Abstract
Purpose
Prostate cancer remains a common disease that is frequently treated with multimodal therapy. The goal of this study was to assess the impact of treatment of the primary tumor on survival in men who go onto receive chemotherapy for prostate cancer.
Methods
Using surveillance, epidemiology and end results (SEER)-Medicare data from 1992 to 2009, we identified a cohort of 1614 men who received chemotherapy for prostate cancer. Primary outcomes were prostate cancer-specific mortality (PCSM) and all-cause mortality (ACM). We compared survival among men who had previously undergone radical prostatectomy (RP), radiation therapy (RT), or neither of these therapies. Propensity score adjusted Cox proportional hazard models and weighted Kaplan–Meier curves were used to assess survival.
Results
Compared to men who received no local treatment, PCSM was lower for men who received RP ± RT (HR 0.65, p < 0.01) and for those who received RT only (HR 0.79, p < 0.05). Patients receiving neither RP nor RT demonstrated higher PCSM and ACM than those receiving treatment in a weighted time-to-event analysis. Men who received RP + RT had longer mean time from diagnosis to initiation of chemotherapy (100.7 ± 47.7 months) than men with no local treatment (48.8 ± 35.0 months, p < 0.05).
Conclusion
In patients who go on to receive chemotherapy, treatment of the primary tumor for prostate cancer appears to confer a survival advantage over those who do not receive primary treatment. These data suggest continued importance for local treatment of prostate cancer, even in patients at high risk of failing local therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Widespread use routine prostate cancer screening has led to increasing discovery of early stage prostate cancer [1]. In this setting, early local treatment with curative intent, in the form of radical prostatectomy (RP) or radiation therapy (RT), has become common practice for localized prostate cancer. Optimal treatment strategies for high-risk prostate cancer with/without loco-regional spread are less well established. In particular, the benefit of treatment of the primary tumor in men who ultimately are destined to develop metastatic castrate-resistant prostate cancer (mCRPC) remains unclear. In men with localized high-risk prostate cancer, previous studies have identified treatment of the primary tumor with RP followed by symptomatic management with ADT to be associated with improved cancer-specific survival [2, 3] and overall survival [3], when compared to ADT alone. Other studies examining the role of RP in men who ultimately develop metastatic prostate cancer have found conflicting results when comparing survival of men who underwent RP to those with intact prostates [4, 5]. Thus, the benefit of treatment of primary tumor in men who are at high risk for developing mCRPC remains unclear.
The purpose of the current study was to further characterize the possible benefit of treatment of primary tumor using RP and/or RT in patients who go on to ultimately develop disease progression and receive systemic chemotherapy. Data demonstrating survival benefit in men who receive chemotherapy for mCRPC [6] have led to common use of these agents in the treatment of this disease. In other malignancies such as renal cell carcinoma, data suggest a survival benefit to removal of primary tumor in those who go on to receive systemic therapy for metastatic disease [7, 8]. Similarly, we sought to examine the potential benefit of treatment of primary tumor in the prostate in patients who ultimately go on to receive systemic chemotherapy for prostate cancer, using a population-based dataset.
Materials and methods
This IRB-approved study used the linked surveillance, epidemiology and end results (SEER)-Medicare database. The SEER registries collect information on cancer cases diagnosed within 17 areas in the USA and include approximately 26 % of the US population [9]. The linked Medicare data provided detailed billing records for treatments provided to Medicare beneficiaries. The details about this method of linkage are described elsewhere [10].
We identified men aged ≥66 years diagnosed with non-metastatic adenocarcinoma of the prostate between 1992 and 2009. To ensure complete claims data and accurate cancer information, men who were diagnosed at autopsy or in nursing homes, those who were not enrolled in Medicare Parts A and B, or who enrolled in health maintenance organizations, those who were diagnosed in Louisiana in 2005, and those who had prior or subsequent cancers were excluded.
The population of interest is men who have treatments consistent with mCRPC, and the administration of ADT for >6 months is commonly used prior to chemotherapy for metastatic prostate cancer. Thus, we defined our cohort as men with claims evidence of receiving ADT followed by a claim for FDA approved chemotherapy (docetaxel or mitoxantrone) (n = 2935). We excluded men with inadequate billing information to evaluate their doses of ADT (n = 618), those who did not receive ADT for at least 6 months (n = 619), those who were diagnosed with another cancer before or after the prostate cancer diagnosis (n = 361), and those with missing socioeconomic variables (n = 84), resulting in a cohort of 1614 men (see Supplemental Figure).
The exposure of interest was the type of local therapy given prior to ADT and chemotherapy administration. We placed men into three groups: RP with or without RT, RT alone, and no local treatment (defined as no evidence of RP or RT). Among the 67 patients with “RP with RT,” fewer than 11 received RT prior to RP, 50 % received RT within 1-year of RP, and the remaining 50 % ranged from 13 months to 12 years later.
We used the International Classification of Disease, Ninth Revision (ICD-9) diagnosis and procedure codes and common procedural terminology (CPT) codes to identify diagnosis and treatment variables including cancer of the prostate, RP, RT (external beam radiation therapy, brachytherapy, intensity-modulated radiation therapy), ADT (use of GnRH agonists), and chemotherapeutic agents (docetaxel and mitoxantrone). A detailed list of codes can be seen in Supplemental Table 1.
We also examine the year of diagnosis, ages at diagnosis in 5-year increments, race/ethnicity, and the US census region. Census tract levels of median income and education were stratified into quartiles. Tumor stage (T1, T2, T3, or T4, and unknown stage) and grade (corresponding to World Health Organization grade: low, medium, high or undifferentiated, and unknown) of disease were based on the SEER-recorded variables. The Klabunde et al. adaptation [11] of the Deyo method [12] was used to calculate Charlson comorbidity score [13, 14] from inpatient and outpatient hospital and physician in the 12 months preceding the diagnosis of prostate cancer.
Differences within demographic variables among the treatment groups were compared via Chi-square (χ 2). To minimize the effect of treatment selection bias, patient characteristics were adjusted with inverse probability of treatment weighting. Briefly, multivariable logistic regression models used year of treatment, age at diagnosis, race/ethnicity, median income, education, stage, grade, and Charlson comorbidity index to estimate the probability the assigned treatment, conditional on observed baseline characteristics. The inverse of this probability, termed the inverse probability of treatment weight (IPTW), was then truncated to eliminate outliers. The balance of variables was confirmed by Chi-square tests of the weighted observations. With the exception of age, there were no longer significant differences in the treatment groups among the aforementioned variables. The balance was improved for age; however, the small number of patients over age 75 in the RP group made achieving total balance difficult.
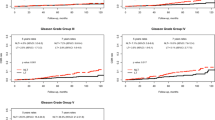
Survival was defined as the number of months from cancer diagnosis to death. Observations were censored at the end of claims availability (December 2009). Unweighted and IPTW-weighted Kaplan–Meier time-to-event analyses were used to measure the risks of mortality by treatment type and compared by log-rank test. For these curves, patients were assigned to their local treatment group beginning at diagnosis.
IPTW-weighted time-dependent Cox proportional hazard (CPH) models were fitted for prostate cancer-specific mortality (PCSM) and all-cause mortality (ACM). To reduce bias caused by the timing of local cancer treatment, a time-dependent covariate was included in the model. Subjects were counted as “no local treatment” until the time of their local therapy (if initiated prior to ADT) at which point the relevant time-dependent covariate changed from 0 to 1 (the RP + RT treatment indicator switched at the time of the second treatment).
We also evaluated the association of treatment group with time from diagnosis of prostate cancer to initiation of chemotherapy for each group using the propensity-weighted CPH mode. Statistical analyses were performed using SAS statistical software, version 9.3 (SAS Institute, Inc, Cary, NC, USA). All statistical tests were two-sided, and the level of significance was set at p < 0.05.
Results
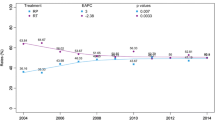
Cohort characteristics are shown in Table 1. The mean age was 73.1 years (SD ± 5.0 years), and median follow-up time was 63 months. The majority (73 %, n = 1172) of the patients received no local therapy prior to ADT use. Approximately 4 % (n = 67) had RP + RT, 7 % (n = 109) had RP only, and 17 % (n = 266) had RT only as local therapy. While the use of RT or no treatment increased with age, of those men who received primary treatment, RP was the most common modality in men under age 70.
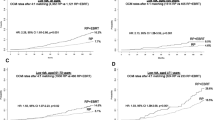
Table 2 shows findings from the multivariate models predicting PCSM and ACM. Compared to men who received no local therapy, the risk of PCSM was significantly lower for men who received RP ± RT (HR 0.65, p < 0.01) and for men who received RT only (HR 0.79, p < 0.05), and the risk of ACM was significantly lower for men who received RP ± RT (HR 0.65, p < 0.01) and for men who received RT only (HR 0.76, p < 0.01). The hazard ratios for PCSM and ACM increased with age at diagnosis and became significant after age 75 years (p < 0.01). The risk of PCSM and ACM increased significantly with higher grade and unknown stage disease. Charlson score did not predict increased PCSM or ACM.
Data regarding time from diagnosis to initiation of chemotherapy are shown in Table 3. Mean time from diagnosis to chemotherapy was 79.4 months (SD ± 47.8) for RP only, 79.6 months (SD ± 38.6) for RT only, 100.7 months (SD ± 47.7) for RP + RT, and 48.8 months (SD ± 35.0) for no RP or RT. Compared to no local therapy, there was a significant increase in time lag from diagnosis to chemotherapy for those who had RT only (HR 0.76, p < 0.01) and those who received RP + RT (HR 0.72, p < 0.05).
Discussion
We sought to evaluate the benefit of initial treatment of the primary tumor in patients who go on to receive chemotherapy for the treatment of prostate cancer. Our data suggest that men who receive such local treatment in have lower PCSM, lower ACM, and longer time lag from diagnosis to initiation of chemotherapy, compared to patients who did not receive any reported treatment of the primary tumor. Overall, our findings suggest that in men with high-risk disease who go on to receive chemotherapy, presumably in the setting of mCRPC, there is benefit to prior local therapy of the primary tumor.
Our data suggest a PCSM benefit in patients who had RP as a component of primary prostate cancer treatment, similar to previously published studies in a variety of cohorts [15–17]. Other studies have identified a survival benefit for local therapy over no local treatment in men who developed metastatic disease [18] and also in men with known metastasis at time of intervention [19]. Our study builds on this body of the literature, particularly with the use of a unique cohort from the linked SEER-Medicare dataset allowing for inclusion of comorbidity data, evaluation of time to secondary therapy, and a more complete multivariable model.
The role of cytoreductive surgery has been established in other genitourinary malignancies including renal cell carcinoma [8] and has been explored for unresectable or regionally metastatic bladder cancer [20]. Biochemical theories to explain this suggest that the primary site of malignancy releases cytokines and chemokines that facilitate metastatic spread of disease [21]. In addition, it is hypothesized that primary tumors can release circulating tumor cells that perpetuate a process of “self-seeding” the primary organ [22]. Thus, removal of a primary tumor has the potential to inhibit these processes which may explain delayed tumor progression and improved survival. Our data suggest that this cytoreductive model may apply to prostate cancer given that patients who had primary therapy demonstrated improved survival, even with the development of disease requiring chemotherapy.
In addition to potential survival benefit, our data suggest that treatment of the primary tumor also appears to delay the time to initiation of chemotherapy, which suggests a delay in time to development of clinically significant mCRPC. In additional analysis of our cohort, with survival defined as time of initiation of chemotherapy to time of death, we did not identify differences in PCSM or ACM between groups (Supplemental Table 3). Thus, the benefit received from primary therapy may be in the delay to development of mCRPC and initiation of chemotherapy.
Previous studies have suggested benefit to RP in the presence of low-volume nodal metastases and oligometastatic disease [2, 18, 23, 24]. Our study extends this concept to those patients with and without metastatic disease at the time of initial treatment. As we seek to optimize therapy for those patients with high-risk disease using multi-modality approaches, initial treatment of the primary tumor will likely remain a part of the equation in order to maximize the long-term survival benefits and benefits to local tumor control including prevention of outlet obstruction, hematuria, and extension to contiguous organs [25].
One potential explanation for our findings may be that undergoing treatment of primary tumor is truly a proxy for performance status, thereby suggesting a selection bias with healthier patients receiving therapy, and performance status acting as the true predictor of lower PCSM and ACM. However, higher Charlson comorbidity score was not associated with higher PCSM in a multivariable model arguing against the possibility that comorbidity score was directly predictive of PCSM (although Charlson score was not predictive of ACM either). Furthermore, there was not a significant difference in comorbidity scores between treatment groups on weighted analysis, further suggesting that comorbidity is not the sole driver of our findings.
We acknowledge the limitations of this study, including its retrospective, non-randomized design. Furthermore, mean age of diagnosis was 73.7 years. A population including a higher proportion of younger men would likely have differing comorbidity and treatment characteristics. An additional potential confounder is the possibility that men received cancer treatment that was not captured by our queries. This concern was minimized in that all patients included in the cohort received their initial diagnosis after age 65 (after enrolling in Medicare), and patients enrolled in HMOs were excluded. Thus, all prostate cancer treatments should be captured via Medicare billing codes. While selection bias and possible unmeasured confounding variables may have influenced our results, statistical analysis included a propensity-weighted multivariate model in attempt to limit the impact of such variables. Overall, we were able to utilize a large, population-based dataset for analysis which is reflective of common practice standards outside of the confined parameters of a clinical trial.
Conclusion
Our data identify improved PCSM and ACM in men who have treatment of the primary tumor for prostate cancer in men who later receive chemotherapy. These data further suggest a longer time lag from diagnosis to chemotherapy for men who receive local therapy. Further study with prospective trials is needed to further delineate this benefit and continue to refine optimal treatment strategies for men with high-risk prostate cancer.
References
Han M, Partin AW, Piantadosi S, Epstein JI, Walsh PC (2001) Era specific biochemical recurrence-free survival following radical prostatectomy for clinically localized prostate cancer. J Urol 166(2):416–419
Steuber T, Budaus L, Walz J, Zorn KC, Schlomm T, Chun F et al (2011) Radical prostatectomy improves progression-free and cancer-specific survival in men with lymph node positive prostate cancer in the prostate-specific antigen era: a confirmatory study. BJU Int 107(11):1755–1761
Ghavamian R, Bergstralh EJ, Blute ML, Slezak J, Zincke H (1999) Radical retropubic prostatectomy plus orchiectomy versus orchiectomy alone for pTxN+ prostate cancer: a matched comparison. J Urol 161(4):1223–1227
Thompson IM, Tangen C, Basler J, Crawford ED (2002) Impact of previous local treatment for prostate cancer on subsequent metastatic disease. J Urol 168(3):1008–1012
Halabi S, Vogelzang NJ, Ou SS, Small EJ (2007) The impact of prior radical prostatectomy in men with metastatic castration recurrent prostate cancer: a pooled analysis of 9 cancer and leukemia group B trials. J Urol 177(2):531–534
Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN et al (2004) Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med 351(15):1502–1512
Flanigan RC, Salmon SE, Blumenstein BA, Bearman SI, Roy V, McGrath PC et al (2001) Nephrectomy followed by interferon alfa-2b compared with interferon alfa-2b alone for metastatic renal-cell cancer. N Engl J Med 345(23):1655–1659
Belldegrun A, Shvarts O, Figlin RA (2000) Expanding the indications for surgery and adjuvant interleukin-2-based immunotherapy in patients with advanced renal cell carcinoma. Cancer J Sci Am 6(Suppl 1):S88–S92
Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF (2002) Overview of the SEER-medicare data: content, research applications, and generalizability to the united states elderly population. Med Care 40(8 Suppl):IV-3-18
Potosky AL, Riley GF, Lubitz JD, Mentnech RM, Kessler LG (1993) Potential for cancer related health services research using a linked medicare-tumor registry database. Med Care 31(8):732–748
Klabunde CN, Potosky AL, Legler JM, Warren JL (2000) Development of a comorbidity index using physician claims data. J Clin Epidemiol 53(12):1258–1267
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45(6):613–619
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 40(5):373–383
Charlson ME, Sax FL, MacKenzie CR, Braham RL, Fields SD, Douglas RG Jr (1987) Morbidity during hospitalization: Can we predict it? J Chronic Dis 40(7):705–712
Zelefsky MJ, Eastham JA, Cronin AM, Fuks Z, Zhang Z, Yamada Y et al (2010) Metastasis after radical prostatectomy or external beam radiotherapy for patients with clinically localized prostate cancer: a comparison of clinical cohorts adjusted for case mix. J Clin Oncol 28(9):1508–1513
Cooperberg MR, Vickers AJ, Broering JM, Carroll PR (2010) Comparative risk-adjusted mortality outcomes after primary surgery, radiotherapy, or androgen-deprivation therapy for localized prostate cancer. Cancer 116(22):5226–5234
Swanson GP, Riggs M, Earle J (2004) Failure after primary radiation or surgery for prostate cancer: differences in response to androgen ablation. J Urol 172(2):525–528
Culp SH, Schellhammer PF, Williams MB (2014) Might men diagnosed with metastatic prostate cancer benefit from definitive treatment of the primary tumor? A SEER-based study. Eur Urol 65:1058–1066
Satkunasivam R, Kim AE, Desai M, Nguyen MM, Quinn DI, Ballas L et al (2015) Radical prostatectomy or external beam radiation therapy vs no local therapy for survival benefit in metastatic prostate cancer: as SEER-Medicare analysis. J Urol 194:378–385
Herr HW, Donat SM, Bajorin DF (2001) Post-chemotherapy surgery in patients with unresectable or regionally metastatic bladder cancer. J Urol 165(3):811–814
Kaplan RN, Rafii S, Lyden D (2006) Preparing the “soil”: the premetastatic niche. Cancer Res 66(23):11089–11093
Kim MY, Oskarsson T, Acharyya S, Nguyen DX, Zhang XHF, Norton L et al (2009) Tumor self-seeding by circulating cancer cells. Cell 139:1315–1326
Briganti A, Karnes JR, Da Pozzo LF, Cozzarini C, Gallina A, Suardi N et al (2009) Two positive nodes represent a significant cut-off value for cancer specific survival in patients with node positive prostate cancer. A new proposal based on a two-institution experience on 703 consecutive N+ patients treated with radical prostatectomy, extended pelvic lymph node dissection and adjuvant therapy. Eur Urol 55(2):261–270
Heidenreich A, Pfister D, Porres D (2015) Cytoreductive radical prostatectomy in patients with prostate cancer and low volume skeletal metastases: results of a feasibility and case–control study. J Urol 193:832–838
Steinberg GD, Epstein JI, Piantadosi S, Walsh PC (1990) Management of stage D1 adenocarcinoma of the prostate: the Johns Hopkins experience 1974 to 1987. J Urol 144(6):1425–1432
Acknowledgments
The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the Applied Research Program, NCI; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database.
Authors’ contribution
J. Zabell was involved in project development and manuscript writing. O. Adejoro participated in project development, data management, data analysis, and manuscript editing. S. Jarosek was involved in data analysis and manuscript editing. S. P. Elliott contributed to project development and manuscript editing. B. R. Konety was involved in project development and manuscript writing/editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The collection of this data was performed under and IRB-approved protocol. Retrospective analysis was performed using de-identified data.
Conflict of interest
The authors declare no directly relevant conflicts of interest, but all potential conflicts and associations are listed below. Authors J Zabell, O Adejoro, and S Jarosek declare no conflict of interest. Drs. Elliott and Konety have no directly relevant conflicts of interest, but do have the following financial relationships. Dr. Elliott is a consultant/advisor for AMS, GT Urological, Percuvision, Auxilium. Dr. Konety is a consultant/advisor for Photocure, Inc., Axogen, Inc., Dendreon, and has been involved in scientific trial for Dendreon, Myriad Genetics.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zabell, J.R., Adejoro, O., Jarosek, S.L. et al. Impact of initial local therapy on survival in men later receiving chemotherapy for prostate cancer: a population-based, propensity-weighted multivariable analysis. World J Urol 34, 1397–1403 (2016). https://doi.org/10.1007/s00345-016-1790-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-016-1790-x