Abstract
Purpose
The aim of this study was to investigate the optimal age for starting cranial-remolding-orthosis therapy in children with deformational plagiocephaly.
Methods
Medical records of 310 patients with deformational plagiocephaly were retrospectively reviewed and the initial and final cranial vault asymmetry index (CVAI), age when starting therapy, duration of therapy, mean change of CVAI, improvement rate, and treatment success were analyzed. We compared outcomes according to the groups divided by ages starting therapy.
Results
There were no significant differences in improvement rate and duration of cranial-remolding-orthosis therapy among patients starting therapy at the age of 3, 4, and 5 months. However, when starting therapy after the age of 6 months, the rates of CVAI improvement were significantly lower and the duration of therapy was significantly increased.
Conclusion
Considering the spontaneous resolution effect according to the head growth nature, the age 5 month is the optimal period to start cranial-remolding-orthosis therapy for deformational plagiocephaly.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Deformational plagiocephaly refers to the misshaping of the infant’s head caused by extrinsic molding rather than intrinsic synostotic events [1]. It usually occurs through preferential head positioning during the first few months of life and is related to risk factors such as assisted delivery, firstborn child, prematurity, neck problems, male sex, larger cerebrospinal fluid spaces, and spending >20 h in the supine position each day [2]. Many studies suggest that infants with deformational plagiocephaly may develop facial asymmetry, especially ipsilateral occipital flattening, protrusion of ipsilateral frontal bone, and anterior displacement of the ipsilateral ear [3, 4]. Furthermore, these malformations can affect the child psychologically and cause distress to parents [5]. Therefore, identifying and appropriately managing infants with cranial asymmetry is important to minimize the facial asymmetry and psychological impact of patients and their caregivers [6,7,8].
Treatments for deformational plagiocephaly include observation, head-repositioning therapy, physical therapy, external orthotics, and surgery. Among these, cranial-remolding-orthosis (helmet) therapy has become widespread because it is believed to be safe with no reported harmful effects on cranial growth [1]. The indications to start the cranial-remolding-orthosis therapy are considered the patients who failed sufficient improvement of cranial asymmetry after conservative care such as positioning therapy or physical therapy [9]. However, considering the nature recovery period and timing of conservative therapeutic effect, optimal age for starting cranial-remolding-orthosis therapy remains controversial. There have been some reports of the inverse correlation between the rate of correction of cranial asymmetry and the starting age of cranial-remolding-orthosis therapy [10,11,12]. However, other authors have found no such correlation [13]. Therefore, for patients with deformational plagiocephaly that requires cranial-remolding-orthosis therapy, we sought to elucidate the optimal age to begin treatment, to avoid excessive and unnecessarily early treatment. The aim of this study was to evaluate the effectiveness of cranial-remolding-orthosis therapy according to the age of starting treatment to determine the optimal age at which therapy should begin.
Materials and methods
We obtained the records of patients who underwent cranial-remolding-orthosis therapy for cranial deformities between 2010 and 2016. Parents were instructed to keep their child in the cranial-remolding orthosis for as long as possible, with use recommended for 23.5 h/day and at least 20 h/day. In the present study, patients with regular follow-up for whom compliance could be checked by physicians were included. The termination of treatment was decided by the treating physician based on a satisfactory change of the cranial asymmetry, patient tolerance, and parental satisfaction. Before starting cranial-remolding-orthosis therapy, every child underwent three-dimensional (3D) head surface scanning (STARscanner™ Laser Data Acquisition System; Orthomerica Products, Orlando, FL, USA). Each patient received a customized cranial-remolding orthotic consisting of a polyethylene foam liner and a copolymer outer shell. Follow-up laser scans were performed every 3–4 weeks to adjust for head growth and changes in skull shape. The inclusion criteria for this study were infants who completed the recommended cranial-remolding-orthosis treatment with regular monthly follow-up. A total of 349 patients underwent cranial-remolding-orthosis therapy for cranial deformities between 2010 and 2016. Of these, 31 patients did not complete cranial-remolding-orthosis therapy for recommended time of day or failed to follow up on a regular basis. Three patients with genetic disorders such as Down’s syndrome were excluded. In addition, other causes of developmental delay such as cerebral palsy (3 patients) and postoperative conditions (2 patients) were excluded.
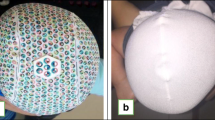
For this study, we retrospectively analyzed the age at which cranial-remolding-orthosis therapy was started, duration of treatment, initial and final cranial vault asymmetry indices (CVAIs, %), change value and improvement rate of CVAI, and treatment success. Anthropometric measurements were obtained at the beginning and end of therapy using the STARscanner™ device. The cranial diagonal measurement was obtained according to the method of Plank et al. [14]. First, a cross-sectional plane through the sellion and both tragions was designated as the level 0 plane. The overall height of the child’s head above 0 plane divided into 10 equally spaced cross-sectional planes, with each plane being parallel to the reference plane (Fig. 1a). The cranial diagonal was finally obtained at the level 3 plane and defined as the cranial diameter 30° from the line connecting the sellion and origin (the midpoint between the right and left tragion) (Fig. 1b). CVAI was used to represent the individual asymmetry of the cranial vault and was calculated as follows: CVAI (%) = ([difference between cranial diagonals/shorter cranial diagonal] × 100). The change of CVAI was the difference between initial and final CVAI and the improvement rate of CVAI was calculated as follows: difference between initial and final CVAI/initial CVAI. Treatment success was evaluated by cutoff points: a final CVAI of ≤3.5% [15]. Loveday and De defined a CVAI 0% as a perfect symmetrical infant’s skull and considered up to 3.5% as a higher value represents significant asymmetry [15].
How the cranial diagonal was obtained using cross-sectional planes. a The sellion is the deepest point of the nasofrontal angle between the forehead slope and proximal nasal bridge. The tragion is in the notch just above the tragus of the ear. b The origin is the midpoint between the right and left tragion. The Y-axis is defined as the line through the sellion and origin, and the X-axis is defined as the line perpendicular to the Y-axis that crosses the origin. The difference in the cranial diagonal diameters is the difference between the longest diagonal and the shortest diagonal (i.e., AB-CD). The cranial vault asymmetry index (%) was calculated as [(AB-CD)/CD] × 100. XXXX® provided this photo for the present report
Data analysis was performed using PASW Statistics, Version 18.0 (SPSS, Inc., Chicago, IL, USA). The initial and final CVAIs were compared using paired t tests. The duration of cranial-remolding-orthosis therapy and improvement rate of CVAI were analyzed for each group using one-way analysis of variance with post hoc Bonferroni procedure. Treatment success rates were compared for each group using chi-squared tests. Statistical significance was set at a p value of <0.05.
Results
We obtained the records of 310 patients who met the inclusion criteria (187 boys and 123 girls) and the mean age at the start of cranial-remolding-orthosis therapy was 184.3 ± 65.7 days. The initial severity of plagiocephaly was categorized by CVAI as mild group (range, 3.5–7%, n = 47), moderate group (range, 7–12%, n = 203) and severe group (range, >12%, n = 60), and this did not significantly differ between the study groups [15]. A total of 310 patients were classified according to initiation age (month; M) of cranial-remolding-orthosis therapy: 3M (<120 days, n = 42), 4M (120–149 days, n = 64), 5M (150–179 days, n = 66), 6M (180–209 days, n = 56), 7M (210–239 days, n = 32), 8M (240–269 days, n = 21), and 9M (≥270 days, n = 29). Table 1 summarizes these baseline characteristics of patients.
The mean duration of cranial-remolding-orthosis therapy was 165.3 ± 65.9 days (range, 99.4–231.2). The mean CVAI before cranial-remolding-orthosis therapy was 9.7% (range, 6.9–12.5%) and the mean CVAI at the end of therapy was 4.0% (range, 2.1–5.9%). A reduction in head asymmetry was observed in all groups and the mean reduction value of CVAI was 5.7 ± 2.0% (range, 3.7–7.7%). The mean improvement rate 59.6 ± 13.6% (range, 46.0–73.2%) and the mean success rate, using the cutoff value of CVAI of ≤3.5%, was 43.0% (range, 14–55%) [15].
The mean CVAI change was the greatest in group 3M from initial to final CVAI of 10.4 to 3.5%. In contrast, the mean CVAI change was the shortest in group 9M from initial to final CVAI of 9.8 to 5.7%. The mean CVAI change was significantly lower in group 6, 7, 8, and 9M than group 3M (p = 0.001, p < 0.05, p < 0.05, and p < 0.001) but, there were no significant differences in mean CVAI change among groups 3, 4, and 5M (6.9, 6.3, and 5.9%) (Table 2, Fig. 2).
The mean CVAI improvement rate was the greatest in group 3M (67.9%) and was the lowest in group 9M (43.4%). Group 3M showed significantly higher CVAI improvement rate than groups 6, 7, 8, and 9M (p < 0.05, p < 0.001, p < 0.001, and p < 0.001). However, there were no significant differences in mean CVAI improvement rate among groups 3, 4, and 5M (67.9, 62.3, and 63.0%) (Table 2, Fig. 3) The treatment success rate of each group, defined as CVAI ≤3.5% was the greatest in group 3M (55%) [15]. The success rates of 4, 5, 6, and 7M groups showed similar success rates (44, 48, 48, and 44%) but after 8 months, success rate was decreased below 20%. However, there were no significant intergroup differences in treatment success rates among groups.
The mean duration of cranial-remolding-orthosis therapy was the shortest in group 3M (124.0 days) and the longest in group 8M (222.0 days). There were no significant differences in the mean duration of therapy among groups 3, 4, and 5M, but group 3M showed a significantly shorter duration of treatment than groups 6, 7, 8, and 9M (p < 0.001, p < 0.001, p < 0.001, and p = 0.004). (Table 2 and Fig. 4).
Discussion
In this study, we evaluated the effects of cranial-remolding-orthosis therapy by using final CVAI. Compared to other measurement parameters such as cranial index, orbitotragial depth asymmetry, and cranial base asymmetry, CVAI is easy to measure and can be evaluated independently of the head size; furthermore, it provides accurate, reproducible comparison among subjects [15, 16]. In the present study, we found that the reduction value of CVAI and the rates of CVAI improvements were not significantly different among children treated between the ages of 3 and 5 months. However, when starting therapy after age 6 months, the change of CVAI and rates of CVAI improvement were significantly lower. Similarly, the duration of cranial-remolding-orthosis therapy was not significantly different between the ages of 3 and 5 months but significantly increased after age 6 months. Overall, our results indicate that the effectiveness of cranial-remolding-orthosis therapy differed according to the age at which treatment was started, with a notable benefit when starting age was between 3 and 5 months.
Cranial-remolding-orthosis therapy for children with deformational plagiocephaly was first introduced by Clarren et al. in 1979 and has undergone substantial advances. Currently, cranial-remolding orthotics for deformational plagiocephaly are custom-made by 3D head surface laser or 3D computed tomography scanning [17]. There are some reports of complications related to cranial-remolding-orthosis therapy, such as skin rashes augmented sweating, unpleasant odor, pain, and expensive cost [18,19,20,21,22]. Despite these disadvantages, cranial-remolding-orthosis therapy has been used widely because of superior effect for correcting cranial asymmetry. Yim et al. compared cranial-remolding-orthosis therapy with repositioning therapy in moderate to severe deformational plagiocephaly and found that patients treated with cranial-remolding-orthosis therapy had greater improvement of cranial and ear asymmetry than those treated with repositioning therapy [23]. Likewise, a retrospective cohort study of 298 infants treated for deformational plagiocephaly reported that cranial-remolding-orthosis therapy was significantly more effective than repositioning therapy in decreasing the diagonal difference [10]. Finally, a systematic review reported that cranial-remolding-orthosis therapy was 1.3 times more effective to repositioning therapy at achieving good outcomes [24].
Despite the known effectiveness of cranial-remolding-orthosis therapy, controversy still exists regarding the optimal treatment regimen and starting age. A prospective study of 36 infants where cranial-remolding-orthosis therapy was started at different ages found that there was no significant relationship between age and percentage change in cranial asymmetry [13]. However, many other studies have showed correlation between the optimal age to start and the effectiveness of cranial-remolding-orthosis therapy, Graham et al. reported that starting cranial-remolding-orthosis therapy before the age of 8 months was significantly more effective [10]. Furthermore, Freudlsperger et al. reported that cranial-remolding-orthosis therapy should be initiated within 25 weeks of birth, the youngest of the proposed periods [15]. Yasuo Aihara et al. documented that treatment was effective when started at age 4 months in the severe deformation group and at age 6 months in the mild deformation group [5]. In addition, Kluba et al. showed that infants younger than 6 months had significant better outcomes and proposed that the optimal age for starting cranial-remolding-orthosis therapy was 5–6 months [11]. Generally, most studies proposed that the optimal age for starting therapy was before 6 months, no longer than 12 months and suggested that the earlier treatment could bring the better outcome of cranial-remolding-orthosis therapy.
The previous studies analyzed the therapeutic effect of cranial-remolding-orthosis therapy using the absolute change of CVAI values [5, 9, 15, 16]; however, the change in CVAI has limit that cannot reflect the initial severity of plagiocephaly. We further calculated the CVAI improvement rate based on the patient’s initial CVAI value and analyzed the accurate therapeutic effects of cranial-remolding-orthosis therapy [25]. Further analysis of the mean CVAI improvement rate among groups showed that the group 3M showed significantly better results than the 6, 7, 8, and 9M groups. In addition, there were no significant differences among groups 3, 4, and 5M. Compared to previous studies, we further subdivided patients according to specific age in months and evaluated their parameters. Most studies suggesting that the best time to start cranial-remolding-orthosis therapy is 6 months, divided their patients into 3 or 4 groups based on 6–7 months [9, 15, 16]. However, our study subdivided patient’s age by month and more specific age with better effect of cranial-remolding-orthosis treatment.
The success of cranial-remolding-orthosis therapy relies on the potential for brain growth to redirect head shape [17, 26]. The brain grows to 200% of its birth size by age 6 months and increases in size by only an additional 50% over the next 24 months. By age 2 years, the brain is approximately 70% of its adult size, and the remaining growth occurs slowly over the next 4 years. Regarding the treatment interval of cranial-remolding-orthosis therapy, Clarren et al. described that older infants required longer treatment periods because of physiologic deceleration in brain growth [17]. Furthermore, Dorhage et al. conducted the follow-up study of 102 children with cranial asymmetry and reported that the treatment effects of cranial-remolding-orthosis therapy are shown after 75 days and the treatment longer than 150 days did not show any meaningful improvement in the change of CVAI [9]. In our study, groups 6, 7, 8, and 9M showed a significantly longer duration of treatment than 3M and these groups were above 150 days, respectively. It is difficult to achieve a satisfactory change in skull asymmetry in children aged 6 months or longer, which require longer time to compensate for increased head growth and malformations. Considering period effects of cranial-remolding-orthosis therapy, we concluded that the cranial-remolding-orthosis therapy should be started at least 5 months age to achieve the meaningful therapeutic effects.
Because of trend toward spontaneous improvement of cranial asymmetry and therapeutic effect of conservative management, several reports have recommended that cranial-remolding-orthosis therapy be delayed until after 6 months, when options such as repositioning and physical therapies have failed [18, 27]. This approach may be appropriate given our findings. There were no significant differences in the CVAI improvement and duration of therapy among children younger than 5 months. However, after 6 months, the CVAI improvement rates of cranial-remolding-orthosis therapy were significantly reduced and the duration of therapy was significantly longer. Therefore, in deformational plagiocephaly, close observation and conservative therapy could be applied until infants reach age 5 months. If deformational plagiocephaly fails to improve over this time, cranial-remolding-orthosis therapy should be considered to achieve the maximal therapeutic benefit over the shortest treatment time.
Our study has some limitations. First, because of the retrospective design, the severity of plagiocephaly and the numbers of patients were unevenly distributed among the age groups. Second, treatment termination was not determined by strict criteria; therefore, some patients continued treatment despite achievement of treatment success because they were not satisfied with the outcome. In the evaluation of treatment duration, patients of group 9M showed shorter treatment periods than those of groups 6, 7, and 8M. We estimated this result might be due to the adherence to the treatment. In our study, group 9M was the subjects older than 9M and their compliance of helmet therapy was poor because of their ability to take off their helmet. This caused an unexpected early termination of therapy and made the shorter duration of treatment in group 9M. Third, we did not evaluate treatment compliance. However, the patients were instructed to ensure that the orthotic was worn for 23.5 h/day, and physicians checked the compliance regularly. Fourth, there was a chance of regression after the orthosis was discontinued in any of the groups, but we could not extend follow-up because of the retrospective study design. There was one study with approximately 5 years of follow-up treatment of the effectiveness of molding cranial-remolding-orthosis therapy reported that cranial vault asymmetry appeared to regress, but the regression was not statistically meaningful [28]. Head growth and cranial base resistance after the completion of cranial-remolding-orthosis therapy could be the reason for the small amount of regression in cranial vault and base asymmetries [27]. There are many factors that can affect the follow-up results of cranial-remolding-orthosis therapy, and the reasons for regression after completion of therapy are not clear. Further studies about ongoing effectiveness of cranial-remolding-orthosis therapy are needed.
Conclusions
We found that starting cranial-remolding-orthosis therapy after age 6 months was associated with longer duration of treatment. In addition, starting therapy after age 6 months was associated with decreased rates of CVAI improvement. Thus, our results suggest that cranial-remolding-orthosis therapy provides optimal outcomes when started age 5 months with respect to treatment effectiveness. Considering the spontaneous resolution effect according to the head growth nature, the 5 months appears to be the optimal period for starting cranial-remolding-orthosis therapy for deformational plagiocephaly.
References
Kelly KM, Littlefield TR, Pomatto JK, Manwaring KH, Beals SP (1999) Cranial growth unrestricted during treatment of deformational plagiocephaly. Pediatr Neurosurg 30:193–199. doi: 28794
Bialocerkowski AE, Vladusic SL, Wei Ng C (2008) Prevalence, risk factors, and natural history of positional plagiocephaly: a systematic review. Dev Med Child Neurol 50:577–586. doi:10.1111/j.1469-8749.2008.03029.x
Looman WS, Flannery AB (2012) Evidence-based care of the child with deformational plagiocephaly, part I: assessment and diagnosis. J Pediatr Health Care 26:242–250; quiz 251-243. doi:10.1016/j.pedhc.2011.10.003
Mortenson P, Steinbok P, Smith D (2012) Deformational plagiocephaly and orthotic treatment: indications and limitations. Childs Nerv Syst 28:1407–1412. doi:10.1007/s00381-012-1755-3
Aihara Y, Komatsu K, Dairoku H, Kubo O, Hori T, Okada Y (2014) Cranial molding helmet therapy and establishment of practical criteria for management in Asian infant positional head deformity. Childs Nerv Syst 30:1499–1509. doi:10.1007/s00381-014-2471-y
Speltz ML, Collett BR, Stott-Miller M, Starr JR, Heike C, Wolfram-Aduan AM, King D, Cunningham ML (2010) Case-control study of neurodevelopment in deformational plagiocephaly. Pediatrics 125:e537–542. doi:10.1542/peds.2009-0052
Collett BR, Gray KE, Starr JR, Heike CL, Cunningham ML, Speltz ML (2013) Development at age 36 months in children with deformational plagiocephaly. Pediatrics 131:e109–e115. doi:10.1542/peds.2012-1779
Cabrera-Martos I, Valenza MC, Valenza-Demet G, Benitez-Feliponi A, Robles-Vizcaino C, Ruiz-Extremera A (2016) Effects of manual therapy on treatment duration and motor development in infants with severe nonsynostotic plagiocephaly: a randomised controlled pilot study. Childs Nerv Syst 32:2211–2217. doi:10.1007/s00381-016-3200-5
Dorhage KW, Beck-Broichsitter BE, von Grabe V, Sonntag A, Becker ST, Wiltfang J (2016) Therapy effects of head orthoses in positional plagiocephaly. J Craniomaxillofac Surg 44:1508–1514. doi:10.1016/j.jcms.2016.06.035
Graham JM Jr, Gomez M, Halberg A, Earl DL, Kreutzman JT, Cui J, Guo X (2005) Management of deformational plagiocephaly: repositioning versus orthotic therapy. J Pediatr 146:258–262. doi:10.1016/j.jpeds.2004.10.016
Kluba S, Kraut W, Reinert S, Krimmel M (2011) What is the optimal time to start helmet therapy in positional plagiocephaly? Plast Reconstr Surg 128:492–498. doi:10.1097/PRS.0b013e31821b62d6
Thompson JT, David LR, Wood B, Argenta A, Simpson J, Argenta LC (2009) Outcome analysis of helmet therapy for positional plagiocephaly using a three-dimensional surface scanning laser. J Craniofac Surg 20:362–365. doi:10.1097/SCS.0b013e3181992382
Mulliken JB, Vander Woude DL, Hansen M, LaBrie RA, Scott RM (1999) Analysis of posterior plagiocephaly: deformational versus synostotic. Plast Reconstr Surg 103:371–380
Plank LH, Giavedoni B, Lombardo JR, Geil MD, Reisner A (2006) Comparison of infant head shape changes in deformational plagiocephaly following treatment with a cranial remolding orthosis using a noninvasive laser shape digitizer. J Craniofac Surg 17:1084–1091. doi:10.1097/01.scs.0000244920.07383.85
Freudlsperger C, Steinmacher S, Saure D, Bodem JP, Kuhle R, Hoffmann J, Engel M (2016) Impact of severity and therapy onset on helmet therapy in positional plagiocephaly. J Craniomaxillofac Surg 44:110–115. doi:10.1016/j.jcms.2015.11.016
Yoo HS, Rah DK, Kim YO (2012) Outcome analysis of cranial molding therapy in nonsynostotic plagiocephaly. Arch Plast Surg 39:338–344. doi:10.5999/aps.2012.39.4.338
Clarren SK, Smith DW, Hanson JW (1979) Helmet treatment for plagiocephaly and congenital muscular torticollis. J Pediatr 94:43–46
Loveday BP, de Chalain TB (2001) Active counterpositioning or orthotic device to treat positional plagiocephaly? J Craniofac Surg 12:308–313
Clarren SK (1981) Plagiocephaly and torticollis: etiology, natural history, and helmet treatment. J Pediatr 98:92–95
Littlefield TR (2001) Food and Drug Administration regulation of orthotic cranioplasty. Cleft Palate Craniofac J 38:337–340. doi:10.1597/1545-1569(2001)038<0337:fadaro>2.0.co;2
van Wijk RM, van Vlimmeren LA, Groothuis-Oudshoorn CG, Van der Ploeg CP, Ijzerman MJ, Boere-Boonekamp MM (2014) Helmet therapy in infants with positional skull deformation: randomised controlled trial. Bmj 348:g2741. doi:10.1136/bmj.g2741
Bruner TW, David LR, Gage HD, Argenta LC (2004) Objective outcome analysis of soft shell helmet therapy in the treatment of deformational plagiocephaly. J Craniofac Surg 15:643–650
Kim SY, Park MS, Yang JI, Yim SY (2013) Comparison of helmet therapy and counter positioning for deformational plagiocephaly. Ann Rehabil Med 37:785–795. doi:10.5535/arm.2013.37.6.785
Xia JJ, Kennedy KA, Teichgraeber JF, Wu KQ, Baumgartner JB, Gateno J (2008) Nonsurgical treatment of deformational plagiocephaly: a systematic review. Arch Pediatr Adolesc Med 162:719–727. doi:10.1001/archpedi.162.8.719
Kluba S, Kraut W, Calgeer B, Reinert S, Krimmel M (2014) Treatment of positional plagiocephaly--helmet or no helmet? J Craniomaxillofac Surg 42:683–688. doi:10.1016/j.jcms.2013.09.015
Miller RI, Clarren SK (2000) Long-term developmental outcomes in patients with deformational plagiocephaly. Pediatrics 105:E26
Robinson S, Proctor M (2009) Diagnosis and management of deformational plagiocephaly. J Neurosurg Pediatr 3:284–295. doi:10.3171/2009.1.peds08330
Lee RP, Teichgraeber JF, Baumgartner JE, Waller AL, English JD, Lasky RE, Miller CC, Gateno J, Xia JJ (2008) Long-term treatment effectiveness of molding helmet therapy in the correction of posterior deformational plagiocephaly: a five-year follow-up. Cleft Palate Craniofac J 45:240–245. doi:10.1597/06-210.1
Acknowledgments
We appreciate Orthokorea® that provided data for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Mi-hyang Han: No conflict of interest to disclose. Jin Young Kang: No conflict of interest to disclose. Hye Young Han: No conflict of interest to disclose. Yun-hwa Cho: No conflict of interest to disclose. Dae-Hyun Jang: No conflict of interest to disclose.
Rights and permissions
About this article
Cite this article
Han, Mh., Kang, J.Y., Han, H.Y. et al. Relationship between starting age of cranial-remolding-orthosis therapy and effectiveness of treatment in children with deformational plagiocephaly. Childs Nerv Syst 33, 1349–1356 (2017). https://doi.org/10.1007/s00381-017-3427-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-017-3427-9