Abstract
Objectives
To determine added value of permeability MRI in parotid tumor characterization to T2-weighted imaging (T2WI), semi-quantitative analysis of time-intensity curve (TIC), and intra-voxel incoherent motion diffusion-weighted imaging (IVIM-DWI).
Methods
This retrospective study was approved by the institutional review board, and the informed consent was waived. Sixty-one parotid tumors in 61 patients were examined using T2WI, IVIM-DWI, and permeability MRI. TIC patterns were categorized as persistent, washout, or plateau. Signal intensity ratio of lesion-to-muscle on T2WI, apparent diffusion coefficients (ADCs), D and f values from IVIM-DWI, and Ktrans, kep, Ve, and Vp values from permeability MRI were measured. Multiple comparisons were applied to determine whether any differences among 4 histopathologic types (pleomorphic adenomas, Warthin’s tumors, other benign tumors, and malignant tumors) existed. Diagnostic accuracy was compared before and after modification diagnosis referring to permeability MRI. In a validation study, 60 parotid tumors in 60 patients were examined.
Results
ADC and D values of malignant tumors were significantly lower than those of benign tumors other than Warthin’s tumors, but higher than those of Warthin’s tumors. kep and Vp values of Warthin’s tumors were significantly higher than those of malignant tumors. Multivariate analyses showed that TIC pattern, D, and kep values were suitable parameters. McNemar’s test showed a significant increase of sensitivity (11/12, 92%) and specificity (46/49, 94%) with adding kep. The validation study yielded high sensitivity (14/16, 88%) and specificity (41/44, 93%).
Conclusion
Permeability MRI offers added value to IVIM-MRI and semi-quantitative TIC analysis of DCE-MRI in characterization of parotid tumors
Key Points
• Permeability MR imaging offers added value in the characterization of parotid gland tumors in combination with semi-quantitative TIC analysis and IVIM analyses with D parameter.
• The combination of TIC pattern, D, and k ep might facilitate accurate characterization of parotid gland tumor, thereby avoiding unnecessary surgery for benign tumors or delayed treatment for malignant tumors.
• A combination of permeability and diffusion MR imaging can be used to guide the selection of an appropriate biopsy site.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Parotid gland tumors account for about 80–85% of all salivary gland tumors, and approximately 75% of them are benign, especially pleomorphic adenomas [1, 2]. Since the surgical approaches for benign and malignant parotid tumors are different, accurate differentiation of these tumors is important. A superficial parotidectomy or extracapsular dissection is recommended for most benign tumors in the superficial lobe, whereas a conservative parotidectomy is selected for benign tumors in the deep lobe or the inferior portion of the parotid gland [3, 4]. In contrast, a conservative parotidectomy with preservation of facial nerve function is recommended for low-grade malignant parotid tumors in the superficial lobe, and a total parotidectomy is selected for high-grade malignant parotid tumors [2, 5].
Because computed tomography and ultrasound, including elastography, are disappointing [6, 7], preoperative fine-needle aspiration (FNA) cytology is usually performed for initial evaluation of parotid gland tumors [8,9,10]. FNA offers the advantages of minimal invasiveness and a low risk of complications; however, it shows variable sensitivity and specificity in differentiating benign and malignant lesions and has a relatively high rate of insufficient diagnosis [10].
Many studies have assessed MRI findings of parotid gland tumors, and the signal intensity on T2-weighted imaging (T2WI), T2 mapping, tumor capsule, time-intensity curve (TIC) pattern, apparent diffusion coefficient (ADC) values derived from diffusion-weighted imaging (DWI), and intra-voxel incoherent motion diffusion-weighted imaging (IVIM-DWI) parameters have been reported to be suitable parameters [11,12,13,14,15,16]. However, for semi-quantitative and quantitative analyses of the TIC on dynamic contrast-enhanced (DCE)-MRI and DWI, signal intensity or ADC values cannot be considered reliable indicators, because there is relatively large inter-study differences in results, or standardization is still lacking [17, 18].
Permeability imaging or quantitative DCE-MRI is a functional MRI modality that involves repeated acquisition of images of the same lesion and analyses of the TICs of the tumor and feeding artery to yield various parameters related to perfusion and permeability within the tumor. It has been reported to be useful in the differentiation of head and neck tumors [19] as well as tumors in other organs [20,21,22]. Kato et al [23] reported that arterial spin labeling (ASL) could differentiate Warthin’s tumor from pleomorphic adenoma and malignant tumors but could not differentiate pleomorphic adenomas and malignant tumors.
Multiparametric quantitative analyses of MR parameters including quantitative DCE-MRI and DWI in the characterization of parotid tumors have been recently reported using combination pseudo-continuous arterial spin labeling (pCASL) and DWI [24] or TIC pattern with the extracellular extravascular volume fraction (Ve) based on quantitative DCE-MRI [25]. These studies certainly showed the superior diagnostic performance of multiparametric analysis; however, they did not validate their results using another cohort [24, 25].
Thus, the purpose of this study was to determine the added value of permeability MRI to T2WI, semi-quantitative analysis of DCE-MRI, and IVIM-DWI in the characterization of parotid gland tumors.
Materials and methods
Patients
Our retrospective study was approved by the institutional review board, and the requirement for informed consent was waived. A computer search of the radiological reports and surgical records at our institution revealed 124 patients who underwent both DCE-MRI and IVIM-MRI between July 2015 and September 2017. Finally, a total of 61 patients (mean age, 58.5 years; age range, 15–89 years) with parotid gland tumors was enrolled in the clinical and MR data analyses. All patients underwent examinations with DCE-MRI and IVIM-DWI at our hospital. A flow diagram summarizing the initial candidates and each exclusion procedure is shown in Fig. 1.
Histological diagnoses
Histopathologic diagnoses were made on the basis of the findings in specimens obtained by surgical resection (n = 53) or US-guided biopsy (n = 8). Table 1 shows the distribution of histological diagnoses for the 61 parotid gland tumors.
MR imaging technique
MR examinations were performed within 2 weeks before surgery or biopsy in all patients. Patients were examined by using a 3.0-T MR unit (Achieva 3.0T TX, Philips Healthcare) with a 16-channel phased-array neurovascular coil. First, precontrast transverse T1-weighted spin-echo images (see Supplementary material 1 for details) and transverse T2-weighted fast spin-echo images without fat suppression (see Supplementary material 2 for details) were obtained. The IVIM-DWI was performed by using a multisection spin-echo single-shot echo-planar sequence in the transverse plane (see Supplementary material 3 for details). Sensitizing diffusion gradients were applied sequentially in the x, y, and z directions with b values of 0, 50, 500, and 1000 s/mm2. ADC maps were generated. Tumors were identified on the transverse T1-weighted MR images, and 10 sections, including one section that accounted for the maximum diameter of the tumor, were selected for DCE-MRI. A precontrast 3D-T1 fast field echo (FFE) sequence (see Supplementary material 4 for details) was obtained at first. Thereafter, gadobutrol (Gadovist, Bayer HealthCare Pharmaceuticals) was administered intravenously at a rate of 2 mL/s (total dose, 0.1 mmol per kg of body weight) by using a power injector (Sonic Shot 50, Nemoto Kyorindo Co., Ltd.), followed by a 20-mL saline flush. DCE-MRI using the 3D-T1 FFE sequence (using the same parameters as those for precontrast 3D-T1 FFE, but with a flip angle of 15°) was sequentially performed before and every 3.5 s after contrast material administration 95 times for a total of 333 s. Finally, post-contrast transverse T1-weighted spin-echo imaging using the same parameters as precontrast T1-weighted imaging (T1WI) was performed.
Data processing and MRI analysis
Morphological analyses on static MR images
First, the maximal diameters of the tumors were measured on axial T1WI. The presence of a capsule on T2WI was also analyzed. A capsule was defined as a low-intensity thin rim (2 mm or less) surrounding the mass. We assigned grade 2 when the capsule was identified in the entire perimeter of the tumor, grade 1 when the capsule was equal to or more than half the perimeter of the tumor, and grade 0 when the capsule was visible over less than half the perimeter of the tumor.
These analyses were independently interpreted by 2 authors (28 and 22 years of experience in head and neck MRI) who were blinded to the clinical information and histopathological results; a consensus interpretation was reached in cases of disagreement.
Semi-quantitative analysis in DCE-MRI
The same 2 authors who performed morphological analyses on static MR images independently and manually drew regions of interest (ROIs) for signal intensity measurements to avoid the cystic parts of the tumors. Each observer independently selected the maximum diameter level of the tumor, set ROIs on the post-contrast-enhanced T1WI, and copied and pasted it to other images. The range and average of ROI size for each observer in the initial study were as follows: for observer 1, range 36–1408 mm2 and mean 322 mm2, and for observer 2, range 39–1432 mm2 and mean 329 mm2, and those for the validation study were as follows: for observer 1, range 45–956 mm2 and mean 300 mm2, and for observer 2, range 48–972 mm2 and mean 308 mm2. When we had to set two or more ROIs to avoid cystic parts within the tumor, we set multiple circular ROIs with a diameter equal or larger than 6 mm. Then, we selected the area with the highest maximal enhancement among multiple areas. Maximal enhancement was calculated from the following formula: see Supplementary material 5 for details. Then, the average signal intensity within the ROI was plotted against time, and TICs were constructed. Based on the parameters derived from TICs previously reported in an MRI-based study of parotid gland tumors [13], the time to peak and the washout ratio (WR) were defined with the following equations (see Supplementary material 6 for details). The TIC patterns were categorized as follows: persistent pattern, in which the time to peak was more than 120 s; plateau pattern, in which the time to peak was 120 s or less with a low WR (< 30%); and washout pattern, in which the time to peak was 120 s or less with a high WR (≥ 30%).
Quantitative analysis in DCE-MRI
All quantitative analyses in DCE-MRI were performed using a vendor-provided software program (IntelliSpace Portal Ver. 6.0, Philips Healthcare). This system is based on a Tofts model, by which pixel-based parameter maps are generated from TICs [26]. For the quantitative analysis, the same 2 authors independently copied and pasted the ROI to each permeability maps to obtain Ktrans, kep, Ve, plasma fraction, and area under the curve values from the semi-quantitative analysis. The 2 authors also set the same ROI size in the contralateral normal parotid gland to obtain Ktrans, kep, Ve, plasma fraction, and area under the curve values of normal parotid gland tissue. The contrast relaxivity was set to 3.9 s−1/mmol. Arterial input function (AIF) correction was used to set the ROI in the affected side of external carotid artery (Supplementary Fig. a) and judged whether it showed a pulsed input pattern or a non-pulsed input pattern. AIF correction was not adopted unless at least one AIF curve among 49 AIF curves showed the pulsed input pattern (Supplementary Fig. b, yellow curve).
Quantitative analysis of IVIM images
For measurements of the ADC and IVIM parameters (D and f), pixel-based ADC and D maps were obtained at a commercial workstation (Synapse Vincent, Fujifilm), and the same 2 authors independently placed the ROIs within the same areas as those used for the TIC construction. ROIs for TIC construction and ADC measurement were chosen such that they avoided obvious cystic areas. A cystic area was defined as a lesion area that showed high intensity on T2WI and was not enhanced on contrast-enhanced MRI images. The 2 authors also set the same ROI size in the contralateral normal parotid gland to obtain IVIM parameters of normal parotid gland tissue. In addition, the same authors measured the signal intensity of the tumor and that of the neighborhood muscle on T2-weighted images to set the ROIs within the same areas as those used for the TIC construction, and calculated the signal intensity (SI) ratiolesion/muscle. The 2 authors also set the same ROI size in the contralateral normal parotid gland and that of the neighborhood muscle to obtain the SI ratiolesion/muscle of normal parotid gland tissue. In this study, T2-weighted images were obtained using a parallel imaging technique, and various degrees of sensitivity corrections were used for each receiver coil. Therefore, we used SI ratiolesion/muscle, not absolute SI on T2-weighted images.
Statistical analysis
Inter-observer agreements in the measurement of each quantitative MR parameter were assessed by using Spearman’s rank correlation coefficient and Bland-Altman plot. Limits of agreement given by 95% confidence intervals (CIs) were calculated by using Bland-Altman analysis [27]. We also added the intra-class correlation coefficients (ICCs). Both Spearman’s correlation coefficients and ICCs were regarded as follows: r/ICC < 0.2, poor correlation/agreement; r/ICC = 0.2–0.4, fair correlation/agreement; r/ICC = 0.41–0.6, moderate correlation/agreement; r/ICC = 0.61–0.8, good correlation/agreement; and r/ICC > 0.81, excellent correlation/agreement. For categorical variables, such as the presence of a capsule and the TIC pattern, inter-observer agreements were evaluated by using a linear type of weighted k statistics.
In the present study, all statistical analyses were performed using non-parametric statistical tests because a normal distribution of the continuous variables could not be assumed (age, maximal diameter of the tumor, SI ratiolesion/muscle, ADC, D, f, D*, Ktrans, kep, Ve, Vp). For statistical analyses, we analyzed age, sex, presence of facial nerve palsy, maximal diameter, presence of capsule, lesion-to-muscle SI ratio, TIC pattern, IVIM parameters (ADC, D, f, and D*), and permeability MRI parameters (Ktrans, kep, Ve, Vp). First, we performed univariate analysis among 4 groups: pleomorphic adenomas, Warthin’s tumors, other benign tumors, and malignant tumors using Kruskal-Wallis and Steel-Dwass tests for multigroup comparisons. The level of significance in the univariate analysis that was used for inclusion in the multivariate analysis model was less than 0.05/6 = 0.008. In addition, receiver operating characteristic (ROC) curves were used to determine the optimal cutoff levels of the significant parameters to enable differentiation of specific pairs of histological types. Next, we performed multivariate analyses with logistic regression analyses. These multivariate analyses were also performed in 4 subgroups. These subgroup analyses could increase type I error; therefore, we applied the Bonferroni correction for multiple comparisons and set the corrected significance level to less than 0.05/6 = 0.008. Third, we performed decision tree analysis using the significant parameters obtained after multivariate analysis. Finally, using McNemar’s test, we compared the diagnostic accuracy before and after diagnoses using the TIC pattern alone versus the TIC pattern and IVIM, and the TIC pattern and IVIM versus a combination of the TIC pattern, IVIM, and permeability MRI. These comparisons among three patterns could also increase type I error; therefore, we applied the Bonferroni correction for multiple comparisons and set the corrected significance level to less than 0.05/3 = 0.017. Computer software programs (JMP Pro 13.0.0; SAS and MedCalc, version 18; MedCalc software) were used to analyze the raw data.
Validation study
To test the true diagnostic value of the proposed diagnostic flow diagram, we applied it to 60 parotid gland tumors in 60 consecutive adult patients who underwent T2WI, DCE-MRI, and IVIM-DWI between October 2017 and December 2018. The technique used to visualize and evaluate the tumors and the exclusion criteria was otherwise the same as that used in the initial part of the study. A flow diagram summarizing the candidates of the validation study and each exclusion procedure is shown in Fig. 2.
The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of the proposed classifications derived from the initial study results for differentiation of parotid gland tumors were examined. When we assumed tumors as malignant based on the decision tree analysis and histological results were also malignant tumors, they were regarded as true-positive results.
Results
Inter-observer agreements
Spearman’s rank correlation coefficients between 2 observers showed good to excellent correlation in evaluations of quantitative parameters (see Supplementary material 7 for details). Limits of agreement in Bland-Altman plots of inter-observer variabilities in the measurement of quantitative parameters showed the following findings: see Supplementary material 8 for details. ICC of the tumor assessment also showed excellent agreements except for f as fair agreement (see Supplementary material 10 for details). In addition, ICC of the normal parotid gland assessment also showed excellent agreements except for f as moderate agreement (see Supplementary material 9 for details).
For the inter-observer agreements of categorical variables of TIC pattern, k value for the 2 observers was in the almost perfect range (0.98).
Clinical data evaluation
Table 2 shows the distribution of clinical data among the 4 histological groups (pleomorphic adenomas, Warthin’s tumors, other benign tumors, and malignant tumors). Multivariate analysis showed that there was no significant difference among the four histologic types in terms of age, sex, and facial nerve palsy.
MR image evaluation
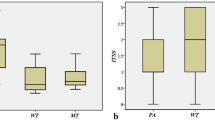
Table 2 shows the distribution of MR characteristics among the 4 histological diagnosis groups. Univariate analysis showed significant differences among the 4 histologic types in the grade of the peritumoral capsule, SI ratiolesion/muscle on T2WI, TIC pattern, ADC, D, kep, Ve, and Vp. Multivariate analysis revealed 3 significant features, i.e., the TIC pattern, the IVIM parameter of D, and the permeability parameter of kep. Figure 3 a and b show scatter plots of D value and kep with cutoff values among 4 histologic subtypes, respectively. Figure 4 shows a flow diagram derived from a decision tree analysis combining the TIC pattern, D values, and kep values of the lesions to differentiate the 4 histological types of parotid gland tumors based on the results of the initial study. It involves the TIC pattern in the first step, the D value in the second step, and the kep value in the last step. Regarding the AIF correction, we could select the best pulsed input pattern among 49 AIF curves in all patients and use manual AIF correction in all patients in both initial and validation study groups.
a Scatter plot of D value among 4 histologic subtypes. The black circles show each D value of the case. The red square and error bars represent the median value and 25th–75th percentiles of D value in each histologic type, respectively. The cutoff value to differentiate between pleomorphic adenomas and other 3 histologic types is 1.22 (× 10−3 mm2/s), that between other benign tumors and malignant tumors/Warthin’s tumors is 1.06 (× 10−3 mm2/s), and that between malignant tumors and Warthin’s tumors is 0.89 (× 10−3 mm2/s), respectively. b Scatter plot of kep value among 4 histologic subtypes The black circles show each kep value of the case. The red square and error bars represent the median value and 25th–75th percentiles of kep value in each histologic type, respectively. The cutoff value to differentiate between Warthin’s tumors and other 3 histologic types is 581 (× 10−3/min), and that between malignant tumors and other benign tumors/pleomorphic adenomas is 321 (× 10−3/min), respectively
Decision-tree algorithm for differential diagnosis of a parotid tumor The first row shows the classifications according to the TIC pattern, the second row shows those according to the D values, and the bottom row shows those according to the kep values. The blue steps show the benign tumor diagnoses, and the pink steps show the malignant tumor diagnoses
Evaluation of diagnostic value
Table 3 summarizes the diagnostic value of TIC patterns alone, the combination of TIC patterns and D values, and the combination of TIC patterns, D values, and kep values. When we assigned a diagnosis on the basis of TIC patterns alone and regarded persistent and washout TIC pattern lesions as benign tumors and plateau TIC pattern lesions as malignant tumors, the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value were 50% (6/12), 69% (34/9), 66% (40/61), 29% (6/21), and 85% (34/40), respectively. Single sensitivity, specificity, and accuracy from TIC pattern, D, and kep were (6/12, 50%; 34/49, 69%; 40/61, 66%), (3/12, 25%; 42/49, 86%; 45/61, 74%), and (9/12, 75%; 40/49, 82%; 49/61, 80%), respectively. When we applied D values to TIC patterns and modified the diagnosis with reference to the D values, the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value were 67% (8/12), 82% (40/49), 79% (48/61), 53% (8/15), and 87% (40/46), respectively. The use of D value thresholds improved the diagnostic values, although p value did not reach the corrected significance level (p = 0.013). When we applied kep values to TIC patterns plus D values and modified the diagnosis with reference to the kep values, the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value were 92% (11/12), 94% (46/49), 93% (57/61), 79% (11/14), and 98% (46/47), respectively. The use of kep value thresholds significantly improved the diagnostic values further (p = 0.0078). Two representative cases are shown in Figs. 5 and 6. These cases could be correctly diagnosed because of permeability imaging.
Pleomorphic adenoma of the right parotid gland in a 66-year-old woman. a Transverse T2-weighted MR image shows a heterogeneously hyperintense mass with the entire capsule (arrow) in the right parotid gland. b TIC pattern derived from DCE-MRI shows a plateau pattern. c The D map derived from IVIM-DWI shows a mass with slightly low signal intensity (arrow, D = 0.78). d The kep map derived from DCE-MRI shows low kep (264) of the tumor (arrow). The plateau TIC pattern and the low D value, which is smaller than the cutoff value (1.06), indicate a malignant tumor; however, the low kep value (264), which is smaller than the cutoff value (321), finally leads to a diagnosis of a benign tumor. This is a representative case in which the addition of permeability imaging was useful
Acinic cell carcinoma of the right parotid gland in a 73-year-old man. a Transverse T2-weighted MR image shows a heterogeneously hyperintense mass with incomplete capsule (arrow) in the right parotid gland. b TIC pattern derived from DCE-MRI shows a plateau pattern. c The D map derived from IVIM-DWI shows a mass with slightly high-signal intensity mass (arrow, D = 1.15). d The kep map derived from DCE-MRI shows slightly high kep value (398) of the tumor (arrow). The plateau TIC pattern indicates a malignant tumor; however, the addition of the relatively high D value (1.15), which is larger than the cutoff value (1.06), indicates a benign tumor; the high kep value (398), which is larger than the cutoff value (321), finally leads to the correct diagnosis of a malignant tumor
Validation study results
Tables 1 and 3 also show the results of the validation study involving 60 tumors in 60 patients. When we applied the diagnostic algorithm combining the TIC pattern and the D and kep values, the sensitivity, specificity, accuracy, positive predictive value, and negative predictive value were 88% (14/16), 93% (41/44), 92% (55/60), 82% (14/17), and 95% (41/43), respectively (Table 3). The use of kep value thresholds improved the diagnostic values although p value did not reach the corrected significance level (p = 0.03).
Discussion
Our study findings showed that the addition of permeability MRI to semi-quantitative TIC analysis and IVIM imaging could improve diagnostic accuracy in the characterization of parotid gland tumors. The addition of kep values is particularly useful when differentiating benign parotid gland tumors with a plateau TIC pattern and a low D value and malignant tumors with a washout TIC pattern with a low D value, which were respectively misdiagnosed as malignant and benign tumors without permeability MRI.
Semi-quantitative analyses in DCE-MRI could be affected by the total dose and injection rate of the contrast medium, input arterial flow, and patient hemodynamics including the cardiac ejection fraction [17]. Perfusion MRI can be adjusted by the AIF, and it can provide additional physiological information related to the permeability of capillary membrane, capillary vascular space, and extravascular and extracellular space [18]. Therefore, we hypothesized that we might be able to obtain unique information from permeability MRI that could not be known by semi-quantitative analysis of TIC patterns or diffusion.
The only significant parameter derived from perfusion MRI in this study was kep, which represents a rate constant between the extravascular extracellular space and blood plasma. We speculated that these results are similar to those for the semi-quantitative TIC pattern; high kep values corresponded to a high WR, and low kep values corresponded to a low WR. Using this approach, it may be possible to analyze the movement of contrast medium between the extravascular extracellular space and blood plasma more accurately.
There have been several reports on the characterization of parotid gland tumors using functional MRI data such as the semi-quantitative and quantitative analyses of DCE-MRI, ADC values, IVIM parameters, pCASL parameter, and T2 mapping. Yabuuchi et al [14] reported that a persistent or flat TIC pattern on dynamic contrast-enhanced MR images indicates benign disease, but there is added value from including the ADC value in the evaluation of tumors that show a plateau or washout TIC pattern. Sumi et al [15] reported that IVIM parameters including f, D, and D* values could differentiate benign from malignant salivary gland tumors. As for the utility of perfusion imaging in the characterization of parotid gland tumors, Xu et al [25] recently reported that TIC pattern in combination with the Ve based on quantitative DCE-MRI could achieve the best diagnostic performance in the differential diagnosis of parotid tumors, and Kato et al [23] reported that ASL could differentiate Warthin’s tumors from pleomorphic adenomas and malignant tumors. Razek [24] recently reported that multiparametric MR imaging using pCASL and DWI was useful for differentiating parotid tumors. These studies certainly showed the superior diagnostic performance of multiparametric analysis; however, they did not validate their results using another cohort [24, 25].
This study has some limitations. First, the number of malignant lesions is relatively small. Therefore, the distribution of histologic types among the malignant tumors might have affected the results. Moreover, the small sample size of each subgroup might have reduced the statistic power. The low rates of malignancy (initial study, 20%; validation study, 27%) in our study might lead to disadvantage for sensitivity and to advantage for specificity, because we defined malignancy as a true positive case. Second, the number of b factors in IVIM imaging was limited to shorten the total imaging time. Third, it is well known that volumetric analysis avoids the possibility of sampling error that is inherent in 2D evaluations; however, we could not perform a 3D VOI approach, because it was not available in our institute. However, to our knowledge, this is the first report on the added value of using a combination of semi-quantitative TIC analysis, IVIM-MRI, and permeability MRI using decision tree analysis based on multiparametric analysis of 3 parameters for characterization of parotid gland tumors.
In conclusion, permeability MRI offers added value in the characterization of parotid gland tumors to IVIM-MRI and semi-quantitative TIC analysis of DCE-MRI.
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- AIF:
-
Arterial input function
- ASL:
-
Arterial spin labeling
- D :
-
True diffusion coefficient
- DWI:
-
Diffusion-weighted imaging
- FFE:
-
Fast field echo
- FNA:
-
Fine-needle aspiration
- IVIM:
-
Intra-voxel incoherent motion
- k ep :
-
Rate constant from extracellular extravascular space to plasma
- K trans :
-
Rate constant from plasma to extracellular extravascular space
- MRI:
-
Magnetic resonance imaging
- ROI:
-
Region of interest
- SI:
-
Signal intensity
- T2WI:
-
T2-weighted imaging
- TIC:
-
Time-intensity curve
- V e :
-
Extracellular extravascular volume fraction
- V p :
-
Plasma fraction
- WR:
-
Washout ratio
References
Guzzo M, Locati LD, Prott FJ, Gatta G, McGurk M, Licitra L (2010) Major and minor salivary gland tumors. Crit Rev Oncol Hematol 74:134–148
Spiro RH (1986) Salivary neoplasms: overview of a 35-year experience with 2,807 patients. Head Neck Surg 8:177–184
Larian B (2016) Parotidectomy for benign parotid tumors. Otolaryngol Clin North Am 49:395–413
Dell'Aversana Orabona G, Bonavolontà P, Iaconetta G, Forte R, Califano L (2013) Surgical management of benign tumors of the parotid gland: extracapsular dissection versus superficial parotidectomy-our experience in 232 cases. J Oral Maxillofac Surg 71:410–413
Lim YC, Lee SY, Kim K et al (2005) Conservative parotidectomy for the treatment of parotid cancers. Oral Oncol 41:1021–1027
Zhang YF, Li H, Wang XM, Cai YF (2019) Sonoelastography for differential diagnosis between malignant and benign parotid lesions: a meta-analysis. Eur Radiol 29:725–735
Zengel P, Notter F, Clevert DA (2018) Does acoustic radiation force elastography improve the diagnostic capability of ultrasound in the preoperative characterization of masses of the parotid gland? Dentomaxillofac Radiol 47:20180068
Christensen RK, Bjørndal K, Godballe C, Krogdahl A (2010) Value of fine-needle aspiration biopsy of salivary gland lesions. Head Neck 32:104–108
Howlett DC, Menezes LJ, Lewis K, Moody AB, Violaris N, Williams MD (2007) Sonographically guided core biopsy of a parotid mass. AJR Am J Roentgenol 188:223–227
Liu CC, Jethwa AR, Khariwala SS, Johnson J, Shin JJ (2016) Sensitivity, specificity, and posttest probability of parotid fine-needle aspiration: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 154:9–23
Ishibashi M, Fujii S, Kawamoto K et al (2010) Capsule of parotid gland tumor: evaluation by 3.0 T magnetic resonance imaging using surface coils. Acta Radiol 51:1103–1110
Okahara M, Kiyosue H, Hori Y, Matsumoto A, Mori H, Yokoyama S (2003) Parotid tumors: MR imaging with pathological correlation. Eur Radiol 13:25–33
Yabuuchi H, Fukuya T, Tajima T, Hachitanda Y, Tomita K, Koga M (2003) Salivary gland tumors: diagnostic value of gadolinium-enhanced dynamic MR imaging with histopathologic correlation. Radiology 226:345–354
Yabuuchi H, Matsuo Y, Kamitani T et al (2008) Parotid gland tumors: can addition of diffusion-weighted MR imaging to dynamic contrast-enhanced MR imaging improve diagnostic accuracy in characterization? Radiology 249:909–916
Sumi M, Van Cauteren M, Sumi T, Obara M, Ichikawa Y, Nakamura T (2012) Salivary gland tumors: use of intravoxel incoherent motion MR imaging for assessment of diffusion and perfusion for the differentiation of benign from malignant tumors. Radiology 263:770–777
Wu Q, Zhu LN, Jiang JS, Bu SS, Xu XQ, Wu FY (2020) Characterization of parotid gland tumors using T2 mapping imaging: initial findings. Acta Radiol:629–635
Leiva-Salinas C, Provenzale JM, Kudo K, Sasaki M, Wintermark M (2012) The alphabet soup of perfusion CT and MR imaging: terminology revisited and clarified in five questions. Neuroradiology 54:907–918
Calamante F (2013) Arterial input function in perfusion MRI: a comprehensive review. Prog Nucl Magn Reson Spectrosc 74:1–32
Lee FK, King AD, Ma BB, Yeung DK (2012) Dynamic contrast enhancement magnetic resonance imaging (DCE-MRI) for differential diagnosis in head and neck cancers. Eur J Radiol 81:784–788
Cha S, Yang L, Johnson G et al (2006) Comparison of microvascular permeability measurements, K(trans), determined with conventional steady-state T1-weighted and first-pass T2*-weighted MR imaging methods in gliomas and meningiomas. AJNR Am J Neuroradiol 27:409–417
Falk A, Fahlström M, Rostrup E et al (2014) Discrimination between glioma grades II and III in suspected low-grade gliomas using dynamic contrast-enhanced and dynamic susceptibility contrast perfusion MR imaging: a histogram analysis approach. Neuroradiology 56:1031–1038
Li X, Arlinghaus LR, Ayers GD et al (2014) DCE-MRI analysis methods for predicting the response of breast cancer to neoadjuvant chemotherapy: pilot study findings. Magn Reson Med 71:1592–1602
Kato H, Kanematsu M, Watanabe H et al (2015) Perfusion imaging of parotid gland tumours: usefulness of arterial spin labeling for differentiating Warthin’s tumours. Eur Radiol 25:3247–3254
Razek AAKA (2019) Multi-parametric MR imaging using pseudo-continuous arterial-spin labeling and diffusion-weighted MR imaging in differentiating subtypes of parotid tumors. Magn Reson Imaging 63:55–59
Xu Z, Zheng S, Pan A, Cheng X, Gao M (2019) A multiparametric analysis based on DCE-MRI to improve the accuracy of parotid tumor discrimination. Eur J Nucl Med Mol Imaging 46:2228–2234
Tofts PS, Brix G, Buckley DL et al (1999) Estimating kinetic parameters from dynamic contrast-enhanced T(1)-weighted MRI of a diffusable tracer: standardized quantities and symbols. J Magn Reson Imaging 10:223–232
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Hidetake Yabuuchi.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Informed consent was waived.
Ethical approval
Institutional review board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 19 kb)
Rights and permissions
About this article
Cite this article
Yabuuchi, H., Kamitani, T., Sagiyama, K. et al. Characterization of parotid gland tumors: added value of permeability MR imaging to DWI and DCE-MRI. Eur Radiol 30, 6402–6412 (2020). https://doi.org/10.1007/s00330-020-07004-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07004-3