Abstract
Background
Sudden cardiac death (SCD) is frequent in patients with heart failure due to dilated cardiomyopathy (DCM). Implantable cardioverter/defibrillator (ICD) device therapy is currently used for primary prevention. However, publication of the DANISH trial has recently given reason for doubt, showing no significant improvement in all-cause mortality in comparison to contemporary medical therapy.
Methods
We performed a meta-analysis of all randomized controlled trials comparing ICD therapy to medical therapy (MT) for primary prevention in DCM. The primary outcome was all-cause mortality; secondary analyses were performed on sudden cardiac death, cardiovascular death and non-cardiac death.
Results
Five trials including a total of 2992 patients were included in the pooled analysis. Compared to contemporary medical treatment there was a significant mortality reduction with ICD device therapy [odds ratio (OR) 0.77, 95% confidence interval (CI) 0.64–0.93; p = 0.006]. SCD was decreased significantly (OR 0.43, CI 0.27–0.69; p = 0.0004), while cardiovascular death and non-cardiac death showed no differences. Sensitivity analyses showed no influence of amiodarone therapy on overall results. Analysis of MT details revealed the DANISH population to adhere the most to current guideline recommendations. In addition, it was the only study including a substantial amount of CRT devices (58%).
Conclusions
Our meta-analysis of all available randomized evidence shows a survival benefit of ICD therapy for primary prevention in DCM. DANISH results suggest an attenuation of this ICD advantage when compared to contemporary medical and cardiac resynchronization therapy. Until larger trials have confirmed this finding, ICD therapy should remain the recommendation for primary prevention of SCD in DCM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart failure patients with reduced ejection fraction (HFrEF) are at increased risk for arrhythmic events and sudden cardiac death (SCD) [1, 2], and its prevention has been a clinical subject of interest for more than 25 years [3–5]. Implantable cardioverter/defibrillator (ICD) device therapy has been shown to reduce SCD and all-cause mortality in primary [6–8] and secondary [9–12] prevention. The guidelines of the European Society of Cardiology (ESC) [13, 14] and the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) [15] give class 1 recommendations for implantation of ICD devices for primary prevention in symptomatic (NYHA II-III) HFrEF patients with EF ≤35% despite optimal medical therapy for ≥3 months.
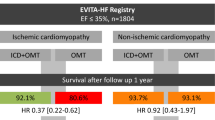
The etiology of heart failure thus far is not of immediate concern for ICD indication. Although some authors believe patients with ischemic cardiomyopathy (ICM) to be at greater risk of arrhythmic events [13, 16], other studies have found equal hazards [17, 18]. While there is strong evidence in ICM demonstrating ICD benefits in primary prevention [6, 7, 19], randomized trial data in dilated cardiomyopathy (DCM) patients have been limited to small trials and subgroup analyses. Based on meta-analyses [16, 20], guidelines give IA (ACCF/AHA) [15] and IB (ESC) [13, 14] recommendations for primary prevention until now.
The recent publication of the DANISH trial [21] has evoked discussion about this recommendation, as it showed no mortality benefit of ICD therapy for primary prevention in HFrEF patients with DCM. Since this study has substantially altered the available evidence in this field, we here aimed to present an updated meta-analysis and systematic review of current randomized data on ICD therapy for primary prevention in DCM patients.
Materials and methods
Data sources and search strategy
This meta-analysis was performed according to established methods recommended by the Cochrane guidelines [22] and in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for conducting systematic reviews and meta-analyses in health care interventions [23].
We performed a systematic literature search of English articles published until September 10th 2016 in the medical databases of MEDLINE, EMBASE, Google Scholar, Web of Science and the Cochrane Controlled Trials Register. Search terms according to medical subjects headings included: dilated cardiomyopathy, internal cardioverter defibrillator, defibrillator, ICD, DCM, primary prevention, heart failure, sudden cardiac death, cardiac resynchronization therapy and CRT. A bibliography search within landmark articles, meta-analyses and guidelines of cardiac societies on the subject was additionally performed. Relevant citations were screened at the title/abstract level and retrieved as full-text reports.
Study design, selection criteria and outcome measures
This meta-analysis was designed to compare survival after ICD implantation for primary prevention of sudden cardiac death to medical therapy in patients with dilated cardiomyopathy and heart failure with severely reduced left ventricular ejection fraction ≤35%. All prospective randomized controlled trials in this patient population comparing ICD implantation to a conservative strategy of medical therapy with a minimum follow-up of 24 months and reporting all-cause mortality were eligible for inclusion. Exclusion criteria were: (1) non-randomized study; (2) less than 24 months of follow-up; (3) secondary prevention study; (4) no full-text available; (5) article not in English language.
The primary clinical endpoint was all-cause mortality; secondary endpoints were cardiovascular mortality, sudden cardiac death and non-cardiac mortality.
Data abstraction and quality assessment
The most updated or inclusive data for each study were used for abstraction. An independent investigator (YL), who was not personally involved in any of the included trials, performed the primary data abstraction from each report into pre-specified forms. Data were abstracted according to the intention-to-treat principle. Due to lack of reporting, data on the amiodarone group in SCD-HeFT [19] was extracted from the Kaplan–Meier curve. Internal validity was independently appraised by three investigators (GW, AK, VS); divergences were resolved by discussion in the group (GW, AK, YL, HM, AF, VS). Bias assessment was performed based on the Cochrane Handbook recommendations [22].
Sensitivity analyses were performed to ascertain validity of the meta-analysis results.
Statistical analyses
Odds ratios (OR) and 95% confidence intervals (CI) were used as summary statistics. Heterogeneity was assessed by the Cochran’s Q test, and statistical heterogeneity was summarized by the I 2 statistic, which quantifies the percent of variation in study results that is due to heterogeneity rather than to chance [24]. I² values >20% indicate substantial heterogeneity, which prompted the use of the more conservative DerSimonian and Laird random-effects model [22, 25], instead of the otherwise used fixed-effects model.
A two-tailed p value <0.05 for summary odds ratios was assumed to indicate statistical significance. Review manager, version 5.3 (The Nordic Cochrane Centre, Copenhagen, Denmark), and Microsoft Excel were used for statistical analyses.
Results
Study selection and patient populations
The process of article screening and selection is described in a PRISMA flowchart (Fig. 1). Of a total of 5167 articles retrieved from the primary searches using pre-specified keywords, 4286 were excluded on the basis of title/abstract and another 801 after article screening. After a detailed evaluation of the remaining 80 articles, 75 were excluded for unmet inclusion criteria.
Five prospective randomized controlled trials published between 2002 and September 2016 were finally included in the meta-analysis (Table 1): the amiodarone vs implantable cardioverter–defibrillator trial (AMIOVIRT) [26], the cardiomyopathy trial (CAT) [8], the Danish study to assess the efficacy of ICDs in patients with non-ischemic systolic heart failure on mortality (DANISH) [21], defibrillators in non-ischemic cardiomyopathy treatment evaluation (DEFINITE) [27] and the sudden cardiac death in heart failure trial (SCD-HeFT) [19].
Patient baseline characteristics of all available trials are shown in Table 2. Details on patients in SCD-HeFT were taken from the overall population, as the authors did not report details for the subpopulation of nonischemic patients. SCD-HeFT mortality in DCM patients was not directly reported and thus abstracted from the Kaplan–Meier curve and secondary literature [16]. Of a total of 2992 patients (mean age 61 years, 74% male, mean EF 24%), 1284 were allocated to ICD implantation and compared to 1708 patients treated with medical therapy only. Median follow-up ranged from 24 months (AMIOVIRT [26]) to 68 months (DANISH [21]). Patient enrollment varied from 1991–1997 (CAT) to 2008–2014 (DANISH). Largest studies were DANISH (1116 patients) and SCD-HeFT (1211), while AMIOVIRT and CAT were smallest (103/104 patients, respectively).
The risks of bias of the included studies are summarized in Table 5. Overall, bias is mainly derived from incomplete blinding or failure of blinding reporting, while the study quality in general was very high.
Primary endpoint all-cause mortality in patients with ICD compared to medical therapy
SCD-HeFT [19] and DANISH [21] trials both contributed ~40% of study weight to the pooled analysis. The summary odds ratio showed a significant reduction in all-cause mortality in patients with ICD compared to medical therapy only (OR 0.77, CI 0.64–0.93; I² = 0%; p = 0.006; Fig. 2a). Statistical heterogeneity was low between trials, allowing use of the fixed-effects model.
Individual and summary odds ratios for the primary endpoint of all-cause mortality in studies comparing ICD vs medical therapy. a All-cause mortality in all included trials, b sensitivity analysis of trials without amiodarone, c sensitivity analysis of groups/trials comparing ICD to amiodarone therapy. M–H Mantel–Haenszel; I² describes heterogeneity among studies
Sensitivity analyses
Selective exclusion of trials was performed to determine the impact of singular studies on overall results (Fig. 3). SCD-HeFT [19] was the only trial advocating a significant advantage of ICD over medical therapy on its own, while the other four studies showed no significant differences. Due to its study weight of 38.7%, exclusion of SCD-HeFT resulted in loss of significant difference in the pooled analysis (Fig. 3b), while exclusion of any other study had no effect on overall results (Fig. 3a, c–e).
Two studies explicitly included patients under amiodarone therapy (AMIOVIRT [26] and SCD-HeFT [19]). To exclude outcome-relevant antiarrhythmic effects of amiodarone in these patients, we performed a sensitivity analysis excluding the SCD-HeFT amiodarone group and AMIOVIRT trial. The summary odds ratio was similar to overall results (OR 0.79, CI 0.65–0.96; I² = 0%; p = 0.02; Fig. 2b). In an analysis of these two amiodarone groups compared to ICD treatment, we found an advantage of device therapy comparable to the results of ICD vs MT (OR 0.65, CI 0.47–0.92; I² = 0%, p = 0.01; Fig. 2c), albeit with heavy weight on the SCD-HeFT group (92.7%).
Additional analysis with the more conservative random-effects model [25] did not lead to any change of results.
Secondary endpoints in ICD vs MT
Cardiovascular death
Four trials [8, 21, 26, 27] involving 1781 patients reported cardiovascular death, with the majority of analysis weight on the DANISH study ([21], 84%). No singular trial showed a statistically significant benefit of ICD implantation for cardiovascular mortality. Pooled meta-analysis showed no statistically significant mortality reduction in the ICD group (OR 0.83, CI 0.62–1.12; I² = 0%; p = 0.23; Fig. 4a).
Sudden cardiac death
Four trials with a total of 1781 patients reported data on sudden cardiac death, two of them (DEFINITE and DANISH [21, 27]) being statistically in favor of ICD implantation. CAT was not estimable due to zero event rates [8]. The pooled analysis showed a significant reduction in the summary odds for patients with ICD (OR 0.43, CI 0.27–0.69; I² = 0%; p = 0.0004; Fig. 4b).
Non-cardiac death
Three trials involving 1323 patients reported non-cardiac death, once more with the majority of the study weight on DANISH [21]. The summary odds for non-cardiac death were not statistically different between groups (OR 1.18, CI 0.76–1.83; I² = 0%; p = 0.47; Fig. 4c).
Medical therapy details
Medical therapy for heart failure of all included trials is presented in Table 3.
While treatment with angiotensin-converting enzyme inhibitors (ACEI)/angiotensin receptor blockers (ARB) or diuretics was consistently used in a large majority of patients, betablocker (BB) usage differed substantially between studies (4–92%), as well as therapy with mineralocorticoid receptor antagonists (MRA). Details on medical therapy for SCD-HeFT patients with dilated cardiomyopathy were not available from the published report, which is why we reported details of the overall mixed population of ICM and DCM patients.
Cardiac resynchronization therapy (CRT) devices for eligible patients were used in the DANISH [21] trial, while all other included trials resorted to ICD devices only. In DANISH, 58% of patients in intervention as well as control group were treated with CRT.
Arrhythmia, shock therapy and device-related complications
Available data for arrhythmia and shock therapy of all included trials are presented in Table 4.
Four of the included trials [8, 21, 26, 27] reported rates of appropriate ICD shock therapy. When normalized to study patient count and follow-up duration, average appropriate shock therapy per patient and month of FU was lowest in DANISH [21] with 0.2% shocks per patient and month, and highest in AMIOVIRT [26] with 1.3 shocks per patient and month. Interestingly, inappropriate shock therapy was frequent, accounting for 1/3 of shocked patients in DANISH [21] and more than ½ of shocked patients in DEFINITE [27].
Four of the included trials [8, 19, 21, 27] reported device-related complications (Table 4). However, reports were very inconsistent between trials and obtainable information was scarce, limiting analysis severely. We can conclude that roughly 5–10% of implanted patients experienced longer-term device-related complications (Table 4).
Discussion
The present article—to the best of our knowledge—represents the most updated pooled analysis and systematic review of randomized trials comparing clinical outcomes in patients with dilated cardiomyopathy after primary prevention ICD implantation compared to medical therapy. Our main findings are: (a) overall results show reduced odds for all-cause mortality in favor of ICD therapy; (b) sudden cardiac death is reduced by ICD therapy, while cardiovascular death and non-cardiac death are not different; (c) amiodarone treatment appears to be inferior to ICD implantation in reducing mortality risk.
Compared to primary prevention ICD therapy for ICM HFrEF patients, which has already been well evaluated [6, 7, 19], the guideline recommendation in DCM has been based on a subgroup analysis of the SCD-HeFT trial and meta-analyses alone [16, 20], since no dedicated clinical trial has thus far shown a survival benefit on its own. DANISH was designed to provide this additional information with a projected mortality advantage of 25%; however, its results left us with more questions than answers in this regard, as it did not show significant differences with the included patient count.
Our main analysis of all-cause mortality adds the DANISH data to a wider perspective for the first time. While DANISH did not yield an all-cause mortality reduction, the pooled analysis of all five randomized trials shows a clear survival benefit of ICD therapy for primary prevention in DCM heart failure patients (OR 0.66, p = 0.006), comparable to the results of previous meta-analyses on the subject [16, 20]. The analyzed data set is statistically homogenous (I² = 0) and all trials—including DANISH—tend toward mortality reduction by ICD, which gives confidence in the validity of the cumulative analysis result. The result was driven mainly by a strong reduction in sudden cardiac death (OR 0.43 in favor of ICD), while cardiovascular death and non-cardiac death showed no differences (Fig. 4). This displays that SCD—although frequent with ~30% [3]—is not the most common cause of death in heart failure patients with DCM. The robustness of our analysis is further backed by the performed sensitivity analyses.
The only study comparable in size to the DANISH trial thus far was SCD-HeFT, which showed survival benefits of ICD therapy compared to medical therapy in 2005. The DANISH authors attributed the observed difference in study outcomes to improvement of heart failure therapy and increasing use of CRT in these 10 years since enrollment for SCD-HeFT.
Optimal medical heart failure therapy including the first-line use of betablockers (BB, [28, 29]), angiotensin-converting enzyme inhibitors (ACEI, [30, 31]) and mineralocorticoid receptor antagonists (MRA, [32, 33]) has proven its benefits for prevention of SCD, reducing all-cause mortality and worsening heart failure. Indeed, the DANISH population has the greatest adherence to current guideline-directed pharmacologic therapy, as shown in Table 3 (92% BB, 97% ACEI/ARB and 58% MR). While ACEI/ARB therapy was consistently frequent in all trials with a weighted mean of 97%, BB usage differed, especially between DANISH and SCD-HeFT. In addition, Digoxin is slowly removed from standard heart failure therapy [13], while it was still a prominent drug in AMIOVIRT, CAT and SCD-HeFT and thus may have impacted on clinical outcomes. New pharmacologic treatments such as angiotensin receptor neprilysin inhibitors (ARNI [34]) and funny channel inhibitors [35, 36] have shown promising results in recent trials and have subsequently received guideline support [13], but have not found their way into ICD studies yet and thus were not part of the current analysis.
Two sensitivity analyses were performed on the effect of amiodarone therapy, which did not reveal an amiodarone benefit in HFrEF patients with DCM. The analysis of amiodarone therapy vs ICD (Fig. 2c) in SCD-HeFT and AMIOVIRT showed an advantage of ICD therapy on survival (p = 0.01), although with heavy weight on the SCD-HeFT populations (92.7% weight). Moreover, removal of amiodarone treatment groups from the overall all-cause mortality analysis did not change the results either (p = 0.02 in favor of ICD; Fig. 2b). This is in line with current ESC guideline recommendations, which do not support amiodarone in patients with HFrEF for primary prevention of arrhythmic death [13].
Cardiac resynchronization therapy receives Class I recommendations in current ESC [13, 14] and ACCF/AHA [15] heart failure guidelines for patients with symptomatic heart failure with EF ≤35% and QRS duration ≥150 ms in sinus rhythm for symptom relief and reduction of morbidity and mortality, and the newest update of the 2016 ESC guidelines also gives a class IB recommendation to CRT in patients with ≥130 ms with left bundle-branch block (LBBB) morphology. CRT has been shown to improve symptoms and reduce mortality in eligible HFrEF patients in several trials [37, 38] and meta-analyses [39–41], while the effect on sudden cardiac death (SCD) remains uncertain [38, 42]. CRT in addition to ICD therapy is also significantly superior to ICD alone in MADIT-CRT [43]. Usage of CRT devices in the five included trials was overall too low to allow further analysis, with the DANISH trial being the only study with a significant proportion (58%) of CRT patients. This increases heterogeneity and is a limitation of the current analysis, but may explain improved outcomes in the DANISH control group.
There is ongoing discussion about appropriate selection of patients for ICD implantation based on patient age. The DANISH subgroup of patients <59 years of age showed a significant ICD benefit, whereas overall analysis of patients with mean age of 64 years did not. While this increase in ICD benefit in younger patients appears plausible, results in elderly patients are inconsistent in previous studies [44–46] and thus need to be interpreted with care. Guidelines do not recommend ICD implantation in patients with a life expectancy of less than 1 year [13, 15]. However, they leave the decision about device therapy in special age groups to the treating physician.
Our review suggests attenuation—but not loss—of ICD therapy effect size compared to MT by addition of DANISH data. Contemporary CRT and pharmacological therapy benefits compared to older trials may partially explain this result. The number-needed-to-treat in primary prevention ICD device therapy is believed to be around six device implantations for the prevention of one SCD in 5 years [47, 48], but DANISH suggests that this figure might not be true anymore. If the observed trend through improvement of medical therapy proves true in future trials, even more advanced medication might someday make ICD device therapy futile for primary prevention.
The main limitations of the current analysis lie in reporting bias of SCD-HeFT (Table 5; [19]): data on secondary outcomes, patient characteristics and details on amiodarone therapy (Tables 1, 2, 3, 4) were not available selectively for DCM patients, which weakens interpretation. While being a necessity of the current analysis, the long time period between CAT and DANISH enrollment and the observed change in medical therapy additionally limits the analysis and calls for contemporary trials to answer the questions DANISH has evoked.
Conclusion
ICD device therapy for primary prevention in heart failure patients with dilated cardiomyopathy shows all-cause mortality benefits in our pooled analysis of all randomized controlled trials to date and thus supports current guideline recommendations. Recently published DANISH data, however, suggest an attenuation of ICD benefit compared to modern medical and cardiac resynchronization therapy. As special patients (age) groups potentially profit variably from device therapy, a careful therapy selection is mandatory to gain an optimal risk/benefit ratio for the patient. However, until the DANISH evidence is confirmed in adequately powered randomized trials with modern medical treatment, ICD therapy should remain the therapy of choice for primary prevention of sudden cardiac death in dilated cardiomyopathy.
Abbreviations
- ACEI:
-
Angiotensin-converting enzyme inhibitor
- ARB:
-
Angiotensin receptor blocker
- ARNI:
-
Angiotensin receptor neprilysin inhibitor
- ATP:
-
Antitachycardia pacing
- BB:
-
Betablocker
- CA:
-
Cardiac arrest
- CAD:
-
Coronary artery disease
- CVD:
-
Cardiovascular death
- CHF:
-
Congestive heart failure
- CI:
-
Confidence interval
- CRT:
-
Cardiac resynchronization therapy
- DI:
-
Device infection
- DCM:
-
Dilated cardiomyopathy
- FU:
-
Follow-up
- HFrEF:
-
Heart failure with reduced ejection fraction
- ICD:
-
Implantable cardioverter/defibrillator
- ICM:
-
Ischemic cardiomyopathy
- LBBB:
-
Left bundle-branch block
- MT:
-
Medical therapy
- MRA:
-
Mineralocorticoid receptor antagonist
- OR:
-
Odds ratio
- RBBB:
-
Right bundle branch block
- SCD:
-
Sudden cardiac death
References
Franciosa JA, Wilen M, Ziesche S, Cohn JN (1983) Survival in men with severe chronic left ventricular failure due to either coronary heart disease or idiopathic dilated cardiomyopathy. Am J Cardiol 51:831–836
Zipes DP, Wellens HJJ (1998) Sudden cardiac death. Circulation 98:2334–2351
Tamburro P, Wilber D (1992) Sudden death in idiopathic dilated cardiomyopathy. Am Heart J 124:1035–1045
Sweeney MO, Ruskin JN (1994) Mortality benefits and the implantable cardioverter-defibrillator. Circulation 89:1851–1858
Uretsky BF, Sheahan RG (1997) Primary prevention of sudden cardiac death in heart failure: will the solution be shocking? J Am Coll Cardiol 30:1589–1597
Moss AJ, Hall WJ, Cannom DS et al (1996) Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter automatic defibrillator implantation trial investigators. N Engl J Med 335:1933–1940
Moss AJ, Zareba W, Hall WJ et al (2002) Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 346:877–883
Bänsch D, Antz M, Boczor S et al (2002) Primary prevention of sudden cardiac death in idiopathic dilated cardiomyopathy: the cardiomyopathy trial (CAT). Circulation 105:1453–1458
Kuck KH, Cappato R, Siebels J, Rüppel R (2000) Randomized comparison of antiarrhythmic drug therapy with implantable defibrillators in patients resuscitated from cardiac arrest: the cardiac arrest study hamburg (CASH). Circulation 102:748–754
Connolly SJ, Gent M, Roberts RS et al (2000) Canadian implantable defibrillator study (CIDS): a randomized trial of the implantable cardioverter defibrillator against amiodarone. Circulation 101:1297–1302
Connolly SJ, Hallstrom AP, Cappato R et al (2000) Meta-analysis of the implantable cardioverter defibrillator secondary prevention trials. AVID, CASH and CIDS studies. Antiarrhythmics vs implantable defibrillator study. Cardiac arrest study hamburg. Canadian implantable defibrillator study. Eur Heart J 21:2071–2078
The Antiarrhythmics versus Implantable Defibrillators (AVID) Investigators (1997) A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. The antiarrhythmics versus implantable defibrillators (AVID) investigators. N Engl J Med 337:1576–1583
Ponikowski P, Voors AA, Anker SD et al (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 37:2129–2200
Priori SG, Members AF, Blomström-Lundqvist C et al (2015) 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J 36(41):2757–2759
Yancy CW, Jessup M, Bozkurt B et al (2013) 2013 ACCF/AHA guideline for the management of heart failure a report of the American college of cardiology foundation/American heart association task force on practice guidelines. Circulation 128:e240–e327
Theuns DAMJ, Smith T, Hunink MGM et al (2010) Effectiveness of prophylactic implantation of cardioverter-defibrillators without cardiac resynchronization therapy in patients with ischaemic or non-ischaemic heart disease: a systematic review and meta-analysis. Eur Eur Pacing Arrhythm Card Electrophysiol J Work Groups Card Pacing Arrhythm Card Cell Electrophysiol Europace 12(11):1564–1570
Streitner F, Kuschyk J, Dietrich C et al (2011) Comparison of ventricular tachyarrhythmia characteristics in patients with idiopathic dilated or ischemic cardiomyopathy and defibrillators implanted for primary prevention. Clin Cardiol 34:604–609
Liu X, Yu H, Pei J et al (2014) Clinical characteristics and long-term prognosis in patients with chronic heart failure and reduced ejection fraction in China. Heart Lung Circ 23:818–826
Bardy GH, Lee KL, Mark DB et al (2005) Amiodarone or an Implantable cardioverter–defibrillator for congestive heart failure. N Engl J Med 352:225–237
Desai AS, Fang JC, Maisel WH, Baughman KL (2004) Implantable defibrillators for the prevention of mortality in patients with nonischemic cardiomyopathy: a meta-analysis of randomized controlled trials. JAMA 292:2874–2879
Køber L, Thune JJ, Nielsen JC et al (2016) Defibrillator implantation in patients with nonischemic systolic heart failure. N Engl J Med 375:1221–1230
The Cochrane Collaboration (2011) Cochrane handbook for systematic reviews of interventions|Cochrane community (beta). In: Cochrane Collab. http://community.cochrane.org/handbook. Accessed 20 Feb 2016
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Strickberger SA, Hummel JD, Bartlett TG et al (2003) Amiodarone versus implantable cardioverter-defibrillator: randomized trial in patients with nonischemic dilated cardiomyopathy and asymptomatic nonsustained ventricular tachycardia–AMIOVIRT. J Am Coll Cardiol 41:1707–1712
Kadish A, Dyer A, Daubert JP et al (2004) Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med 350:2151–2158
CIBIS-II Investigators and Committees (1999) The cardiac insufficiency bisoprolol study II (CIBIS-II): a randomised trial. Lancet Lond Engl 353:9–13
MERIT-HF Study Group (1999) Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet Lond Engl 353:2001–2007.
Investigators* TS (1991) Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med 325:293–302
Sharpe DN, Murphy J, Coxon R, Hannan SF (1984) Enalapril in patients with chronic heart failure: a placebo-controlled, randomized, double-blind study. Circulation 70:271–278
Pitt B, Zannad F, Remme WJ et al (1999) The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med 341:709–717
Zannad F, McMurray JJV, Krum H et al (2011) Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med 364:11–21
McMurray JJV, Packer M, Desai AS et al (2014) Angiotensin–neprilysin inhibition versus enalapril in heart failure. N Engl J Med 371:993–1004
Swedberg K, Komajda M, Böhm M et al (2010) Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. The Lancet 376:875–885
Swedberg K, Komajda M, Böhm M et al (2012) Effects on outcomes of heart rate reduction by ivabradine in patients with congestive heart failure: is there an influence of beta-blocker dose?: findings from the SHIFT (Systolic Heart failure treatment with the I(f) inhibitor ivabradine Trial) study. J Am Coll Cardiol 59:1938–1945
Cleland JGF, Daubert J-C, Erdmann E et al (2005) The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 352:1539–1549
Bristow MR, Saxon LA, Boehmer J et al (2004) Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med 350:2140–2150
Rivero-Ayerza M, Theuns DAMJ, Garcia-Garcia HM et al (2006) Effects of cardiac resynchronization therapy on overall mortality and mode of death: a meta-analysis of randomized controlled trials. Eur Heart J 27:2682–2688
Cleland JG, Abraham WT, Linde C et al (2013) An individual patient meta-analysis of five randomized trials assessing the effects of cardiac resynchronization therapy on morbidity and mortality in patients with symptomatic heart failure. Eur Heart J 34:3547–3556
Finegold JA, Raphael CE, Levy WC et al (2013) Quantification of survival gain from cardiac resynchronization therapynonlinear growth with time, and greater gain in low-risk patients, make raw trial data an underestimate of real-world behavior. J Am Coll Cardiol 62:2406–2413
Abraham WT, Young JB, Wheelan K et al (2008) Comparison of sudden cardiac death in heart failure patients with cardiac resynchronization and defibrillator therapy (CRT-D) versus CRT alone (CRT-P). J Card Fail 14:S71
Moss AJ, Hall WJ, Cannom DS et al (2009) Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med 361:1329–1338
Goldenberg I, Vyas AK, Hall WJ et al (2008) Risk stratification for primary implantation of a cardioverter-defibrillator in patients with ischemic left ventricular dysfunction. J Am Coll Cardiol 51:288–296
Rubin GA (2016) Primary prevention implantable cardioverter defibrillator placement in the elderly. In: Am Coll Cardiol. http%3a%2f%2fwww.acc.org%2flatest-in-cardiology%2farticles%2f2016%2f05%2f24%2f07%2f53%2fprimary-prevention-implantable-cardioverter-defibrillator-placement-in-the-elderly. Accessed 13 Sep 2016
Zeitler EP, Hellkamp AS, Fonarow GC et al (2015) Primary prevention implantable cardioverter-defibrillators and survival in older women. JACC Heart Fail 3:159–167
Zwanziger J, Hall WJ, Dick AW et al (2006) The cost effectiveness of implantable cardioverter-defibrillators: results from the multicenter automatic defibrillator implantation trial (MADIT)-II. J Am Coll Cardiol 47:2310–2318
Medical Advisory Secretariat (2005) Implantable cardioverter defibrillators. Prophylactic use: an evidence-based analysis. Ont Health Technol Assess Ser 5:1–74
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Wolff, G., Lin, Y., Karathanos, A. et al. Implantable cardioverter/defibrillators for primary prevention in dilated cardiomyopathy post-DANISH: an updated meta-analysis and systematic review of randomized controlled trials. Clin Res Cardiol 106, 501–513 (2017). https://doi.org/10.1007/s00392-017-1079-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-017-1079-0