Abstract
Hypertrophic cardiomyopathy (HCM) patients with nonvalvular atrial fibrillation (AF) have an increased risk of suffering thromboembolic events. Vitamin K antagonists (VKA) are recommended as therapy but there is still limited data regarding the efficacy of prescribing non-vitamin K antagonist oral anticoagulants (NOACs). This retrospective study investigates the effectiveness and safety of NOAC administration in patients with HCM and AF. A total of 124 patients with HCM and AF on an oral anticoagulant therapy were recruited between January 2015 and December 2019; these patients were followed up until March 31, 2020. Kaplan–Meier analysis was used to compare the clinical outcomes in patients treated with NOACs versus warfarin. The Cox model was used to estimate the risk of clinically relevant bleeding. Our study included 124 patients, of which 48 (38.7%) received warfarin and 76 (61.3%) received NOACs. Survival analysis showed the patients undergoing NOACs had a lower risk of clinically relevant bleeding (log-rank P = 0.039) over a period of 53.6 months. The median time in therapeutic range (TTR) score was 50% (interquartile range: 40.43 to 57.08%). A total of nine patients (18.75%) had a good TTR with a median score of 66.35% (interquartile range: 64.58 to 77.75%). The incidence of death by all causes, cardiovascular death and thromboembolism were similar between NOAC and warfarin-treated patients (log-rank P = 0.239, log-rank P = 0.386, and log-rank P = 0.257, respectively). Patients treated with NOACs showed a significant reduction in the risk of clinical (P = 0.011) and gastrointestinal bleeding (P = 0.032). Cox multiple regression analysis showed age (HR 1.13, 95% CI 1.03–1.24; P = 0.013) and warfarin therapy (HR 7.37, 95% CI 1.63‐33.36; P = 0.010) were independent predictors of clinically relevant bleeding. Compared to warfarin, NOACs were associated with a lower incidence of clinically relevant bleeding in HCM patients with AF, as demonstrated by the similar incidence of death by all causes, cardiovascular death and thromboembolic events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertrophic cardiomyopathy (HCM) is a type of primary cardiomyopathy characterized by increased myocardial weight and asymmetric left ventricular hypertrophy, which eventually leads to heart failure and arrhythmia. Atrial fibrillation (AF) is the most common type of arrhythmia in HCM, and leads to a higher risk of stroke, transient ischemic attack (TIA) and systemic embolism [1]. According to the 2011 guidelines of the AHA / ACC /HRS and the 2014 ESC guidelines, patients presenting with HCM and AF and no contraindications should be treated with the anticoagulant warfarin, irrespective of the CHA2DS2-VASc risk score [2, 3]. However, there are several limitations in the clinical use of warfarin, including the need to regularly monitor the international standardized ratio (INR) and adjust the dose. In addition, there often exists a narrow treatment window, and interactions with several other drugs or food. Because of these limitations, non-vitamin K antagonist oral anticoagulants (NOACs) may constitute a more reasonable therapeutic alternative to warfarin in these patients [4, 5].
Specifically, NOACs represent an improvement in the safety profile of anticoagulant treatment in the prevention of thromboembolic events in AF patients, as demonstrated by several trials showing these drugs perform better than vitamin K antagonists (VKA) in preventing stroke or thromboembolic events, while also reducing the risk of intracranial bleeding [6,7,8,9]. Patients with HCM are often younger and do not usually have typical risk factors for embolization. As a result, very few HCM patients have been included in NOACs trials, leading to a lack of data on the safety and effectiveness of using NOACs to treat these patients.
Nevertheless, the results of some observational studies provide a reference for the safety of NOACs and VKA administration in HCM patients with AF. By using data from the US Insurance database, Noseworthy et al. [10] showed the incidence of thromboembolic events was similar in HCM patients with AF treated with either NOACs or warfarin after 0.56 years. Furthermore, NOACs were associated with a lower incidence of intracranial and major bleeding. Considering the lack of clinical, biochemical and echocardiographic data in previous studies using insurance databases, we conducted a single-center retrospective study to compare the clinical characteristics, thromboembolic events, major bleeding episodes, cardiovascular and all-cause death in HCM-AF patients treated with NOACs versus VKA.
Methods
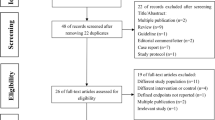
We included 124 HCM-AF patients who received anticoagulant therapy with either NOACs or warfarin between January 2015 and December 2019. The date of inclusion in the study corresponded to the first prescription of warfarin or NOACs. If the treatment was changed from warfarin to NOACs or vice versa, the date when the last oral anticoagulant was used was considered. The final follow-up evaluation was completed on March 31, 2020. All patients included were adults (age ≥ 18 years old). Exclusion criteria included anticoagulation therapy for less than 3 months, incomplete INR records, valvular heart disease, mechanical heart valves, and hospital admission in the month prior to the interview. Demographic and clinical data were obtained by in-person interviews, telephone interviews, hospital records, and electronic INR records. This study was approved by the Ethics Committee of the First Affiliated Hospital of Fujian Medical University (MTCA, ECFAH of FMU 2015 NO.084). Informed consent was obtained from all patients before recruitment.
HCM diagnosis was based on the presence of significant left ventricular hypertrophy on two-dimensional echocardiography that was not explained solely by loading conditions (such as hypertension, valvular disease, and congenital heart) [1, 2]. The echocardiographic criteria included a maximum left ventricular wall thickness of ≥ 15 mm, or ≥ 13 mm in patients with a family history of HCM; and a ratio between the maximum left ventricular wall thickness and the posterior left ventricular wall thickness (MWT/LVPWT) > 1.3 ~ 1.5. AF diagnosis was based on electrocardiographic recordings. Paroxysmal AF was defined as self‐terminating usually within 48 h. Persistent AF, including long-standing persistent AF, was defined by the presence of AF episodes lasting longer than 7 days [11].
Selected patients were aged between 18 and 85 years old (at initial admission). Demographic information, including age and gender, comorbidities, systolic and diastolic blood pressure, heart rate, biochemical parameters were collected by consulting electronic medical records. The comorbidities considered included parameters of the CHA2DS2-VASc and HAS-BLED scores, in particular congestive cardiac failure, hypertension, diabetes mellitus, stroke/TIA/thromboembolism history, vascular disease, and abnormal renal/liver function [12].
During follow-up, death by all causes was defined as death associated with any cause, while cardiovascular death was specifically defined as death due to cardiovascular disease. Thromboembolic events included episodes of ischemic stroke, TIA, left atrial thrombosis, or peripheral embolism. Ischemic stroke was defined as a sudden focal neurologic deficit caused by ischemia, lasting more than 24 h. TIA was defined as a focal neurologic deficit lasting less than 24 h. Peripheral embolism was defined as an acute vascular obstruction of the limbs or organs. According to the International Society on Thrombosis and Hemostasis, major bleeding events or clinically relevant non-major bleeding were defined as clinically relevant bleeding [13, 14]. Major bleeding was defined as a reduction in hemoglobin levels of at least 2 g/dL, transfusion of at least 2 units of packed red blood cells, or symptomatic bleeding at a critical site (intracranial, intraocular, intraspinal, intra-articular, intramuscular with compartment syndrome, pericardial, or retroperitoneal), or death. Clinically relevant non-major bleeding was defined as clinically significant bleeding that did not satisfy the criteria of major bleeding, but led to hospital admission or medical or surgical treatment. After discharge, patients were followed up in the outpatient clinic or by telephone. If death by all causes or cardiovascular death occurred, the exact date was obtained from relatives or medical reports. The clinical endpoints were death by all causes, cardiovascular death, thromboembolic events, and major or clinically relevant bleeding. Survival time was defined as the period of time between the initial admission and the date of the clinical endpoint or last follow-up interview.
Statistical analysis was performed using SPSS version 22.0. Continuous variables were expressed as the median (interquartile range), and categorical variables were expressed as percentages. A Mann–Whitney U test was used for comparing continuous variables between two groups, whereas the chi-square test was used for categorical variables. Multivariate statistical analyses were performed using the Cox proportional hazard regression model through the "Backward LR" method. The time until the manifestation of the clinical endpoint events was analyzed using the Kaplan–Meier method. A P value < 0.05 was considered as statistically significant.
Results
The baseline characteristics of 124 HCM-AF patients are provided in Table 1. VKA was prescribed in 38.7% (n = 48) and NOACs in 61.3% (n = 76) of patients. A total of 42 patients received rivaroxaban (55.3%) and 34 received dabigatran (44.7%). In the NOACs group, 63 patients (82.9%) started using NOACs from the beginning of the anticoagulant treatment. There were only 13 NOAC-treated patients (17.1%) who converted from the VKA treatment (in 8 of these patients, monitoring the INR was inconvenient), and 5 of these patients suffered from bleeding under the VKA treatment). In patients with AF, paroxysmal and persistent AF accounted for 42.7% and 57.3% of cases, respectively.
More than 40.8% of patients in the NOACs group were males, compared to 35.4% in the VKA group (p = 0.891). The average age at the beginning of treatment was similar in the NOACs and VKA groups (P = 0.243). Both groups were also comparable in terms of clinical complications, including previous ischemic stroke/TIA (P = 0.913), previous myocardial infarction (MI) (P = 0.374), hypertension (P = 0.405), diabetes (P = 0.113), peripheral vascular disease (P = 0.782), heart failure (P = 0.668), chronic kidney disease (P = 0.534), liver disease (P = 0.960), and non-sustained ventricular tachycardia (VT) (P = 0.603). The use of concomitant antiplatelet therapy was higher in the VKA (16.7%) vs. NOAC group (7.9%), although the difference was not statistically significant (p = 0.133). As shown in Table 2, there were no significant differences between both groups in most clinical and echocardiographic characteristics.
The time in therapeutic range (TTR) is defined as the percentage of time the patient’s INR is within the target therapeutic range (between 2.0 and 3.0) [15]. There were a total of 48 patients receiving warfarin. TTR was calculated for patients who had at least two INR values, which excludes the INR readings of the first six weeks following initial warfarin treatment. An adequate TTR recommended for warfarin therapy ranges between 58 and 65%, with the optimal control reached above 70% [16]. In our study, we defined a good TTR at 60%. The median TTR score was 50% (interquartile range: 40.43 to 57.08%) during the 53.6 months of the study period; a total of nine patients (18.75%) had a good TTR with a median score of 66.35% (interquartile range: 64.58 to 77.75%).
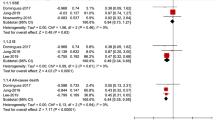
The average follow-up time, from the start of anticoagulation treatment to the final follow-up interview, was 53.6 ± 2.0 months (55.0 ± 2.6 months in the NOACs group and 51.1 ± 3.2 months in the VKA group). In the Kaplan–Meier analysis (Fig. 1), the risk of clinically relevant bleeding was significantly lower in patients treated with NOACs compared to those treated with warfarin (log-rank P = 0.039). The incidence of death by all causes (log-rank P = 0.239), cardiovascular death (log-rank P = 0.386), and thromboembolic events (log-rank P = 0.257) was comparable between the two groups.
Kaplan–Meier curves for the cumulative incidences of clinically relevant bleeding in HCM patients with AF between NOACs- and warfarin-treated group. NOACs non-vitamin K antagonist oral anticoagulant; A Death from all cause; B Clinically relevant bleeding; C Thromboembolic events; and D Cardiovascular death
We enrolled a total of 124 patients in this study. Of these, three patients were lost to follow-up, and 27 patients died (12 of which due to cardiovascular problems, Table 3). In the NOACs group, 4 patients suffered thromboembolic events (of which 2 suffered ischemic stroke, 1 suffered from lower limb arterial embolism, and 1 had atrial thrombosis). One case of atrial thrombosis also occurred in the warfarin group. The risk of death by all causes, cardiovascular death, or thromboembolic events was similar between the NOAC and warfarin groups. In HCM-AF patients receiving NOACs and warfarin, the incidence of clinically relevant bleeding was 3.9% (3 out of 76) and 18.8% (9 out of 48), respectively. NOACs users showed a significant reduction in the risk of clinically relevant bleeding (P = 0.011) and gastrointestinal bleeding (P = 0.032).
As shown in the univariate analysis of Table 4, the factors age (HR 1.08, 95% CI 1.00–1.17; P = 0.034) and warfarin treatment (HR 5.07, 95%CI 1.31–19.67; P = 0.019) were significantly associated with clinically relevant bleeding events. We included several parameters of the HAS-BLED score, such as gender, hypertension, diabetes, previous ischemic stroke / TIA, chronic liver disease, chronic kidney disease, antiplatelet therapy (aspirin and/or clopidogrel) and INR, in the Cox multivariate regression analysis along with age and warfarin treatment. In this analysis, age (HR 1.13, 95% CI 1.03–1.24; P = 0.013) and warfarin treatment (HR 7.37, 95% CI 1.63–33.36; P = 0.010) were also independent predictors of bleeding events.
The different NOACs subgroups (receiving dabigatran and rivaroxaban, respectively) did not present statistically significant differences in the amount of death by all causes, cardiovascular death, thromboembolic events, or clinically relevant bleeding. A total of 2 deaths from cardiovascular causes and 1 death from non-cardiovascular causes occurred in the rivaroxaban group, along with 4 deaths from cardiovascular causes in the dabigatran group. The COX multivariate regression indicated that age (P = 0.011) was an independent predictor of bleeding events. In the subgroup analysis, there was no statistically significant difference in clinically relevant bleeding with NOACs and warfarin between patients older than 65 years old and patients aged ≤ 65 years old.
Discussion
In this study, we found that NOACs treatment was associated with a significantly lower incidence of bleeding events compared to warfarin treatment. Secondly, the incidence of death by all causes, cardiovascular death and thromboembolic events in HCM-AF patients was similar between the NOACs and warfarin group. We found that the use of NOACs was associated with a lower risk of clinically relevant bleeding events (HR 6.80, 95% CI 1.43–32.16; P = 0.016) compared with warfarin treatment, regardless of gender, hypertension, diabetes, previous ischemic stroke/TIA, chronic liver disease and chronic kidney disease.
HCM is considered an important cause of atrial fibrillation, heart failure, and sudden arrhythmic death in young patients [17]. Patients with HCM have an increased risk of developing AF (4–6 × more likely than the general population) and, eventually, 20%-30% of these patients develop this condition [18]. AF is usually poorly tolerated in patients with HCM because of an impaired diastolic relaxation due to the thickening and poor compliance of the ventricular walls [19]. HCM-AF patients have been known to be at high risk of thromboembolism. Several studies reported that the risk of ischemic stroke in these patients is eightfold higher than in HCM patients with no AF [20, 21]. CHA2DS2-VASc score is not effective in predicting thromboembolism risk in HCM patients with AF [22, 23]. In a retrospective study comprising 4821 HCM patients with AF, a total of 9.8% of the patients showing a CHA2DS2-VASc score of 0 had suffered thromboembolic events after 10 years [24]. Lifetime oral anticoagulation was recommended for all HCM-AF patients due to a high risk of thromboembolic events. Additionally, the thromboembolic risk is independent of the AF type, whether paroxysmal or persistent.
Clinical practice guidelines clearly state that oral anticoagulants such as VKA (warfarin) should be initiated in all HCM patients with persistent, permanent, or paroxysmal AF without contraindications, and that INR should be maintained within the therapeutic range (between 2.0 and 3.0) [2, 3]. A retrospective analysis by Jung et al. [25] from the Korean National Health Insurance Service database showed a similar risk of thromboembolic and hemorrhagic events in patients treated with NOACs and VKA over 16 months, with lower incidence of death by all causes and composite fatal cardiovascular events in the former group. Lee et al. used the same database and found that the incidence rates of ischemic stroke, major bleeding events, and a composite outcome that included ischemic stroke, intracranial bleeding, hospital admission for gastrointestinal bleeding and death by all causes, were significantly lower in the NOACs group after 18 months [26]. A meta-analysis that included 4 observational studies showed that NOACs were at least non-inferior to VKAs in preventing stroke in patients with both HCM and AF [27]. Another observational nonrandomized study [28] from four European centers demonstrated the incidences of thromboembolic events or minor bleeding were similar in patients with HCM undergoing catheter ablation for AF. Although HCM-AF patients are underrepresented in randomized trials of direct oral anticoagulants, these studies support the use of the factor Xa inhibitors (rivaroxaban/apixaban) or the oral direct thrombin inhibitor (dabigatran) as therapeutic alternatives for patients that are intolerable to warfarin or that have difficulty maintaining the INR within the therapeutic range.
At present, no results from randomized controlled trials (RCTs) evaluating the role of NOACs in patients with HCM and AF are available. Some data included in the aforementioned studies were collected from insurance databases, without considering the clinical characteristics and echocardiographic parameters of the patients (e.g., left atrial enlargement and left ventricular dysfunction) or factors leading to an increased risk of bleeding (e.g., coagulation function and antiplatelet therapy). Dominguez et al. [29] reported that HCM-AF patients on NOACs therapy showed similar embolic and bleeding rates to those in the VKA group. This provided clinical characteristics but not TTR for warfarin-treated patients. In our study, we showed that clinical characteristics and echocardiographic parameters were not significantly different between NOACs and VKA groups with the exception of antiplatelet therapy usage, which was higher in the latter. Patients treated with VKA had a 6.3% prevalence of previous myocardial infarction versus 2.6% in the NOAC group, and a high prevalence of cardiovascular risk factors, such as hypertension and diabetes, which did not reach statistical significance. In consideration of a higher proportion of cardiovascular complications, this could explain the higher frequency of antiplatelet therapy in the VKA group.
Furthermore, only 18.75% of patients enrolled in our study had a good TTR with a median score of 66.35%. The GARFIELD registry [30] demonstrated that only 16.7% of patients of an Asian cohort had a TTR ≥ 65% compared to 49.4% of patients in a European cohort. However, previous studies reported that TTRs ranged from 58 to 68% in clinical trial settings, and 55% of real worldwide incidence [31]. Compared to patients with a TTR > 70%, patients with a TTR < 50% are associated with a higher risk of ischemic stroke, bleeding, or death [32]. Hence, the lower mean TTR and fewer proportion of patients with an adequate TTR observed in this study were similar to those reported in Asian patients.
Our study still contains several limitations. First of all, we implemented a single-center, retrospective, and observational study. Compared with RCTs, this type of studies are more susceptible to biases. Second, comparisons between NOACs and warfarin groups need to take the limited sample sizes into account. Third, nearly 28% of patients treated with NOACs received a reduced dose of dabigatran. This is consistent with previous studies showing Asian doctors tend to prescribe low-dose NOACs for patients with AF [33]. The predominant use of a lower dose of dabigatran (110 mg) in our center may be related to fewer bleeding events in the NOACs group. Fourth, due to the lack of patients treated with apixaban, only two types of NOACs (dabigatran and rivaroxaban) were evaluated. Fifth, the use of antiplatelet therapy was twice higher in the VKA group compared to the NOAC group, although the difference was not statistical significant. This should be accounted in the interpretation of our results, because the more frequent use of antiplatelets may explain the increased risk of bleeding with VKA vs NOAC. Therefore, the results of this study need to be confirmed in randomized controlled trials or registries from larger HCM centers.
Conclusions
In conclusion, this study shows NOACs were associated with a lower incidence of clinically relevant bleeding compared to warfarin, with similar rates of death by all causes, cardiovascular death, or thromboembolic events. Our data also suggest that NOACs may be used safely and effectively for stroke prevention in patients with HCM and AF. Randomized controlled trials with larger sample sizes are still needed in this special group of patients to gather more evidence on the efficacy and safety of NOAC treatment.
References
January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr, Ellinor PT, Ezekowitz MD, Field ME, Furie KL, Heidenreich PA, Murray KT, Shea JB, Tracy CM, Yancy CW (2019) 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American college of cardiology/American heart association task force on clinical practice guidelines and the heart rhythm society in collaboration with the society of thoracic surgeons. Circulation 140(2):e125–e151
Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, Naidu SS, Nishimura RA, Ommen SR, Rakowski H, Seidman CE, Towbin JA, Udelson JE, Yancy CW (2011) American college of cardiology foundation/American heart association task force on practice guidelines; American association for thoracic surgery; American society of echocardiography; American society of nuclear cardiology; Heart failure society of America; Heart rhythm society; Society for cardiovascular angiography and interventions; Society of thoracic surgeons. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: executive summary: a report of the American college of cardiology foundation/American heart association task force on practice guidelines. Circulation 124(24):2761–2796
Task Force members, Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, Hagege AA, Lafont A, Limongelli G, Mahrholdt H, McKenna WJ, Mogensen J, Nihoyannopoulos P, Nistri S, Pieper PG, Pieske B, Rapezzi C, Rutten FH, Tillmanns C, Watkins H (2014) 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: the task force for the diagnosis and management of hypertrophic cardiomyopathy of the European society of cardiology (ESC). Eur Heart J 35(39):2733–2779
Chao TF, Lip GYH, Lin YJ, Chang SL, Lo LW, Hu YF, Tuan TC, Liao JN, Chung FP, Chen TJ, Chen SA (2018) Major bleeding and intracranial hemorrhage risk prediction in patients with atrial fibrillation: attention to modifiable bleeding risk factors or use of a bleeding risk stratification score? A nationwide cohort study. Int J Cardiol 254:157–161
Uchiyama S, Atarashi H, Inoue H, Kitazono T, Yamashita T, Shimizu W, Ikeda T, Kamouchi M, Kaikita K, Fukuda K, Origasa H, Shimokawa H (2019) Primary and secondary prevention of stroke and systemic embolism with rivaroxaban in patients with non-valvular atrial fibrillation : sub-analysis of the EXPAND Study. Heart Vessels 34(1):141–150
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Paolini JF, Berkowitz SD, Fox KA, Califf RM, ROCKET AF Investigators (2011) Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 365(10):883–891
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, Waldo AL, Ezekowitz MD, Weitz JI, Špinar J, Ruzyllo W, Ruda M, Koretsune Y, Betcher J, Shi M, Grip LT, Patel SP, Patel I, Hanyok JJ, Mercuri M, Antman EM, ENGAGE AF-TIMI 48 Investigators (2013) Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med 369(22):2093–2104
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener HC, Joyner CD, Wallentin L, RE-LY Steering Committee and Investigators (2009) Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 361(12):1139–1151
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, Al-Khalidi HR, Ansell J, Atar D, Avezum A, Bahit MC, Diaz R, Easton JD, Ezekowitz JA, Flaker G, Garcia D, Geraldes M, Gersh BJ, Golitsyn S, Goto S, Hermosillo AG, Hohnloser SH, Horowitz J, Mohan P, Jansky P, Lewis BS, Lopez-Sendon JL, Pais P, Parkhomenko A, Verheugt FW, Zhu J, Wallentin L, ARISTOTLE Committees and Investigators (2011) Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 365(11):981–992
Noseworthy PA, Yao X, Shah ND, Gersh BJ (2016) Stroke and bleeding risks in NOAC- and warfarin-treated patients with hypertrophic cardiomyopathy and atrial fibrillation. J Am Coll Cardiol 67(25):3020–3021
Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, Van Gelder IC, Al-Attar N, Hindricks G, Prendergast B, Heidbuchel H, Alfieri O, Angelini A, Atar D, Colonna P, De Caterina R, De Sutter J, Goette A, Gorenek B, Heldal M, Hohloser SH, Kolh P, Le Heuzey JY, Ponikowski P, Rutten FH (2010) Guidelines for the management of atrial fibrillation: the task force for the management of atrial fibrillation of the European society of cardiology (ESC). Eur Heart J 31(19):2369–2429
Lip GYH, Banerjee A, Boriani G, Chiang CE, Fargo R, Freedman B, Lane DA, Ruff CT, Turakhia M, Werring D, Patel S, Moores L (2018) Antithrombotic therapy for atrial fibrillation: CHEST guideline and expert panel report. Chest 154(5):1121–1201
Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis (2005) Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 3(4):692–694
Takase T, Ikesue H, Nakagawa H, Kinoshita M, Muroi N, Kitai T, Furukawa Y, Hashida T (2020) Risk factors for major bleeding and clinically relevant non-major bleeding in Japanese patients treated with edoxaban. Biol Pharm Bull 43(3):458–462
Marcatto LR, Sacilotto L, Tavares LC, Facin M, Olivetti N, Strunz CMC, Darrieux FCC, Scanavacca MI, Krieger JE, Pereira AC, Santos PCJL (2018) Pharmaceutical care increases time in therapeutic range of patients with poor quality of anticoagulation with warfarin. Front Pharmacol 9:1052
Connolly SJ, Pogue J, Eikelboom J, Flaker G, Commerford P, Franzosi MG, Healey JS, Yusuf S, ACTIVEW Investigators (2008) Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centers and countries as measured by time in therapeutic range. Circulation 118(20):2029–2037
Maron BJ (2018) Clinical course and management of hypertrophic cardiomyopathy. N Engl J Med 379(7):655–668
Lee SE, Park JK, Uhm JS, Kim JY, Pak HN, Lee MH, Joung B (2017) Impact of atrial fibrillation on the clinical course of apical hypertrophic cardiomyopathy. Heart 103(19):1496–1501
Garg L, Gupta M, Sabzwari SRA, Agrawal S, Agarwal M, Nazir T, Gordon J, Bozorgnia B, Martinez MW (2019) Atrial fibrillation in hypertrophic cardiomyopathy: prevalence, clinical impact, and management. Heart Fail Rev 24(2):189–197
Olivotto I, Cecchi F, Casey SA, Dolara A, Traverse JH, Maron BJ (2001) Impact of atrial fibrillation on the clinical course of hypertrophic cardiomyopathy. Circulation 104(21):2517–2524
Guttmann OP, Rahman MS, O’Mahony C, Anastasakis A, Elliott PM (2014) Atrial fibrillation and thromboembolism in patients with hypertrophic cardiomyopathy: systematic review. Heart 100(6):465–472
Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, Naidu SS, Nishimura RA, Ommen SR, Rakowski H, Seidman CE, Towbin JA, Udelson JE, Yancy CW (2011) American college of cardiology foundation/American heart association task force on practice guidelines. Developed in collaboration with the American association for thoracic surgery, American society of echocardiography, American society of nuclear cardiology, Heart failure society of America, Heart rhythm society, society for cardiovascular angiography and interventions, and society of thoracic surgeons. J Am Coll Cardiol 58(25):e212–e260
Ammirati E, Contri R, Coppini R, Cecchi F, Frigerio M, Olivotto I (2016) Pharmacological treatment of hypertrophic cardiomyopathy: current practice and novel perspectives. Eur J Heart Fail 18(9):1106–1118
Guttmann OP, Pavlou M, O’Mahony C, Monserrat L, Anastasakis A, Rapezzi C, Biagini E, Gimeno JR, Limongelli G, Garcia-Pavia P, McKenna WJ, Omar RZ, Elliott PM (2015) Prediction of thrombo-embolic risk in patients with hypertrophic cardiomyopathy (HCM Risk-CVA). Eur J Heart Fail 17(8):837–845
Jung H, Yang PS, Jang E, Yu HT, Kim TH, Uhm JS, Kim JY, Pak HN, Lee MH, Joung B, Lip GYH (2019) Effectiveness and safety of non-vitamin k antagonist oral anticoagulants in patients with atrial fibrillation with hypertrophic cardiomyopathy: a nationwide cohort study. Chest 155(2):354–363
Lee HJ, Kim HK, Jung JH, Han KD, Lee H, Park JB, Kim HM, Kim YJ, Ommen SR (2019) Novel oral anticoagulants for primary stroke prevention in hypertrophic cardiomyopathy patients with atrial fibrillation. Stroke 50(9):2582–2586
Zhou Y, He W, Zhou Y, Zhu W (2020) Non-vitamin K antagonist oral anticoagulants in patients with hypertrophic cardiomyopathy and atrial fibrillation: a systematic review and meta-analysis. J Thromb Thrombolysis 50(2):311–317
Creta A, Hunter RJ, Earley MJ, Finlay M, Dhinoja M, Sporton S, Chow A, Mohiddin SA, Boveda S, Adragao P, Jebberi Z, Matos D, Schilling RJ, Lambiase PD, Providencia R (2020) Non-vitamin K oral anticoagulants in hypertrophic cardiomyopathy patients undergoing catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol 31(10):2626–2631
Dominguez F, Climent V, Zorio E, Ripoll-Vera T, Salazar-Mendiguchía J, García-Pinilla JM, Urbano-Moral JA, Fernández-Fernández X, Lopez-Cuenca D, Ajo-Ferrer R, Sanz-Sanchez J, Gomez-Perez Y, López-Garrido MA, Barriales-Villa R, Gimeno JR, Garcia-Pavia P (2017) Direct oral anticoagulants in patients with hypertrophic cardiomyopathy and atrial fibrillation. Int J Cardiol 248:232–238
Haas S, Ten Cate H, Accetta G, Angchaisuksiri P, Bassand JP, Camm AJ, Corbalan R, Darius H, Fitzmaurice DA, Goldhaber SZ, Goto S, Jacobson B, Kayani G, Mantovani LG, Misselwitz F, Pieper K, Schellong SM, Stepinska J, Turpie AG, van Eickels M, Kakkar AK, GARFIELD-AF Investigators (2016) Quality of vitamin K antagonist control and 1-year outcomes in patients with atrial fibrillation: a global perspective from the GARFIELD-AF registry. PLoS ONE 11(10):e0164076
Reiffel JA (2017) Time in the therapeutic range for patients taking warfarin in clinical trials: useful, but also misleading, misused, and overinterpreted. Circulation 135:1475–1477
White RD, Riggs KW, Ege EJ, Petroski GF, Koerber SM, Flaker G (2016) The effect of the amiodarone warfarin interaction on anticoagulation quality in a single, high-quality anticoagulation center. Blood Coagul Fibrinolysis 27(2):147–150
Chan YH, Kuo CT, Yeh YH, Chang SH, Wu LS, Lee HF, Tu HT, See LC (2016) Thromboembolic, bleeding, and mortality risks of rivaroxaban and dabigatran in Asians with nonvalvular atrial fibrillation. J Am Coll Cardiol 68(13):1389–1401
Funding
This study was financially supported by National Natural Science Foundation of China (Grant No. 81970370); Foreign Cooperation Project of Science and Technology, Fujian Province (No.2021I0013); Fujian Provincial Health Technology Project (Grant No. 2019–1-40); Fujian Provincial Health Technology (Grant No.2019-CX-28). The funder of this study had no role in the study design, data collection, data analysis, data interpretation, or writing of this paper. The corresponding authors had full access to the data used in the study and had final responsibility for the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
FP, YL, HX, JS planned and designed the study, and directed its implementation; FP, YL, HX, JS drafted the protocol; FP, HX, JS obtained statutory and ethics approvals; HX, JS, JL, QZ, ML, WZ contributed to data acquisition; FP, YL, HX, JS, JL, QZ, ML, WZ had access to the raw data; FP, YL, HX, JS, JL were responsible for data preparation, quality control and data analysis; FP, YL wrote the manuscript. All authors approved the final version of the submitted manuscript.
Corresponding author
Ethics declarations
Conflict interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, Y., Xiong, H., Su, J. et al. Effectiveness and safety of non-vitamin K antagonist oral anticoagulants in patients with hypertrophic cardiomyopathy with non-valvular atrial fibrillation. Heart Vessels 37, 1224–1231 (2022). https://doi.org/10.1007/s00380-022-02021-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02021-2