Abstract
The management of bone and soft tissue neoplasms is dependent upon accurate histopathological diagnosis. There are a wide range of surgical, oncological and combined treatment regimes, including limb salvage techniques for appendicular lesions. Accurate histopathological diagnosis relies upon sufficient samples of viable, representative tissue being biopsied from a lesion with minimal harm to the patient. The complex nature of bone and soft tissue lesions and the wide variety of treatment options means that the procedure should be planned in a multidisciplinary team (MDT) setting and performed where the definitive surgery will take place.
In the past, open biopsy had been considered the gold standard. However, the diagnostic accuracy of core needle biopsy (CNB) is greater than 90 % for both bone and soft tissue neoplasms and should be considered the first-line procedure. Image guidance can be by ultrasound, fluoroscopy or CT, depending upon the nature and location of the lesion. MDT discussion as to whether a lesion needs biopsy, biopsy approach, what part of the lesion to biopsy, what image guidance to use and the type of analgesia is vital to ensure successful, uncomplicated retrieval of diagnostic material.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Biopsy-open, closed
- Core needle biopsy-CT-guided, CT-fluoroscopy-guided, CT-ultrasound-guided
- Sarcoma
- Soft tissue tumours
- Techniques
Introduction
The appropriate management of bone and soft tissue neoplasms is dependent not only on the diagnosis of whether the lesion is benign or malignant, but also on tumour grade and increasingly, immunohistochemical and genetic features. Virtually all sarcomas that will undergo surgical or oncological treatment will require pre-surgical histological diagnosis. Furthermore, successful operative treatment and disease control is dependent on a carefully performed and uncomplicated biopsy and this must occur at a treatment centre rather than a referring institution. A biopsy performed at a centre where there are experienced radiologists, pathologists, oncologic orthopaedic surgeons and oncologists will have greater accuracy and lower complication rates [1]. This is particularly important with the increased use of limb salvage surgery (LSS).
A successful biopsy must do no/minimal harm to the patient and ensure sufficient, viable and representative tissue sampling. Harm can occur from biopsying a lesion that doesn’t require biopsy for adequate management, by inappropriate technique or approach, or by damage to neurovascular structures or inadvertently contaminating an uninvolved anatomical compartment or joint. Such mistakes can be minimised by discussing all cases in a multidisciplinary team (MDT) setting.
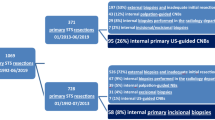
Acquisition of tissue can be via open biopsy or needle biopsy; including fine-needle aspiration (FNA) or core-needle biopsy (CNB). Current evidence supports image guided CNB as the most appropriate initial method; this will be discussed under the initial section on types of biopsy. Indication for biopsy, pre-procedure planning, biopsy technique and complications will be discussed in separate sections.
Types of Biopsy
Open Biopsy
Open biopsy refers to the surgical technique of directly accessing tumour tissue via a skin incision and surgical tract. Open biopsy has long been stated as the gold standard [2], being considered superior in obtaining representative tissue samples by the Musculoskeletal Tumour Society [1] and in a recent meta-analysis [3]. Certainly, larger samples of tumour tissue are retrieved and accuracy is reported of up to 95 % [3]. However, the amount of tissue obtained must be balanced against invasiveness and cost. Open biopsy is usually performed in an inpatient setting and greater complication rates are reported such as tumour seeding [4], joint involvement, neurovascular damage, infection and pain. The need for the biopsy to be performed at a treatment centre by experienced oncological surgeons is continually emphasised in the literature [1]. The incision should be as small as necessary for safe retrieval of tissue.
Needle Biopsy
Although the complications encountered with open biopsy can also occur for percutaneous CNB, the use of radiological (fluoroscopic, ultrasound and CT) guidance increases accuracy of needle placement reducing complication rates and pain. Admission overnight is rarely needed and biopsy can be performed in the out-patient setting or as a day-case when general anaesthesia is required. Needle biopsy produces a smaller biopsy tract that can be marked and resected at the time of definitive surgery. Multiple studies show excellent sensitivity and specificity with minimal complications [5–9].
Fine-Needle Aspiration/Capillary (FNA)/(FNC) Biopsy
Fine needle aspiration (FNA), or its counterpart, fine needle capillary (FNC) biopsy is minimally invasive, cheap and has few reported complications or evidence of tumour spread [10]. The technique involves percutaneous placement of small calibre (20–23 g.) needles into the lesion. Radiological guidance is needed if the lesion is not palpable. Lesional tissue is obtained via aspiration by syringe (FNA) or by using capillary action to obtain cells within the needle and needle hub (FNC). Both techniques have shown similar accuracy [11]. The aspirate is spread onto slides and a cytologist (often present) can analyse the material under microscopy. The advantage of this is that aspirates with acellular or non-diagnostic material can be identified during the procedure and repeat biopsy performed. Studies have shown excellent accuracy in the diagnosis of bone lesions, from 97.1 % to 100 % [12, 13] and therefore, it has been suggested as an effective initial investigation [14].
The main disadvantage is that it offers only cytological features of the lesion. Although it has been shown to be accurate in assessing metastatic bone lesions [15] more recent direct comparison studies show CNB to have higher diagnostic accuracy in all aspects including determining the nature of the tumour, establishing the histological type and grade and achieving a specific diagnosis [16]. This has been confirmed in a meta-analysis of studies [3].
Accurate treatment of sarcoma now depends upon exact diagnosis and upon tumour grade as well as immunohistochemical and cytogenetic features. Given the wide range of bone and soft tissue sarcoma sub-types and the extensive variety of surgical and oncological treatment regimes, lesions positive on FNA will need further evaluation with either open or CNB. Advocates of CNB recognise that a well-planned, successful (uncomplicated acquisition of representative, viable, sufficient tumoral tissue) core biopsy, need only be performed once.
Core-Needle Biopsy (CNB)
Core needle biopsy of bone and soft tissue lesions is less expensive than open biopsy, can be performed in an out-patient setting and is minimally- invasive. Furthermore, in instances where CNB is non-diagnostic, open biopsy is also associated with similar diagnostic difficulties [5].
The technique involves the use of large gauge (11–18 g) cutting needles, usually with radiological guidance. A large array of tissue, site and modality specific needles are available from multiple vendors for both soft tissue and bone tumours. In general core biopsy needles are one of two types: those that use a hollow outer cutting needle with an inner stylet that has a sharpened bevelled tip; the specimen is acquired within the outer hollow needle, and those that have an outer cutting cannula and an inner stylet with a specimen slot and a sharpened bevelled tip; the specimen is acquired within the inner stylet specimen slot.
The choice of core biopsy needle type depends upon the type of lesion. Lesions of cortical or cancellous bone can have cores taken by hollow cutting needles (e.g. Jamshidi; CareFusion, San Diego, California, USA [6]), or Bonopty; AprioMed, Uppsala, Sweden). These needles have a hollow outer core with a solid inner stylet with a sharpened multi-bevelled tip (Fig. 1a). The outer core tip is sharpened and often serrated with teeth that are used to drill through bone and/or tumour. When the stylet is removed the drilling action collects a core sample within the needle. These hollow needles can also be used to aspirate lytic components of tumours (Fig. 1b).
Soft tissue tumours or the extra-osseous components of bone tumours can be biopsied with needles with an inner stylet and a specimen slot (Fig. 2). An outer cutting needle advances over the specimen slot either manually (e.g. Trucut; Baxter Health Care Corp., Deerfield, Il, USA [17]) or using a spring-loaded trigger (e.g. Temno; Bauer, Via del Fosso, Italy [7]). Spring-loaded, one-hand operated units are useful for ultrasound-guided biopsy where one hand is needed to hold the ultrasound probe.
Reported accuracy ranges from 74 % [8] to 93 % [6, 7, 16, 18] with complication rates ranging from 1 % [18] to 2 % [9]. No significant difference in accuracy of diagnosing soft tissue or bone lesions has been demonstrated [18]. A meta-analysis of studies in the paediatric population documented accuracy of 94 % with complications rates of 1 % [19]. Accuracy has been shown to decrease in the biopsy of spinal lesions (61 %) and in cases of infection (50 %) [8].
Diagnostic yield depends upon appropriate planning, operator experience and the intrinsic features of the tumour. In a study of 151 consecutive CNB, factors affecting diagnostic yield included; type of lesion (87 % lytic bone lesions, 57 % sclerotic bone lesions); lesion size (54 % <2 cm, 86 % >5 cm); longer length of specimen and increasing the number of specimens obtained. No difference was identified between soft tissue or bone lesions, by imaging modality used or by needle size. A minimum of three specimens for bone lesions and four for soft tissue lesions was proposed [20].
Despite the advantages and published sensitivity and specificity, concern is still raised regarding the accuracy of needle biopsy. This is often based on findings from older studies with small sample sizes [21]. There has been a recognisable difference in both diagnostic yield and accuracy in assessing heterogeneous soft tissue tumours [22]. Lesions may be spatially heterogeneous in regards to grade and histological features or there may be widespread tumour necrosis. However, the use of MRI for tumour staging can identify areas of viable tissue, necrosis and dedifferentiation, which can be targeted or avoided using radiological guidance. Accuracy is also reduced in the biopsy of bone lesions complicated by pathological fracture where the lesion is primarily intra-osseous or has only a small extra-osseous component. In such cases, primary open biopsy is recommended [23].
The need for specialist radiological opinion in assessing the primary lesion is emphasised as part of a multidisciplinary team (MDT) approach including pathologists, oncologic orthopaedic surgeons and oncologists. The team should discuss each case individually with regards biopsy planning and for pathological diagnosis review. The following questions need to be considered:
-
1.
Does the lesion need biopsy?
-
2.
Has the lesion been imaged and staged appropriately?
-
3.
What is the appropriate approach given the possible treatment options?
-
4.
What type of biopsy will give sufficient, representative and viable tissue?
-
5.
What image guidance is appropriate?
-
6.
What analgesia should be used?
These questions will now be discussed in detail.
Indication for Biopsy
The most important question during biopsy planning is whether the lesion needs to be biopsied. Most primary bone lesions present with focal bone pain and/or swelling and with a focal or multifocal radiological abnormality. However, with increasing radiological investigations asymptomatic incidental findings increase. These may be variations of normal, radiological artefact or non-neoplastic lesions. The latter can also present with focal bone pain and radiological abnormality mimicking neoplasm, and in our experience account for approximately 10 % of all MDT referrals. Non-neoplastic focal lesions of bone may be congenital, traumatic, degenerative, infective or inflammatory in aetiology. Infective lesions are common, both acute [24] and chronic osteomyelitis (including chronic recurrent multifocal osteomyelitis (CRMO) [25]), Brodie’s abscess [26] and TB [27, 28]), which can all mimic neoplasm but often have characteristic radiological appearances. Another common lesion mimicking bone tumour/infection is stress fracture [29]. The pathological differentiation of acute stress fracture from high-grade osteosarcoma can be difficult and diagnosis should depend primarily on the typical radiological characteristics of the former.
Many benign lesions with classical imaging features (such as fibrous cortical defects/small non-ossifying fibromas, chondromas and bone islands) may be asymptomatic and a period of clinical and radiological assessment may be adequate for management, with biopsy only considered in the setting of growth or development of symptoms. Also, the imaging features of osteoid osteoma (OO) are classical enough such that patients may be referred directly for CT-guided radiofrequency ablation (RFA) as a definitive procedure.
CNB may also be avoided in situations where diagnostic yield and accuracy are low and where open biopsy has been shown to be safer and/or more accurate. Examples include lesions less than 2 cm, those in deep or difficult anatomical positions or in cases with associated pathological fracture [23]. Markedly sclerotic lesions may also need primary open biopsy with the use of drills or bone saws.
However, for the majority of tumours that require surgical excision or combined chemotherapy and surgery, a biopsy is necessary for definitive histological diagnosis prior to treatment. Many sarcomas, particularly Ewing sarcoma are well documented for mimicking infection [30, 31]. Furthermore, biopsy of infectious lesions may be necessary for microbiological culture to assess sensitivity to antibiotics, for fungal growth or for PCR diagnosis of TB.
Adequate Pre-Procedure Imaging
Once a lesion has been assessed as requiring CNB, the procedure must be planned in the MDT setting. This includes assessment of tumour stage. Although the referral imaging may be adequate for deciding whether a biopsy needs to be performed, imaging studies may have to be repeated if, for instance, the whole lesion has not been covered or if, in the case of high-grade bone sarcomas, the whole bone has not been imaged to assess for ‘skip’ metastases. Magnetic resonance imaging (MRI) is the technique of choice for local staging of bone and soft tissue neoplasms. In addition MRI will add information on the type of biopsy technique to use to ensure sufficient tissue, the approach, the appropriate part of the lesion to target, the anatomical structures to avoid (e.g. neurovascular bundle) and which imaging technique to use for biopsy guidance.
Staging of bone tumours refers to the clinical and/or radiological evaluation of both the local and distant disease extent. This directly influences surgical and oncological management and determines prognosis. The advent of limb salvage techniques, the variety of endoprosthetic implants and number of possible surgical procedures requires a high degree of accuracy in local staging.
For the purposes of local staging of bone lesions, it is useful to divide disease extent into intramedullary and extramedullary components. Intramedullary extension includes an assessment of longitudinal medullary extent, epiphyseal involvement and skip metastases. These factors will determine the site of bone resection. The presence of skip metastases means that both the primary lesion and the skip lesion must be resected. Therefore, in a case where an additional lesion is present in the bone and it does not have typical appearances of a skip metastasis, the second lesion may also require biopsy (Fig. 3). Extramedullary extension includes an assessment of joint involvement, relationship to the neurovascular bundle and involvement of muscle compartments. These factors will determine the feasibility and type of limb salvage performed.
Distal femoral osteosarcoma. (a) Coronal T1Weighted SE MR image of the distal femur showing extensive intramedullary tumour (arrows) and an extra-osseous extension (arrowhead). (b) Coronal T1Weighted SE MR image of the proximal femur showing a small hypo-intense focus (arrow) which could represent a skip metastasis and may require biopsy for confirmation
Correct Biopsy Approach
The biopsy approach must be discussed with the surgical team who will perform surgical treatment. Relatively recent advances in limb salvage surgery can avoid amputation in the majority of appendicular bone and soft tissue sarcomas, and fore/hind-quarter amputation in shoulder/pelvic girdle disease with its associated operative and psycho-social morbidity. Seeding of sarcoma cells and subsequent needle tract recurrence is reported, but very rare. However, needle tract resection at the time of definitive surgery is strongly advised [32]. Knowledge of surgical approaches is essential since an incorrect approach may preclude limb salvage surgery. The small biopsy scars from CNB are usually visible if surgery is performed within 2–3 months. However, if there is to be a delay between biopsy and surgery, such as for neo-adjuvant chemotherapy, then marking the biopsy site with Indian ink should be considered.
The majority of bone tumours occur around the knee or shoulder. For sarcomas of the proximal humerus requiring endoprosthetic replacement (EPR) a deltopectoral surgical incision is used and the biopsy approach, although sometimes challenging due to the oblique angle, should be from a skin entry point in this region (Fig. 4). However, for proximal humeral tumours that can be adequately treated with intralesional curettage or humeral diaphyseal lesions requiring EPR, a lateral approach is satisfactory. For sarcomas around the knee (distal femur and proximal tibia) requiring EPR, the biopsy approach should be within an anterior 120° arc (Fig. 5) and the posterior compartment should be avoided whenever possible. However, if an anterior approach is not feasible, a posterior biopsy tract can excised separately at the time of definitive surgery. Distal femoral or proximal tibial tumours that can be adequately treated with intralesional curettage can be biopsied from a medial or lateral approach. Femoral diaphyseal sarcomas requiring EPR should be biopsied via a lateral approach (Fig. 6).
Osteosarcoma of the humerus. (a) Sagittal post-contrast T1W SE MR image of the humerus showing extensive intramedullary tumour (arrows) and a posterior extraosseous mass (arrowheads), which would be most easily biopsied via a posterior approach. (b) The humerus will be resected via a deltopectoral approach, requiring CT-guided biopsy via a similar approach at the junction of the pectoralis major medially (arrow) and the deltoid laterally (arrowhead)
Proximal tibial osteosarcoma. (a) Coronal T1W SE MR image showing the intramedullary tumour (arrows) and an extra-osseous tumour mass (arrowhead). (b) Axial PDW FSE MR image showing the extra-osseous component (arrow). (c) CT-guided needle biopsy targeting purely the extra-osseous mass via an anterior approach
Also the biopsy should avoid any uninvolved joint as joint-sparing prostheses have better function and long-term outcomes than those where the joint is replaced. Particular care is needed around the knee as the anterior approach may breach the suprapatellar recess.
Type of Biopsy Technique
In general, biopsy can be divided into three techniques depending upon the nature of the lesion. Solid or sclerotic intra-medullary lesions with minimal or no extra-osseous component require CNB with a hollow cutting needle. We prefer 10 cm. length, 11G Jamshidi needles, for which high diagnostic accuracy has been reported [33].
Lytic lesions of bone or can be biopsied with a similar hollow needle using an aspiration technique (Fig. 1b), since it is difficult to obtain sufficient material using a CNB technique. However, lytic lesions often contain cellular blood clot and diagnostic accuracy and yield have been reported at 73 % and 75 % respectively [34] with high volume (15–20 mls.) aspiration.
For aggressive bone lesions (primary high-grade sarcomas or metastases) with relatively large extra-osseous components and for all soft tissue tumours, a 14G Tru-cut or Temno is our needle of choice. Diagnostic accuracy of 98.4 % has been reported if the extra-osseous component of a primary bone sarcoma is targeted with ultrasound guidance [35].
In addition to gaining sufficient material safely without compromising surgical treatment, the tissue must be representative of the highest-grade component of the lesion. Therefore, surrounding bone and soft tissue reactive changes and tumour necrosis must be avoided, while areas of possible dedifferentiation must be targeted. MRI is the technique of choice in evaluating these tumour characteristics [36].
In regard to appendicular bone sarcomas, there is an excellent correlation between intra-osseous tumour extent on longitudinal non-contrast T1-weighted SE sequences and pathological macroslides [37]. STIR sequences may overestimate tumour extent due to their sensitivity to reactive marrow oedema [38]. Therefore, for planning biopsy of intra-medullary lesions, the T1W SE images should be used.
Areas of fluid signal intensity (SI) on T2W imaging can be indicative of necrosis or haemorrhage, although in the case of myxoid lesions differentiation of fluid and tumour can be difficult. Colour Doppler ultrasound can also confirm vascularity in tumour tissue and show no flow in non-viable tissue. In part, this can explain the superiority of ultrasound-guided CNB over non-image guided biopsy of palpable soft tissue masses (95 % vs. 78 %) [39].
De-differentiation refers to the association of a benign tumour, or more commonly a low-grade sarcoma with a high-grade component. Such tumours assume the management and prognosis of a high-grade sarcoma and may require neo-adjuvant chemotherapy. Therefore, pre-treatment diagnosis is essential. Low-grade sarcomas that commonly de–differentiate are chondrosarcoma (∼11–13 % of cases) [40] and parosteal osteosarcoma (up to 24 % of cases) [41]. MRI can identify differentiation in these lesions. Low-grade chondrosarcoma is characterised by lobular high SI on T2W sequences. Areas of reduced SI are indicative of de-differentiation and these should be the preferred site of biopsy [42] (Fig. 7). Parosteal osteosarcoma is characterised by mature osteoid with corresponding marked low SI on all sequences. Areas of differentiation will be manifest by areas of intermediate SI on both T1W and T2W sequences and increased SI on STIR [43].
De-differentiated chondrosarcoma of the proximal femur. (a) Axial T2W FSE MR image showing an aggressive lesion of the proximal femur. The typical chondral component has high T2W SI (arrows) while the de-differentiated component has intermediate T2W SI (arrowhead). (b) Axial CT study showing biopsy targeting the de-differentiated component
Imaging Technique
The choice of imaging technique (fluoroscopy, USound or CT) will depend upon the type of lesion to be biopsied (soft tissue/extra-osseous component of bone lesion or intra-medullary lesion) and lesion location.
Soft tissue lesions or extra-osseous components of bone lesions in the appendicular skeleton can usually be assessed with US guidance (Fig. 8). The additional use of colour Doppler can identify neovascularity within the tumour and such areas are more likely to be viable and should therefore be targeted. The adjacent neurovascular bundle can also be identified.
Proximal tibial osteosarcoma (same case as in Fig. 5). Coronal longitudinal US study of the proximal tibia showing the extraosseous component of the tumour (arrows)
Deep soft tissue lesions around the pelvic or shoulder girdles or small lesions near neurovascular structures (such as in the popliteal fossa) are more appropriately biopsied under CT guidance. CT is also suggested for bone tumours with primarily intra-cortical (Fig. 9) or intra-medullary location and if there is substantial soft tissue ossification.
Osteofibrous dysplasia of the proximal tibia. (a) Lateral radiograph showing a well-defined, lobular lesion in the anterior tibial cortex (arrow). (b) Axial CT planning study showing the intra-cortical lytic lesion (arrows) and the wire grid over the skin. (c) Axial CT study showing the Jamshidi needle within the tumour
Fluoroscopy can be used for lytic lesions of the appendicular skeleton, particularly around the wrist or in the hand and foot, since patient positioning for such cases using CT may be difficult. In studies comparing the three imaging modalities accuracy has been shown to be very similar [22].
Type of Analgesia
The majority of bone and soft tissue tumours of the appendicular skeleton in adults can be biopsied under local anaesthetic cover with or without conscious sedation. Extensive local anaesthetic infiltration of the periosteum at the biopsy site is necessary to achieve adequate analgesia.
Biopsy of bone or soft tissue lesions in children, and those associated with pathological fracture are unlikely to be tolerated under local anaesthesia. Therefore, it is our practice to perform such cases under general anaesthetic cover with the addition of long- acting local anaesthetic infiltration at the biopsy site for easier post-biopsy pain control. Biopsy of lesions within the posterior capsule of the knee, pelvic lesions and vertebral lesions may also benefit from general anaesthesia.
Biopsy Technique
This section describes the authors experience and protocols within a specialist bone and soft tissue sarcoma service. Different approaches and algorithms exist in the literature [44] and exact protocols should be formulated in the MDT setting dependent on available resources and with consultation between surgeons, pathologists and anaesthetists. Type of technique, approach, target, adjacent anatomical structures to avoid, imaging modality to use and type of analgesia should have been decided and documented before the procedure is started.
General
Before each procedure patient identity, previous images and MDT plan should be checked, particularly location of lesion, approach and anatomical structures to avoid. Surgical scrub and gowning is suggested for all biopsies.
Patient-Informed Consent
The British General Medical Council summarises consent issues in the book “Consent: Patients And Doctors Making Decisions Together” [45]. Specifically, consent must include: “the potential benefits, risks and burdens, and the likelihood of success”. Specifically for tumour biopsy the literature support for CNB can be mentioned. Risks should always include bleeding and infection at the biopsy site although these are rare occurrences. Risk of non-diagnostic sample and need for repeat or for open biopsy is essential to discuss as a second procedure is inherently stressful if unexpected. If using narrow gauge needles the risk of breakage (particularly in sclerotic bone) is higher and the need for an open procedure to resect retained metal should be mentioned.
If the sample is to be used for teaching or research then specific consent must be obtained.
Ultrasound(US)
The lesion should be scanned with the most appropriate probe necessary to adequately image the deep aspect of the lesion and adjacent structures. Assessment of vascular structures and lesion vascularity with colour Doppler is routinely recommended. Very vascular lesions will need substantial pressure on the biopsy tract after each pass to reduce bleeding.
The lesion should be measured and if less than 2 cm. in maximal length, a 1 cm. throw on the needle should be used. Once the middle of the lesion is visualised the skin can be marked showing probe angulation and needle entry point. The most horizontal needle path (parallel to the scan head) is suggested as the needle is better visualised (Fig. 10). When the needle is imaged parallel to the probe head substantial reverberation artefact is seen. The depth of superficial soft tissues should be measured and this used to plan needle length.
Myxoid liposarcoma of the proximal calf. (a) Axial PDW FSE MR image showing a well-defined oval mass (arrow) adjacent to the fibula compressing the common peroneal nerve (arrowhead). (b) Longitudinal US study showing the superficial and deep margins of the lesion (arrows) and the Temno needle within the mass (arrowheads)
Fluoroscopy
This usually applies for lytic lesions of the distal appendicular skeleton. The limb should be positioned so the lesion is appropriately profiled within the middle of the image to avoid parallax error. The needle can be placed on the skin horizontally and the skin entry point marked.
CT
The patient should be positioned comfortably and with the use of appropriate pre-biopsy imaging the skin surface over the lesion marked with a radio-opaque grid. It is easier to have the patient positioned so the needle will head vertically. This reduces the effect of gravity on the handle of the needle, which can cause considerable movement of the needle tip, particularly for superficial lesions. The grid can be a single use adhesive or made from radio-opaque wires. The grid must positioned such that the scan plane is perpendicular to the lines of the grid. Low dose imaging can be used to reduce patient exposure, however thin reconstructions are suggested to adequately image the narrow needle. The axial images obtained are then compared to planning MRI. CT will have less tissue detail than a planning MRI but having the images side by side can ensure corresponding positions. In reference to the MDT plan the approach to the biopsy target is measured using the measurement function on the CT scanner. This helps select needle length. The line will start from the skin surface and be adjacent to one of the radio-opaque markers that now appear as high attenuation dots on the skin surface (Fig. 9b). The table position number is recorded and patient moved to that axial slice. Using the position marking laser a pen is used to mark the skin entry point adjacent to the grid line on the planning scan. The grid can then be removed. The final needle position at the time of biopsy should be imaged.
Skin Preparation
The skin should be thoroughly cleaned with an alcohol or chlorhexidine based solution and allowed to air dry. The skin is then covered using a fenestrated sterile drape through which the biopsy can be performed.
Technique-Specific Biopsy
Bone Core Biopsy: CT-Guided
Once the skin is cleaned and gowning has taken place the appropriate length core biopsy needle should be selected. The authors advocate an 11 g needle for most procedures except in paediatric patients when a 14 g needle can be used. The skin should be infiltrated with local anaesthetic e.g. Lidocaine 1 % (Xylocaine, AstraZeneca, UK). A scalpel should be used to make a 3 mm incision to subcutaneous fat. A long acting local anaesthetic e.g. Bupivicaine 0.5 % (Marcaine, AstraZeneca, UK) should be used to infiltrate fascia and periosteum.
The needle is then advanced using the axial planning image as a guide to angle. It is paramount to keep the needle course within the axial scan plane (not heading superiorly or inferiorly). When the needle is firmly within tissue, the position can be scanned to check that the needle is properly aligned. An axial scan should show the whole needle in the plane of the scan not moving out of the image (Figs. 4b, 5c, and 9c). The needle tip must be imaged. With bone lesions the needle should be advanced to the superficial edge of the lesion with the stylet in. With sclerotic bone a hammer may be necessary to penetrate the bone. When the stylet is removed the outer hollow needle can moved through the lesion using a rotational motion as the needle is advanced. If necessary, a steristrip can be wound around the needle at the depth from the skin to the lesion. A scan is then necessary to show the needle at the deep aspect of the mass confirming that appropriate lesional tissue has been accessed. Usually three passes are suggested to gain good cores although this should be balanced against difficulty of access. Care needs to be taken on removal as the needle can be firmly embedded in sclerotic bone, often relatively vigorous side-to-side movement can free the needle. Cores should be placed in a specimen bottle and sent to the Pathology Department. Preservation fluid is usually not necessary if the specimen is to be prepared immediately. If there are concerns regarding infection, one core can be sent for microbiology; microscopy, culture and sensitivities.
Lytic Bone Lesion Aspiration: CT/Fluoroscopy-Guided
Planning CT imaging of the lesion is the same as above, as is local anaesthetic infiltration. With fluoroscopy the needle should be parallel to the x-ray beam so the needle appears as a round dot on the image when the needle is exactly vertical. The limb or X-ray tube will need to be rotated 90° to check needle position in two planes (Fig. 11). With lytic lesions the Jamshidi stylet should be removed once the needle is within the lesion. The lesion should be aspirated with a 20 ml syringe. If the lesion is fluid but cellular (e.g. giant-cell tumour) the needle tip can be moved within the lesion to enable aspiration. 10–15 mls should be obtained. Again images with the needle tip at the distal border of the lesion should be obtained.
Soft Tissue Lesion Core Biopsy: CT/US-Guided
Soft tissue lesions are often best accessed using ultrasound guidance. This is often faster and can be more accurate as real time needle placement within the lesion can occur. A spring-loaded needle with a specimen slot is suggested. The patient should be warned regarding the noise of the spring-loaded unit. The needle unit is inserted through the skin with the inner specimen slot within the hollow cutting needle. When the needle is within the lesion, the specimen needle can be extended into the lesion under direct vision; the specimen slot can be seen when using high frequency linear probes. Care should be made to make sure the needle tip is always visualised to prevent inadvertent extra – lesional biopsy or neuro-vascular damage (Fig. 10b).
Spinal Biopsy
Spinal biopsy is considered as a separate section due to its anatomical complexity and potentially serious, although uncommon complications. Reported diagnostic accuracy varies markedly in the literature from 61 % [8] to 88.9 % [33] and 93.3 % [46].
In general, pre-procedure planning and biopsy technique should be the same as for any other osseous lesion. Again review of imaging, particularly MRI, is essential. Many degenerative lesions can appear as focal lesions but have typical benign appearances. The commonest non-neoplastic or benign neoplastic lesions of the vertebral body that can be adequately diagnosed with imaging alone include haemangioma, Schmorl’s nodes and benign osteoporotic collapse, while the majority of tumours of the neural arch are benign (osteoid osteoma, osteoblastoma) and can also be diagnosed with a combination of MRI, CT and scintigraphy, such that biopsy is not required.
However, patients presenting with pathological vertebral collapse usually require a diagnostic needle biopsy for management, unless there is clinical and imaging evidence of spinal cord compression, in which situation material can be obtained at the time of surgical decompression. The commonest diagnoses for single level pathological collapse are metastasis, plasmacytoma/myeloma and B-cell lymphoma, which can all appear identical on MRI. In cases of infection, biopsy +/− drainage is performed in order to differentiate bacterial from granulomatous (TB) infection, for antimicrobial sensitivities, and if necessary to decompress the spinal canal.
Spinal biopsy can be performed using open biopsy, FNA and core biopsy techniques [47]. Technique is the same as discussed previously. In our institution core needle biopsy is favoured over FNA due to its greater diagnostic yield. Furthermore, percutaneous biopsy can often reach deep lesions where open biopsy would cause marked morbidity.
Once the decision is made to biopsy a suspicious lesion it should be staged in terms of its anatomical location. As for appendicular biopsy, the site and type of lesion will guide the biopsy technique. The same technique can be used in the spine as elsewhere in the body depending upon whether the lesion is lytic, sclerotic or has an associated soft tissue component. Diagnostic accuracy varies amongst lesions; in a study of 410 consecutive CT-guided biopsies, diagnostic accuracy was 93 % for lytic lesions compared to 76 % for sclerotic lesions. Also, sclerotic lesions had a false negative rate of 24 % [48].
Biopsy approach will depend upon the location of the lesion in the spinal column (cervical, thoracic or lumbar) and within the individual vertebra. Cervical and high thoracic lesions can be difficult to biopsy, and therefore MR imaging of the whole spine is initially recommended to identify a further lesion in the lower thoracic or lumbar region (Fig. 12). In the cervical spine, lesions of the vertebral body are accessed via an anterolateral approach medial to the carotid vessels and lateral to the airway, while tumours located in the neural arch can be accessed via a lateral or posterior approach. The dens can be biopsied via a trans-oral approach. Lesions of the thoracic vertebral body can be accessed via posterolateral, trans-pedicular or costovertebral approaches (Fig. 13), while a posterior approach is adequate for neural arch tumours. Similarly, posterolateral or trans-pedicular approach is used for lumbar vertebral lesions (Fig. 14) while neural arch lesions are biopsied from a direct posterior approach. Aggressive tumours commonly have a prominent extraosseous mass and in our experience, biopsy of this alone gives a high diagnostic yield (Fig. 15).
Recurrent B-Cell lymphoma of the spine. (a) Sagittal T1W SE MR image of the cervical spine showing diffuse infiltration of the C5 and C6 vertebral bodies (arrows). (b) Sagittal T1W SE MR image of the thoraco-lumbar spine showing diffuse infiltration of the L3 vertebral body (arrow) and fatty infiltration of a previously involved T11 vertebra (arrowhead) which is now healed
Suspected breast carcinoma metastasis. (a) Axial T1W SE MR image of the thoracic spine showing a focal area of reduced marrow SI in the posterior right side of the vertebral body (arrows). (b) Axial CT study showing a Jamshidi needle placed in the lesion via a posterolateral costo-vertebral approach
Recurrent B-Cell lymphoma of the spine (same case as Fig. 12). (a) Axial T1W SE MR image of the L3 vertebra showing a focal area of reduced marrow SI in the centre of the vertebral body (arrows). (b) Axial CT study showing a Jamshidi needle placed in the lesion via a posterolateral trans-pedicular approach
Most vertebral body lesions can be approached via one pedicle with anatomical studies showing that a single trans-pedicular approach can access greater than 50 % of vertebral body content [49] (Fig. 14b). Trans-pedicular approaches must be carefully performed to avoid the spinal canal and nerve roots within the neural foramina.
As with other lesions the biopsy target must be from the most viable, highest grade part of the tumour and MRI is necessary to assess this. Care should be taken to avoid biopsy of reactive bone and soft tissue oedematous changes which may mimic tumour extension.
Spinal biopsy is challenging due to the anatomical location. Care must be taken to avoid the neural foramina, the spinal cord and dural sac, the aorta and in the neck the vertebral arteries, while pneumothorax is a potential complication of thoracic vertebral biopsy. There is potential for catastrophic morbidity and again the decision of whether to biopsy, the technique, approach and target should have been decided in an MDT setting before the procedure
Image guidance can be by CT and fluoroscopy. The choice between the two will depend upon the nature and the size of the lesion, operator experience and modality availability. In the literature, fluoroscopic accuracy has been reported as 88.7 % in large series [50] and can be performed via the posterolateral and trans-pedicular approaches. Fluoroscopic guided trans-pedicular approach in both the thoracic and lumbar spine has been reported with accuracy as high as 89 % with no complication recorded [51]. However, due to the risk of neurological complications, CT guidance is continually emphasised in the literature as the method of choice [46].
Analgesia can be via local anaesthesia +/− conscious sedation depending upon patient and lesional factors. More superficial lesions are easy to infiltrate with local anaesthetic. Deeper vertebral body lesions may require general anaesthesia.
Complications depend upon the level and position of the lesion. Haematoma has been reported at all levels. In the thoracic spine, pneumothorax has been reported. Aortic puncture, psoas puncture and haematoma, incorrect biopsy level and abandoning of the procedure due to pain have also been reported [52]. In a recent large series of 430 biopsies at all levels in a specialist centre only nine complications were reported (five transient pareses, four haematomas) all of which spontaneously resolved [46].
Complications
Complications are rare and poorly documented in the literature. The most common is a non-diagnostic sample. Complications can be both acute and delayed and are generally reported in up to 2 % of cases [9].
Acute
Bleeding
Some lesions are very vascular and can bleed profusely. Focal pressure is often enough to stop bleeding. If there is concern regarding ooze into a large potential space (e.g. the knee joint) then a pressure bandage can be applied. However, vascular injury is rare.
Nerve Damage
Nerves can be damaged by the cutting needle and should be avoided. However, the size of the needle often means that mobile structures are pushed out of the way rather than pierced. Pre-procedure planning can ensure awareness and avoidance of large nerves. Large nerves in the limbs can be visualised on ultrasound and CT due the surrounding fat and/or associated vessels.
Joint Contamination
If this occurs it must be recorded and discussed at the MDT as this can reduce limb salvage options. The supra-patellar pouch of the knee joint is often at risk.
Retained Metal
Smaller biopsy needles can break. Procedures should be performed at a centre where orthopaedic surgeons can resect the retained foreign body.
Fracture
Lytic lesions can fracture due to inappropriate leverage on the biopsy needle; again orthopaedic referral is necessary.
Delayed
Infection
Infection is rare with aseptic technique and surgical grade scrubbing/gowning. The patient should be advised to seek medical review if there is erythema, swelling or discharge at the biopsy site.
Non-Diagnosis
The cause for this should be established, this may be due to technical error, patient pain or nature of the lesion. Repeat biopsy, often requiring general anaesthetic or open biopsy may be necessary.
Tumour Seeding
This is a very rarely reported risk in bone or soft tissue tumours and although individual case studies have been reported [53, 54] the true incidence is unknown [1]. In a variety of malignant tumours the incidence of needle tract seeding has been estimated at 0.003 % and 0.009 % [54]. Given the real, albeit low risk, consideration of biopsy tract marking and resection is suggested. The actual approach should be recorded in the procedural notes and, if possible, a cross–sectional image recorded.
Summary
Biopsy of bone and soft tissue neoplasms is an essential component of the management of these conditions. The widespread use of MRI to stage the lesions means that the highest-grade component of the lesion can be targeted. This has enabled the accuracy of core needle biopsy to be greater than 90 % in both bone and soft tissue tumours. MDT planning is essential to ensure that the biopsy is first necessary and successful, the latter depending upon obtaining sufficient, and representative viable tissue without significant harm to the patient. Proper planning establishes the approach so that potential limb salvage or curative resection is not compromised by tumour seeding. The clinical details, staging MRI and biopsy planning should be performed by experienced musculo-skeletal radiology, oncological Orthopaedic and pathology sarcoma specialists at the centre where the definitive treatment is to be performed.
References
Mankin HJ, Mankin CJ, Simon MA. The hazards of the biopsy, revisited. Members of the Musculoskeletal Tumor Society. J Bone Joint Surg Am. 1996;78(5):656–63.
Huvos AG. The importance of the open surgical biopsy in the diagnosis and treatment of bone and soft-tissue tumors. Hematol Oncol Clin North Am. 1995;9(3):541–4.
Rougraff BT, Aboulafia A, Biermann JS, Healey J. Biopsy of soft tissue masses: evidence-based medicine for the musculoskeletal tumor society. Clin Orthop Relat Res. 2009;467(11):2783–91.
Ferguson PC, Sommerville S, Grimer RJ. Possible metastasis of osteosarcoma to a remote biopsy site: a case report. Clin Orthop Relat Res. 2004;424:216–20.
Jelinek JS, Murphey MD, Welker JA, Henshaw RM, Kransdorf MJ, Shmookler BM, et al. Diagnosis of primary bone tumors with image-guided percutaneous biopsy: experience with 110 tumors. Radiology. 2002;223(3):731–7.
van der Bijl AE, Taminiau AH, Hermans J, Beerman H, Hogendoorn PC. Accuracy of the Jamshidi trocar biopsy in the diagnosis of bone tumors. Clin Orthop Relat Res. 1997;334:233–43.
Quinn SF, Demlow T, Dunkley B. Temno biopsy needle: evaluation of efficacy and safety in 165 biopsy procedures. AJR Am J Roentgenol. 1992;158(3):641–3.
Hau A, Kim I, Kattapuram S, Hornicek FJ, Rosenberg AE, Gebhardt MC, et al. Accuracy of CT-guided biopsies in 359 patients with musculoskeletal lesions. Skeletal Radiol. 2002;31(6):349–53.
Puri A, Shingade VU, Agarwal MG, Anchan C, Juvekar S, Desai S, et al. CT-guided percutaneous core needle biopsy in deep seated musculoskeletal lesions: a prospective study of 128 cases. Skeletal Radiol. 2006;35(3):138–43.
Akerman M. Fine-needle aspiration cytology of soft tissue sarcoma: benefits and limitations. Sarcoma. 1998;2(3–4):155–61.
de Carvalho GA, Paz-Filho G, Cavalcanti TC, Graf H. Adequacy and diagnostic accuracy of aspiration vs. capillary fine needle thyroid biopsies. Endocr Pathol. 2009;20(4):204–8.
Bommer KK, Ramzy I, Mody D. Fine-needle aspiration biopsy in the diagnosis and management of bone lesions: a study of 450 cases. Cancer. 1997;81(3):148–56.
Layfield LJ, Glasgow BJ, Anders KH, Mirra JM. Fine needle aspiration cytology of primary bone lesions. Acta Cytol. 1987;31(2):177–84.
Wedin R, Bauer HC, Skoog L, Soderlund V, Tani E. Cytological diagnosis of skeletal lesions. Fine-needle aspiration biopsy in 110 tumours. J Bone Joint Surg Br. 2000;82(5):673–8.
Treaba D, Assad L, Govil H, Sariya D, Reddy VB, Kluskens L, et al. Diagnostic role of fine-needle aspiration of bone lesions in patients with a previous history of malignancy. Diagn Cytopathol. 2002;26(6):380–3.
Yang YJ, Damron TA. Comparison of needle core biopsy and fine-needle aspiration for diagnostic accuracy in musculoskeletal lesions. Arch Pathol Lab Med. 2004;128(7):759–64.
Westbury G. Surgery in the management of soft tissue sarcoma. Clin Oncol (R Coll Radiol). 1989;1(2):101–5.
Dupuy DE, Rosenberg AE, Punyaratabandhu T, Tan MH, Mankin HJ. Accuracy of CT-guided needle biopsy of musculoskeletal neoplasms. AJR Am J Roentgenol. 1998;171(3):759–62.
Sebire NJ, Roebuck DJ. Pathological diagnosis of paediatric tumours from image-guided needle core biopsies: a systematic review. Pediatr Radiol. 2006;36(5):426–31.
Wu JS, Goldsmith JD, Horwich PJ, Shetty SK, Hochman MG. Bone and soft-tissue lesions: what factors affect diagnostic yield of image-guided core-needle biopsy? Radiology. 2008;248(3):962–70.
Skrzynski MC, Biermann JS, Montag A, Simon MA. Diagnostic accuracy and charge-savings of outpatient core needle biopsy compared with open biopsy of musculoskeletal tumors. J Bone Joint Surg Am. 1996;78(5):644–9.
Sung KS, Seo SW, Shon MS. The diagnostic value of needle biopsy for musculoskeletal lesions. Int Orthop. 2009;33:1701.
Datir A, Pechon P, Saifuddin A. Imaging-guided percutaneous biopsy of pathologic fractures: a retrospective analysis of 129 cases. AJR Am J Roentgenol. 2009;193(2):504–8.
Sheppard JE, Switlick DN. Coccidioides immitis osteomyelitis of the radius presenting as Ewing’s sarcoma. Orthopedics. 2008;31(6):607.
Sundaram M, McDonald D, Engel E, Rotman M, Siegfried EC. Chronic recurrent multifocal osteomyelitis: an evolving clinical and radiological spectrum. Skeletal Radiol. 1996;25(4):333–6.
Abril JC, Castillo F, Casas J, Diaz A. Brodie’s abscess of the hip simulating osteoid osteoma. Orthopedics. 2000;23(3):285–7.
Yip KM, Lin J, Leung PC. Cystic tuberculosis of the bone mimicking osteogenic sarcoma. Tuber Lung Dis. 1996;77(6):566–8.
Kalbermatten DF, Kalbermatten NT, Siebenrock KA. Osteolytic lesion in the greater trochanter mimicking tumor. Arch Orthop Trauma Surg. 2002;122(1):53–5.
Solomon L. Stress fractures of the femur and tibia simulating malignant bone tumous. S Afr J Surg. 1974;12(1):19–25.
Jordanov MI, Block JJ, Gonzalez AL, Green NE. Transarticular spread of Ewing sarcoma mimicking septic arthritis. Pediatr Radiol. 2009;39(4):381–4.
Datir A, Lidder S, Pollock R, Tirabosco R, Saifuddin A. High-grade chondrosarcoma mimicking Brodie’s abscess. Clin Radiol. 2009;64(9):944–7.
Schwartz HS, Spengler DM. Needle tract recurrences after closed biopsy for sarcoma: three cases and review of the literature. Ann Surg Oncol. 1997;4(3):228–36.
Stoker DJ, Cobb JP, Pringle JA. Needle biopsy of musculoskeletal lesions. A review of 208 procedures. J Bone Joint Surg Br. 1991;73(3):498–500.
Harish S, Hughes RJ, Saifuddin A, Flanagan AM. Image-guided percutaneous biopsy of intramedullary lytic bone lesions: utility of aspirated blood clots. Eur Radiol. 2006;16(9):2120–5.
Saifuddin A, Mitchell R, Burnett SJ, Sandison A, Pringle JA. Ultrasound-guided needle biopsy of primary bone tumours. J Bone Joint Surg Br. 2000;82(1):50–4.
Alyas F, James SL, Davies AM, Saifuddin A. The role of MR imaging in the diagnostic characterisation of appendicular bone tumours and tumour-like conditions. Eur Radiol. 2007;17(10):2675–86.
Gillespy 3 T, Manfrini M, Ruggieri P, Spanier SS, Pettersson H, Springfield DS. Staging of intraosseous extent of osteosarcoma: correlation of preoperative CT and MR imaging with pathologic macroslides. Radiology. 1988;167(3):765–7.
Golfieri R, Baddeley H, Pringle JS, Souhami R. The role of the STIR sequence in magnetic resonance imaging examination of bone tumours. Br J Radiol. 1990;63(748):251–6.
Narvani AA, Tsiridis E, Saifuddin A, Briggs T, Cannon S. Does image guidance improve accuracy of core needle biopsy in diagnosis of soft tissue tumours? Acta Orthop Belg. 2009;75(2):239–44.
Frassica FJ, Unni KK, Beabout JW, Sim FH. Dedifferentiated chondrosarcoma. A report of the clinicopathological features and treatment of seventy-eight cases. J Bone Joint Surg Am. 1986;68(8):1197–205.
Bertoni F, Bacchini P, Staals EL, Davidovitz P. Dedifferentiated parosteal osteosarcoma: the experience of the Rizzoli Institute. Cancer. 2005;103(11):2373–82.
Saifuddin A, Mann BS, Mahroof S, Pringle JA, Briggs TW, Cannon SR. Dedifferentiated chondrosarcoma: use of MRI to guide needle biopsy. Clin Radiol. 2004;59(3):268–72.
Jelinek JS, Murphey MD, Kransdorf MJ, Shmookler BM, Malawer MM, Hur RC. Parosteal osteosarcoma: value of MR imaging and CT in the prediction of histologic grade. Radiology. 1996;201(3):837–42.
Logan PM, Connell DG, O‘Connell JX, Munk PL, Janzen DL. Image-guided percutaneous biopsy of musculoskeletal tumors: an algorithm for selection of specific biopsy techniques. AJR Am J Roentgenol. 1996;166(1):137–41.
General Medical Council. Consent: patients and doctors making decisions together. London: General Medical Council; 2008.
Rimondi E, Staals EL, Errani C, Bianchi G, Casadei R, Alberghini M, et al. Percutaneous CT-guided biopsy of the spine: results of 430 biopsies. Eur Spine J. 2008;17(7):975–81.
Tehranzadeh J, Tao C, Browning CA. Percutaneous needle biopsy of the spine. Acta Radiol. 2007;48(8):860–8.
Lis E, Bilsky MH, Pisinski L, Boland P, Healey JH, O‘Malley B, et al. Percutaneous CT-guided biopsy of osseous lesion of the spine in patients with known or suspected malignancy. AJNR Am J Neuroradiol. 2004;25(9):1583–8.
Stringham DR, Hadjipavlou A, Dzioba RB, Lander P. Percutaneous transpedicular biopsy of the spine. Spine (Phila Pa 1976). 1994;19(17):1985–91.
Dave BR, Nanda A, Anandjiwala JV. Transpedicular percutaneous biopsy of vertebral body lesions: a series of 71 cases. Spinal Cord. 2009;47(5):384–9.
Pierot L, Boulin A. Percutaneous biopsy of the thoracic and lumbar spine: transpedicular approach under fluoroscopic guidance. AJNR Am J Neuroradiol. 1999;20(1):23–5.
Olscamp A, Rollins J, Tao SS, Ebraheim NA. Complications of CT-guided biopsy of the spine and sacrum. Orthopedics. 1997;20(12):1149–52.
Davies NM, Livesley PJ, Cannon SR. Recurrence of an osteosarcoma in a needle biopsy track. J Bone Joint Surg Br. 1993;75(6):977–8.
Iemsawatdikul K, Gooding CA, Twomey EL, Kim GE, Goldsby RE, Cohen I, et al. Seeding of osteosarcoma in the biopsy tract of a patient with multifocal osteosarcoma. Pediatr Radiol. 2005;35(7):717–21.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 EFORT
About this entry
Cite this entry
Saifuddin, A., Clarke, A.W. (2014). Biopsy of Bone and Soft Tissue Sarcomas. In: Bentley, G. (eds) European Surgical Orthopaedics and Traumatology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-34746-7_176
Download citation
DOI: https://doi.org/10.1007/978-3-642-34746-7_176
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-34745-0
Online ISBN: 978-3-642-34746-7
eBook Packages: MedicineReference Module Medicine