Abstract
The objective of this study is to evaluate the clinical feasibility of serum matrix metalloproteinase-9 (MMP-9) for screening plaque composition as assessed by coronary computed tomography angiography (CCTA) in outpatients with chest pain,and the effects of sex on this feasibility. Eight hundred and sixty-two consecutive outpatients with chest pain were divided into three groups according to the results of CCTA: non-plaque (NP, n = 474), calcified plaques (CPs, n = 179), non-calcified and mixed plaques (NCPs and MPs, n = 209). We found that serum MMP-9 levels were significantly higher in patients with NCPs and MPs compared to those with either NP or CPs, especially in women (649.7 ± 279.8 vs. 485.7 ± 231.6 ng/mL or 515.7 ± 274.5 ng/mL, P < 0.001). MMP-9 showed better identification of NCPs and MPs than other related factors and was an independent predictor for NCPs and MPs both in women and men. The receiver operating characteristic analysis indicated a substantial superiority in women with area under the curve of 0.75 (95% CI 0.69–0.82, P < 0.01), compared with men of 0.59 (95% CI 0.53–0.65, z = 3.71, P < 0.01). The diagnostic tests revealed a moderate risk of the presence of NCPs and MPs with MMP-9 ≥531.6 ng/mL in female patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Atherosclerosis remains the primary cause of coronary artery disease (CAD), one of the most common causes of death worldwide. In addition, atherosclerotic plaque rupture causes 75% of episodes of acute coronary syndrome (ACS) according to postmortem studies [1]. Lipid-enriched non-calcified and mixed plaques are associated with increased coronary event rates as well as plaque volume progression; therefore, they are considered to be high-risk and more prone to rupture [2, 3]. Furthermore, Hou et al. [4] demonstrated that the probability of 3-year major adverse cardiac events (MACE) increased significantly with a probability of 22.7% for non-calcified plaques (NCPs) and 37.7% for mixed plaques (MPs), compared to 5.5% for calcified plaques (CPs). However, current imaging examinations used to identify high-risk atherosclerotic plaques, including optical coherence tomography (OCT) [5], intravascular ultrasound (IVUS) and computed tomography angiography (CTA) [6], are not suitable for large-scale screening due to the invasive nature or the high cost of these procedures. In contrast, early detection of serological markers is a preferred screening method as it is easy to perform and low cost.
Matrix metalloproteinases (MMPs), a family of zinc-dependent proteases, are involved in the breakdown of extracellular matrix in physiological processes, such as embryonic development and angiogenesis, as well as in pathological processes, such as cancer and cardiovascular diseases [7,8,9]. Matrix metalloproteinase-9 (MMP-9) mainly degrades type IV collagen and fibronectin and contributes to both the formation as well as destabilization of atherosclerotic plaques [10, 11]. Since Wagsater et al. [12] reported that MMP-9 is involved in atherogenesis in mice, many studies have revealed its association with plaque vulnerability [13, 14]. However, the value of MMP-9 in identifying high-risk coronary plaques in daily clinical practice remains to be explored.
In the present study, we explored the possibility of using serum MMP-9 as a biomarker to identify patients with coronary atherosclerotic NCPs and MPs in a consecutive cohort and the effects of sex on this feasibility.
Methods
Study population
Eight hundred and sixty-two consecutive outpatients who underwent coronary computed tomography angiography (CCTA) due to stable typical or atypical chest pain were recruited from July 2012 to February 2014 in Fuwai Hospital. Exclusion criteria were any recent surgeries impacting accurate measurement, such as percutaneous coronary intervention (PCI), coronary artery bypass grafting (CABG), or heart transplantation. After completing a brief questionnaire, the study subjects provided blood samples for tests, including conventional biochemical analysis and measurement of serum MMP-9 levels. The protocol of this study was carried out according to the principles of the Declaration of Helsinki and approved by the ethics review board of Fuwai Hospital. Written informed consent was obtained from each individual.
Data acquisition
Scans were performed using a 64-row spiral computed tomographic scanner (Light Speed VCT; GE Healthcare, Milwaukee, WI, USA). The main scanning parameters were as follows: 64 detectors; individual detector width, 0.625 mm; gantry rotation time, 350 ms; tube voltage, 120 kV; electrocardiographically modulated tube current; pitch, 0.16–0.22; table feed per rotation, 400 mm; and field of view, 200–250 mm. The images were transferred to a stand-alone workstation (Deep Blue, ADW 4.3; GE Healthcare, Little Chalfont, UK), and evaluated by radiology staff blinded to serum MMP-9 levels using dedicated analysis software.
Image analysis
The scans were retrospectively analyzed on the workstation and atherosclerotic plaques were classified as calcified, non-calcified or mixed as described previously [15]. Briefly, lesions with attenuation values (measured by HU) >130 HU were classified as calcified plaques. Structures clearly assignable to the vessel wall (in at least two views) with densities less than the lumen contrast were classified as non-calcified plaques, composed exclusively of those ≤130 HU. Mixed plaques comprised both calcified and non-calcified components. If more than one type of plaque was present, the characteristic of the most stenotic plaques was recorded for statistical analysis [16]. Notably, we combined the NCPs (n = 112) and MPs (n = 97) groups (NCPs and MPs) for statistical analysis because there were too few patients in each group.
Assessment of CAD risk factors
Conventional coronary risk factors, such as hypertension, diabetes mellitus, and family history, were assessed. Hypertension was defined as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥ 90 mmHg, or antihypertensive medication use. Diabetes mellitus was defined as receiving insulin or oral hypoglycemic therapy, fasting glucose of ≥126 mg/dL, or non-fasting glucose of ≥200 mg/dL. Family history of CAD was defined as myocardial infarction (MI), coronary revascularization, or sudden cardiac death for father <55 years of age or mother <65 years of age.
Laboratory procedures
Blood samples were stored at −80 °C until analysis. Serum levels of MMP-9 were determined using a commercial enzyme-linked immunosorbent assay kit (R&D Systems, Minneapolis, MN, USA) according to the manufacturer’s instructions. The intra-assay coefficient of variation for MMP-9 was <3.0%, and the inter-assay coefficient of variation was <8.0%. Serum total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), triglycerides (TG), high-sensitivity c-reactive protein (Hs-CRP), creatinine (CREA), apolipoprotein A1 (ApoA1) and apolipoprotein B (ApoB) were measured using an automatic chemistry analyzer (UniCel DxC 800 Synchron, Beckman Coulter, Brea, CA, USA) in the Laboratory Medicine Centre of Fuwai Hospital.
Statistical analysis
All statistical analyses were performed using SPSS version 17.0 (SPSS, Inc., Chicago, IL, USA). For descriptive analysis, continuous variables are expressed as mean ± standard deviation and categorical variables as percentages. Comparisons among the groups were performed using the Chi-square test or one-way ANOVA. Bivariate correlation analysis was performed to evaluate unadjusted associations between MMP-9 and other variables. Multiple logistic regression was used to assess the association of serum MMP-9 levels with atherosclerotic plaque type, adjusting for the other covariates. Receiver-operating characteristic (ROC) curves were used to evaluate the screening ability of MMP-9 for NCPs and MPs. Youden’s index (YI) was calculated as (sensitivity + specificity − 1) to determine the optimal cutoff point. Screening accuracy for various cutoff points was evaluated by sensitivity (Sen), specificity (Spe), and positive and negative likelihood ratio (LR+ and LR−).
Results
Characteristics of study participants
Eight hundred and sixty-two consecutive subjects (516 men, 346 women; mean age 53.7 ± 9.3 years) with stable typical or atypical chest pain underwent CCTA. Baseline characteristics of the study population are shown in Table 1. In patients with NCPs and MPs, men accounted for a greater proportion than in those with CPs (70.3 vs. 60.9%, P = 0.001). Hs-CRP was significantly higher in patients with NCPs and MPs, as compared to those with CPs (1.84:0.98–3.76 vs. 1.62:0.83–3.20, P = 0.009). More patients in the NCPs and MPs group had at least one coronary artery stenosis >50% than those in the CPs group (46.4 vs. 16.9%, P < 0.001).
Correlation between serum MMP-9 levels and cardiovascular risk factors
With Spearman correlation analysis, serum MMP-9 levels correlated positively with sex (r = 0.183, P < 0.001), LDL-C (r = 0.075, P = 0.028), and inflammation-related factors such as Hs-CRP (r = 0.151, P < 0.001) and CREA (r = 0.131, P < 0.023), yet negatively with age (r = −0.091, P = 0.008), HDL-C (r = −0.077, P = 0.023), and affected coronary branches (r = −0.113, P = 0.026) (Table 2). No correlations were found between MMP-9 and BMI, TC, TG, hypertension, diabetes mellitus, family history of CAD, or even severity of coronary stenosis. Multiple logistic regression analysis was performed to determine whether the correlations between MMP-9 and NCPs and MPs observed on univariate analysis were significant after controlling for potential confounding factors. Multiple logistic regression in Table 3 indicated that MMP-9 was an independent predictor of NCPs and MPs after adjustment for age, sex, BMI, hypertension, diabetes mellitus, family history of CAD, stenosis, branch, TC, TG, HDL-C, LDL-C, Hs-CRP, CREA.
Changes in serum levels of MMP-9 according to sex
We found that serum MMP-9 levels in the NP, CPs and NCPs and MPs groups increased gradually in the overall population (533.7 ± 243.8 vs. 588.4 ± 270.1 vs. 646.4 ± 267.2 ng/mL, P < 0.001). Furthermore, after stratification by sex, the increase of MMP-9 in the NCPs and MPs group was more prominent in women (649.7 ± 279.8 vs. 485.7 ± 231.6 ng/mL, P < 0.001), compared with in men (644.9 ± 262.7 vs. 573.1 ± 247.0 ng/mL, P < 0.01) or in the overall population (646.4 ± 267.2 vs. 533.7 ± 243.8 ng/mL, P < 0.001) (Fig. 1).
Comparison of MMP-9 levels among NP, CPs and NCPs and MPs groups in the overall population, women and men. The serum level of MMP-9 in the NCPs and MPs patients was significantly higher than that in the NP group in the overall population (646.4 ± 267.2 vs. 533.7 ± 243.8 ng/mL, P < 0.001) and in men (644.9 ± 262.7 vs. 573.1 ± 247.0 ng/mL, P < 0.01). In women, serum level of MMP-9 in the NCPs and MPs patients increased significantly compared with NP and CPs patients (649.7 ± 279.8 vs. 485.7 ± 231.6 vs. 515.7 ± 274.5 ng/mL, P < 0.001). *P < 0.01, compared with non-plaque (NP) group. # P < 0.01, compared with calcified plaques (CPs) group
Identification performance of serum MMP-9 levels for NCPs and MPs
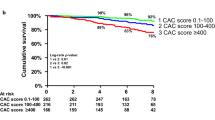
ROC curves and area under the curve (AUC) were generated to evaluate diagnostic values. As shown in Fig. 2a, among multiple variables related to atherosclerosis, the AUC value of circulating MMP-9 for identifying NCPs and MPs was highest in the overall population, with 0.66 (95% CI 0.61–0.70, P < 0.001) vs. 0.51 (95% CI 0.46–0.55, P = 0.712) for TC, 0.53 (95% CI 0.48–0.57, P = 0.251) for TG, 0.51 (95% CI 0.46–0.55, P = 0.508) for HDL-C, 0.51 (95% CI 0.46–0.55, P = 0.765) for LDL-C, 0.57 (95% CI 0.52–0.62, P = 0.003) for Hs-CRP, and 0.58 (95% CI 0.53–0.62, P = 0.001) for CREA. Importantly, there was a substantial superiority of the diagnostic capability of MMP-9 for NCPs and MPs in women with AUC = 0.75 (95% CI 0.69–0.82, P < 0.001), compared with the overall population of 0.66 (95% CI 0.61–0.70, z = 2.45, P < 0.05) and men of 0.59 (95% CI 0.53–0.65, z = 3.71, P < 0.01) (Fig. 2b, c). No significant difference was found between men and the overall population (z = 1.81, P > 0.05).
Receiver operating characteristic (ROC) curve for non-calcified and mixed plaques in overall population (a), women (b) and men (c). The area under ROC curve in women with 0.75 (95% CI 0.68–0.82) increased significantly compared with overall population without stratification by sex with 0.66 (95% CI 0.61–0.70, z = 2.45, P < 0.05) and man with 0.59 (95% CI 0.53–0.65, z = 3.71, P < 0.01)
Diagnostic accuracy of serum MMP-9 levels for NCPs and MPs
The optimal cutoff points were determined by the maximum Youden index as shown in Table 4. In overall patients, MMP-9 was able to identify NCPs and MPs at cutoff value of 576.7 ng/mL with sensitivity of 78.2% and specificity of 45.1%, LR+ of 1.42 (1.24–1.63) and LR− of 0.48 (0.35–0.64). Interestingly, quite a few increases in women were demonstrated with 85.0% sensitivity and 56.5% specificity, 1.95 (1.69–2.28) LR+ and 0.27 (0.18–0.37) LR− at cutoff value of 531.6 ng/mL. However, there were the poorer sensitivity of 34.9% and higher specificity of 79.5% in men with diagnostic cutoff value of 630.7 ng/mL.
Discussion
The present study was designed to investigate the suitability of serum MMP-9 for identifying the characteristics of coronary atherosclerotic plaques in a hospital population undergoing CCTA owing to chest pain. Analysis of a large and single-centre consecutive cohort demonstrated that (1) MMP-9 is associated with plaque composition, with increased levels in patients with NCPs and MPs compared with the other groups; (2) there was a moderate value for MMP-9 in the diagnosis of NCPs and MPs in women, but not in men. Serum MMP-9 may be a promising approach for screening NCPs and MPs in health institutions in females, but not in males.
Lesions leading to ACS often have a large necrotic core containing abundant lipid material, and these are classified as NCPs and MPs by CCTA. Hoffmann et al. [16] reported that non-calcified plaques were consistently present in culprit lesions and the incidence of ACS was higher than in those with calcified plaques. Pundziute et al. [17] showed that the number of mixed plaques defined by MSCT (Multisice Computed Tomography) was a significant predictor of acute cardiovascular events. Hou et al. [4] performed a follow-up study of 5007 outpatients suspected of having CAD and found that the presence of plaques with non-calcified and mixed components was more relevant to the occurrence of 3-year MACE than calcified components, therefore, these were considered as high-risk plaques. Recent publications reported that MMP-9 was localized in macrophage-rich lesions and that expression was increased in atherosclerotic plaques compared with normal arteries or stable plaques [18]. Similarly, some studies have indicated that peripheral blood levels of MMP-9 are elevated in patients with acute coronary syndromes [19, 20], or carotid artery atherosclerosis vulnerable plaques [21, 22]. However, another minority view also appeared to suggest that serum MMP-9 levels had no association with plaque burden or morphology, as reported by Lehrke et al. [23]. Obviously, our results are consistent with the former view that high serum MMP-9 level is a significant predictor for unstable NCPs and MPs. Furthermore, the better diagnostic performance of MMP-9, in women than men, may provide clues to explain this controversy.
Kobayashi et al. [24] showed that MMP-9 level was regarded as a biomarker of plaque vulnerability and had a high diagnostic value of AUC of about 0.88 for early ST elevation ACS, reflecting plaque rupture or vulnerability. In our large-scale screening programs, the diagnostic performance of serum MMP-9 alone was poor in clinical practice. The discrepancy was due to the characteristics of the study population, with ACS symptoms occurring in Kobayashi’s cohort and with unstable plaques before ACS occurring in ours. It is noteworthy that serum MMP-9 concentrations exhibit sexual dimorphism, with females having higher levels than males. In our study, MMP-9 levels of patients with NPs and stable CPs were lower in women than men, while no differences between the sexes were observed in patients with NCPs. Moreover, the ability of MMP-9 to identify unstable NCPs and MPs was better in women with AUC = 0.75 (z = 3.71, P < 0.01) compared with men, implying that MMP-9 has a better recognition ability for female patients as a marker of NCPs and MPs. Although MMP-9 was found to be a significant predictor for the presence of NCPs and MPs, the diagnostic capability was unsatisfactory. However, the improved diagnostic performance in women with optimal cutoffs suggests this might provide a new way of scoring risk to predict NCPs and MPs through sex stratification.
Atherosclerotic plaque destabilization is a maladaptive inflammatory response of the arterial wall. The exact mechanisms of the association between MMP-9 and non-calcified and mixed plaques remain to be illuminated, but inflammation is one of the most important explanations. MMP-9 promotes matrix degradation, thus facilitating the entry of immune cells into lesion sites and promoting neovascularization [25]. In the meantime, collagen degradation of MMP-9 in the plaque makes the fibrous cap thinner with subsequent activation of major atherogenic factors such as vascular endothelial growth factor [26]. Together, this series of effects of MMP-9 eventually leads to plaque rupture [27]. Based on their roles in plaque stability, MMP inhibitors (MMPis) and gene therapy might be considered for clinical treatment [28, 29]. With the increased understanding of plaque rupture mechanisms, more and more studies have focused on changes in circulating inflammatory biomarkers, such as C-reactive protein (CRP) [30], interleukin-6 (IL-6) [31], and oxidized low-density lipoprotein (Lp-PLA2) [32] as predictors of plaque instability and future vascular events. In our study, ROC analysis demonstrated that serum MMP-9 levels provided better discrimination of NCPs and MPs than CRP and other inflammatory factors.
Study limitations
Our study has several limitations. This cross-sectional study design cannot predict the rate of future cardiac events and a prospective design is required to confirm our findings. Also unfortunately we do not have information on smoking habits. However, results from a small number of populations show that MMP-9 is a factor independent of smoking, hypertension and diabetes, consistent with the findings of Tayebjee [33].
In summary, serum MMP-9 levels were significantly and independently correlated with NCPs and MPs and its diagnostic performance increased in women compared with that in men. Furthermore, our observations highlight the potential utility of MMP-9 in screening for coronary atherosclerotic plaque characteristics in routine clinical practice.
Conclusions
High MMP-9 levels provide a moderate contribution to the diagnosis of non-calcified and mixed plaques in women, but not in men. Serum MMP-9 level may be a promising approach for screening high-risk atherosclerosis patients in routine clinical practice through sex stratification.
References
Narula J, Nakano M, Virmani R, Kolodgie FD, Petersen R, Newcomb R, Malik S, Fuster V, Finn AV (2013) Histopathologic characteristics of atherosclerotic coronary disease and implications of the findings for the invasive and noninvasive detection of vulnerable plaques. J Am Coll Cardiol 61:1041–1051
Leber AW, von Ziegler F, Becker A, Becker CR, Reiser M, Steinbeck G, Knez A, Boekstegers P (2008) Characteristics of coronary plaques before angiographic progression determined by multi-slice CT. Int J Cardiovasc Imaging 24:423–428
Yamagishi M, Terashima M, Awano K, Kijima M, Nakatani S, Daikoku S, Ito K, Yasumura Y, Miyatake K (2000) Morphology of vulnerable coronary plaque: insights from follow-up of patients examined by intravascular ultrasound before an acute coronary syndrome. J Am Coll Cardiol 35:106–111
Hou ZH, Lu B, Gao Y, Jiang SL, Wang Y, Li W, Budoff MJ (2012) Prognostic value of coronary CT angiography and calcium score for major adverse cardiac events in outpatients. JACC Cardiovasc Imaging 5:990–999
Sakaguchi M, Ehara S, Hasegawa T, Matsumoto K, Nishimura S, Yoshikawa J, Shimada K (2017) Coronary plaque rupture with subsequent thrombosis typifies the culprit lesion of non-ST-segment-elevation myocardial infarction, not unstable angina: non-ST-segment-elevation acute coronary syndrome study. Heart Vessels 32:241–251
Ehara S, Matsumoto K, Hasegawa T, Otsuka K, Sakaguchi M, Shimada K, Yoshikawa J, Yoshiyama M (2016) Characteristic patterns of the longitudinal and circumferential distribution of calcium deposits by parent coronary arteries observed from computed tomography angiography. Heart Vessels 31:508–518
Newby AC (2008) Metalloproteinase expression in monocytes and macrophages and its relationship to atherosclerotic plaque instability. Arterioscler Thromb Vasc Biol 28:2108–2114
Visse R, Nagase H (2003) Matrix metalloproteinases and tissue inhibitors of metalloproteinases: structure, function, and biochemistry. Circ Res 92:827–839
Wang Y, Wu B, Dong L, Wang C, Wang X, Shu X (2016) Circulating matrix metalloproteinase patterns in association with aortic dilatation in bicuspid aortic valve patients with isolated severe aortic stenosis. Heart Vessels 31:189–197
Sukhova GK, Schonbeck U, Rabkin E, Schoen FJ, Poole AR, Billinghurst RC, Libby P (1999) Evidence for increased collagenolysis by interstitial collagenases-1 and -3 in vulnerable human atheromatous plaques. Circulation 99:2503–2509
Welgus HG, Campbell EJ, Cury JD, Eisen AZ, Senior RM, Wilhelm SM, Goldberg GI (1990) Neutral metalloproteinases produced by human mononuclear phagocytes. Enzyme profile, regulation, and expression during cellular development. J Clin Investig 86:1496–1502
Wagsater D, Zhu C, Bjorkegren J, Skogsberg J, Eriksson P (2011) MMP-2 and MMP-9 are prominent matrix metalloproteinases during atherosclerosis development in the Ldlr(−/−)Apob(100/100) mouse. Int J Mol Med 28:247–253
Muller A, Kramer SD, Meletta R, Beck K, Selivanova SV, Rancic Z, Kaufmann PA, Vos B, Meding J, Stellfeld T, Heinrich TK, Bauser M, Hutter J, Dinkelborg LM, Schibli R, Ametamey SM (2014) Gene expression levels of matrix metalloproteinases in human atherosclerotic plaques and evaluation of radiolabeled inhibitors as imaging agents for plaque vulnerability. Nucl Med Biol 41:562–569
Zeng B, Prasan A, Fung KC, Solanki V, Bruce D, Freedman SB, Brieger D (2005) Elevated circulating levels of matrix metalloproteinase-9 and -2 in patients with symptomatic coronary artery disease. Intern Med J 35:331–335
Leber AW, Becker A, Knez A, von Ziegler F, Sirol M, Nikolaou K, Ohnesorge B, Fayad ZA, Becker CR, Reiser M, Steinbeck G, Boekstegers P (2006) Accuracy of 64-slice computed tomography to classify and quantify plaque volumes in the proximal coronary system: a comparative study using intravascular ultrasound. J Am Coll Cardiol 47:672–677
Hoffmann U, Moselewski F, Nieman K, Jang IK, Ferencik M, Rahman AM, Cury RC, Abbara S, Joneidi-Jafari H, Achenbach S, Brady TJ (2006) Noninvasive assessment of plaque morphology and composition in culprit and stable lesions in acute coronary syndrome and stable lesions in stable angina by multidetector computed tomography. J Am Coll Cardiol 47:1655–1662
Pundziute G, Schuijf JD, Jukema JW, Boersma E, de Roos A, van der Wall EE, Bax JJ (2007) Prognostic value of multislice computed tomography coronary angiography in patients with known or suspected coronary artery disease. J Am Coll Cardiol 49:62–70
Sluijter JP, Pulskens WP, Schoneveld AH, Velema E, Strijder CF, Moll F, de Vries JP, Verheijen J, Hanemaaijer R, de Kleijn DP, Pasterkamp G (2006) Matrix metalloproteinase 2 is associated with stable and matrix metalloproteinases 8 and 9 with vulnerable carotid atherosclerotic lesions: a study in human endarterectomy specimen pointing to a role for different extracellular matrix metalloproteinase inducer glycosylation forms. Stroke 37:235–239
Inokubo Y, Hanada H, Ishizaka H, Fukushi T, Kamada T, Okumura K (2001) Plasma levels of matrix metalloproteinase-9 and tissue inhibitor of metalloproteinase-1 are increased in the coronary circulation in patients with acute coronary syndrome. Am Heart J 141:211–217
Kai H, Ikeda H, Yasukawa H, Kai M, Seki Y, Kuwahara F, Ueno T, Sugi K, Imaizumi T (1998) Peripheral blood levels of matrix metalloproteases-2 and -9 are elevated in patients with acute coronary syndromes. J Am Coll Cardiol 32:368–372
Silvello D, Narvaes LB, Albuquerque LC, Forgiarini LF, Meurer L, Martinelli NC, Andrades ME, Clausell N, dos Santos KG, Rohde LE (2014) Serum levels and polymorphisms of matrix metalloproteinases (MMPs) in carotid artery atherosclerosis: higher MMP-9 levels are associated with plaque vulnerability. Biomarkers 19:49–55
Tan C, Liu Y, Li W, Deng F, Liu X, Wang X, Gui Y, Qin L, Hu C, Chen L (2014) Associations of matrix metalloproteinase-9 and monocyte chemoattractant protein-1 concentrations with carotid atherosclerosis, based on measurements of plaque and intima-media thickness. Atherosclerosis 232:199–203
Lehrke M, Greif M, Broedl UC, Lebherz C, Laubender RP, Becker A, von Ziegler F, Tittus J, Reiser M, Becker C, Goke B, Steinbeck G, Leber AW, Parhofer KG (2009) MMP-1 serum levels predict coronary atherosclerosis in humans. Cardiovasc Diabetol 8:50
Kobayashi N, Hata N, Kume N, Yokoyama S, Shinada T, Tomita K, Kitamura M, Shirakabe A, Inami T, Yamamoto M, Seino Y, Mizuno K (2011) Matrix metalloproteinase-9 for the earliest stage acute coronary syndrome. Circ J 75:2853–2861
Gough PJ, Gomez IG, Wille PT, Raines EW (2006) Macrophage expression of active MMP-9 induces acute plaque disruption in apoE-deficient mice. J Clin Investig 116:59–69
Yabluchanskiy A, Ma Y, Iyer RP, Hall ME, Lindsey ML (2013) Matrix metalloproteinase-9: many shades of function in cardiovascular disease. Physiology (Bethesda) 28:391–403
Newby AC (2005) Dual role of matrix metalloproteinases (matrixins) in intimal thickening and atherosclerotic plaque rupture. Physiol Rev 85:1–31
Campestre C, Agamennone M, Tauro M, Tortorella P (2015) Phosphonate emerging zinc binding group in matrix metalloproteinase inhibitors. Curr Drug Targets 16:1634–1644
Li NG, Tang YP, Duan JA, Shi ZH (2014) Matrix metalloproteinase inhibitors: a patent review (2011–2013). Expert Opin Ther Pat 24:1039–1052
Danesh J, Wheeler JG, Hirschfield GM, Eda S, Eiriksdottir G, Rumley A, Lowe GD, Pepys MB, Gudnason V (2004) C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N Engl J Med 350:1387–1397
Schieffer B, Schieffer E, Hilfiker-Kleiner D, Hilfiker A, Kovanen PT, Kaartinen M, Nussberger J, Harringer W, Drexler H (2000) Expression of angiotensin II and interleukin 6 in human coronary atherosclerotic plaques: potential implications for inflammation and plaque instability. Circulation 101:1372–1378
Koenig W, Twardella D, Brenner H, Rothenbacher D (2006) Lipoprotein-associated phospholipase A2 predicts future cardiovascular events in patients with coronary heart disease independently of traditional risk factors, markers of inflammation, renal function, and hemodynamic stress. Arterioscler Thromb Vasc Biol 26:1586–1593
Tayebjee MH, Lip GY, Tan KT, Patel JV, Hughes EA, MacFadyen RJ (2005) Plasma matrix metalloproteinase-9, tissue inhibitor of metalloproteinase-2, and CD40 ligand levels in patients with stable coronary artery disease. Am J Cardiol 96:339–345
Acknowledgements
This work is supported by the National Natural Science Foundation of China (81371887) and (81470484), National Key Technology Support Program (2011BAI11B03) and Capital Clinical Characteristics Research (Z121107005112013). The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed. No writing assistance was utilized in the production of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gu, C., Wang, F., Hou, Z. et al. Sex-related differences in serum matrix metalloproteinase-9 screening non-calcified and mixed coronary atherosclerotic plaques in outpatients with chest pain. Heart Vessels 32, 1424–1431 (2017). https://doi.org/10.1007/s00380-017-1014-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-017-1014-3