Abstract
Objective
To assess the value of image-guided needle biopsy of bone lesions completely filled with fluid–fluid levels (FFLs) on magnetic resonance imaging (MRI) and the safety of primary surgical curettage.
Materials and methods
The radiology database was searched for all reports containing “fluid level” from 1998 to 2011 and the imaging was reviewed retrospectively. Inclusion criteria were patients with bone lesions completely filled with FFLs on MRI (defined as FFLs on every axial and/or sagittal T2-weighted or Short Tau Inversion Recovery (STIR) sequence). The pathology database was then reviewed for the outcome of needle biopsy (n = 14) and for the outcome of surgical curettage, either post-biopsy or primary (n = 52).
Results
There were 53 patients (mean age 18 years; M = 34, F = 19). Fourteen patients underwent percutaneous needle biopsy, which was diagnostic in five (36 %) and non-diagnostic in nine (64 %). Fifty-two patients had surgical curettage/resection, which was diagnostic in 50 (96 %) and non-diagnostic in two (4 %). All lesions were benign; 78 % were aneurysmal bone cysts (ABC), 8 % were lesions with ABC change, and 14 % were simple bone cysts.
Conclusions
Our results suggest that patients with bone lesions completely filled with FFLs on MRI are almost certain to be benign, provided that the clinical and radiological features are not atypical. Percutaneous needle biopsy in such cases is unlikely to be of value and these lesions can be safely managed with primary surgical curettage.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The first report of a fluid–fluid level (FFL) in a bone lesion was demonstrated in an aneurysmal bone cyst (ABC) using magnetic resonance imaging (MRI) [1]. Since then, FFLs have been reported in a variety of benign and malignant bone lesions, including simple bone cyst, giant cell tumor (GCT), chondroblastoma (CB), intraosseous ganglion, brown tumor, osteoblastoma, osteomyelitis, telangiectatic osteosarcoma, and plasmacytoma [2–9].
Given the wide associated differential diagnosis, the presence or absence of FFLs within a bone tumor alone cannot be used as a diagnostic criterion to differentiate between benign and malignant lesions. This presents difficulty in the multidisciplinary team (MDT) setting when deciding which lesions require biopsy and/or excision and which can be managed conservatively.
In a review of 83 patients with FFLs, O’Donnell et al. found that the proportion of FFLs within a bone lesion was inversely related to the likelihood of malignancy [10]. However, the only group in which there was no malignancy whatsoever, was the group with complete FFLs although the number of these lesions was too small (n = 11) to draw significant conclusions.
In the early management of such patients, percutaneous needle biopsy was being performed for all of the cases. Following the report by O’Donnell et al. and the finding of a poor diagnostic yield from needle biopsy, we changed our management to primary surgical curettage for all cases where the lesion was completely filled with FFLs on T2-weighted (T2W) MRI, and the clinical and radiological features were felt to be consistent with an ABC. The purpose of the current study was to audit this practice, thereby identifying the outcome of diagnostic percutaneous needle biopsy in patients with focal bone lesions that were completely filled with FFLs, and also to determine the safety of managing such lesions without needle biopsy prior to definitive surgical management.
Materials and methods
The patients were initially identified from a prospective database of new referrals to the Bone Sarcoma Service between 1998 and 2008. The MRI studies were all assessed by a senior radiologist with 18 years of experience of bone tumor imaging, who was blinded to the clinical details and histopathology reports. The presence and degree of FFL change within the lesion based on a combination of sagittal and axial T2W or STIR sequences was recorded and all patients in whom MRI showed the lesion to be completely filled with FFLs were selected. Between 2008 and 2011, The Bone Sarcoma Service database was no longer in use and to identify cases during this period, the Radiology Management System was searched for reports containing the term “fluid level”, “fluid-level”, “fluid fluid level” and “fluid-fluid level” and the reports of all such cases were reviewed. For all new patients not identified between 1998 and 2008, the MR studies were reviewed and all cases that showed complete FFL change were selected, thus increasing the total number of cases for the study.
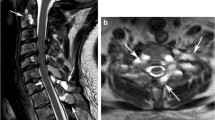
The inclusion criteria for the study were: 1) patients with bone lesions containing complete FFLs on MRI, defined as the presence of FFLs on every axial or sagittal T2W or STIR sequence through the lesion (Fig. 1), and 2) patients who had undergone either needle biopsy prior to definitive surgical management or had undergone primary surgical curettage. Therefore, no patients who were treated conservatively, and therefore for whom no histological diagnosis was present, were included.
Histologically-proven aneurysmal bone cyst of the proximal right tibia in a 15-year-old female to demonstrate a typical lesion with a complete fluid–fluid level (FFL) on magnetic resonance imaging (MRI). a anterior-posterior (AP) radiograph of the right knee demonstrating a well-defined lucent lesion in the proximal right tibia with a well-defined sclerotic margin and a narrow zone of transition (white arrow). b Axial and c sagittal proton density MR images through the tibial lesion seen in a demonstrating a well-defined low signal margin to the lesion that has septated internal fluid contents, which demonstrate horizontal interfaces between the dependent lower signal fluid and the non-dependent higher signal fluid in keeping with multiple FFLs (white arrows). The FFLs completely fill the lesion, with no soft tissue element demonstrated on any of the images through the lesion
The study group included 53 patients with a mean age of 18 years (range 3–55 years). There were 34 males and 19 females. All biopsies were performed with an 11-gauge Jamshidi needle under computed tomography guidance, using an aspiration biopsy technique, which usually yielded between 10 and 20 ml of clot from the lesion. Age, sex, imaging findings, MDT meeting reports, histopathological reports, and final diagnosis were recorded prospectively and reviewed retrospectively. The final diagnosis was made based on the histopathological report alone from percutaneous needle biopsy or surgical curettage/resection or, where the histopathological report was non-diagnostic, at MDT review using a combination of the histopathological report and the imaging, clinical, and follow-up findings.
As the study was classed as a retrospective audit by our Research and Development Committee, no formal ethics submission or informed consent was required.
Results
Of the 53 patients, 14 underwent percutaneous needle biopsy. The biopsy was reported by the histopathologist to be diagnostic in five patients (36 %). In the other nine patients (64 %), the biopsy specimen was reported as non-diagnostic, either showing blood only, blood with osteoclast-rich cells, or with an insufficient specimen for diagnosis. Thirteen of these patients went on to have surgical resection/curettage. The other patient was reviewed in the MDT Meeting and the imaging thought to be consistent with a non-ossifying fibroma with ABC change. The patient is being managed conservatively with clinical and imaging follow-up, and there has been no change for 16 months.
Fifty-two patients had surgical curettage/resection, of which 39 patients went straight to surgery without having a percutaneous needle biopsy. Of the 52 patients, the biopsy specimen was reported as diagnostic in 50 (96 %), with two patients (4 %) reported as having insufficient tissue in the provided specimen to make a diagnosis, but showing no evidence of malignancy. The first of these two cases was a metaphyseal lesion in the distal fibula with histology from curettage revealing an aneurysmal bone cyst with some atypical features (perilesional new bone formation as well as some mitoses), but no overt evidence of malignancy—the case has been followed-up closely and there has been no change clinically or radiologically for more than 4 years. The second case was curettage from the talus, which showed necrotic tissue only with no evidence of malignancy; on radiological and clinical follow-up there has been no change for more than 7 years.
The results of the biopsies and surgically treated cases are provided in Fig. 2, Tables 1, and 2.
Discussion
Both liquids and gases are fluids, so, strictly speaking, a FFL is a horizontal interface between two liquid layers, two gas layers, or a gas layer and a liquid layer. However, in the context of the medical literature, the term FFL is used almost exclusively to describe the horizontal interface (level) between a sedimentation layer (composed of cells/cellular debris) suspended in a liquid layer. The physical properties of the sedimentation layer (its ability to fill a container/space, to form a horizontal boundary at right angles to the direction of gravity, and to flow) make it almost impossible to differentiate from fluid using imaging or histopathological assessment. As such, the term FFL is used somewhat inaccurately.
FFLs usually occur within a cystic or compartmentalized structure due to hemorrhage (and associated breakdown of blood products), tumor necrosis (with sedimentation of tumor cells and tissue fluid) or separation of blood and serum in blood-filled cavities [11–15].
To detect FFLs using cross-sectional imaging, the images must be obtained perpendicular to the plane of the FFL and on MRI, FFLs are only seen on axial or sagittal sequences.
FFLs were first described in an ABC and in a bone lesion with FFLs, ABC, or secondary ABC change within a primary bone tumor (such as GCT, CB, and osteoblastoma) remains the most likely diagnosis. However, FFLs have subsequently been described in a variety of benign and malignant bone tumors, leading to it being considered a non-specific, rather than diagnostic, sign [14]. This means that in many bone lesions with FFLs, it is difficult to differentiate benign from malignant causes and, as such, many benign lesions may undergo unnecessary biopsy or excision.
In 2004, O’Donnell et al. found that the extent of FFL change within a bony lesion was inversely related to the degree of malignancy, with lesions that showed more than 2/3 FFLs being benign in 81 % of cases (13/16) and lesions with complete FFLs being benign in 100 % of cases (11/11). Given the relatively small sample size of lesions with complete FFLs their findings were not significant enough to effect a change in the management of these cases, with the decision to biopsy or excise still currently based on a combination of clinical and radiological findings.
To our knowledge there are no reported cases in the literature of malignant lesions with complete FFLs, and our study of 53 patients is the largest review of bone lesions with complete FFLs.
Pre-operative needle biopsy is usually performed for bone lesions that are to undergo surgical resection. However, our results suggest that percutaneous needle biopsy of lesions with complete FFL on MRI is unhelpful, with only 36 % of such biopsies yielding a definitive diagnosis in our patient cohort. The main reason for this is likely to be the difficulty of obtaining sufficient diagnostic cellular material from a lesion that is predominantly hemorrhagic.
In our patient cohort, all lesions with complete FFLs on MRI were shown to be benign (53/53) with 78 % diagnosed as ABC, 8 % diagnosed as lesions with ABC change (CB or GCT), and 14 % diagnosed as simple bone cysts. The results also suggest that primary surgical curettage of such cases is a safe management option.
A minor limitation of our study is that only one radiologist assessed all of the MR images.
Conclusions
We conclude that bone lesions completely filled with FFLs are almost certain to be benign, provided that the clinical and radiological features are not atypical. Percutaneous needle biopsy in such cases is unlikely to be of value and these lesions can be managed safely with primary surgical curettage.
References
Hudson TM, Hamlin DJ, Fitzsimmons JR. Magnetic resonance imaging of fluid levels in an aneurysmal bone cyst and in anticoagulated human blood. Skeletal Radiol. 1985;13(4):267–70.
Maas EJ, Craig JG, Swisher PK, Amin MB, Marcus N. Fluid-fluid levels in a simple bone cyst on magnetic resonance imaging. Australas Radiol. 1998;42(3):267–70.
Buetow PC, Newman S, Kransdorf MJ. Giant-cell tumor of the tibia in a child presenting as an expansile metaphyseal lesion with fluid-fluid levels on MR. Magn Reson Imaging. 1990;8(3):341–4.
Kudo T, Okada K, Hirano Y, Sageshima M. Chondroblastoma of a metacarpal bone mimicking an aneurysmal bone cyst: a case report and a review of the literature. Tohoku J Exp Med. 2001;194(4):251–7.
Grey AC, Mangham DC, Davies AM, Grimer RJ. Fluid-fluid level in an intraosseous ganglion. Skeletal Radiol. 1997;26(11):667–70.
Davies AM, Evans N, Mangham DC, Grimer RJ. MR imaging of brown tumour with fluid-fluid levels: a report of three cases. Eur Radiol. 2001;11(8):1445–9.
Vilanova JC, Dolz JL, de Leon JL M, Aparicio A, Aldoma J, Capdevila A. MR imaging of a malignant schwannoma and an osteoblastoma with fluid-fluid levels. Report of two new cases. Eur Radiol. 1998;8(8):1359–62.
Rafii M, Firooznia H, Golimbu C, McCauley DI. Hematogenous osteomyelitis with fat-fluid level shown by CT. Radiology. 1984;153(2):493–4.
Harter SB, Nokes SR. Plasmacytoma of the sacrum: fluid-fluid levels on MR images. AJR Am J Roentgenol. 1995;165(3):741–2.
O’Donnell P, Saifuddin A. The prevalence and diagnostic significance of fluid-fluid levels in focal lesions of bone. Skeletal Radiol. 2004;33(6):330–6.
Alyas F, Lee J, Ahmed M, Connell D, Saifuddin A. Prevalence and diagnostic significance of fluid-fluid levels in soft-tissue neoplasms. Clin Radiol. 2007;62(8):769–74.
Tsai JC, Dalinka MK, Fallon MD, Zlatkin MB, Kressel HY. Fluid-fluid level: a nonspecific finding in tumors of bone and soft tissue. Radiology. 1990;175(3):779–82.
Sone M, Ehara S, Sasaki M, Nakasato T, Tamakawa Y, Shiraishi H, et al. Fluid-fluid levels in bone and soft tissue tumors demonstrated by MR imaging. Nihon Igaku Hoshasen Gakkai Zasshi. 1992;52(8):1110–5 [in Japanese].
Van Dyck P, Vanhoenacker FM, Vogel J, Venstermans C, Kroon HM, Gielen J, et al. Prevalence, extension and characteristics of fluid-fluid levels in bone and soft tissue tumors. Eur Radiol. 2006;16(12):2644–51.
Davies AM, Cassar-Pullicino VN, Grimer RJ. The incidence and significance of fluid-fluid levels on computed tomography of osseous lesions. Br J Radiol. 1992;65(771):193–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rajeswaran, G., Malik, Q. & Saifuddin, A. The role of needle biopsy for focal bone lesions with complete fluid-fluid levels on magnetic resonance imaging. Skeletal Radiol 42, 765–769 (2013). https://doi.org/10.1007/s00256-012-1542-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-012-1542-y