Abstract
Background
Atrial fibrillation (AF) frequently complicates hypertrophic cardiomyopathy (HCM), and anticoagulation significantly decreases the risk of stroke in this population. To date, no randomized controlled trials (RCTs) have compared direct oral anticoagulants (DOACs) and vitamin K antagonists (VKAs). The present study aimed to systematically compare the two anticoagulation strategies in terms of effectiveness and safety.
Method
We performed a systematic literature search and meta-analysis in the PubMed, MEDLINE, and EMBASE databases for studies reporting all-cause mortality, major bleeding, or thromboembolic events (TEs). Since no RCTs were available, we included observational studies only. The overall hazard ratio (HR) and 95% confidence interval (CI) for each analyzed parameter were pooled using a random-effects model.
Results
Five observational studies including 6919 patients were eligible for inclusion. Compared with VKAs, DOACs were associated with statistically significant lower rates of all-cause mortality (HR 0.64, 95% CI 0.35–0.54; p < 0.00001), comparable major bleeding events (HR 0.64, 95% CI 0.40–1.03; p = 0.07), and TEs (HR 0.94, 95% CI 0.73–1.22; p = 0.65).
Conclusions
Compared with VKAs, a DOAC-based strategy might represent an effective and safe strategy regarding all-cause mortality, major/life-threatening bleeding complications, and TEs in HCM patients with concomitant AF. However, further prospective studies are necessary to reinforce a DOAC-based anticoagulation strategy in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Up to one of five patients with hypertrophic cardiomyopathy (HCM) experience atrial fibrillation (AF), significantly affecting prognosis. |
To date, no randomized controlled trials (RCTs) have compared direct oral anticoagulants (DOACs) and vitamin K antagonists (VKAs). |
Our study highlighted that compared with VKAs, a DOAC-based strategy might represent an effective and safe strategy regarding all-cause mortality, major/life-threatening bleeding complications, and thromboembolic events in this population. |
1 Introduction
The prevalence and incidence of atrial fibrillation (AF) in patients with hypertrophic cardiomyopathy (HCM) is four to six times higher than in the general population, ranging from 20 to 23% and 2 to 5% per year, respectively [1,2,3]. The majority of the affected patients experience paroxysmal episodes [4]. Since left ventricular diastolic compliance is decreased in HCM patients, atrial pump function is essential to provide adequate ventricular filling and maintain enough cardiac output. Aging, increased left atrial size, and reduced left ventricular ejection fraction are well-recognized risk factors for AF [2, 5, 6]. Notably, AF is associated with a poor prognosis in terms of worsening heart failure, risk of stroke, and mortality [2, 7, 8]. Specifically, AF per se in the HCM population is associated with a 50% relative risk of increased mortality, mostly secondary to heart failure- or stroke-related complications [8]. As for the general population, the risk of thromboembolic events (TEs) in patients with HCM and AF is increased, even in cases of isolated brief episodes [2, 4, 9]. However, the CHA2DS2-VASc score cannot be applied to patients with HCM to determine the need for anticoagulation since these patients are not included in most clinical trials of thrombotic prevention in AF [10,11,12,13]. Thus, because of the high risk of thromboembolism, even patients with a CHA2DS2-VASc score of 0 or 1 should be anticoagulated [4]. Evidence comparing direct oral anticoagulants (DOACs) and vitamin K antagonists (VKAs) has highlighted the efficacy and safety of a DOAC-based strategy for AF in the general population, even if the HCM subpopulation was not effectively represented [10,11,12,13]. The European Cardiology Society has recommended, unless contraindicated, VKAs in HCM patients who develop AF [14]. On the other hand, the American College of Cardiology Foundation Task Force recommends DOACs regardless of the CHA2DS2-VASc score [15]. Specific antithrombotic regimens in patients with HCM have not been validated in randomized controlled trials (RCTs). However, recent observational studies tested DOAC-based regimens in HCM patients with concomitant AF [16, 17]. Thus, the present study aimed to systematically compare a DOAC-based versus a VKA-based strategy in terms of effectiveness and safety.
2 Methods
2.1 Search Strategy and Study Selection
According to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [18], we conducted a systematic literature search of the PubMed, MEDLINE, Cochrane, and EMBASE databases through September 2022 for relevant studies. Keywords utilized to find the pertinent articles were ‘AF and HCM’, ‘HCM and anticoagulation’, ‘vitamin K antagonist in HCM and AF’, ‘direct oral anticoagulants in HCM’, and ‘vitamin K antagonist or direct oral anticoagulants in HCM’.
Three co-authors (FO, DC, and AP) independently proceeded with the preliminary screening process to recognize all citations of potential acceptability, and also looked for additional citations from the reference list of the included articles. The inclusion criteria were as follows:
-
1.
Comparison between DOACs and VKAs in HCM patients with AF and at least one of the following outcomes:
-
overall mortality
-
major bleeding.
-
-
2.
Follow-up ≥ 3 months.
-
3.
Original, untranslated studies (written in the English language only) published in a peer-reviewed journal.
-
4.
Total study participants ≥100.
Full-text papers of recognized abstracts pertinent to our inclusion criteria were evaluated for eligibility. We excluded conference abstracts, case reports/series, letters, and editorials. The inter-rater reliability of the reviewers was assessed using the Kappa statistic [19].
2.2 Data Extraction
Two authors (AB and MA) independently identified inherent data using a standardized recording tool to document the study design, year of publication, number of study participants, country of origin, follow-up length, participant clinical characteristics, anticoagulation protocol, and study outcomes.
2.3 Quality Assessment
The Newcastle–Ottawa Scale (NOS) was applied to assess the quality assessment of the included observational studies. Two authors (LT and FRG) evaluated the quality of each study by checking three principal categories: (1) selection; (2) comparability; and (3) outcomes. Any study can achieve a maximum of nine stars (four stars for selection, two for comparability, and three for the outcome) [20]. We then converted an individual study’s NOS score into the Agency for Healthcare Research and Quality (AHRQ) standards [21]. Thus, studies were subclassified into the three following classes of quality categories (electronic supplementary Table S1).
-
1.
Poor quality: ≤ 1 star for the selection domain OR 0 stars for the comparability domain OR ≤ 1 star for the outcome domain.
-
2.
Fair quality: 2 stars for the selection domain AND 1 or 2 stars for the comparability domain AND 2 or 3 stars for the outcome domain.
-
3.
Good quality: ≥ 3 stars for the selection domain AND ≥ 1 star for the comparability domain AND ≥ 2 stars in the outcome domain.
2.4 Data Analysis and Synthesis
We utilized the Review Manager software (RevMan 5.4.1) to conduct our statistical analyses. The overall hazard ratio (HR) and 95% confidence interval (CI) for each analyzed parameter were pooled using a random-effects model. Furthermore, we have presented forest plots to visually evaluate the pooling results. An HR value of >1 indicates an increased risk of the considered outcome; an HR value of 1 indicates no observed association; and an HR value of <1 indicates decreased risk of the outcome of interest. A two-sided p value <0.05 was considered statistically significant. Furthermore, the studies’ heterogeneity results were calculated using the Higgins I2, which measures the percentage of the total variation across the included studies [22]. The I2 values lie between 0 and 100%. A value of 0% indicates no heterogeneity, and we classified heterogeneity into mild (I2 < 25%), moderate (25 ≤ I2 < 50%), severe (50 ≤ I2 < 75%), and very severe (I2 ≥ 75%) [23].
3 Results
3.1 Literature Search
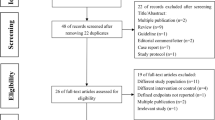
Figure 1 shows the flow diagram of the identified studies. We identified 1200 records in the preliminary search, and 1087 records were excluded as they did not meet the inclusion criteria. A total of 18 studies were used for data extraction and synthesis for our systematic review. Five articles were finally included in our meta-analysis [16, 17, 24,25,26].
3.2 Characteristics of the Included Studies
The characteristics of the included studies are listed in Table 1. All five studies were of an observational, retrospective design [30,31,32,33,34] and were based on four countries (Korea, China, Spain, United States) and three continents. The total number of individuals included in our meta-analysis was 6919 (3652 and 3267 receiving DOACs and VKAs, respectively). Follow-up was heterogeneous, ranging from 0.56 years to 6.5 years. Rivaroxaban was the most utilized DOAC, while edoxaban was the least administered. Warfarin was the VKA of choice in all studies except for the study by Dominguez et al., in which acenocoumarol was used [24]. There was a fair gender distribution, while hypertension was the main cardiovascular risk factor. TEs were characterized by stroke plus systemic thromboembolism. There was heterogeneity in the major bleeding criteria among the studies, even when hemoglobin dropped by > 2 g/dL or when unscheduled visits/hospitalizations were included.
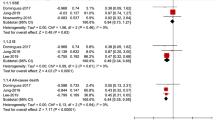
3.3 All-Cause Mortality
Four studies compared DOACs and VKA in terms of all-cause mortality (Fig. 2). The DOACs strategy was associated with a statistically significant reduction in all-cause mortality outcome (HR 0.64, 95% CI 0.35–0.54; p < 0.00001) with no heterogeneity (I2 = 0%).
Forest plots comparing DOAC versus VKA anticoagulation strategies. a Overall mortality; b major bleeding; c intracranial hemorrhage; d gastrointestinal bleeding; e thromboembolic events. SE standard error, IV inverse variance, CI confidence interval, df degrees of freedom, DOACs direct oral anticoagulants, VKAs vitamin K antagonists, ICH intracranial hemorrhage, GI gastrointestinal, TE thromboembolic events
3.4 Major Bleeding
A pooled analysis of five papers was performed (Fig. 2b). DOACs reduced major bleeding events but the results were not statistically significant (HR 0.64, 95% CI 0.40–1.03; p = 0.07). Heterogeneity was severe (I2 = 63%).
3.4.1 Intracranial Bleeding
Figure 2c reports the pooled analysis of the three available studies reporting intracranial bleeding. The DOAC-based regimen was associated with a reduced risk of intracranial hemorrhage (ICH; HR 0.43, 95% CI 0.24–0.76; p = 0.004), with low heterogeneity (I2 = 1%).
3.4.2 Gastrointestinal Bleeding
Gastrointestinal bleeding events were reported in four studies (Fig. 2d). No statistically significant difference between the two anticoagulation regimens was assessed (HR 0.68, 95% CI 0.42–1.13; p = 0.14), however heterogeneity was substantial (I2 = 60%).
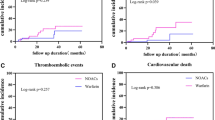
3.5 Thromboembolic Events
Figure 2e reported TEs in the population considered. No statistically significant difference between DOACs and VKAs was appreciated between the two groups (HR 0.94, 95% CI 0.73–1.22; p = 0.65), with no heterogeneity (I2 = 0%).
4 Discussion
AF represents a common complication associated with poor prognosis in patients with HCM [2, 7, 8]. Pivotal RCTs comparing DOACs and VKAs demonstrated the safety and efficacy of a DOAC-based strategy for AF in the general population, even if the HCM subpopulation was not effectively represented [10,11,12,13]. In this setting, the 2014 European Society of Cardiology (ESC) guidelines recommend VKAs in HCM patients who develop AF to prevent thromboembolism [14], although the newest 2018 practical guidelines opted for the use of DOACs [27]. On the other hand, the more recent 2020 American College of Cardiology Foundation Task Force recommends DOACs in HCM patients with concomitant AF [15]. Notably, the CHA2DS2-VASc score is unnecessary to start treatment with a DOAC in this setting [15].
Our meta-analysis included the main studies examining DOAC-based strategies compared with VKA-based strategies. Although all of the studies were of an observational, retrospective design, interesting data have emerged. The overall mortality rate was statistically lower in the DOAC group, with no heterogeneity between studies (HR 0.64, 95% CI 0.35–0.54; p < 0.00001, I2 0%). Moreover, major bleeding events were comparable between the two strategies (HR 0.64, 95% CI 0.40–1.03; p = 0.07), even if DOACs were associated with a reduced ICH burden (HR 0.43, 95% CI 0.24–0.76; p = 0.004). Lastly, both strategies showed comparable protection from TEs (HR 0.94, 95% CI 0.73–1.22; p = 0.65).
However, for a comprehensive evaluation, our results must be considered thoroughly. First, Lee et al. and Jung et al. conducted retrospective studies based on Korean health insurance review and assessment service databases from 2013 and 2016, and 2011 to 2016, respectively [17, 25]. Overall, they represent about two-thirds of the included population sample. Many patients were likely included in both studies, possibly affecting the results by overestimating the effect size. Second, although the pooled analysis of the pivotal RCTs comparing DOACs and VKAs in patients with AF showed a modest but significant all-cause mortality reduction in the DOAC arm [28], our results showed a more substantial effect. It is plausible that without randomization, frailer patients with more comorbidities or a contraindication for DOACs would be considered for VKA administration. Thus, allocation bias may affect the enhanced effect on overall mortality outcome. Third, we found severe heterogeneity when major bleeding events were considered. Different bleeding criteria definitions, possible under/overtherapeutic INR in the VKA group, compliance issues, and allocation bias might explain the above finding.
Besides the above considerations, due to issues with adherence to VKAs, DOACs are easily prescribed for convenience [29]. Moreover, new oral anticoagulants had a favorable risk–benefit profile in the general population, with significant reductions in stroke, intracranial hemorrhage, and mortality, and with similar major bleeding as for warfarin [28]. Furthermore, the DOAC-based strategy is a cost-effective advantage compared with warfarin use. Specifically, although warfarin remained the cheapest outpatient drug, considering inpatient admissions, the total cost per patient in the DOAC group is lower than VKAs [30].
In the general population, rhythm control strategy based on catheter ablation is a widely used strategy to relieve symtoms or treat heart failure [31, 32]. Because of the valuable contribution of atrial contraction in providing adequate ventricular filling and maintaining sufficient cardiac output, maintaining rhythm control is pivotal in the HCM population. In this setting, a recent study observed that catheter ablation is effective in patients with HCM and AF and is associated with a low complication rate, even though the success rate following a single procedure is low (about 40%) and the risk of relapse is twofold higher [33, 34]. Moreover, Creta et al. demonstrated that both VKAs and DOACs are comparable in terms of safety and effectiveness in HCM patients, even those undergoing catheter ablation [35].
4.1 Study Limitations
As we elaborated on in the Discussion section of this article, the results of our study are affected by non-insignificant limitations:
-
1.
Observational studies per se are implicitly affected by higher sources of biases compared with RCTs (i.e., allocation bias);
-
2.
We combined all DOACs without assessing a subgroup analysis of the specific molecules;
-
3.
Medication compliance is not specified, resulting in an important variable affecting effect size;
-
4.
Dfferent follow-ups may influence the results of our study.
5 Conclusion
Compared with VKAs, observational-based evidence showed that DOACs might represent an effective and safe strategy in terms of all-cause mortality, major/life-threatening bleeding complications and TEs in HCM patients with concomitant AF. However, further prospective studies are necessary to reinforce a DOAC-based anticoagulation strategy in this population.
References
Robinson K, Frenneaux MP, Stockins B, Karatasakis G, Poloniecki JD, McKenna WJ. Atrial fibrillation in hypertrophic cardiomyopathy: a longitudinal study. J Am Coll Cardiol. 1990;15(6):1279–85. https://doi.org/10.1016/s0735-1097(10)80014-2.
Olivotto I, Cecchi F, Casey SA, Dolara A, Traverse JH, Maron BJ. Impact of atrial fibrillation on the clinical course of hypertrophic cardiomyopathy. Circulation. 2001;104(21):2517–24. https://doi.org/10.1161/hc4601.097997.
Rowin EJ, Orfanos A, Estes NAM, et al. Occurrence and natural history of clinically silent episodes of atrial fibrillation in hypertrophic cardiomyopathy. Am J Cardiol. 2017;119(11):1862–5. https://doi.org/10.1016/j.amjcard.2017.02.040.
Rowin EJ, Hausvater A, Link MS, et al. Clinical profile and consequences of atrial fibrillation in hypertrophic cardiomyopathy. Circulation. 2017;136(25):2420–36. https://doi.org/10.1161/CIRCULATIONAHA.117.029267.
Tani T, Tanabe K, Ono M, et al. Left atrial volume and the risk of paroxysmal atrial fibrillation in patients with hypertrophic cardiomyopathy. J Am Soc Echocardiogr. 2004;17(6):644–8. https://doi.org/10.1016/j.echo.2004.02.010.
Sivalokanathan S, Zghaib T, Greenland GV, et al. Hypertrophic cardiomyopathy patients with paroxysmal atrial fibrillation have a high burden of left atrial fibrosis by cardiac magnetic resonance imaging. JACC Clin Electrophysiol. 2019;5(3):364–75. https://doi.org/10.1016/j.jacep.2018.10.016.
Cecchi F, Olivotto I, Montereggi A, Santoro G, Dolara A, Maron BJ. Hypertrophic cardiomyopathy in Tuscany: clinical course and outcome in an unselected regional population. J Am Coll Cardiol. 1995;26(6):1529–36. https://doi.org/10.1016/0735-1097(95)00353-3.
Siontis KC, Geske JB, Ong K, Nishimura RA, Ommen SR, Gersh BJ. Atrial fibrillation in hypertrophic cardiomyopathy: prevalence, clinical correlations, and mortality in a large high-risk population. J Am Heart Assoc. 2014;3(3): e001002. https://doi.org/10.1161/JAHA.114.001002.
Tsuda T, Hayashi K, Fujino N, et al. Effect of hypertrophic cardiomyopathy on the prediction of thromboembolism in patients with nonvalvular atrial fibrillation. Heart Rhythm. 2019;16(6):829–37. https://doi.org/10.1016/j.hrthm.2018.11.029.
Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92.
Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91.
Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation [published erratum appears in N Engl J Med. 2010 Nov;363(19):1877]. N Engl J Med. 2009;361(12):1139–51.
Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104.
Authors/Task Force members, Elliott PM, Anastasakis A, et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014;35(39):2733–79. https://doi.org/10.1093/eurheartj/ehu284.
Ommen SR, Mital S, Burke MA, et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2020;142(25):e533–57. https://doi.org/10.1161/CIR.0000000000000938.
Noseworthy PA, Yao X, Shah ND, Gersh BJ. Stroke and bleeding risks in NOAC- and warfarin-treated patients with hypertrophic cardiomyopathy and atrial fibrillation. J Am Coll Cardiol. 2016;67(25):3020–1. https://doi.org/10.1016/j.jacc.2016.04.026.
Jung H, Yang PS, Jang E, et al. Effectiveness and safety of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation with hypertrophic cardiomyopathy: a nationwide cohort study. Chest. 2019;155(2):354–63. https://doi.org/10.1016/j.chest.2018.11.009.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7): e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. https://doi.org/10.1007/s10654-010-9491-z.
Zeng X, Zhang Y, Kwong JS, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. 2015;8(1):2–10. https://doi.org/10.1111/jebm.12141.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. https://doi.org/10.1002/sim.1186.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Dominguez F, Climent V, Zorio E, et al. Direct oral anticoagulants in patients with hypertrophic cardiomyopathy and atrial fibrillation. Int J Cardiol. 2017;248:232–8. https://doi.org/10.1016/j.ijcard.2017.08.010.
Lee HJ, Kim HK, Jung JH, et al. Novel oral anticoagulants for primary stroke prevention in hypertrophic cardiomyopathy patients with atrial fibrillation. Stroke. 2019;50(9):2582–6. https://doi.org/10.1161/STROKEAHA.119.026048.
Lin Y, Xiong H, Su J, et al. Effectiveness and safety of non-vitamin K antagonist oral anticoagulants in patients with hypertrophic cardiomyopathy with non-valvular atrial fibrillation. Heart Vessels. 2022;37(7):1224–31. https://doi.org/10.1007/s00380-022-02021-2.
Steffel J, Verhamme P, Potpara TS, et al. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018;39(16):1330–93. https://doi.org/10.1093/eurheartj/ehy136.
Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955–62. https://doi.org/10.1016/S0140-6736(13)62343-0.
Hendriks T, McGregor S, Rakesh S, Robinson J, Ho KM, Baker R. Patient satisfaction after conversion from warfarin to direct oral anticoagulants for patients on extended duration of anticoagulation for venous thromboembolism—the SWAN Study. PLoS ONE. 2020;15(6): e0234048. https://doi.org/10.1371/journal.pone.0234048.
Ortiz-Cartagena I, Gotay A, Acevedo J, et al. Cost effectiveness of oral anticoagulation therapy for non-valvular atrial fibrillation patients: warfarin versus the new oral anticogulants rivaroxaban, dabigatran and apixaban. J Am Coll Cardiol. 2018;71(11 Suppl):A490.
Packer DL, Mark DB, Robb RA, et al. Effect of catheter ablation vs antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA. 2019;321(13):1261–74. https://doi.org/10.1001/jama.2019.0693.
Marrouche NF, Brachmann J, Andresen D, et al. Catheter ablation for atrial fibrillation with heart failure. N Engl J Med. 2018;378(5):417–27. https://doi.org/10.1056/NEJMoa1707855.
Providencia R, Elliott P, Patel K, et al. Catheter ablation for atrial fibrillation in hypertrophic cardiomyopathy: a systematic review and meta-analysis. Heart. 2016;102(19):1533–43. https://doi.org/10.1136/heartjnl-2016-309406.
Faraz F, Rehman MEU, Sabir B, et al. Efficacy of catheter ablation for atrial fibrillation in hypertrophic cardiomyopathy: a systematic review and meta-analysis. Curr Probl Cardiol. 2023;48(3): 101524. https://doi.org/10.1016/j.cpcardiol.2022.101524.
Creta A, Hunter RJ, Earley MJ, et al. Non-vitamin K oral anticoagulants in hypertrophic cardiomyopathy patients undergoing catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2020;31(10):2626–31. https://doi.org/10.1111/jce.14659.
Acknowledgements
All authors have participated in this work and have reviewed and agree with the contents of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflicts of interest
Federico Oliveri, Antonella Pepe, Andrea Bongiorno, Alessandro Fasolino, Francesca Romana Gentile, Sandra Schirinzi, Davide Colombo, Federico Breviario, Alessandra Greco, Annalisa Turco, Mauro Acquaro, Lorenzo Tua, Laura Scelsi, and Stefano Ghio declare they have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Author contributions
All authors participated in the conceptualization, data curation, analysis, writing, reviewing and editing of this manuscript.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oliveri, F., Pepe, A., Bongiorno, A. et al. Hypertrophic Cardiomyopathy and Atrial Fibrillation: A Systematic Review and Meta-analysis of Anticoagulation Strategy. Am J Cardiovasc Drugs 23, 269–276 (2023). https://doi.org/10.1007/s40256-023-00580-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-023-00580-x