Abstract
According to current guidelines prophylactic implantable cardioverter-defibrillator (ICD) therapy is recommended in patients with significantly impaired left ventricular systolic function. However, the recently published DANISH trial did not find a significantly lower long-term rate of death from any cause compared with usual clinical care in patients with non-ischemic cardiomyopathy. We investigated whether registry data from a multi-center ‘real-life’ registry on patients with non-ischemic cardiomyopathy are similar to this trial. The German Device Registry (DEVICE) is a nationwide, prospective registry with one-year follow-up investigating 5451 patients receiving device implantations in 50 German centers. The present analysis of DEVICE focused on patients with non-ischemic cardiomyopathy and a left ventricular ejection fraction ≤35% who received a prophylactic ICD. Out of 779 patients with symptomatic heart failure and nonischemic cardiomyopathy, 33.1% received a single chamber ICD (VVI), while 11.0% were implanted with a dual-chamber ICD (DDD), and 55.8% received a defibrillator system for cardiac resynchronization therapy. Median follow-up was 16.1 months. 90.7% were alive at follow-up, 9.3% had died during this period. Overall mortality after one year was 5.4%. Overall mortality one year after implantation was significantly increased in patients 68 years and older(7.9%) as compared to younger patients (59–68 years: 2.5%; < 59 years: 3.8%; p < 0.015). Data from the present registry support the recently published results of the DANISH trial. In particular the influence of an increased age as proven in the DANISH trial might also play a role in the present collective. This limits the potential beneficial effect of ICD therapy in particular in the elderly population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In patients with heart failure and left ventricular ejection fraction ≤ 35%, prophylactic implantation of an implantable cardioverter-defibrillator (ICD) is recommended in current guidelines (class I) [1]. ICD therapy significantly reduces the rate of sudden cardiac death as well as overall mortality in patients with ischemic cardiomyopathy [2,3,4]. In patients with non-ischemic cardiomyopathy and significantly impaired left ventricular function, studies did not display convincing effects on mortality [5,6,7].
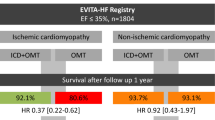
The Cardiomyopathy trial (CAT), published in 2002, with 104 patients suffering from dilated cardiomyopathy did not reveal significant effects in favor of ICD implantation in these patients [5]. In accordance, AMIOVIRT (Amiodarone versus implantable cardioverter-defibrillator: randomized trial in patients with nonischemic dilated cardiomyopathy and asymptomatic non-sustained ventricular tachycardia) was stopped prematurely as no significant differences between both study groups were observed [6]. On the other hand, the “Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy” trial (DEFINITE) which included 458 patients with dilated cardiomyopathy, a left ventricular ejection fraction of less than 36% and non-sustained ventricular tachycardia presented a significant reduction in the risk of sudden cardiac death as well as a nonsignificant reduction of overall mortality [7]. The only clinical trial that revealed a reduction of overall mortality in patients with nonischemic cardiomyopathy was the “Sudden cardiac death in heart failure” trial (SCD-HeFT) [4]. From this time, ICD implantation is regularly performed in patients with symptomatic heart failure and non-ischemic cardiomyopathy. However, the recent DANISH trial (Danish study to Assess the Efficacy of ICDs in Patients with Non-ischemic Systolic Heart Failure on Mortality) did not reveal a reduction of long-term mortality by ICD therapy compared with usual clinical care [8]. This in particular accounted for patients aged 68 years or older; while for younger patients below 59 years, beneficial effects of ICD therapy were observed [8]. According to a recent survey of the European Heart Rhythm Association, results of the DANISH study have already changed clinical decisions [9].
In the present study, data from a multi-center real-world registry on patients with non-ischemic cardiomyopathy are discussed in the light of the DANISH trial.
Methods
The German Device Registry is a nationwide, prospective database of ICD or CRT implantations and revisions which is organized by the Stiftung Institut für Herzinfarktforschung Ludwigshafen, Germany (IHF) [10]. In 50 participating centers, information on demographic data, indication for the device, implantation procedure, as well as peri-interventional complications was documented at the time of device operation. Recruitment of patients for the German Device Registry started in March 2007 until March 2011, then continued as Device II registry and was terminated in February 2014. After written informed consent, data were entered into an internet-based electronic case report form by the centers. Case report forms were thereafter transmitted encrypted with a secure socket layer and the IHF took responsibility for data management and monitoring. The present study includes symptomatic patients in NYHA classes II–IV with non-ischemic cardiomyopathy who received a first implantation of ICD for primary prevention (LVEF ≤ 35%). Exclusion criteria of the present analysis were coronary artery disease, secondary prevention, renal failure requiring haemodialysis and permanent atrial fibrillation with a resting heart rate > 100 beats per minute (Fig. 1). Follow-up contacts were scheduled one year after implantation or revision by telephone. The follow-up was performed by the IHF. During telephone contact questions on arrhythmias (e.g., syncope, resuscitation, ablation), cardiac events (e.g., myocardial infarction, revascularization), complications, medication, and heart failure symptoms were posed. In case of an ineffective call, further information was gathered from other caring physicians or civil registration offices.
Statistical analysis
The patient population is characterized by descriptive statistical measures. Categorical data are presented as percentages, metrical data as medians with 25th and 75th percentiles. The distribution of binary variables was compared between age groups by Pearson Chi-square test, and that of metrical variables by Mann–Whitney test. The shown baseline data are 99% complete except where indicated. The descriptive statistics are based on the available cases.
Observation time was calculated as the time span from the index intervention to the last follow-up contact. One-year mortality during 366 days was estimated using the Kaplan–Meier method.
The statistical computations were performed using SAS release 9.3 on a personal computer (SAS Institute, Inc., Cary, North Carolina, USA).
Results
Patient characteristics/demographics
Demographic characteristics are summarized in Table 1. Out of 5451 patients registered in DEVICE I and DEVICE II, 779 patients met the inclusion and exclusion criteria. Median age was 66 years (57; 73) and 589 patients (75.6%) were males. 258 patients (33.1%) received a single-chamber ICD (VVI), while 86 patients (11%) were implanted with a dual-chamber ICD (DDD) and 435 patients (55.8%) received a defibrillator system for cardiac resynchronization therapy (CRT). All included patients presented symptomatic heart failure. 246 patients (31.6%) were in NYHA class II, 492 patients (63.2%) in NYHA class III and 41 patients (5.3%) in NYHA class IV. Median left ventricular ejection fraction was 25% (20%, 30%). 201 patients (25.8%) had diabetes; while hypertension was diagnosed in 371 patients (47.7%). Renal insufficiency not requiring hemodialysis was present in 129 patients (16.6%). ECG findings and rhythm disorders are summarized in Table 1.
Implantation procedure
530 patients (72.6%) underwent perioperative defibrillation testing which was successful in 527 patients (99.4%) and failed in three patients (0.6%). Severe peri-interventional complications were observed in five patients (0.5%). These included pericardial effusion requiring pericardiocentesis (n = 1), hematothorax (n = 1) and pneumothorax (n = 3). 778 patients (99.9%) were discharged, while one patient died in hospital. This event was classified as sudden cardiac death.
Relevant cardiovascular medication is displayed in Table 2. Of note, 188 patients (24.2%) received digitalis glycosides. 66 patients (8.5%) were treated with class-III antiarrhythmic agents.
Follow-up
Follow-up information was obtained for 755 (96.9%) of the 779 patients at a median observation time of 16.1 months (13.1; 19.7), and for 23 patients, observation time was restricted to hospital stay. 706 patients (90.7%) were alive at their last contact, while 72 patients (9.3%) had died during their observation period. 34 patients (47.2%) died of unknown cause. 25 deaths (34.7%) were classified as cardiovascular, while 13 deaths (18.1%) were classified as non-cardiovascular deaths. Estimated 1-year overall mortality was 5.4%. The rate of major adverse cardiac and cerebrovascular events (MACCE; including death, myocardial infarction and stroke) was 6% (n = 45) after 1 year. 77 patients (10.9%) experienced shock deliveries of the implanted ICD. Syncope occurred in 15 patients (2.1%) and electrical storm was documented in 9 patients (1.6%).
Sub-analyzes
A more detailed sub-analysis between NYHA classes II and III displayed a trend towards an increased 1-year mortality (5.9% vs. 3.0%, p = 0.078) and significant differences regarding severe adverse events including death, myocardial infarction and stroke in NYHA III patients (6.9% vs. 2.9%, p = 0.026). In accordance, rehospitalization was also increased in NYHA III patients (44.4% vs. 34.0%, p = 0.017).
Regarding a potential effect of CRT, a significantly elevated proportion of clinical heart failure, atrioventricular conduction disturbances, bundle branch block and prevalence of atrial fibrillation was observed in CRT patients compared with ICD patients. Left ventricular ejection fraction did not differ between both groups. Of note, during follow-up, no differences regarding mortality or major adverse events were observed. However, CRT patients reported a significant improvement of NYHA class as compared with ICD patients.
Role of age at implantation
According to the analysis of the DANISH study, patients were divided into three subgroups regarding their age at the time of implantation (Table 3). 221 patients (28.5%) were younger than 59 years, 200 patients (25.8%) were between 59 and 67 years and 355 patients (45.7%) were 68 years or older. Younger patients were significantly more often implanted with VVI ICD systems (< 59 years: 42.1%; 59 to < 68 years: 38.0%) than patients of 68 years or older (24.8%, p < 0.001). The rate of CRT–ICD implantations was significantly higher in patients older than 68 years (66.2%) as compared with younger patients (< 59 years: 47.5%; 59 to < 68 years: 46.5%, p < 0.001). Hypertension and renal failure were present more often in older patients than in younger patients. In accordance, atrial fibrillation as well as left bundle branch block was more frequently present in older patients. Median QRS duration was 150 ms (120, 170) in patients 68 years and older, 130 ms (100; 160) in patients 59 to < 68 years and 125 ms (100; 160) in patients younger than 59 years (p < 0.001). Regarding peri-interventional complications, no significant differences between these subgroups were observed. Overall mortality 1 year after implantation was significantly higher in patients of 68 years and older (7.9%) as compared with the other study groups (59 to <68 years: 2.5%; < 59 years: 3.8%; p < 0.015; Fig. 2a). In accordance, MACCE occurred more frequently in older patients (9.0% vs. 3.0% and 3.8%, p < 0.005). A trend towards more frequent shock deliveries as a correlate of arrhythmic events was observed in younger patients (< 59 years: 15.1%) as compared with older patients (59 to <68 years: 13.6%;> 68 years: 11.0%), although this did not reach statistical significance. No significant differences regarding syncope were observed, while electrical storm occurred more often in younger patients (< 59 years: 3.7%; > 68 years: 1.3%, p = 0.029).
Discussion
The results of the present study support the recently published results of the DANISH trial. These results contradict those of a recent meta-analysis where similar results regarding mortality were reported for both patients with ischemic and non-ischemic heart disease [11]. A further meta-analysis also suggested a survival benefit mediated by ICD therapy in patients with dilated cardiomyopathy [12].
Patient collective and demographics
Patient characteristics of the present registry and the multicenter randomized DANISH study [8] match very well. Basic characteristics such as median age, gender, body mass index, and median blood pressure were very similar. Median left ventricular ejection fraction was identical in both collectives. Median QRS duration was also similar in both studies. Of note, the proportion of CRT implantations was 55.8% in the present registry and 58% in the DANISH study [8]. Regarding NYHA classification, slight differences between both collectives were observed. In the present registry, more patients were classified as NYHA III (63.2% vs. 45%) or NYHA IV (5.3% vs. 1%) as compared with the DANISH population indicating that heart failure was more symptomatic in DEVICE. Heart failure medication was also similar in both populations. This accounts for ACE inhibitors, beta-blockers, and mineralocorticoid receptor antagonists.
Follow-up and age-dependent effects
Mortality as well as the rate of major cardiovascular and cerebrovascular events is almost equivalent to values reported in DANISH after one year. In addition, NYHA class exerted significant effects on major adverse events and rehospitalizations.
Of course, follow-up duration of the DANISH study was longer with a median of more than 67 months. Due to the characteristics of DEVICE, the cause of death remained unknown in the present collective. In contrast, in the randomized DANISH study, the follow-up was more detailed. Nonetheless, the above-described event rates regarding overall mortality are similar. The congruence with the results of the present ‘real-life’ DEVICE registry again underlines the transferability of the results of the DANISH study to clinical practice.
The results of the DANISH study suggested that ICD implantation in patients with nonischemic heart disease did not result in an overall benefit in terms of mortality, although the rate of sudden cardiac death was significantly reduced [8]. Of note, an important role of age was reported. In the subgroup of patients younger than 59 years, beneficial effects of ICD therapy in terms of total mortality were observed. Besides, in patients between 59 and 68 years, there was a trend towards a reduction in mortality. These effects were independent of implantation of a CRT–ICD or a single-or dual-chamber ICD. These implied that in patients with non-ischemic cardiomyopathy, the cause of death may vary over time and non-cardiovascular death may be less prominent in older patients, which questions the value of ICD implantation in older patients with non-ischemic cardiomyopathy. The authors of the study speculated that optimized medical treatment and CRT therapy may have lowered the risk of arrhythmic death. In accordance, in the present DEVICE registry, patients older than 68 years also presented a significantly increased overall mortality as compared with younger patients. Furthermore, the risk of major cardiac and cerebrovascular events was also significantly higher in this group. Regarding shock deliveries, a trend towards more arrhythmic events in younger patients was observed. However, this trend did not reach statistical significance, which is most likely due to the limited follow-up duration of one year.
Limitations
As the present data are derived from a registry, several limitations are obvious. Due to the design of the registry, a selection bias may be present as patient selection may not have been as strict as in randomized clinical trials. Furthermore, collection of complementary data is not as thorough as it usually is in randomized trials. In particular, there is no direct control group in this registry. Of note, the follow-up duration of one year is rather short in particular with regard to the DANISH study, where a follow-up duration of more than 5.5 years was achieved. This represents an important limitation. In addition, no direct control group for this registry is available. A comparison with other registries is impeded by inclusion and exclusion criteria that significantly differ from the present registry. Furthermore, a comparison with a matched cohort of patients with ischemic cardiomyopathy is not available. Therefore, the results were compared with the population of the DANISH study. Nonetheless, the results of the present study represent ‘real-life’ data in patients with non-ischemic cardiomyopathy that after a follow-up duration of one year are very congruent to the results of DANISH [8] and thereby, further support the conclusion of this important clinical trial.
Conclusion
Data from the present registry support the recently published results of the DANISH trial where prophylactic ICD implantation in patients with symptomatic systolic heart failure in non-ischemic cardiomyopathy was not associated with a significantly lower long-term rate of death from any cause than was usual clinical care. According to DANISH, a significant interaction with age suggested that younger patients might have a survival benefit that is not preserved in older patients. This was consistent in the present study. The results of the DANISH study have already led to changes of ICD indications according to a recent survey of the European Heart Rhythm Association [9]. The present DEVICE data clearly support this approach, although further data from randomized controlled trials are definitely needed.
References
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, ESC Scientific Document Group (2016) 2016 esc guidelines for the diagnosis and treatment of acute and chronic heart failure: The task force for the diagnosis and treatment of acute and chronic heart failure of the European society of cardiology (ESC)developed with the special contribution of the heart failure association (HFA) of the ESC. Eur Heart J 37:2129–2200
Moss AJ, Hall WJ, Cannom DS, Daubert JP, Higgins SL, Klein H, Levine JH, Saksena S, Waldo AL, Wilber D, Brown MW, Heo M (1996) Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter automatic defibrillator implantation trial investigators. N Engl J Med 335:1933–1940
Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, Daubert JP, Higgins SL, Brown MW, Andrews ML, Multicenter Automatic Defibrillator Implantation Trial II Investigators (2002) Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 346:877–883
Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH, Sudden Cardiac Death in Heart Failure Trial Investigators (2005) Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 352:225–237
Bansch D, Antz M, Boczor S, Volkmer M, Tebbenjohanns J, Seidl K, Block M, Gietzen F, Berger J, Kuck KH (2002) Primary prevention of sudden cardiac death in idiopathic dilated cardiomyopathy: the cardiomyopathy trial (cat). Circulation 105:1453–1458
Strickberger SA, Hummel JD, Bartlett TG, Frumin HI, Schuger CD, Beau SL, Bitar C, Morady F, AMIOVIRT Investigators (2003) Amiodarone versus implantable cardioverter-defibrillator: randomized trial in patients with nonischemic dilated cardiomyopathy and asymptomatic nonsustained ventricular tachycardia–amiovirt. J Am Coll Cardiol 41:1707–1712
Kadish A, Dyer A, Daubert JP, Quigg R, Estes NA, Anderson KP, Calkins H, Hoch D, Goldberger J, Shalaby A, Sanders WE, Schaechter A, Levine JH, Defibrillators in Non-Ischemic Cardiomyopathy Treatment Evaluation Investigators (2004) Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med 350:2151–2158
Kober L, Thune JJ, Nielsen JC, Haarbo J, Videbaek L, Korup E, Jensen G, Hildebrandt P, Steffensen FH, Bruun NE, Eiskjaer H, Brandes A, Thogersen AM, Gustafsson F, Egstrup K, Videbaek R, Hassager C, Svendsen JH, Hofsten DE, Torp-Pedersen C, Pehrson S, DANISH Investigators (2016) Defibrillator implantation in patients with nonischemic systolic heart failure. N Engl J Med 375:1221–1230
Haugaa KH, Tilz R, Boveda S, Dobreanu D, Sciaraffia E, Mansourati J, Papiashvili G, Dagres N (2017) Implantable cardioverter defibrillator use for primary prevention in ischaemic and non-ischaemic heart disease-indications in the post-danish trial era: results of the European heart rhythm association survey. Europace 19:660–664
Kobe J, Andresen D, Maier S, Stellbrink C, Kleemann T, Gonska BD, Reif S, Hochadel M, Senges J, Eckardt L (2017) Complications and 1-year benefit of cardiac resynchronization therapy in patients over 75 years of age—insights from the German device registry. Int J Cardiol 228:784–789
Shun-Shin MJ, Zheng SL, Cole GD, Howard JP, Whinnett ZI, Francis DP (2017) Implantable cardioverter defibrillators for primary prevention of death in left ventricular dysfunction with and without ischaemic heart disease: a meta-analysis of 8567 patients in the 11 trials. Eur Heart J 38:1738–1746
Wolff G, Lin Y, Karathanos A, Brockmeyer M, Wolters S, Nowak B, Furnkranz A, Makimoto H, Kelm M, Schulze V (2017) Implantable cardioverter/defibrillators for primary prevention in dilated cardiomyopathy post-danish: an updated meta-analysis and systematic review of randomized controlled trials. Clin Res Cardiol 106:501–513
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Karlheinz Seidl reported lecture honoraria from Medtronic and St. Jude Medical. All other authors declared no conflict of interest related to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Frommeyer, G., Andresen, D., Ince, H. et al. Can we rely on Danish? Real-world data on patients with nonischemic cardiomyopathy from the German Device Registry. Heart Vessels 34, 1196–1202 (2019). https://doi.org/10.1007/s00380-018-01337-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-018-01337-2