These improvements have increased the success rate of total and near-total obliteration of cerebral AVM. However, the use of Onyx causes significant distortion of the MR and CT images, which must be accounted for in any radiation treatment planning predicated on CT and MRI. These image distortions impact on the actual delivered dose to the nidus and behoove heterogeneity correction. Our group has previously shared a solution for heterogeneity correction in the adult population. The purpose of this study is to show our experience in this unique group of pediatric patients.
Methods
This is a retrospective review of pediatric patients, who were undergoing combined endovascular embolization followed by SRS. The cohort consists of 14 patients undergoing SRS treatment in our institute between November 2006 and December 2012 with a mean follow-up of 49.9 months. Within this cohort, we retrospectively reviewed 12 consecutive pediatric patients who underwent a combined endovascular and SRS approach with a mean follow-up of 52.1 months and two patients receiving SRS-only treatment were excluded.
Results
In our cohort of 14 patients, 7 (50%) were male, with a mean age of 17.3 years (12.0–22.9) at the time of radiosurgery treatment. Mean age of beginning the combined modality treatment was 15.3 years (8.4–20). The median time from diagnosis to SRS was 24.3 months (11.1–64.4 months) in the complete cohort and 25.6 months (11.1–64.4) in the multimodality group. The overall median follow-up period was 49.9 months (range 12.8–118.8 months) in the complete cohort and 52.1 months (range 12.8–118.8 months) in the multimodality group. Eleven (78.6%) patients had at least one episode of hemorrhage prior to treatment. Spezler-Martin grades at baseline ranged from 2 to 5 (mean 3.2). Fifty percent had grade IV and V. Patients underwent a median of 2 (range 1–5) embolization procedures. The radiosurgical treatment dose to the margin of the angiography-based nidus: median prescription dose of 21.49 Gy (14.39–27.51) with a median max dose of 27.77 Gy (18.93–32.52). The median treatment volume was 0.6 cm3 (0.1–7.3 cm3). The Onyx embolization reduced the nidus target volume by a median of 66.7% (12.0–92.7%). We confirmed 10/14 (71%) complete closures. In 2/14 (14.2%) additional patients, a significant flow reduction was noted. In 1/14 (7.1%) patients, no significant change was noted during the observation period and two (14.2%) patients were without follow-up information. In two patients, post-treatment edema was noted; however, none was clinically significant and resolved without additional intervention or treatment.
Conclusions
This cohort comprises the largest combined Onyx-SRS pediatric experience in the literature. In conjunction with our adult group study, we show that the use of Onyx reduces the SRS treatment target volume significantly. Importantly, we implemented the heterogeneity correction to avoid increased radiation exposure to normal surrounding brain tissue. The combined approach appears to be safe provided that the above-mentioned corrections are implemented.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The therapeutic approach for cerebral arteriovenous malformation (AVM) has evolved significantly in recent years by refinement of endovascular, microsurgical, and radiosurgical techniques [1], all of which are considered viable treatments alone or in combination. Combined endovascular embolization and stereotactic radiosurgery (SRS) in the treatment of AVM has been the subject of multiple publications in the last decade [2,3,4,5,6] including reports from our group [7, 8]. Still, radiation-induced complications especially when the volume of the lesion is large constitute an obstacle to overcome. In the adult population, it has been demonstrated that the efficacy of SRS is volume-dependent, and obliteration rates in larger AVMs have been reported as low as 23–36% [9, 10]. Two approaches have been developed to neutralize this limitation. Staged volume SRS, although considered relatively safe, is associated with the risk of re-bleeding until the entire AVM is obliterated. The second option, AVM embolization, allows additional size reduction.
The combination of embolization and radiosurgery is often used in the treatment of cerebral AVMs of higher grades. Specific factors as reflected by surgical (Spezler-Martin) and radiosurgical (AVM score Pollock-Flickinger) scores depending on location, volume, and venous drainage will markedly influence the decision-making for the optimal treatment recommendation [11,12,13]. Although there is no score that takes combined treatment approaches into account, the goal remains complete obliteration of the AVM nidus while minimizing postprocedural adverse radiation effects [14,15,16]. Radiation-related toxicity is thought to be a function of nidus volume. The pre-radiosurgery embolization which yields volume reduction should impact and reduce treatment morbidity.
Extensive data have been published concerning combined endovascular and radiosurgery treatment in the adult population, but this has been rarely applied to the pediatric population and, to the best of our knowledge, not in combination with Onyx™ (Medtronic, USA). In addition to recent improvements in catheter techniques, our group has utilized Onyx as the primary embolization material with the aim of definitive obliteration since 2006.
We followed this line of treatment, in partially occluded nidus AVM, and added stereotactic radiosurgery after previous embolization. This report summarizes our experience in the pediatric patient cohort.
Materials and methods
Patient population and analysis
This is a retrospective review of pediatric patients, who were undergoing combined endovascular embolization followed by SRS. Data concerning treatment details were prospectively entered into our institutional radiosurgery and angiography databases. This cohort consists of 14 patients undergoing SRS treatment in our medical center between November 2006 and December 2012 with a mean follow-up of 49.9 months. Of this cohort, we retrospectively reviewed 12 consecutive pediatric patients who underwent a combined endovascular and SRS approach with a mean follow-up of 52.1 months and two patients receiving SRS-only treatment were excluded. This study was approved by our institutional ethics review committee. Inclusion criteria mandated a follow-up of at least 18 months after the SRS procedure.
Endovascular treatment procedure
All endovascular procedures were performed by a single invasive neuroradiologist (S.M.). Detailed description of the embolization procedure, clinical outcomes, and risks was recently published by our group [8, 17]. All endovascular treatments were carried out while the patients were under general anesthesia. Catheterization was performed by a trans-femoral approach using standard coaxial techniques, navigating the tip of the microcatheter as close as possible to the nidus. Onyx was slowly and progressively injected into the nidus under continuous visual control in an attempt to completely occlude the proximal draining veins at the end of treatment. The embolization sessions were halted when the nidus became inaccessible due to unfavorable anatomy of feeders and a high-risk/benefit ratio for the patient. At that point, other treatment options were considered. Patients with small remnants without bleeding, or with remnants in deep or eloquent areas, were referred to radiosurgery. Patients underwent a median of 2 (range 1–5) embolization procedures. The embolization material used in total was mean 2.8 cm3 (0.5–7.7 cm3) per patient.
Radiosurgical procedures
Precise target definition of the residual AVM nidus was achieved using stereotactic cerebral digital subtraction angiography fused with cranial CT and MRI/MRA scans. All the angiography and embolization procedures were performed by the same neuroradiologist (S.M.), who was also involved in the target definition of the nidus prior to the SRS treatment. The embolized portion of the AVM was not typically included in the SRS target volume. When it could be clearly identified, we included the origin of the draining veins into the target volume. The nidus volume was measured using iPlan® software (BrainLab, Munich Germany). The follow-up review of all neuro-imaging and the decision-making process for follow-up angiography was likewise performed jointly by the senior neuroradiologist and neurosurgeon (A.A.K.).
The details of the SRS treatment procedure are published elsewhere [7] Briefly, the procedure was performed with a LINAC-based platform (Synergy S®, ELEKTA, Sweden), using frame-based head immobilization for registration and treatment. SRS treatment was accomplished using a combination of static fixed beams and/or static arcs to achieve optimal and conformal target coverage. The median treatment volume was 0.6 cm3 (0.1–7.3 cm3). The radiosurgical treatment dose to the margin of the angiography-based nidus: median prescription dose of 21.49 Gy (14.39–27.51) with a median max dose of 27.77 Gy (18.93–32.52) taking volume, location, and clinical aspects into consideration.
Follow-up visits in our outpatient clinic were scheduled after MRI/MRA at 6 months and at 1, 2, 3, 4, and 5 years after the initial SRS procedure. Treatment success was defined when the MRI/MRA indicated significant reduction or absence of the T1-T2 flow artifacts as well as contrast enhancement of pathological vessels [18, 19]. Patients were also invited to undergo a diagnostic digital angiography evaluation.
Two patients were lost to follow-up immediately after treatment.
Pre- and post-embolization, as well as SRS modified Rankin Score (mRS), was calculated. Average mRS on admission was 2 (median 1), average mRS on follow-up 0 (median 0).
All patients and treatment modalities were discussed in a multidisciplinary neurovascular conference and final decisions were discussed during the consent process with family members.
Results
Patient demographics
In our cohort of 14 patients, 7 (50%) were male, with a mean age of 17.3 years (12.0–22.9) at the time of radiosurgery treatment. Mean age of beginning the combined modality treatment was 15.3 years (8.4–20). The median time from diagnosis to SRS was 24.3 months (11.1–64.4 months) in the complete cohort and 25.6 months (11.1–64.4) in the multimodality group. Eleven (78.6%) patients had at least one episode of hemorrhage prior to their treatment. Two patients presented with seizures and no evidence of hemorrhage; one patient presented with hemiparesis. Spezler/Martin grade prior to the embolization was mean 3.2 (range 2–5), reflecting 50% with IV and V grade. Follow-up was done for a median of 51.0 months and mean of 49.9 months. (Table 1).
Embolization procedure
Patients underwent a median of two (range 1–5) embolization procedures. The embolization material used in total was mean 2.8 cm3 (0.5–7.7 cm3) per patient. The radiosurgical treatment dose to the margin of the angiography-based nidus: median prescription dose of 21.49 Gy (14.39–27.51 Gy) with a median max dose of 27.77 Gy (18.93–32.52 Gy). The median SRS treatment volume was 0.6 cm3 (0.1–7.3 cm3). The Onyx embolization reduced the nidus target volume by a median of 66.7% (12.0–92.7%), mean follow-up period of 49.9 months (12.8–71.6 months).
Obliteration rates and outcome
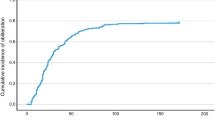
The overall median follow-up period was 49.9 months (range 12.8–118.8 months) in the complete cohort and 52.1 months (range 12.8–118.8 months) in the multimodality treatment group. We confirmed 10 (71%) complete nidus closure at a median time of 49.9 from SRS, similar to our adult subgroup study [20]. The lesion of one patient has shown improvement in flow reduction, the lesion of another patient remains patent, and two patients were lost to follow-up. High-resolution MRI/MRA was routinely performed in all patients. Confirmation digital subtraction angiography (DSA) was performed in five patients and five performed only MRI-MRA studies.
Complications related to SRS treatment
Transient edema developed in two patients. Each patient had a frontal lesion. In each case, the edema resolved over a course of 12 weeks. One patient diagnosed with SM grade 4 temporal AVM presenting with hemiparesis had non-closure following two endovascular treatments. He remains with mild facial asymmetry and continues to be followed.
Discussion
The current report of a pediatric AVM cohort comprises the largest combined Onyx-SRS experience in the literature. Aside from the difference in age, the pediatric AVM population, when compared to adults, is characterized by a significantly higher risk of intracranial hemorrhage and frank mortality. By definition, the pediatric population is a high-risk population that must be addressed with appropriate procedures [4, 5].
We have previously shown [8, 17] that the use of Onyx reduces the treatment volume significantly. Of note, we implemented a heterogeneity correction to avoid increased radiation exposure to normal surrounding brain tissue. The combined approach appears to be safe provided that the above-mentioned corrections are implemented.
The combination treatment of SRS following Onyx embolization for AVM has been recently reported [6] as a definitive treatment option. The use of Onyx has been proposed by several groups as a replacement for glue and histoacryl [21]. The potential delineation and distortion of the radiosurgical target following embolization is a common planning obstacle. Our group has published a possible dosage error correction in treatment planning in the past [7]. Notwithstanding, the identification of patent nidus and image distortion due to Onyx residue remains challenging.
Understanding and targeting the AVM in an efficient fashion and accounting for corrected electron density of Onyx is crucial in these treatment modalities. When considering a multimodal treatment approach to complex lesions, often a single SRS treatment is not possible. Using radiosurgery treatment after endovascular embolization with Onyx enabled us to reach relatively high obliteration rates in otherwise high-risk AVMs.
We emphasize that using Onyx as a definitive embolization agent does not show the same recanalization rates as previous agents had shown, thus allowing a higher SRS radiation dosage for a smaller non-embolized residual target, resulting in fewer side effects.
The follow-up modality for assessing the obliteration progress usually consists of DSA or MRI-MRA. We recommend DSA when we observe a closed nidus in MRI (i.e., no flow void or nidus). In the absence of complete closure, we recommend obtaining a DSA. However, it is important to note that the time to closure of the AVM or rather the exact improvement cannot be known or feasible due to relatively long follow-up windows. MRI scans were obtained with high-resolution 3D volumetric calculations using MRI time of flight (case Fig. 1).
Classification of Spetzler Martin grade has been used for over 20 years and represents the widely accepted method for predicting surgical outcome. AVM grading classification with focus on radiosurgery treatment risk and outcome, developed by the Mayo Clinic and the University of Pittsburgh Medical Center initially proposed in 2002 by Pollock and colleagues [12] and later modified in 2008 [13], is widely accepted by the neurosurgical community to predict obliteration without new deficits and decline in mRS.
Specific factors as reflected by surgical (Spezler/Martin) and radiosurgical (AVM score Pollock-Flickinger) scores depending on location, volume, and venous drainage will markedly influence the decision-making for the optimal treatment recommendation. There is no score that takes combined treatment approaches into account.
Our results (Table 2) reveal mRS decline in follow-up with a corresponding Pollock Flickinger score of favorable outcome [22]. Relatively minor clinical complications following the procedures, including seizures and transient hemiparesis, resolved. Meanwhile, edema that was evident on imaging resolved spontaneously.
Other than one patient harboring a single small ACA pseudo aneurysm feeding a basal ganglia AVM which was subsequently embolized, we have not identified associated intracranial aneurysms in our study, supporting a lesser risk of re-bleed after treatment [15]. Furthermore, consistent with the findings of Kano et al. [15, 16], we did not identify any hemorrhage after obliteration had occurred, although patients do remain at risk during the latency period between treatments.
Study limitations
We encountered several limitations in our analysis. Small number of patients and intermediate follow-up compromise significant subgroup analysis. We speculate that longer follow-up would result in more apparent complications possibly related to this multimodal treatment including adverse radiation effect, intracranial hemorrhage, seizures, long-term morbidity, and mortality. As both embolization technique and SRS require considerable technical experience, one should take into account this combined modality approach and the advantage of consistent treatment given by a multidisciplinary treatment team.
Conclusion
Cerebral AVM treatment in the pediatric population continues to require a unique and multidisciplinary approach. Incorporating multimodality planning with Onyx embolization prior to SRS treatment plan, particularly when accounting for distortion and heterogeneity correction, may provide the safest treatment paradigm.
References
Lanzino G (2012) Role of radiosurgery for arteriovenous malformations. J Neurosurg 116:7–8 discussion 9-10
Blackburn SL, Ashley WW Jr, Rich KM, Simpson JR, Drzymala RE, Ray WZ, Moran CJ, Cross DT 3rd, Chicoine MR, Dacey RG Jr, Derdeyn CP, Zipfel GJ (2011) Combined endovascular embolization and stereotactic radiosurgery in the treatment of large arteriovenous malformations. J Neurosurg 114:1758–1767
Gobin YP, Laurent A, Merienne L, Schlienger M, Aymard A, Houdart E, Casasco A, Lefkopoulos D, George B, Merland JJ (1996) Treatment of brain arteriovenous malformations by embolization and radiosurgery. J Neurosurg 85:19–28
Ding D, Starke RM, Kano H, Mathieu D, Huang PP, Feliciano C, Rodriguez-Mercado R, Almodovar L, Grills IS, Silva D, Abbassy M, Missios S, Kondziolka D, Barnett GH, Dade Lunsford L, Sheehan JP (2017) International multicenter cohort study of pediatric brain arteriovenous malformations. Part 1: predictors of hemorrhagic presentation. J Neurosurg Pediatr 19:127–135
Starke RM, Ding D, Kano H, Mathieu D, Huang PP, Feliciano C, Rodriguez-Mercado R, Almodovar L, Grills IS, Silva D, Abbassy M, Missios S, Kondziolka D, Barnett GH, Dade Lunsford L, Sheehan JP (2017) International multicenter cohort study of pediatric brain arteriovenous malformations. Part 2: outcomes after stereotactic radiosurgery. J Neurosurg Pediatr 19:136–148
Lee CC, Chen CJ, Ball B, Schlesinger D, Xu Z, Yen CP, Sheehan J (2015) Stereotactic radiosurgery for arteriovenous malformations after Onyx embolization: a case-control study. J Neurosurg 123:126–135
Shtraus N, Schifter D, Corn BW, Maimon S, Alani S, Frolov V, Matceyevsky D, Kanner AA (2010) Radiosurgical treatment planning of AVM following embolization with Onyx: possible dosage error in treatment planning can be averted. J Neuro-Oncol 98:271–276
Strauss I, Frolov V, Buchbut D, Gonen L, Maimon S (2013) Critical appraisal of endovascular treatment of brain arteriovenous malformation using Onyx in a series of 92 consecutive patients. Acta Neurochir 155:611–617
Miyawaki L, Dowd C, Wara W, Goldsmith B, Albright N, Gutin P, Halbach V, Hieshima G, Higashida R, Lulu B, Pitts L, Schell M, Smith V, Weaver K, Wilson C, Larson D (1999) Five year results of LINAC radiosurgery for arteriovenous malformations: outcome for large AVMS. Int J Radiat Oncol Biol Phys 44:1089–1106
Pollock BE, Gorman DA, Coffey RJ (2003) Patient outcomes after arteriovenous malformation radiosurgical management: results based on a 5- to 14-year follow-up study. Neurosurgery 52:1291–1296 discussion 1296–1297
Spetzler RF, Martin NA (1986) A proposed grading system for arteriovenous malformations. J Neurosurg 65:476–483
Pollock BE, Flickinger JC (2002) A proposed radiosurgery-based grading system for arteriovenous malformations. J Neurosurg 96:79–85
Pollock BE, Flickinger JC (2008) Modification of the radiosurgery-based arteriovenous malformation grading system. Neurosurgery 63:239–243 discussion 243
Kano H, Kondziolka D, Flickinger JC, Yang HC, Flannery TJ, Awan NR, Niranjan A, Novotny J, Lunsford LD (2012) Stereotactic radiosurgery for arteriovenous malformations, part 2: management of pediatric patients. J Neurosurg Pediatr 9:1–10
Kano H, Kondziolka D, Flickinger JC, Yang HC, Park KJ, Flannery TJ, Liu X, Niranjan A, Lunsford LD (2012) Aneurysms increase the risk of rebleeding after stereotactic radiosurgery for hemorrhagic arteriovenous malformations. Stroke 43:2586–2591
Kano H, Lunsford LD, Flickinger JC, Yang HC, Flannery TJ, Awan NR, Niranjan A, Novotny J Jr, Kondziolka D (2012) Stereotactic radiosurgery for arteriovenous malformations, part 1: management of Spetzler-Martin Grade I and II arteriovenous malformations. J Neurosurg 116:11–20
Maimon S, Strauss I, Frolov V, Margalit N, Ram Z (2010) Brain arteriovenous malformation treatment using a combination of Onyx and a new detachable tip microcatheter, SONIC: short-term results. AJNR Am J Neuroradiol 31:947–954
Lee CC, Reardon MA, Ball BZ, Chen CJ, Yen CP, Xu Z, Wintermark M, Sheehan J (2015) The predictive value of magnetic resonance imaging in evaluating intracranial arteriovenous malformation obliteration after stereotactic radiosurgery. J Neurosurg 123:136–144
Pollock BE, Kondziolka D, Flickinger JC, Patel AK, Bissonette DJ, Lunsford LD (1996) Magnetic resonance imaging: an accurate method to evaluate arteriovenous malformations after stereotactic radiosurgery. J Neurosurg 85:1044–1049
Strauss I, Haim O, Umansky D, Corn BW, Frolov V, Shtraus N, Maimon S, Kanner AA (2017) Impact of Onyx embolization on radiosurgical management of cerebral arteriovenous malformations: treatment and outcome. World neurosurgery 108:656–661
Pierot L, Kadziolka K, Litre F, Rousseaux P (2013) Combined treatment of brain AVMs with use of Onyx embolization followed by radiosurgery. AJNR Am J Neuroradiol 34:1395–1400
Wegner RE, Oysul K, Pollock BE, Sirin S, Kondziolka D, Niranjan A, Lunsford LD, Flickinger JC (2011) A modified radiosurgery-based arteriovenous malformation grading scale and its correlation with outcomes. Int J Radiat Oncol Biol Phys 79:1147–1150
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Umansky, D., Corn, B.W., Strauss, I. et al. Combined treatment approach to cerebral arteriovenous malformation in pediatric patients: stereotactic radiosurgery to partially Onyx-embolized AVM. Childs Nerv Syst 34, 2269–2274 (2018). https://doi.org/10.1007/s00381-018-3854-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3854-2