Abstract
Purpose
The purpose of this paper is to investigate occult spinal dysraphisms (OSD) using lumbar ultrasonography (LUS) in newborns presenting with specific skin markers or sacrococcygeal dimple.
Method
From 2012 to 2015, we performed LUS in newborns with cutaneous stigmata and/or sacroccygeal dimple. Magnetic resonance imaging (MRI) was performed in all patients with abnormal ultrasound or features of neurological involvement in order to detect spinal lesions.
Results
We prospectively evaluated 475 newborns who presented cutaneous stigmata performing LUS during their 4 weeks of life though 439 completed the study. All patients had a follow-up of almost 12 months. Of these, 39 presented abnormal ultrasonography and underwent MRI. In this group, spinal dysraphism was confirmed in 12 patients. When considering skin markers, dermal sinus correlated with higher risk of spinal cord lesions, on the other hand the presence of simple sacral dimple alone denoted a very low risk of occult spinal dysraphism. The simultaneous presence of more skin markers and/or the presence of lumbar ultrasonography abnormality regarding the level of the conus, pulsatility, and the position of the cord, thickness of the filum terminale, or the presence of an intratecal mass, lipoma, or dermal sinus tract indicated the necessity to perform MRI in order to detect spinal cord abnormalities because of higher risk of spinal lesions.
Conclusion
LUS in newborns with specific skin markers is a valid method to select patients in which MRI can be performed to detect OSD. The presence of a simple sacral dimple alone is a negligible marker for occult neural pathology while the presence of isolated dermal sinus or more than one cutaneous marker could be considered indicative of higher risk of spinal dysraphism.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spinal cord dysraphisms represent a broad spectrum of congenital anomalies resulting from impaired formation of structures along the craniospinal axis during development of the brain and spinal cord. They occur during weeks 2 to 6 of gestation and proceeds through a complex, multistep process [1].
In the case that these malformations are open or large, they are easily recognized, whereas closed or smaller herniation anomalies may present only as cutaneous abnormalities overlying the defect [2].
Occult spinal dysraphisms (OSD) refer to a broad range of skin-covered congenital anomalies caused by embryologic defects in the neural tube formation process. OSD may cause progressive neurological deterioration by a condition called tethered cord syndrome (TCS). TCS is caused by ischemia of the lower conus due to “traction” of the spinal cord occurring with growth and flexion.
In newborn, a tethered cord may be suspected if the sonography demonstrates a low conus medullaris terminating below the superior aspect of L3 vertebral body, in most cases beneath L3. In addition, the low tethered cord is usually eccentric within the spinal canal, often dorsal [3, 4].
The most common location for these defects along the spinal axis is the lumbosacral area. The presence of overlying cutaneous stigmata as a marker of OSD has been long recognized and is not surprising considering their intimate embryological association. The identification of the stigmata commonly associated with OSD is crucial because it may lead to an early intervention preventing irreversible damage from TCS. In fact, TCS causes neurologic and orthopedic abnormalities that may occur as a result of spinal dysraphisms. Treatment usually involves neurosurgical intervention [5, 6].
Cutaneous stigmata are found in 2.2 to 7.2% of all neonates but just few of these have a real occult dysraphism and only 0.5% of them require surgical intervention. Although these cutaneous stigmata are frequently found in patients with OSD, the positive predictive value of these stigmata for the presence of OSD cannot be known without adequate large-scale prospective studies. However, it is widely accepted that a combination of two or more cutaneous stigmata has a high predictive value, and some stigmata have a higher risk than others [7,8,9].
Infants with simple, low-lying sacrococcygeal dimples typically have normal spinal contents. On the other hand, atypical dimples, such those larger than 5 mm, located greater than 2.5 cm above the anus, or seen in combination with other lesions, are at higher risk of occult spinal dysraphism [(10,11,12).]
MRI is the standard criterion of radiological imaging test for spinal dysraphism. Nevertheless, the use of MRI is limited by its cost, availability, and the need for sedation in many children. Despite these limitations, MRI is still recommended as the preferred imaging modality when there is high pretest probability (high-risk findings) [1, 10,11,12,13].
Ultrasound (US) is a noninvasive screening modality that may be used for infants up to 6 months of age before ossification of the vertebral bodies; on the other hand, it is operator dependent and less sensitive than MRI [11–16].
The presence of small subcutaneous mass or small dermal sinus tracts may also decrease the sensitivity of US [7, 14, 17]. The MRI should be performed in the case that findings from ultrasound are inconclusive or abnormal.
We carried out a prospective study to detect spinal dysraphisms in newborns with cutaneous markers and/or sacrococcygeal dimple. We propose a flowchart for clinicians who utilize clinical signs and sacral US in newborns to select patients for MRI and neurosurgery to detect OSD.
Methods
Population
This prospective study was conducted between January 1, 2012, and December 31, 2015. Four hundred seventy-five newborns with sacral cutaneous markers underwent LUS at Spina Bifida Center, Women’s and Infant Health Sciences, A. Gemelli Policlinic, Catholic University of Sacred Heart of Rome. Newborns with neurological or orthopedic impairments at birth were excluded from the study because MRI was performed as soon as possible. During the study, 36 patients were excluded because of incomplete records. Therefore, 439 patients completed the study with a follow-up of almost 12 months. Every newborn with abnormal US performed MRI and neurosurgeon evaluation. Summary of the study design is reported in Fig. 1.
Regarding to sacral dimple, we classified atypical dimples, those larger than 5 mm, located more than 2.5 cm above the anus.
A database was created to include demographic information, referral sources, clinical signs, testing, and surgical results. Clinical and radiological information were obtained from radiology reports, the clinical charts of the referring pediatrician, and the evaluating pediatric neurosurgeon.
Imaging technique
LUS studies were performed in the prone decubitus using high-resolution 7–12-MHz linear array transducers utilizing a GE Logiq S8 ultrasound machine. Longitudinal and transverse images of the entire back can be obtained from the level of craniocervical junction to the tip of the coccyx [7].
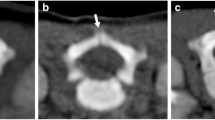
The normal range of the pediatric conus tip position is from T10–T11 interspace to the superior aspect of L3, most frequently located at L1. In neonates, the conus medullaris tip is usually located between L1 and L2 and occasionally extends to the superior end plate of L3. Real-time LUS allows evaluation of the normal oscillation of the spinal cord and cauda equine roots, which is synchronous with the heartbeat. Particular attention was given to the morphology of the conus, the presence or absence of a syrinx, thickening of the filum greater than or equal to 2 mm, lipomatous filum, soft-tissue mass, intradural or extradural mass, motion of the conus, vertebral anomaly, and dermal sinus [2, 7, 14,15,16, 18, 19].
MRI examination of the spine was performed in all patients with US abnormalities. When necessary, newborns and infants were sedated to keep them quiet during scanning by giving oral chloral hydrate syrup or intravenous lorazepam. MRI was performed with a 1.5 Tesla Siemens Magnetom Avanto B15 MR system (Siemens Healthcare, Erlangen, Germany) with the patient in the supine position.
Imaging was done using FOV of 200–250 mm in newborns and infants. First, T1-weighted (T1WI), T2-weighted (T2WI), and T2-weighted fat-suppressed sequences were taken in the sagittal plane. Then, T1WI and T2WI were taken in axial plane in affected spinal regions.
Statistical analysis
Statistical analysis was performed with SAS 9.1 (SAS Institute. Inc., Cary, NC).
Tables were used to analyze categorical variables, and continuous variables were compared using the Student t test. A p value of 0.05 or less was considered statically significant.
Results
Demographic information
From January 2012 to December 2015, 475 newborns with sacral cutaneous stigmata or sacral dimple were performed ultrasound examination. Of these, 439 newborns completed the study (233 boys and 206 girls) with a follow-up of almost 12 months (range 12–36 months). Mean gestational age at birth was 38.3 ± 2.56 (range 27–42 weeks). Mean birth weight was 3027 ± 635 g (range 660–4850 g). The mean age of the newborns at time of the LUS study was 7 ± 3 days (range 3–28 days). Characteristics of population were resumed in Table 1.
The six most commonly reported stigmata were the following:
sacral dimple; with a total of 323 patients (73%); of these 270 with only sacral dimple (61%), 53 with sacral dimple in association with others markers (12%), and 48 with atypical sacral dimple(10, %);
hairy patch (65 patients, 14%), hemangioma (51 patients, 11%), deviated gluteal cleft (75 patients, 17%), lipoma/fat mass (44 patients, 10%), and dermal sinus (10 patients, 2%). Results of cutaneous stigmata and correlation with OSD are resumed in Table 2.
Seventy newborns (16%) presented with a combination of cutaneous lesions. The most commonly seen combination was a hairy patch with a sacral dimple (30 of 70) and lipoma/fat mass with sacral dimple (15 of 70).
An abnormal LUS result was seen in 39 infants. Isolated abnormalities or in associated with low conus (defined as below the L2–3 interspace) were seen in 12 newborns, fat filum in 5 patients, thick filum in 7, cyst in the filum in 6, vertebral anomalies in 8, soft-tissue abnormalities in 15 one, and dermal sinus in 10 patients. All 39 patients were referred for MRI study, and abnormal results were confirmed in 22 patients: 7 dermal sinus, 5 spinal lipoma, 2 diastematomyelia, 2 spina bifida occulta, 1 ventriculus terminalis, 1 arachnoid cyst, 2 terminal myelocistocele, and 2 lateral meningocele. Findings on the other 17 imaging studies were unremarkable. Results are reported in Table 3.
At the moment, 5 patients (12.8%) in US abnormal group underwent neurosurgical procedures (2 intraspinal lipoma with cord tethering, 3 dermal sinus), while only 1 patient (0.25%) in the US normal group (400 newborns), when neurological involvement occurred, was performed MRI that evidenced dermal sinus and he was operated for tethered cord syndrome. At the end of the study, a total of 6 patients (1.4%) require neurosurgical procedures.
Discussion
OSD are a large spectrum of skin-covered congenital disorders caused by embryological defects in the neural tube formation process. Patients have different clinical findings from asymptomatic situations to association with anorectal or urogenital malformations.
In patients with OSD, there may appear a progressive neurological deterioration due to TCS.
The detection of OSD and the subsequent neurosurgical intervention are crucial to avoid this dangerous condition [20]. Many studies evidenced that a range of 43–95% patients with OSD presented at birth single or combinations of cutaneous sacrococcygeal stigmata [9, 21]. In accordance with literature in this sample, 5% of our newborns had an OSD and 1.2% requires surgical procedures. Sacrococcygeal dimple is present in 2–4% of normal newborns [2, 14]. Robinson et Mcgovern in their studies, reported a poor correlation of sacral dimple alone and OSD accordingly; the routine investigation of such findings is unnecessary [14, 22]. On the other hand, Kucera et al. evidenced that atypical dimple is strongly associated with spinal lesions. In our data, we confirm that there is no correlation between the mere presence of sacral dimple and OSD, whereas in presence of an atypical one, there is a higher risk of spinal lesions. Some authors pointed out that medial little hemangioma and pigmentary nevus are benign lesions and do not entail further diagnostic investigations in the absence of signs or symptoms. In accordance with these studies, no patients with these stigmata were correlated with OSD in our cohort.
OSD can be detected with US and MRI [1, 4, 10,11,12,13]. Mcgovern et al. evidenced that LUS performed on the basis of multiple clinical indications is six times more likely to detect spinal dysraphism than imaging performed for isolated abnormalities or risk factors and that sacral dimple is a poor marker for occult spinal pathology.
US is a noninvasive imaging modality that should be considered as first method of screening in order to investigate spinal cord dysraphism in newborns before six month of life when the ossification process of vertebral bodies is still not completed [9, 21, 23].
Unsinn et al. demonstrated that US of the spinal cord and spinal canal is a reliable method of examining newborns and young infants. Indications for early US examination during the newborn period are the following clinical findings: cutaneous lesions of the back (e.g., hypertrichosis, sacral sinus, subcutaneous lipoma); deformities of the spinal column (e.g., scoliosis, malformations of the sacrum); neurologic disturbances (e.g., paresis, neurogenic bladder or bowel dysfunction); suspected spinal cord injury due to traumatic birth; and syndromes with associated spinal cord compression. An early performed US allows an exact examination of the spinal canal and its contents; furthermore, it enables one to rule out significant pathologic conditions. In patients with normal findings, no further imaging examinations are necessary. In patients with spinal malformations detected by US, a further examination can be performed at the time of the elective surgical intervention. In addition, in complex spinal malformations, the role of US is to allow detection of associated anomalies. In the first month of life, US is a good choice to perform a screening in patients with specific cutaneous markers of OSD. US is operator dependent and less sensitive than MRI. In his work, Dick concluded that the US was equal to spinal MRI in demonstrating OSD. Most authors agree with this result, thus given SUS multiple advantages with respect to MRI (including cost, speed, and ease of examination), US should be a first-line screening investigation for occult SD and only those with an abnormal US should proceed to MRI. An exciting new development which will further improve the quality of US is the development of 3D US. The ability to retrieve multiplanar 3D images at any time should mean that for clinicians, 3D US will be as easily interpretable and therefore as acceptable as spinal MRI.
Nevertheless, many studies evidenced that MRI is the current “gold standard” test for detecting OSD but it should be performed in high-risk conditions, in markers association group, and when US is abnormal [10,11,12,13].
In our sample, we evidenced a difference between patients with LUS abnormalities and OSD confirmed after MRI. These results, in accordance with literature, demonstrated that MRI remains the gold standard because it has higher specificity and sensibility and because in LUS images could be some artifacts and sometimes it is operator dependent. However, the improvement in US instrumentation and the refinement of US techniques are making these differences particularly negligible in some low-risk conditions.
For our evidences and in accordance with previous study [9, 14, 21, 23, 24], we propose a clinical and radiological approach on the basis of number and characteristics of cutaneous markers. In newborns with neurological and/or orthopedic findings, we propose as soon as possible an investigation with MRI for high risk of OSD.
OSD is frequently associated with a combination of two or more different congenital midline lumbosacral lesions. It is important to detect these lesions in advance of any neurologic or orthopedic manifestations. Magnetic resonance imaging is the best radiologic imaging method; however, LUS may be used in some cases. A few isolated lesions are clearly associated with OSD: lipomas, dermal sinuses, and tails. In these patients, there is a high correlation with OSD and US has a poor sensibility and a high risk of false negative. In our sample, dermal sinus was at higher risk of OSD. Literature demonstrated that dermal sinus tract is an innocuous-appearing spinal dysraphism that may contribute to devastating morbidities if not timely addressed. In order to prevent complications, timely surgical intervention including complete resection of sinus tract with intradural exploration and correction of associated abnormalities is of utmost importance [25].
In patients with combination of less than two cutaneous stigmata, atypical dimple, and deviation of gluteal cleft, we propose to perform a LUS during the first month of life, and if anomalies are detected, MRI should be executed. In this group to start with, LUS is the best choice to reduce costs and to detect OSD. Abnormal LUS findings have poor sensitivity but good specificity at detecting anatomical findings consistent with OSD. Abnormal findings from LUS studies need to be confirmed with MRI studies, which may provide additional anatomical details relevant to surgical planning [2, 3, 9, 26].
In accordance with literature in others patients with sacral dimple alone, pigmentary nevus, and little hemangioma, we propose only a clinical follow-up and to perform a MRI only if there is an appearance of neurological or orthopedic alterations. In neonates with atypical dimple isolated, our group proposes to reassure parents and not perform MRI if LUS is normal and to continue only with a clinical follow-up.
Literature evidenced that these cutaneous stigmata are very common abnormalities of the skin and does not seem to be of pathologic significance and further investigation is not required [26,27,28]. These specific stigmata when present as a single marker are associated with a small incidence for associated neurologic infection or neurologic deterioration. Therapeutic evaluation may be limited to physical examination and clinical follow-up while same lesions, but in association with other well-defined cutaneous stigmata of OSD, warrant further radiographic and/or surgical inspection. The algorithm proposed in our study is resumed in Fig. 2.
The limitation of our study is that MRI was performed only in patients with abnormal US, because it is necessary a deep sedation to do this detection. Nevertheless, in patients that were not performed MRI, no any clinical signs suggesting a neurological involvement was detected during the follow up, except in one case.
Conclusions
In this prospective study, we propose a practical algorithm to detect occult spinal dysraphism in newborns with sacral dimple and/or cutaneous markers using lumbosacral ultrasonography examination and/or magnetic resonance imaging.
We propose MRI when patients have neurological or orthopedic impairment, more cutaneous stigmata, or specific markers as dermal sinus, human tail, and lipoma because of high risk of OSD.
Otherwise, in the case of atypical sacral dimple, deviated gluteal cleft, or association of two specific cutaneous markers, we suggest to perform US.
Lastly, in the presence of isolated sacral dimple, hypertrichosis, small hemangioma, and pigmentary nevus, which are linked to a very low risk of OSD, we propose only a clinical evaluation and a follow-up.
References
Sewell MJ, Pharm D, Chiu YE, Drolet BA (2015) Neural tube dysraphism: review of cutaneous markers and imaging. Pediatric Dermatology 32(n2):161–170
Chern J, Kirmakman BS, Shannon C, Tubbs S, Stone J (2012) Use of lumbar ultrasonograpghy to detect occult spinal dysraphism. J Neurosurg Pediatrics 9:274–279
Ben-Sira L, Ponger P, Miller E, Beni-Adani L, Constantini S (2009) Low-risk lumbar skin stigmata in infants: the role of ultrasound screening. J Pediatr 155(864–869):2
Ladino Torres MF, DiPietro MA (2014) Spine ultrasound imaging in the newborn. Semin Ultrasound CT MRI 35:652–661
Rozzelle CJ, Reed GT, Kirkman JL, Shannon CN, Chern JJ (2014) Sonographic determination of normal conus medullaris level and ascent in early infancy. Childs Nerv Syst 30:655–658
Schropp C, Sörensen N, Collmann H, Krauss J (2006) Cutaneous lesions in occult spinal dysraphism—correlation with intraspinal findings. Childs Nerv Syst 22:125–131
Unsinn KM, Geley T, Freund MC (2000) US of the spinal cord in newborns: spectrum of normal findings, variants, congenital anomalies and acquired diseases. Radiographies 20(4):923–938
Henriques JG, Pianetti G, Henriques KS, Costa P, Gusmão S (2005) Minor skin lesions as markers of occult spinal dysraphisms—prospective study. Surg Neurol 63(Suppl 1):S8–S12
Guggisberg D, Hadj-Rabia S, Viney C, Bodemer C, Brunelle F, Zerah M et al (2004) Skin markers of occult spinal dysraphism in children: a review of 54 cases. Arch Dermatol 140:1109–1115
Chern JJ, Aksut B, Kirkman JL, Shoja MM, Tubbs RS, Royal SA, Wellons JC 3rd, Rozzelle CJ (2012) The accuracy of abnormal lumbar sonography findings in detecting occult spinal dysraphism: a comparison with magnetic resonance imaging. J Neurosurg Pediatr 10(2):150–153
Kumar J, Afsal M, Garg A (2017) Imaging spectrum of spinal dysraphism on magnetic resonance: a pictorial review. World J Radiol 9(4):178–190
O'Neill BR, Gallegos D, Herron A, Palmer C, Stence NV, Hankinson TC, Corbett Wilkinson C, Handler MH (2017) Use of magnetic resonance imaging to detect occult spinal dysraphism in infants. J Neurosurg Pediatr 19(2):217–226
Dhingani DD, Boruah DK, Dutta HK, Gogoi RK (2016) Ultrasonography and magnetic resonance imaging evaluation of pediatric spinal anomalies. J Pediatr Neurosci 11(3):206–212
Inchingolo R, Maresca G, Cacaci S, Ausili E, Paolucci V, Bonomo L, Romagnoli C, Rendeli C (2013 Aug) Post-natal ultrasound morpho-dynamic evaluation of mild fetal hydronephrosis: a new management. Eur Rev Med Pharmacol Sci 17(16):2232–2239
McGovern M, Mulligan S, Carney O, Wall D, Moylett E (2013) Ultrasound investigation of sacral dimples and other stigmata of spinal dysraphism. Arch Dis Child 98:784–786
Fitzgerald K (2011) Ultrasound examination of neonatal Spine. Autralas J Ultrasound Med 14(1):39–41
Kriss VM, Desai NS (1998) Occult spinal dysraphism in neonates: assessment of high-risk cutaneous stigmata on sonography. AJR Am J Roentgenol 171:1687–1692
DiPietro MA (1993) The conus medullaris: normal US findings throughout childhood. Radiology 188(1):149–153
Hughes JA, De Bruyn R, Patel K, Thompson D (2003) Evaluation of spinal ultrasound in spinal dysraphism. Clin Radiol 58(227–233):5
Rendeli C, Ausili E, Tabacco F, Focarelli B, Massimi L, Caldarelli M, Tamburrini G, Di Rocco C (2007) Urodynamic evaluation in children with lipomeningocele: timing for neurosurgery, spinal cord tethering and followup. J Urol 177(6):2319–2324
Kucera J, Coley I, O’Hara S, Kosnik E, Coley BD (2015) The simple sacral dimple: diagnostic yield of ultrasound in neonates. Pediatr Radiol 45:211–216
Dick EA, de Bruyn R (2003) Ultrasound of the spinal cord in children: its role. Eur Radiol 13:552–562
Block SL (2014) The enigmatic sacro-coccygeal dimple: to ignore or explore? Pediatr Ann 43:95–100
Akira G (2013) Sacrococcygeal dimple: new classification and relationship with spinal lesions. Childs Nerv Syst 29:1641–1645
Robinson AJ, Russell S, Rimmer S (2005) The value of ultrasonic examination of the lumbar spine in infants with specific reference to cutaneous markers of occult spinal dysraphism. Clin Radiol 60:72–77
Weprin BE, Oakes WJ (2000) Coccygeal pits. Pediatrics 105(5):E69
Radmanesh F, Nejat F, El Khashab M (2010) Dermal sinus tract of the spine. Chlids Nerv Syst 26:349–357
Valentini LG, Selvaggio G, Erbetta A, Cordella R (2013) Occult spinal dysraphism: lessons learned by retrospective analysis of 149 surgical cases about natural history, surgical indications, urodynamic testing, and intraoperative neurophysiological monitoring. Childs Nerv Syst 29:1657–1669
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Rights and permissions
About this article
Cite this article
Ausili, E., Maresca, G., Massimi, L. et al. Occult spinal dysraphisms in newborns with skin markers: role of ultrasonography and magnetic resonance imaging. Childs Nerv Syst 34, 285–291 (2018). https://doi.org/10.1007/s00381-017-3638-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-017-3638-0