Abstract
Several studies have explored the use of NOACs compared with vitamin K antagonists (VKAs) in patients with hypertrophic cardiomyopathy (HCM) and atrial fibrillation (AF); and therefore, we aimed to compare the efficacy and safety outcomes of NOACs with VKAs in this population. We systematically searched the PubMed and Embase databases until August 5, 2019 for studies that compared the effect of NOACs with VKAs in patients with HCM and AF. The risk ratios (RRs) with 95% confidence intervals (CIs) were pooled using a random-effects model. A total of four observational studies were included in this meta-analysis. Overall, compared with VKAs use, the use of NOACs was associated with reduced risks of ischemic stroke (RR 0.49, 95% CI 0.34–0.69), all-cause death (RR 0.44, 95% CI 0.35–0.55), and intracranial hemorrhage (RR 0.43, 95% CI 0.24–0.77). There were no differences in the risks of stroke or systemic embolism, major or clinically relevant bleeding, and gastrointestinal bleeding in patients with NOACs versus VKAs. Re-analyses with a fixed-effects model produced the similar results as the main analyses. For the efficacy and safety outcomes, comparisons of NOACs versus warfarin produced the similar results as those of NOACs versus VKAs. Based on current data from observational studies, compared with VKAs, NOACs had similar or lower risks of thromboembolic and bleeding events in patients with HCM and AF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Highlights
-
Compared with VKAs, NOACs had similar or lower risks of thromboembolic and bleeding events in patients with HCM and AF.
-
The use of NOACs was at least non-inferior to VKAs for stroke prevention in patients with HCM and AF.
Introduction
Hypertrophic cardiomyopathy (HCM) is a common non-ischaemic primary myocardial disease, resulting in increased risks of stroke and death. Atrial fibrillation (AF) is the most common cardiac arrhythmia, which may greatly increase the mortality and morbidity, and result in a lot of unnecessary medical wastes and additional costs of care [1]. AF is commonly observed in patients with HCM and associated with elevated risks of thromboembolic events [2, 3]. The stroke-scoring systems such as the CHA2DS2-VASc tool for stroke prediction have not completely been validated in HCM patients with AF [4, 5]. Due to the increased thromboembolic and bleeding risks, current guidelines recommend the lifelong oral anticoagulant therapy in HCM patients who develop AF without contraindications, regardless of the stroke-scoring systems [6]. The use of vitamin K antagonists (VKAs) is effective in this population [7], but have several shortcomings including variations in medication dosage, narrow therapeutic window, frequent international normalized ratio monitoring, and interactions with other foods or drugs.
Several randomized clinical trials (RCTs) have demonstrated that non-vitamin K antagonist oral anticoagulants (NOACs) are at least as effective as VKAs for stroke prevention, and even have a better safety profile in AF patients [8,9,10,11]. However, HCM patients are not included in these landmark RCTs. Data on the use of NOACs in AF patients could not be extrapolated to patients with AF and HCM directly because different forms of structural abnormalities in the heart may lead to different responses to anticoagulant therapy. The assumed role of NOACs in HCM patients with AF remains unknown because of the extremely limited data. Despite these, the results from the observational studies would provide some lights into the use of NOACs compared with VKAs in patients with HCM and AF [12,13,14,15], which may have great clinical significance in guiding the use of anticoagulants in this population. Therefore, we performed a meta-analysis to compare the efficacy and safety outcomes of NOACs with VKAs in patients with HCM and AF.
Methods
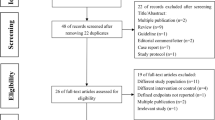
In this meta-analysis, the whole process was established according to the Cochrane handbook for systematic reviews [16]. The protocol and reporting of the results adhere to the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) statement [17]. Only the published studies were included in this meta-analysis; and therefore, the ethical approval was not warranted.
Eligibility criteria
We included studies if they met the following criteria: (1) study population-patients with HCM and AF. (2) Interventions: any NOAC (dabigatran, rivaroxaban, edoxaban or apixaban; any dose) versus VKAs (warfarin, coumadin, acenocoumarol, or phenprocoumon). (3) Outcomes: studies reported at least one of the efficacy or safety outcomes. Efficacy outcomes included stroke or systemic embolism (SSE), ischemic stroke (IS), and all-cause death; and safety outcomes included major or clinically relevant bleeding, intracranial hemorrhage (ICH) and gastrointestinal (GI) bleeding. We adopted the definitions of outcomes from the original studies. (4) Study design-observational studies. (5) Effect estimates of the study: propensity score-matched or adjusted risk ratios (RRs) and 95% confidence intervals (CIs).
Studies reporting AF patients undergoing radiofrequency ablation, cardioversion, or left-atrial appendage closure were excluded. Studies with no relevant data such as reviews, case reports, case series, editorials, letters, guidelines, and meeting abstracts were also excluded. If study participants had a substantial overlap, the study with the longest follow-up or largest sample size could be included.
Literature search
We systematically searched two computer-based databases (PubMed and Embase) from inception to August 5, 2019 for studies that evaluated the effect of any NOAC with VKAs in patients with HCM and AF. The following four types of search terms (and their similar terms) were combined by using the Boolean operator “and”: hypertrophic cardiomyopathy, atrial fibrillation, non-vitamin K antagonist oral anticoagulants, and vitamin K antagonists. The literature search strategy is shown in Supplemental Table 1. In additional, we performed further searches using the reference lists of the retrieved studies for additional studies. No language restrictions for publication were applied in the search.
Study selection and data abstraction
All of the retrieved studies were screened by three researchers (Yunguo Zhou, Wenfeng He, and Yue Zhou) independently. According to the pre-defined inclusion criteria, we first read the titles and abstracts to screen out the potentially available studies, and then reviewed the full texts of these studies in more detail. Discrepancies were resolved by consensus, or resolved by another researcher (Wengen zhu). For each study, we abstracted the following characteristics: the first author and publication year, study design, number of NOACs/warfarin users, and type of NOACs, follow-up time, and the efficacy and safety outcomes. We presented the definitions of AF or HCM in the Supplementary Table 2.
Quality assessment
For the observational studies, the study quality was assessed by using the Newcastle–Ottawa score (NOS), which involved the selection of cohorts, the comparability of cohorts, and the assessment of the outcome [18]. In this meta-analysis, the modified NOS tool was applied to evaluate the study quality (Supplemental Table 3). An NOS score of < 6 indicated a low-quality as previously described [19].
Statistical analysis
The Cochrane Q test and I2 statistic were used to evaluate heterogeneity, where P < 0.1 and I2 > 50% indicated a substantial heterogeneity, respectively. The RRs and 95% CIs were regarded as the risk estimates. For each study, we calculated the natural logarithm of the RR (Ln[RR]) and its corresponding standard error (SELn[RR]). To estimate the pooled results more conservative, Ln[RR] and SELn[RR] were pooled by a random-effects model weighted by the inverse-variance method. Two sensitivity analyses were performed as follows: (1) re-analyses with a fixed-effects model were used; and (2) the efficacy and safety outcomes of NOACs versus warfarin were analyzed solely. The subgroup analysis was not performed because of the limited data. According to the Cochrane handbook, it was unsuitable to perform the publication bias for the reported effect estimates when the number of included studies was less than 10.
All statistical analyses were performed by using Review Manager version 5.30 software (the Cochrane Collaboration, Copenhagen, Denmark).
Results
Study selection
The steps of literature retrieval are shown in Supplemental Fig. 1. A total of 60 studies were initially identified through the electronic searches. No additional articles were found through the search of the reference lists. Finally, 4 observational studies were included in this meta-analysis [12,13,14,15]. The baseline characteristics of these included studies were presented in Table 1. Two studies were from Korea [12, 15], 1 study from America [14], and 1 study from Spain [13]. Only the study of Dominguez et al. [13] used acenocoumarol as the reference, whereas warfarin was regarded as controls in other included studies [12, 14, 15]. The follow-up time of the included studies ranged from 0.6 to 5.3 years. All of the included studies had an acceptable quality with an NOS score of ≥ 6.
Random-effects model for comparing the efficacy outcomes of NOACs with VKAs in patients with AF and HCM. AF atrial fibrillation, HCM hypertrophic cardiomyopathy, NOACs non-Vitamin K antagonist oral anticoagulants, VKAs vitamin K antagonists, SSE stroke or systemic embolism, IS ischemic stroke, CI confidence interval, SE standard error, IV inverse of the variance
Efficacy and safety of NOACs versus VKAs
Efficacy
As shown in Fig. 1, compared with VKAs use, the use of NOACs was significantly associated with a reduced risk of IS (RR 0.49, 95% CI 0.34–0.69; P <0.0001) and all-cause death (RR 0.44, 95% CI 0.35–0.55; P <0.00001). We observed no difference in the rate of SSE (RR 0.94, 95% CI 0.73–1.21; P = 0.63) in patients with NOACs versus VKAs. In this part, no evidence of heterogeneity was found across the included studies (all I2= 0%).
Safety
As presented in Fig. 2, compared with VKAs use, the use of NOACs was significantly associated with a decreased risk of ICH (RR 0.43, 95% CI 0.24–0.77; P = 0.004; I2= 2%). There were no differences in the risks of major or clinically relevant bleeding (RR 0.76, 95% CI 0.46–1.26; P = 0.29; I2= 57%) and GI bleeding (RR 0.82, 95% CI 0.58–1.10; P = 0.17; I2= 23%) in patients with NOACs versus VKAs.
Random-effects model for comparing the safety outcomes of NOACs with VKAs in patients with AF and HCM. AF atrial fibrillation, HCM hypertrophic cardiomyopathy, NOACs non-Vitamin K antagonist oral anticoagulants, VKAs vitamin K antagonists, ICH intracranial hemorrhage, GI gastrointestinal, CI confidence interval, SE standard error, IV inverse of the variance
Sensitivity analysis
For the efficacy outcomes of NOACs versus VKAs, re-analyses with a fixed-effects model produced similar results as the main analyses (Supplemental Fig. 2). For the safety outcomes, the use of NOACs versus VKAs reduced the risks of major or clinically relevant bleeding (RR 0.75, 95% CI 0.59–0.96; P = 0.02) and ICH (RR 0.43, 95% CI 0.24–0.76; P = 0.004), but not GI bleeding (RR 0.81, 95% CI 0.62–1.06; P = 0.12) (Supplemental Fig. 3). We compared the efficacy and safety outcomes of NOACs with warfarin solely. As shown in Figs. 3 and 4, the pooled results did not change after we excluded the study of Dominguez et al. [13].
Random-effects model for comparing the efficacy outcomes of NOACs with warfarin in patients with AF and HCM. AF atrial fibrillation, HCM hypertrophic cardiomyopathy, NOACs non-Vitamin K antagonist oral anticoagulants, SSE stroke or systemic embolism, IS ischemic stroke, CI confidence interval, SE standard error, IV inverse of the variance
Random-effects model for comparing the safety outcomes of NOACs with warfarin in patients with AF and HCM. AF atrial fibrillation, HCM hypertrophic cardiomyopathy, NOACs non-Vitamin K antagonist oral anticoagulants, ICH intracranial hemorrhage, GI gastrointestinal, CI confidence interval, SE standard error, IV inverse of the variance
Discussion
In the present study, we first conducted a meta-analysis to compare the effect of NOACs versus VKAs in patients with HCM and AF. Our pooled data indicated that compared with VKAs use, the use of NOACs was associated with the reduced risks of IS, all-cause death, and ICH. There were no differences in the risks of SSE, major or clinically relevant bleeding, and GI bleeding in patients with NOACs versus VKAs. Re-analyses with a fixed-effects model produced the similar results as the main analyses. For the efficacy and safety outcomes, comparisons of NOACs versus warfarin produced the similar results as those of NOACs versus VKAs. Overall, in patients with HCM and AF, compared with VKAs, NOACs had similar or lower risks of thromboembolic and bleeding events and posed a reduced risk of all-cause death. Based on the published real-world studies, the use of NOACs was at least non-inferior to VKAs for stroke prevention in patients with HCM and AF.
Prior studies have indicated that VKAs such as warfarin, are the effective anticoagulants for reducing thromboembolic and bleeding events in patients with HCM and AF [7]. At present, there still have no RCTs to assess the role of NOACs in this high-risk population. Based on results from the previous studies taken together with our findings, the use of NOACs was associated with a lower risk of all-cause death compared with VKAs, especially for reducing the composite of fatal cardiovascular events [12]. NOACs might be effective and safe for stroke prevention in patients with HCM and AF. Jung et al. [12] reported that NOACs had a lower rate of all-cause death than VKAs in patients with HCM and AF irrespective of the NOAC type and dose. In addition, although the quality of life was similar, NOACs users had a higher treatment satisfaction than VKAs users [13]. In the post hoc analysis of RE-LY trial, dabigatran is superior to warfarin in reducing the efficacy outcomes in AF patients with left ventricle hypertrophy assessed by electrocardiogram [20]. Although this study did not examine the role of NOACs in AF patients with HCM directly, data from this study still suggested that AF patients with HCM might benefit from the treatment of NOACs [20].
All guidelines from different organizations including the American College of Cardiology, American College Of Cardiology Foundation, American Heart Association, European Society Of Cardiology, and Heart Rhythm Society uniformly recommend the lifelong oral anticoagulant therapy in HCM patients with AF [6, 21,22,23,24,25]. However, the recommendations for NOACs in HCM patients with AF remain unaligned. In 2011 American College Of Cardiology Foundation/American Heart Association guidelines, direct thrombin inhibitors (i.e., dabigatran) could be considered; however, evidence is unavailable [25]. The 2014 European Society Of Cardiology HCM guidelines proposed that NOACs could be recommended as the second-line drugs in patients with HCM and AF; [6] and the 2016 European Society Of Cardiology AF guidelines discuss the use of either VKAs or NOACs [26]. Since current recommendation for warfarin in patients with AF and HCM arises from observational data [7], our meta-analysis could give some confidences to clinicians when selecting the NOACs in this population. At least, the use of NOACs is a convenient anticoagulant choice that do not need the monitoring, and appears to be superior to VKAs in reducing the risk of death. As the use of NOACs becomes more widespread, further studies should take more factors into consideration to confirm our findings before arriving at a definitive conclusion.
Limitations
We acknowledged several limitations in this meta-analysis. First, some comparisons between NOACs versus warfarin were probably underpowered in terms of the limited sample size and small number of events. Second, we did not perform the subgroup analysis based on the type or dosage of NOACs due to the limited data. Third, the time in the therapeutic range of warfarin users was not considered. Fourth, due to the real-world data, the residual confounders should be considered when interpretation of our current results. Finally, HCM is a complex, genetic disease with a wide variety of phenotypes, ranging form apical variants to HCM with or without an outflow tract gradient, end-stage dilated cardiomyopathy and isolated apical aneurysms. The attendant risks of cardioembolic events may differ widely according to the phenotypes. Further study should address this in their analyses. Based on these limitations, we should interpret these findings cautiously, and these findings can not be completely generalizable to all HCM patients in clinical practice.
Conclusions
Based on current data from observational studies, compared with VKAs, NOACs had similar or lower rates of thromboembolic and bleeding events in patients with HCM and AF. NOACs might be reasonable alternatives to VKAs in patients with HCM and AF. These findings should be confirmed by including more prospective studies.
References
Staerk L, Sherer JA, Ko D, Benjamin EJ, Helm RH (2017) Atrial fibrillation: epidemiology, pathophysiology, and clinical outcomes. Circ Res 120(9):1501–1517
Guttmann OP, Rahman MS, O’Mahony C, Anastasakis A, Elliott PM (2014) Atrial fibrillation and thromboembolism in patients with hypertrophic cardiomyopathy: systematic review. Heart 100(6):465–472
Vaidya K, Semsarian C, Chan KH (2017) Atrial fibrillation in hypertrophic cardiomyopathy. Heart Lung Circ 26(9):975–982
Borer J, Atar D, Marciniak T, Kim M, Serebruany V (2019) Atrial fibrillation and stroke in patients with hypertrophic cardiomyopathy: important new insights. Thromb Haemosts 119(3):355–357
Jung H, Yang P, Sung J, Jang E, Yu H, Kim T, Uhm J, Kim J, Pak H, Lee M, Lip G, Joung B (2019) Hypertrophic cardiomyopathy in patients with atrial fibrillation: prevalence and associated stroke risks in a nationwide cohort study. Thromb Haemost 119(02):285–293
Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, Hagege AA, Lafont A, Limongelli G, Mahrholdt H, McKenna WJ, Mogensen J, Nihoyannopoulos P, Nistri S, Pieper PG, Pieske B, Rapezzi C, Rutten FH, Tillmanns C, Watkins H (2014) 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J 35(39):2733–2779
Maron BJ, Olivotto I, Bellone P, Conte MR, Cecchi F, Flygenring BP, Casey SA, Gohman TE, Bongioanni S, Spirito P (2002) Clinical profile of stroke in 900 patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 39(2):301–307
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, Waldo AL, Ezekowitz MD, Weitz JI, Špinar J, Ruzyllo W, Ruda M, Koretsune Y, Betcher J, Shi M, Grip LT, Patel SP, Patel I, Hanyok JJ, Mercuri M, Antman EM (2013) Edoxaban versus warfarin in patients with atrial fibrillation. New Engl J Med 369(22):2093–2104
Granger CB, Alexander JH, McMurray JJV, Lopes RD, Hylek EM, Hanna M, Al-Khalidi HR, Ansell J, Atar D, Avezum A, Bahit MC, Diaz R, Easton JD, Ezekowitz JA, Flaker G, Garcia D, Geraldes M, Gersh BJ, Golitsyn S, Goto S, Hermosillo AG, Hohnloser SH, Horowitz J, Mohan P, Jansky P, Lewis BS, Lopez-Sendon JL, Pais P, Parkhomenko A, Verheugt FWA, Zhu J, Wallentin L (2011) Apixaban versus warfarin in patients with atrial fibrillation. New Engl J Med 365(11):981–992
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Paolini JF, Berkowitz SD, Fox KAA, Califf RM (2011) Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. New Engl J Med 365(10):883–891
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener H, Joyner CD, Wallentin L (2009) Dabigatran versus warfarin in patients with atrial fibrillation. New Engl J Med 361(12):1139–1151
Jung H, Yang P, Jang E, Yu HT, Kim T, Uhm J, Kim J, Pak H, Lee M, Joung B, Lip GYH (2019) Effectiveness and safety of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation with hypertrophic cardiomyopathy. Chest 155(2):354–363
Dominguez F, Climent V, Zorio E, Ripoll-Vera T, Salazar-Mendiguchía J, García-Pinilla JM, Urbano-Moral JA, Fernández-Fernández X, Lopez-Cuenca D, Ajo-Ferrer R, Sanz-Sanchez J, Gomez-Perez Y, López-Garrido MA, Barriales-Villa R, Gimeno JR, Garcia-Pavia P (2017) Direct oral anticoagulants in patients with hypertrophic cardiomyopathy and atrial fibrillation. Int J Cardiol 248:232–238
Noseworthy PA, Yao X, Shah ND, Gersh BJ (2016) Stroke and bleeding risks in NOAC- and warfarin-treated patients with hypertrophic cardiomyopathy and atrial fibrillation. J Am Coll Cardiol 67(25):3020–3021
Lee H, Kim H, Jung J, Han K, Lee H, Park J, Kim HM, Kim Y, Ommen SR (2019) Novel oral anticoagulants for primary stroke prevention in hypertrophic cardiomyopathy patients with atrial fibrillation. Stroke 50(9):2582–2586
Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0[updated March 2011]. www.cochrane-handbook.org. Accessed Aug 10, 2019
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Wells GA, Shea B, O Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. 2014. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed Aug 10 2019
Zhu W, Guo L, Hong K (2016) Relationship between smoking and adverse outcomes in patients with atrial fibrillation: a meta-analysis and systematic review. Int J Cardiol 222:289–294
Verdecchia P, Reboldi G, Angeli F, Mazzotta G, Lip G, Brueckmann M, Kleine E, Wallentin L, Ezekowitz MD, Yusuf S, Connolly SJ, Di Pasquale G (2018) Dabigatran vs. warfarin in relation to the presence of left ventricular hypertrophy in patients with atrial fibrillation- the Randomized Evaluation of Long-term anticoagulation therapY (RE-LY) study. Europace 20(2):253–262
January CT, Wann LS, Calkins H, Field ME, Chen LY, Furie KL, Cigarroa JE, Heidenreich PA, Cleveland JJ, Murray KT, Ellinor PT, Shea JB, Ezekowitz MD, Tracy CM, Yancy CW (2019) 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm 16(8):e66–e93
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener HC, Heidbuchel H, Hendriks J, Hindricks G, Manolis AS, Oldgren J, Popescu BA, Schotten U, Van Putte B, Vardas P, Agewall S, Camm J, Baron Esquivias G, Budts W, Carerj S, Casselman F, Coca A, De Caterina R, Deftereos S, Dobrev D, Ferro JM, Filippatos G, Fitzsimons D, Gorenek B, Guenoun M, Hohnloser SH, Kolh P, Lip GYH, Manolis A, McMurray J, Ponikowski P, Rosenhek R, Ruschitzka F, Savelieva I, Sharma S, Suwalski P, Tamargo JL, Taylor CJ, Van Gelder IC, Voors AA, Windecker S, Zamorano JL, Zeppenfeld K (2016) 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Europace 18(11):1609–1678
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JJ, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW (2014) 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 64(21):e1–e76
JCS Joint Working Group (2014) Guidelines for pharmacotherapy of atrial fibrillation (JCS 2013). Circ J 78(8):1997–2021
Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, Naidu SS, Nishimura RA, Ommen SR, Rakowski H, Seidman CE, Towbin JA, Udelson JE, Yancy CW (2011) 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: executive summary: A report of the American College of cardiology foundation/American heart association task force on practice guidelines. Circulation 124(24):2761–2796
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener H, Heidbuchel H, Hendriks J, Hindricks G, Manolis AS, Oldgren J, Popescu BA, Schotten U, Van Putte B, Vardas P, Agewall S, Camm J, Baron Esquivias G, Budts W, Carerj S, Casselman F, Coca A, De Caterina R, Deftereos S, Dobrev D, Ferro JM, Filippatos G, Fitzsimons D, Gorenek B, Guenoun M, Hohnloser SH, Kolh P, Lip GYH, Manolis A, McMurray J, Ponikowski P, Rosenhek R, Ruschitzka F, Savelieva I, Sharma S, Suwalski P, Tamargo JL, Taylor CJ, Van Gelder IC, Voors AA, Windecker S, Zamorano JL, Zeppenfeld K (2016) 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 37(38):2893–2962
Funding
None.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhou, Y., He, W., Zhou, Y. et al. Non-vitamin K antagonist oral anticoagulants in patients with hypertrophic cardiomyopathy and atrial fibrillation: a systematic review and meta-analysis. J Thromb Thrombolysis 50, 311–317 (2020). https://doi.org/10.1007/s11239-019-02008-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-019-02008-3