Abstract
Objective
To evaluate the performance of image-guided core needle biopsy (IGCNB) for the diagnosis of Ewing sarcoma of bone.
Methods
All patients with a confirmed diagnosis of Ewing sarcoma who underwent IGCNB between January 2007 and December 2016 were included in this retrospective study. Analysis included mean age, skeletal distribution, imaging modality used for biopsy guidance, type of anaesthesia, needle type, number of passes, type of tissue sampled, and complications.
Results
The study included 139 patients (94 males and 45 females; mean age 18.7 years) who underwent 141 image-guided core needle biopsies as the primary diagnostic test. Of these, 101 were CT-guided, 38 ultrasound-guided, and 2 utilised both CT and ultrasound guidance. A total of 97.9% were diagnostic at first procedure. Of the 3 non-diagnostic cases, 2 underwent a further IGCNB and were positive, while 1 patient required an open surgical procedure. Only 1 patient (0.7%) suffered an immediate complication, and there were no recorded delayed complications.
Conclusion
IGCNB is a safe procedure providing a positive diagnosis of Ewing sarcoma of bone in a very high percentage of cases. It should be the first-line method for establishing a diagnosis in suspected Ewing sarcoma of bone.
Key Points
• Image-guided core needle biopsy is a safe procedure providing a positive diagnosis of Ewing sarcoma of bone in a very high percentage of cases.
• Image-guided core needle biopsy should be the first-line method for establishing a definitive diagnosis in Ewing sarcoma and should be performed at a specialist sarcoma referral centre.
• When technically feasible, extra-osseous soft tissue alone can be sampled with confidence as there is no difference in diagnostic performance whether bone or an extra-osseous soft tissue component of the tumour is sampled.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A variety of options are available for achieving a histological diagnosis of a suspected bone tumour, including fine needle aspiration cytology (FNAC), image-guided core needle biopsy (IGCNB), and surgical incisional biopsy [1, 2]. CT-guided core needle biopsy has a diagnostic accuracy that is not significantly inferior to incisional biopsy in a wide variety of bone and soft tissue tumours, while being associated with fewer complications [3], and a recent meta-analysis has supported the role of specialist radiologists utilising IGCNB for the diagnosis of musculoskeletal bone and soft tissue lesions [4].
However, with regard to individual tumour types, it is known that IGCNB can be problematic. A diagnosis of aneurysmal bone cyst (ABC) was achieved in only 36% of cases by IGCNB compared with 96% for surgical curettage/resection [5], and the correct grading of chondral tumours may show mismatch on IGCNB compared with final surgical resection histology in up to 74% of pelvic tumours [6]. With regard to Ewing sarcoma of bone, reported biopsy success rates vary from 50 to 88% in sample sizes ranging from 5 to 40 patients [7,8,9,10,11]. A study comparing open biopsy with needle biopsy for suspected Ewing sarcoma suggested that the success rate for needle biopsy is inferior [11], which would support the continued use of surgical open biopsy with its associated increased risks and cost. This prompted us to review our experience of IGCNB as the primary technique for the diagnosis of Ewing sarcoma of bone.
Materials and methods
The study was approved by the local Research and Innovation Centre of The Institute of Orthopaedics, with no requirement for informed patient consent.
All patients with a histologically confirmed diagnosis of Ewing sarcoma of bone between January 2007 and December 2016 were identified from the pathology database. Patients presenting with recurrent Ewing sarcoma or extra-skeletal Ewing sarcoma were excluded. Data collected included gender, mean age, skeletal distribution, imaging modality for biopsy guidance, type of anaesthesia, type of needle, number of passes, type of tissue sampled (bone, soft tissue, or both), and complications. The histology results for IGCNB were then reviewed, with the biopsy considered to be diagnostic if adequate tissue had been obtained to yield a definitive histological diagnosis.
All biopsies were performed in line with the British Sarcoma Group 2016 guidelines [12], with a summary of the biopsy guidelines outlined in Table 1. Each biopsy was planned in the sarcoma multidisciplinary team (MDT) meeting following consultation between a radiologist and a surgeon. All patients had pre-biopsy MRI studies available, and the optimal biopsy approach was marked with an arrow on an axial image for future reference. The type of image guidance and anaesthesia was based on certain patient and lesion characteristics. CT guidance was chosen for lesions where it was felt that the bone needed to be sampled, or for lesions at difficult anatomical sites such as the pelvis or spine. US guidance was chosen for lesions which had a large (> 2 cm) extra-osseous component which was located close to the skin surface and was therefore easily amenable to US evaluation. General anaesthesia (GA) was chosen for children and adolescents, for deeply located lesions, and in cases with pathological fracture. Local anaesthesia (LA) was chosen for adult patients where there was an extra-osseous component close to the skin surface which could be easily accessed. All biopsies were performed by or under the direct supervision of a consultant musculoskeletal radiologist. The entry point was chosen corresponding to the biopsy site decided at MDT, and a single 5-mm stab incision was made. When multiple passes were undertaken, these were always made through the same entry point but with slightly varied angulation of the needle allowing different parts of the tumour to be sampled. Following completion of the biopsy, the biopsy site was marked with a tiny India ink tattoo so that it could be identified and excised at the time of surgery. All specimens were evaluated by experienced bone tumour pathologists. The procedure report and correspondence from the first outpatient appointment following biopsy were reviewed to identify any immediate or delayed complications.
Statistical analysis
Descriptive statistics were performed to determine the assessed variables, including lesion location, type of image guidance, type of needle used, type of anaesthetic, type of tissue sampled, and rate of positive biopsies for each of the above.
Results
The study group comprised 139 patients with a mean age of 18.7 years (range 2–56 years), including 94 males and 45 females. All patients had undergone IGCNB as the primary diagnostic procedure, with no patients having a primary open surgical biopsy. The lesions arose in the appendicular skeleton in 64 of 139 cases (46.0%), the flat bones in 59 of 139 cases (42.4%), the spine in 11 of 139 cases (7.9%), and the foot in 5 of 139 cases (3.6%). The most common location was the pelvis, affecting 36 of 139 cases (25.9%), followed by the femur which accounted for 33 of 139 cases (23.7%). The skeletal distribution is summarised in Table 2. One hundred and thirty-four (96.4%) tumours were located centrally in the medullary cavity, while 5 (3.6%) arose from the surface of the bone. Of the 134 intra-medullary tumours, 132 (98.5%) had an extra-osseous component as identified by MRI at the time of initial staging.
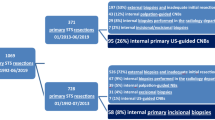
Procedure characteristics are summarised in Table 3. A total of 141 IGCNBs were performed, 101 of 141 (71.6%) CT-guided, 38 of 141 (26.9%) US-guided, and 2 of 141 (1.4%) utilising both CT and US guidance. This was due to the personal choice of the performing radiologist to use CT guidance to target bone and US to target the soft tissue component. One hundred and nine of 139 (78.4%) cases were performed under GA and 30 of 139 (21.6%) under LA. The mean age for patients undergoing GA biopsy was 15.8 years (range 2–49 years) and for those undergoing LA biopsy was 28.2 years (range 18–56 years). Of the CT-guided biopsies, 91 of 101 (90.1%) were under GA and 10 of 101 (9.9%) under LA. Nineteen of 38 (50%) US-guided biopsies were performed under GA while 19 of 38 (50%) were under LA. GA was administered in 1 of the 2 biopsies where both CT and US guidance was used.
As demonstrated in Table 4, a variety of needle types were used, including 14G Temno (Temno Evolution™ Biopsy Needle; Merit Medical), 11G and 13G Jamshidi (T-handle Jamshidi™ bone marrow biopsy aspiration needle; BD), and 14G Tru-Cut (Tru-Cut™ biopsy needle; Merit Medical). In certain cases where both bone and soft tissue were biopsied, a combination of needles was employed. The number of passes was recorded in 91 cases and ranged from 1 to 10 (mean number of passes 4.9), while in the remaining cases, the reports simply indicated that multiple passes had been made. Only 8 procedures recorded a single pass, when an aspiration biopsy of the medullary cavity had been performed.
With regard to the type of tissue sampled, soft tissue only was sampled in 95 of 141 cases (67.4%), bone only in 27 of 141 cases (19.1%), and both bone and soft tissue in 19 of 141 cases (13.5%). Among CT-guided procedures, soft tissue only was sampled in 57 of 101 (56.4%) and bone only in 27 of 101 (26.7%), while in 17 of 101 procedures (16.8%), a combination of bone and soft tissue was taken. As expected, all 38 (100%) US-guided biopsies targeted soft tissue only, and in the 2 cases using both CT and US guidance, both soft tissue and bone were sampled. Figures 1, 2, and 3 illustrate the varied techniques in 3 selected cases.
a Lateral and (b) AP radiographs in a 15-year-old male demonstrate periosteal reaction with a Codman triangle in the left distal femoral diaphysis. c Coronal STIR and (d) axial T1W SE MR images demonstrate a heterogeneous mass arising from the left femoral diaphysis. e CT-guided biopsy under general anaesthesia of the soft tissue mass using a 14G Temno needle yielded a diagnosis of Ewing sarcoma
a Coronal T1W SE and (b) axial STIR MR images in a 28-year-old male with an infiltrative mass in the right ilium crossing the sacroiliac joint into the right sacral ala, associated with a large extra-osseous soft tissue mass. c CT-guided biopsy of the right iliac bone using an 11G Jamshidi needle and (d) of the extra-osseous soft tissue mass posterior to the sacrum using a 14G Temno needle was performed under general anaesthesia confirming Ewing sarcoma
a AP radiograph in a 20-year-old male demonstrating permeative bone destruction and periosteal reaction in the left fibular diaphysis. b Coronal T1W SE and (c) axial fat-saturated T2W FSE MR images showing an infiltrative mass with a large extra-osseous soft tissue component. d US-guided biopsy of the soft tissue mass performed under local anaesthesia with a 14G Temno needle yielded a diagnosis of Ewing sarcoma
Of the 141 IGCNBs, 138 (97.9%) provided a positive diagnosis at the first procedure. All US-guided needle biopsies were diagnostic, while 98 of 101 (97.0%) CT-guided biopsies were positive. Three of the 101 (2.97%) CT-guided procedures were non-diagnostic. Details of these are as follows:
-
Case 1: A 10-year-old female with a mass arising from the left ischium, where the large soft tissue component was initially biopsied with 3 passes of a 14G Tru-Cut needle under CT guidance and GA. As there was insufficient material for diagnosis, the biopsy was repeated under CT guidance and GA 1 week later at which time bone was sampled with 2 passes using an 11G Jamshidi needle, confirming a diagnosis of Ewing sarcoma.
-
Case 2: A 17-year-old male with a right proximal tibial metaphyseal tumour, in whom initial histology revealed a high-grade malignant round cell tumour with extensive necrosis precluding definitive diagnosis. The initial biopsy was performed under CT guidance and GA with 2 passes using an 11G Jamshidi needle into bone. A definitive diagnosis of Ewing sarcoma was reached when the CT-guided needle biopsy was repeated under GA 2 weeks later, this time sampling the associated soft tissue mass with 3 passes of a 14G Temno needle.
-
Case 3: A 15-year-old male with a right proximal femoral metadiaphyseal mass who underwent a CT-guided biopsy under GA. Two passes with an 11G Jamshidi needle into bone yielded a paucicellular sample, following which a diagnostic open biopsy was required.
Post-procedural complications were recorded in one case, a 17-year-old female with Ewing sarcoma in her left hemi-pelvis who underwent a CT-guided biopsy under GA sampling soft tissue with 4 passes of a 14G Temno needle. The patient developed urinary retention following the procedure requiring an indwelling catheter and had a prolonged hospital stay, with an admission to the intensive care unit for pain management. However, there was no long-term complication. The immediate clinically apparent complication rate was therefore 0.7%. Review of the first outpatient clinic letter following biopsy revealed no clinically apparent delayed complications.
Discussion
As outlined in the British Sarcoma Group 2016 guidelines by Gerrand and colleagues [12], IGCNB of suspected primary bone sarcomas should be performed at a specialist sarcoma referral centre in consultation with the surgical team that will carry out definitive tumour resection. MRI of the affected bone should be available to plan the biopsy approach and most representative area to sample [13]. The biopsy needle track should be placed to minimise contamination of normal tissues, and so that it can be incorporated into the final surgical excision. The biopsy site can be marked with a skin tattoo, which will allow its identification at time of surgery following neoadjuvant chemotherapy [14].
Open biopsy had historically been considered the gold standard for histological diagnosis of bone tumours [1]. However, open biopsy poses certain risks to the patient, while needle biopsy possesses several advantages. IGCNB has therefore become the gold standard for definitive diagnosis due to its less invasive nature, safety, and cost-effectiveness [3]. Needle biopsy has been reported to be less painful, require a shorter length of hospital stay, and more readily enable sampling of different tumour components to obtain representative tissue compared with open biopsy. Needle biopsy results in lower complication rates including infection, haematoma, fracture, and tumour seeding, leading to local progression. Neoadjuvant chemotherapy and radiotherapy can be commenced more rapidly following needle biopsy, whereas a delay of 10 days to 3 weeks may be required to allow wound healing following an open surgical approach. Furthermore, a percutaneous approach may reduce the amount of tissue that needs to be resected at the time of definitive surgery. The rates of altered treatment and altered outcome due to a poorly performed biopsy have been found to be significantly lower for needle biopsy compared with those for open biopsy [15]. Nevertheless, larger resections and amputations due to inappropriate needle biopsy technique where limb salvage would otherwise have been possible, have also been reported [15]. Finally, tumours in deep locations such as the pelvis or the spine may be more readily accessible via a percutaneous approach.
The current study is the largest report of IGCNB for primary Ewing sarcoma of bone, in which a positive diagnosis was achieved at the first procedure in 97.9%, and in 2 of 3 initially negative results at second IGCNB. Only a single patient required an open surgical procedure to obtain the diagnosis. The positive diagnostic rate was not dependent upon type of image guidance, type of anaesthesia, or type of needle used. The number of needle passes was not specifically recorded in each individual case, but also did not appear to impact upon diagnostic performance since all 3 failed procedures had more than a single pass. Over 98% of intra-medullary tumours exhibited an extra-osseous component. Given that there was no difference in diagnostic performance whether soft tissue or bone was sampled, we believe that when technically feasible extra-osseous soft tissue alone can be sampled with confidence. This may in turn reduce the difficulty and length of the procedure, enable the use of US guidance, and obviate the need for GA in many adult cases. In the 3 non-diagnostic biopsies, there were no technical factors that could be identified to explain the outcome. All were performed under CT guidance and GA. Two of these patients had a successful repeat CT-guided biopsy under GA where the type of tissue sampled differed from the initial biopsy, while one patient proceeded to a diagnostic open biopsy. In a review of lesion-related and technical factors affecting diagnostic yield in IGCNB of bone and soft tissue lesions, Wu and colleagues found that diagnostic yield was higher in lytic than in sclerotic bone lesions and in larger lesions, factors that we did not assess although Ewing sarcoma is almost always a lytic lesion. In line with our findings, needle type and imaging modality did not impact upon their diagnostic yield [16].
Our positive diagnostic rate for Ewing sarcoma of bone is well above figures reported in the literature, which range from 50 to 88% in sample sizes ranging from 5 to 40 patients [7,8,9,10,11]. Interiano et al performed a retrospective review of children and young adults diagnosed with osteosarcoma and Ewing sarcoma over a 10-year period [9]. One hundred and forty-two biopsies of primary and distant sites were performed in 105 patients, of which 38 biopsies revealed a diagnosis of Ewing sarcoma. Where the primary lesion was sampled, a diagnostic specimen was obtained in 94.1% of open biopsies, but only 73.1% of percutaneous biopsies. Adverse events including post-operative haematoma, pathological fracture, wound infection, and blood transfusion were recorded in 4 patients, of whom 3 had undergone open procedures. Jelinek et al found percutaneous biopsy to have a diagnostic accuracy of 88% in 110 patients with primary bone tumours, of which 6 were Ewing sarcoma [10]. Didolkar et al reviewed 778 IGCNB of bone and soft tissue lesions, reporting a diagnostic accuracy of 74% overall and of 80% in their 5 cases of Ewing sarcoma of bone [7]. In their review of CT-guided needle biopsy of musculoskeletal neoplasms, Dupuy and colleagues reported an overall diagnostic accuracy of 93% in 176 biopsies [8]. The diagnostic accuracy fell to 75% for round cell neoplasms which comprised 32 cases, this including both Ewing sarcoma of bone and extra-skeletal Ewing sarcoma. Most recently, McCarville et al evaluated 31 patients with Ewing sarcoma and 32 patients with osteomyelitis, reporting a diagnostic accuracy of only 50% in the 6 patients with Ewing sarcoma who underwent IGCNB [11]. From the above literature review, it appears that the diagnostic accuracy of both IGCNB and open biopsy may be lower for Ewing sarcoma compared with other primary tumours. This seems to be the case particularly for surgical series that presumably utilise bone biopsy under fluoroscopic guidance which could only target the intra-medullary component of the tumour, rather than the extra-osseous component. We postulate that the lower positive biopsy rate in such cases is likely due to the presence of spontaneous necrosis of the intra-medullary tumour component, as has been described with osteosarcoma [17].
Our high positive diagnostic rate is considered to be the result of many factors including expertise, biopsy planning in the MDT setting, and the frequent use of GA for needle biopsies of bone, which enables a greater number of cores using larger gauge needles. A further factor which is likely to increase diagnostic yield significantly is the sampling of extra-osseous soft tissue components of the tumour. A diagnostic accuracy of 98.4% for primary malignant appendicular bone tumours has previously been reported by Saifuddin et al who used US guidance to target only the extra-osseous component of the tumour [18].
The safety of IGCNB and far lower rates of complications compared with open procedures has been established [3]. We observed complications in one case of a 17-year-old female, who following a CT-guided biopsy under GA developed urinary retention requiring an indwelling catheter, and had a prolonged hospital stay including an intensive care unit admission for pain management. It is unlikely that this represented a complication of the biopsy itself since the needle was placed well away from the bladder, but more likely was related to post-procedure pain. Also, since each biopsy was planned in the MDT meeting and the biopsy site agreed with the orthopaedic oncologist and marked at the time of the procedure with a skin tattoo allowing identification at the time of surgery, there were no cases in which the biopsy was incorrectly placed and therefore impacted upon the planned surgery.
In conclusion, our results indicate that IGCNB can be performed safely and with a very high positive diagnostic rate to establish a diagnosis of Ewing sarcoma of bone. IGCNB should be the first-line method for establishing a definitive diagnosis in Ewing sarcoma and should be performed at a specialist sarcoma referral centre.
Abbreviations
- ABC:
-
Aneurysmal bone cyst
- FNAC:
-
Fine needle aspiration cytology
- GA:
-
General anaesthesia
- IGCNB:
-
Image-guided core needle biopsy
- LA:
-
Local anaesthesia
- MDT:
-
Multidisciplinary team
References
Traina F, Errani C, Toscano A et al (2015) Current concepts in the biopsy of musculoskeletal tumors: AAOS exhibit selection. J Bone Joint Surg Am 97(2):e7. https://doi.org/10.2106/JBJS.N.00661
Exner GU, Kurrer MO, Mamisch-Saupe N, Cannon SR (2017) The tactics and technique of musculoskeletal biopsy. EFORT Open Rev 2(2):51–57
Kiatisevi P, Thanakit V, Sukunthanak B, Boonthatip M, Bumrungchart S, Witoonchart K (2013) Computed tomography-guided core needle biopsy versus incisional biopsy in diagnosing musculoskeletal lesions. J Orthop Surg (Hong Kong) 21(2):204–208
Kubo T, Furuta T, Johan MP, Sakuda T, Ochi M, Adachi N (2018) A meta-analysis supports core needle biopsy by radiologists for better histological diagnosis in soft tissue and bone sarcomas. Medicine (Baltimore) 97(29):e11567. https://doi.org/10.1097/MD.0000000000011567
Rajeswaran G, Malik Q, Saifuddin A (2013) The role of needle biopsy for focal bone lesions with complete fluid-fluid levels on magnetic resonance imaging. Skeletal Radiol 42(6):765–769
Roitman PD, Farfalli GL, Ayerza MA, Múscolo DL, Milano FE, Aponte-Tinao LA (2017) Is needle biopsy clinically useful in preoperative grading of central chondrosarcoma of the pelvis and long bones? Clin Orthop Relat Res 475(3):808–814
Didolkar MM, Anderson ME, Hochman MG et al (2013) Image guided core needle biopsy of musculoskeletal lesions: are non-diagnostic results clinically useful? Clin Orthop Relat Res 471:3601–3609
Dupuy DE, Rosenberg AE, Punyaratabandhu T, Tan MH, Mankin HJ (1998) Accuracy of CT-guided needle biopsy of musculoskeletal neoplasms. AJR Am J Roentgenol 171:759–762
Interiano RB, Malkan AD, Loh AHP et al (2016) Initial diagnostic management of pediatric bone tumors. J Pediatr Surg 51:981–985
Jelinek JS, Murphey MD, Welker JA et al (2002) Diagnosis of primary bone tumors with image-guided percutaneous biopsy: experience with 110 tumors. Radiology 223:731–737
McCarville MB, Chen JY, Coleman JL et al (2015) Distinguishing osteomyelitis from Ewing sarcoma on radiography and MRI. AJR Am J Roentgenol 205:640–650
Gerrand C, Athanasou N, Brennan B et al (2016) UK guidelines for the management of bone sarcomas. Clin Sarcoma Res 6:7
Khoo MMY, Saifuddin A (2013) The role of MRI in image-guided needle biopsy of focal bone and soft tissue neoplasms. Skeletal Radiol 42:905–915
Jalgaonkar A, Dawson-Bowling SJ, Mohan AT et al (2013) Identification of the biopsy track in musculoskeletal tumour surgery: a novel technique using India ink. Bone Joint J 95-B:250–253
Mankin HJ, Mankin CJ, Simon MA (1996) The hazards of the biopsy, revisited. Members of the Musculoskeletal Tumor Society. J Bone Joint Surg Am 78:656–663
Wu JS, Goldsmith JD, Horwich PJ, Shetty SK, Hochman MG (2008) Bone and soft-tissue lesions: what factors affect diagnostic yield of image-guided core-needle biopsy? Radiology 248:962–970
Song WS, Jeon DG, Cho WH et al (2015) Spontaneous necrosis and additional tumour necrosis induced by preoperative chemotherapy for osteosarcoma: a case-control study. J Orthop Sci 20:174–179
Saifuddin A, Mitchell R, Burnett SJ, Sandison A, Pringle JA (2000) Ultrasound-guided needle biopsy of primary bone tumours. J Bone Joint Surg Br 82:50–54
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Asif Saifuddin.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Diagnostic or prognostic study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kalus, S., Vidoni, A., Oliveira, I. et al. Image-guided core needle biopsy for Ewing sarcoma of bone: a 10-year single-institution review. Eur Radiol 30, 5308–5314 (2020). https://doi.org/10.1007/s00330-020-06926-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06926-2