Abstract
Objectives
The study aimed to explore the effects of codeine-containing cough syrup (CCS) exposure on cortical morphology and the relationship between cortical characteristics and CCS dependence.
Methods
Cortical morphometry based on Computational Anatomy Toolbox (CAT12) was used to compare changes in sulcal depth, gyrification, and cortical thickness of the cerebral cortex from 40 CCS users and 40 healthy controls (HCs) with two-sample t tests (p < 0.05, multiple comparison corrected). Relationships between abnormal cortical morphological changes and the duration of CCS use, impulsivity traits, and age of first use were investigated with correlation analysis (p < 0.05, uncorrected).
Results
CCS users exhibited significantly increased sulcal depth in the bilateral insula, bilateral lingual, bilateral superior frontal, right precuneus, and right middle frontal regions; increased gyrification in the right precentral cortex; and increased cortical thickness in the bilateral precentral, bilateral precuneus, and right superior temporal cortices compared to HCs. In addition, we found significant correlations between the bilateral insula, right superior frontal cortex, and right precentral gyrus and Barratt Impulsiveness Scale (BIS) total scores.
Conclusions
Chronic CCS abuse may be associated with aberrant sulcal depth, gyrification, and cortical thickness. These morphological changes might serve as an underlying neurobiological mechanism of impulsive behavior in the CCS users.
Key Points
• Cortical morphological changes were detected in CCS users.
• Increased sulcal depth, gyrification, and cortical thickness of some regions were found in the CCS users.
• Positive correlations between cortical morphological changes and BIS total scores were identified.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Codeine-containing cough syrup (CCS) is one of the most wildly used opiates in the world [1, 2]. Although codeine is less addictive than other opiates, long-term use can lead to physical and psychological dependence [3]. Neuroimaging studies showed that addiction can induce changes in brain structure [4,5,6,7,8] and function [9,10,11]. Nevertheless, most of these studies focused on the illicit drugs, such as heroin [8, 11], marijuana [12, 13], and cocaine [14, 15], and limited studies paid attention to the abuse of licit drugs, such as CCS [16, 17], which can be easily accessed over the counter. Previous studies have demonstrated abnormal white matter integrity [16] and gray matter volume [18] in the CCS users. However, neurobiological relationships of CCS abuse still remain enigmatic.
Most previous studies have analyzed regional alterations within the brain gray matter volume or density in addicts in response to drug use [4,5,6,7,8]. For example, Lin et al [19] found lower gray matter volume over the right dorsal lateral prefrontal cortex in heroin-dependent men in comparison with the controls. Ersche et al [7] investigated the cocaine-dependent individuals and reported decreases of gray matter volume in the orbitofrontal, cingulate, insular, temporoparietal, and cerebellar cortex, and increases in the basal ganglia. As for the CCS users, Qiu et al [18] found decreased gray matter volume in the ventromedial prefrontal cortex, which was also correlated with the Barratt Impulsiveness Scale (BIS) total scores and the duration of CCS use. However, whether and how CCS dependence can affect cortical characteristics is still unknown.
Cortical characteristics, such as cortical thickness, local gyrification index, and sulcal depth, have been shown to be sensitive to normal aging [20], cognitive performance [21], and pathological changes [22] and seem to reflect the architecture of the cerebral column [23]. Cortical morphometric analysis might provide more precise information about underling drug-related mechanisms. Several previous studies used surface-based morphometry to assess cortical thickness and found abnormalities in the brain structures of a variety of substance users, such as heroin users [8], smokers [24, 25], alcohol users [26, 27], and marijuana users [12, 26]. To the best of our knowledge, very few studies have explored cortical thickness abnormalities in CCS, except that Qiu et al [28] reported cortical thickness alterations in the young adults who were dependent on dextromethorphan-containing cough syrups. Nevertheless, another two morphometric characteristics, gyrification and sulcal depth, that are thought to be independent of cortical thickness [29, 30] have never been explored in CCS users.
Therefore, the purposes of the present study were (1) to perform a comprehensive analysis on the cortical morphology of CCS users vs. matched healthy controls and (2) to investigate the clinical significance between cortical characteristic’s changes and clinical symptoms in the CCS users. Based on the previous structural and functional studies of addiction, we hypothesized that cortical morphometry would be altered in some regions of the brain, especially in the regions responsible for executive control. In addition, the cortical characteristics in abnormal regions observed in CCS users may be correlated with the impulsivity behavior.
Materials and methods
Participants
Forty CCS users (38 males, 2 females; mean age 24.13 years ± 3.16 years) were recruited from the Addiction Medicine Division at Guangdong Second Provincial General Hospital. Each of the CCS users was screened based on the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) criteria to confirm the diagnosis of substance dependence, along with a urine test and an interview conducted by a clinical psychologist. Furthermore, none of the CCS users had any known use of any other types of illicit drugs and had drug treatments. We also recruited 40 age-, hand-, and gender-matched healthy controls (HCs) (38 males, 2 females; mean age 24.40 years ± 3.59 years) from the local community by means of advertisements. Inclusion criteria for the control subjects included lack of diagnosis of substance abuse or dependence based on a clinical diagnosis and an interview. Exclusion criteria for all participants were as follows: neurological illness, head injury, schizophrenia or affective disorder, and other substance dependences. This study was approved by the Ethics Committee of the Guangdong Second Provincial General Hospital. Written informed consent was obtained from all subjects.
Impulsivity assessment
To evaluate the impulsive personality traits, all participants underwent BIS 11 before undergoing MRI. BIS 11 has three oblique factors: attentional/cognitive, which measures toleration for cognitive complexity and persistence; motor, which measures the tendency to act upon the spur of the moment; and non-planning impulsivity, which measures the lack of sense about the future. Items are rated from 1 (rarely/never) to 4 (almost always/always), and the sum of all items stands for overall impulsiveness. That is, the higher the scores, the greater the impulsivity [31].
MRI scanning
MRI data were obtained on a Philips Achieva 1.5 T Nova Dual MR scanner using a 16-channel NV coil in the Department of Medical Imaging, Guangdong Second Provincial General Hospital. Tight but comfortable foam padding was used to minimize head motion, and earplugs were used to reduce scanner noise. Sagittal structural images [160 sagittal slices, repetition time (TR) = 25 ms, echo time (TE) = 4.1 ms, thickness = 1.0 mm, no gap, in-plane resolution = 231 × 232, field of view (FOV) = 230 mm × 230 mm, flip angle = 30°] were acquired using a fast field echo (FFE) three-dimensional T1-weighted sequence. All the CCS users were scanned after 24–48 h from the last time of CCS use. After scanning, the patients were consulted, and it was determined that none of them experience craving or withdrawal symptoms during the MRI scanning.
Data processing
The surface analysis was conducted using the Computational Anatomy Toolbox (CAT12) (http://dbm.neuro.uni-jena.de/cat/) that provides a fully automated method to estimate cortical thickness and the central surface of hemispheres based on the projection-based thickness (PBT) method [32]. All images underwent automated segmentation to gray matter (GM), white matter (WM), and cerebrospinal fluid (CSF); affine registration to an MNI template space; and subsequently, a nonlinear deformation. In the CAT12, a new fully automated method allows cortical thickness to be measured and the central surface to be reconstructed in a single step [32]. The program uses tissue segmentation to estimate the white matter distance and projects the local maxima (which is equal to the cortical thickness) to other gray matter voxels using a neighbor relationship that is described by the white matter distance. This projection-based thickness method also includes partial volume correction, sulcal blurring, and sulcal asymmetries without sulcus reconstruction. Newly created images were smoothed with a 15 mm FWHM of Gaussian smoothing kernel, and total intracranial volume (TIV) was calculated. We extracted several additional measures for surface, such as gyrification index and sulcal depth. Gyrification index is measured as a ratio of the external brain surface with the outer surface excluding the sulci. Gyrification index calculation was based on absolute mean curvature [33]. Square root–transformed sulcus depth was based on the Euclidean distance between the central surface and its convex hull. Transformation with square root function was used to render the data more normally distributed.
In order to compare the difference in a measure of atrophy, we calculated the relative alterations between brain volume and intracranial volume using the following equation:
where GM, WM, and CSF represent the volume of gray matter, white matter, and cerebrospinal fluid, respectively.
Statistical analyses
Two-sample t tests were performed to assess the differences in age, education, impulsive behavior, and cigarette smoking, and a chi-square test was used to assess the gender composition between the CCS users and HCs using SPSS 22.0.
The cortical morphometric maps on the left and right hemispheres were separately statistically analyzed using two-sample t tests including age, gender, nicotine usage, and education as covariates. Correction for multiple comparisons was performed using the cluster-level family-wise error (FWE) method, resulting in a cluster defining threshold of a p value equal to 0.001 and a corrected cluster significance of a p value < 0.05. We also performed a mean cortical thickness measure within the regions that show sulcal depth differences between groups.
In addition, correlation analyses were performed between the mean cortical characteristics of each significant cluster and the duration of CCS use, impulsivity traits, age of first use, age while taking, gender, nicotine usage, and education as covariates (p < 0.05, uncorrected).
Results
Demographics and clinical characteristics
We found no significant differences in age, gender, education, total intracranial volume, and cigarette smoking between the CCS users and the HCs. The mean duration of CCS use was 5.21 years, and the mean age of first use of CCS was 18.9 years. We also observed that CCS users had significant higher attentional impulsivity, motor impulsivity, non-plan impulsivity, and BIS total scores than the HC group (Table 1).
Alterations of cortical morphology
Sulcal depth
We found significant increases in sulcal depth in seven clusters in the CCS users compared to the HCs (p < 0.05, FWE corrected; Table 2). Figure 1 shows the location of these clusters on the cortical surface, and Table 2 lists the detailed information of these clusters, including left and right insula (INS.L and INS.R, respectively), left and right lingual gyrus (LING.L and LING.R, respectively), left and right superior frontal cortex (SFC.L and SFC.R, respectively), right precuneus (PCUN.R), and right middle frontal cortex (MFC.R).
Gyrification index
We found a significant increase in the right precentral gyrus (PreCG.R) in the CCS users compared to the HCs (Fig. 1, Table 2).
Cortical thickness
We found significant increases in cortical thickness in five clusters, which were primarily located in the bilateral PreCG, bilateral PCUN, and the right superior temporal cortex (STC.R) (Fig. 1, Table 2).
However, there was no inter-group difference of cortical thickness in the brain regions showing increased sulcal depth after multiple comparison correction.
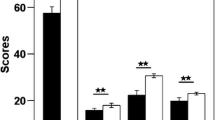
Correlation
Correlation analysis demonstrated significantly positively correlations between mean sulcal depth in the bilateral INS (INS.R, r = 0.343; INS.L, r = 0.421) and SFC.R (r = 0.352) and BIS total scores in CCS users (Fig. 2). We also found a significant positive correlation between the thickness in the PreCG.R (r = 0.340) and the BIS total scores (Fig. 2). However, we did not find significant correlations between mean cortical characteristics and the initial age of CCS use or BIS total scores in the other clusters listed in Table 2. In addition, we did not find significant correlations between characteristics and the duration of CCS use as well as the BIS subscales in CCS users. Within the HC, we also did not find significant correlations between the cortical characteristics and impulsive behavior. Unfortunately, for any region listed in Table 2, we found no significant correlations between the mean cortical characteristics and the BIS total scores when we performed the multiple comparison correction.
Scatter plots of the mean sulcal depth of the clusters in the bilateral insula (INS) and the right superior frontal cortex (SFC.R), and the mean cortical thickness of the right precentral gyrus (PreCG.R) positively correlated with the BIS total scores in the codeine-containing cough syrup (CCS) users
Discussion
In the current study, cortical morphometry based on CAT12 was applied to quantify the sulcal depth, gyrification, and cortical thickness in the codeine-containing cough syrup users compared to healthy controls. We found abnormal changes in cortical morphology in the CCS users in clusters primarily located in the frontal and temporal cortices as well as in the insula (Fig. 1). In addition, we also observed positive correlations between the mean sulcal depth/cortical thickness with BIS total scores.
We found significantly increased sulcal depth in the bilateral SFC and MFC.R, which are located in the prefrontal cortex (PFC) and belong to the cognitive control circuit of drug addiction [34]. The circuit plays a vital role in the higher-order cognitive function, including goal-directed attention [35, 36], decision [37, 38], and execution [39]. Previous neuroimaging studies in the drug addiction have revealed disruption across regions of the control circuit [4, 5, 7, 8, 12, 18, 19]. Several fMRI studies indicated that resting-state abnormalities of the prefrontal cortex in the addicts were associated with the degree of cognitive impairments [11, 40]. Brain morphological studies also revealed abnormalities in the frontal cortex of drug users, which have reported decreases in gray matter volume/density or in cortical thickness of the PFC in addicts compared to control subjects [5, 8, 12, 24]. In the current study, despite no significant changes in cortical thickness of the PFC, the increased cortical complexity of sulcal depth may lead to controversial results in contrast to previous studies. The discrepancy may be explained by two ways. First, different substance dependences may induce diverse neurotoxic effects on the cortex. Some may result in neural cell death or shrinkage [41], while others may bring about synaptic refinement [28, 42]. Previous studies have shown that drug taking plays a role in blocking the dopamine transporters (DATs) to reinforce effects [17, 43, 44]. By blocking DATs, CCS increases the concentration of DA in the synapse, enhancing its signal. Synaptic refinement involves eliminating unnecessary neural connections to reduce gray matter [45]. The increased concentration of DA may interfere with synaptic pruning processes, which may explain the increased cortical complexity of sulcal depth in the CCS addicts [46, 17]. Second, altered developmental trajectory of the frontal cortex may attribute to the increases in sulcal depth of the CCS abuse. Previous studies have shown linear decreased gray matter in frontal regions with age from adolescent to adulthood years [47,48,49,50]. The increased DA levels induced by drug taking have an important role in coding reward and prediction of reward [51]. What is more, the PFC has been involved in processing the reward value of various stimuli [52]. Thus, our findings of abnormal cortical characteristics in the PFC may be responsible for seeking rewards and the compulsiveness of drug taking in CCS, which may disrupt the original developmental trajectory. Combined with previous addictive studies, our finding might indicate that the frontal cortex is susceptible to CCS dependence.
In this study, we also detected increases in cortical complexity in the INS of the CCS users. Daglish et al [10] applied the functional connectivity analysis and found abnormal brain activation in the INS in opiate users while they were exposed to environmental cues. Hester et al [53] studied chronic cannabis users with a Go/No-Go response inhibition task and also found abnormal insula activity. Previous studies [54,55,56] suggested that the INS plays a broader role in the interoception and subjective feeling states that are usually changing with satiety and with the top-down cognitive modulation of cravings. A study of Contreras et al [57] inactivated the insular cortex in amphetamine-experienced rats, which prevented the urge to seek amphetamine in a place preference task. Naqvi et al [58] also found that smokers with brain damage involving the insula were more likely than smokers with brain damage not involving the insula to undergo a disruption of smoking addiction. Thus, we speculated that the increases of sulcal depth in the INS may induce to more sensitively perceive inner subjective feeling states of stimulation after drug intake, leading to increased impulsivity in drug use [54]. In addition, the INS, connected with precentral and temporal regions, belongs to the salience network [56]. Previous studies have suggested the salience network played a role in dynamically controlling changes of activity of other brain networks [59], and in the integration of sensations, self-awareness, and information which could contribute to how addicted individuals decide about taking drugs [60, 61]. The increased changes in the network might suggest that CCS abuse influences the “salience” processing, such as connection with cognitive control network [59]. Therefore, the increased cortical characteristics (cortical thickness, gyrification, and sulcal depth) in the insula and in the precentral and temporal cortices within salience network may cause CCS users to be unable to make appropriate decisions to avoid of craving when exposed to drug cues.
In addition, we also found increased cortical characteristics (cortical thickness and sulcal depth) in the precuneus (extending to cuneus) and lingual regions. Previous studies suggested that the PCUN had been involved in visual processing and inhibitory control [62]. The increased cortical thickness in the precuneus observed in the present study is consistent with several previous addictive studies [8, 28]. For example, in a study of heroin addiction, researchers reported increased amplitude of low-frequency fluctuation of the spontaneous neuronal activity in the left precuneus compared to controls [63]. Another study of active and abstinent marijuana users performed visual-attention tasks and detected greater activation in various parietal and occipital regions, including the precuneus and lingual regions [64]. As for the morphometric studies, Lopez-Larson et al [12] investigated brain structural alterations in marijuana users and found significantly increased cortical thickness in the lingual and temporal regions. A study by our group about heroin-dependent individuals has also reported increased cortical thickness in the PCUN and LING regions [8]. Thus, the increased cortical characteristics of the PCUN and LING regions may indicate the presence of neuroadaptive processes in the brains of drug users.
In this study, we reported that the group difference in sulcal depth was greater than that of cortical thickness. Previous studies have indicated that sulcal depth is sensitive to cortical atrophy and development [65,66,67]. For example, in mild cognitive impairment, when detecting group differences between control and patients, measuring the degree of sulcal widening was more sensitive than cortical thickness [65]. In normal aging, while cortical thickness undergoes relatively small changes, the average span of sulcal spaces is greatly increased [66, 67]. Thus, our finding of increased sulcal depth may also prove the point that sulcal depth is a more sensitive measure of function than cortical thickness.
We found that in the bilateral INS and SFC, the sulcal depth was significantly positively correlated with BIS total scores, and that in the PreCG.R, the cortical thickness was significantly positively correlated with BIS total scores. That is, the increased cortical characteristics of the INS, SFC, and PreCG are associated with the higher impulsivity of the CCS use. The study of Qiu et al [28] reported similar findings, which analyzed alterations in cortical thickness in adolescents and young adults dependent on dextromethorphan-containing cough syrups, and found a positive correlation between thickness of the prefrontal cortex and BIS total scores. Therefore, the correlations between cortical characteristics and BIS scores may indicate that abnormalities in these brain regions might be a major influencer in the craving of drug taking. However, when multiple comparison correction had been performed, no correlations remained significant. The possible explanation is that the different severities of addiction among abusers may contribute to the findings. The light or moderate severity of CCS users may reduce the relationships between the impulsive behaviors and cortical characteristics. Further studies should pay more attention to the effects of classification of severity on the brain structure.
This study has several limitations. First, because this was a cross-sectional study, we cannot conclusively clarify the causal relationship between cortical morphological differences and CCS use. Second, most of the CCS users and healthy controls in the present study also used nicotine, which may confound the results, despite taking nicotine as a covariate in our analysis. In the future studies, we may need to recruit non-nicotine users to exclude the possible effect. Third, we could not assess the influence of severity of CCS use on the cortical morphology, because we did not quantitatively measure them with specific scales. This issue should be considered in the future study. Last but not the least, the gender composition was imbalanced. Although neuroimaging studies have investigated gender effects on brain structure in drug users [13, 68], any gender differences in the relationship between cortical morphology and CCS use are worth further exploration.
Conclusion
In summary, this is one of the first studies to evaluate cortical morphology with sulcal depth gyrification and cortical thickness in CCS users compared to non-users. We detected alterations in the cortical morphology of the prefrontal cortex (SFC and MFC.R) and insula in CCS users, which may affect the capacity of inhibitory control and self-interoception and contribute to conscious drug craving. We also found increased cortical characteristics of the INS, SFC, and PreCG.R correlated with the BIS total scores. These results may provide important information to neurophysiological mechanisms of impulsive behavior in CCS users.
Abbreviations
- BIS:
-
Barratt Impulsiveness Scale
- CAT12:
-
Computational Anatomy Toolbox
- CCS:
-
Codeine-containing cough syrup
- HCs:
-
Healthy controls
- INS:
-
Insula
- LING:
-
Lingual
- MFC:
-
Middle frontal cortex
- PBT:
-
Projection-based thickness
- PCUN:
-
Precuneus
- PFC:
-
Prefrontal cortex
- PreCG:
-
Precentral gyrus
- SFC:
-
Superior frontal cortex
- STC:
-
Superior temporal cortex
- TIV:
-
Total intracranial volume
References
Hutchings HA, Eccles R (1994) The opioid agonist codeine and antagonist naltrexone do not affect voluntary suppression of capsaicin induced cough in healthy subjects. Eur Respir J 7:715–719
Shek DT, Lam CM (2006) Adolescent cough medicine abuse in Hong Kong: implications for the design of positive youth development programs in Hong Kong. Int J Adolesc Med Health 18:493–503
Vree TB, van Dongen RT, Koopman-Kimenai PM (2000) Codeine analgesia is due to codeine-6-glucuronide, not morphine. Int J Clin Pract 54:395–398
Daumann J, Koester P, Becker B et al (2011) Medial prefrontal gray matter volume reductions in users of amphetamine-type stimulants revealed by combined tract-based spatial statistics and voxel-based morphometry. Neuroimage 54:794–801
Brody AL, Mandelkern MA, Jarvik ME et al (2004) Differences between smokers and nonsmokers in regional gray matter volumes and densities. Biol Psychiatry 55:77–84
Ersche KD, Jones PS, Williams GB, Turton AJ, Robbins TW, Bullmore ET (2012) Abnormal brain structure implicated in stimulant drug addiction. Science 335:601–604
Ersche KD, Barnes A, Jones PS, Morein-Zamir S, Robbins TW, Bullmore ET (2011) Abnormal structure of frontostriatal brain systems is associated with aspects of impulsivity and compulsivity in cocaine dependence. Brain 134:2013–2024
Li M, Tian J, Zhang R et al (2014) Abnormal cortical thickness in heroin-dependent individuals. Neuroimage 88:295–307
Meunier D, Ersche KD, Craig KJ et al (2012) Brain functional connectivity in stimulant drug dependence and obsessive-compulsive disorder. Neuroimage 59:1461–1468
Daglish MR, Weinstein A, Malizia AL et al (2003) Functional connectivity analysis of the neural circuits of opiate craving: “more” rather than “different”? Neuroimage 20:1964–1970
Qiu YW, Han LJ, Lv XF et al (2011) Regional homogeneity changes in heroin-dependent individuals: resting-state functional MR imaging study. Radiology 261:551–559
Lopez-Larson MP, Bogorodzki P, Rogowska J et al (2011) Altered prefrontal and insular cortical thickness in adolescent marijuana users. Behav Brain Res 220:164–172
McQueeny T, Padula CB, Price J, Medina KL, Logan P, Tapert SF (2011) Gender effects on amygdala morphometry in adolescent marijuana users. Behav Brain Res 224:128–134
Makris N, Gasic GP, Kennedy DN et al (2008) Cortical thickness abnormalities in cocaine addiction—a reflection of both drug use and a pre-existing disposition to drug abuse? Neuron 60:174–188
Moreno-López L, Catena A, Fernández-Serrano MJ et al (2012) Trait impulsivity and prefrontal gray matter reductions in cocaine dependent individuals. Drug Alcohol Depend 125:208–214
Qiu YW, Su HH, Lv XF, Jiang GH (2015) Abnormal white matter integrity in chronic users of codeine-containing cough syrups: a tract-based spatial statistics study. AJNR Am J Neuroradiol 36:50–56
Hou H, Yin S, Jia S et al (2011) Decreased striatal dopamine transporters in codeine-containing cough syrup abusers. Drug Alcohol Depend 118:148–151
Qiu YW, Lv XF, Jiang GH et al (2014) Reduced ventral medial prefrontal cortex (vmPFC) volume and impaired vmPFC-default mode network integration in codeine-containing cough syrups users. Drug Alcohol Depend 134:314–321
Lin HC, Wang PW, Wu HC, Ko CH, Yang YH, Yen CF (2018) Altered gray matter volume and disrupted functional connectivity of dorsolateral prefrontal cortex in men with heroin dependence. Psychiatry Clin Neurosci 72:435–444
Tamnes CK, Ostby Y, Fjell AM, Westlye LT, Due-Tønnessen P, Walhovd KB (2010) Brain maturation in adolescence and young adulthood: regional age-related changes in cortical thickness and white matter volume and microstructure. Cereb Cortex 20:534–548
Gautam P, Anstey KJ, Wen W, Sachdev PS, Cherbuin N (2015) Cortical gyrification and its relationships with cortical volume, cortical thickness, and cognitive performance in healthy mid-life adults. Behav Brain Res 287:331–339
Wei Q, Li M, Kang Z et al (2015) ZNF804A rs1344706 is associated with cortical thickness, surface area, and cortical volume of the unmedicated first episode schizophrenia and healthy controls. Am J Med Genet B Neuropsychiatr Genet 168B:265–273
Pontious A, Kowalczyk T, Englund C, Hevner RF (2008) Role of intermediate progenitor cells in cerebral cortex development. Dev Neurosci 30:24–32
Li Y, Yuan K, Cai C et al (2015) Reduced frontal cortical thickness and increased caudate volume within fronto-striatal circuits in young adult smokers. Drug Alcohol Depend 151:211–219
Kühn S, Schubert F, Gallinat J (2010) Reduced thickness of medial orbitofrontal cortex in smokers. Biol Psychiatry 68:1061–1065
Jacobus J, Squeglia LM, Sorg SF, Nguyen-Louie TT, Tapert SF (2014) Cortical thickness and neurocognition in adolescent marijuana and alcohol users following 28 days of monitored abstinence. J Stud Alcohol Drugs 75:729–743
Migliorini R, Moore EM, Glass L et al (2015) Anterior cingulate cortex surface area relates to behavioral inhibition in adolescents with and without heavy prenatal alcohol exposure. Behav Brain Res 292:26–35
Qiu YW, Lv XF, Jiang GH et al (2017) Potential gray matter unpruned in adolescents and young adults dependent on dextromethorphan-containing cough syrups: evidence from cortical and subcortical study. Brain Imaging Behav 11:1470–1478
Im K, Lee JM, Yoon U et al (2006) Fractal dimension in human cortical surface: multiple regression analysis with cortical thickness, sulcal depth, and folding area. Hum Brain Mapp 27:994–1003
Hogstrom LJ, Westlye LT, Walhovd KB, Fjell AM (2013) The structure of the cerebral cortex across adult life: age-related patterns of surface area, thickness, and gyrification. Cereb Cortex 23:2521–2530
Patton JH, Stanford MS, Barratt ES (1995) Factor structure of the Barratt Impulsiveness Scale. J Clin Psychol 51:768–774
Dahnke R, Yotter RA, Gaser C (2013) Cortical thickness and central surface estimation. Neuroimage 65:336–348
Luders E, Thompson PM, Narr KL, Toga AW, Jancke L, Gaser C (2006) A curvature-based approach to estimate local gyrification on the cortical surface. Neuroimage 29:1224–1230
Baler RD, Volkow ND (2006) Drug addiction: the neurobiology of disrupted self-control. Trends Mol Med 12:559–566
Asplund CL, Todd JJ, Snyder AP, Marois R (2010) A central role for the lateral prefrontal cortex in goal-directed and stimulus-driven attention. Nat Neurosci 13:507–512
Benoit RG, Gilbert SJ, Frith CD, Burgess PW (2012) Rostral prefrontal cortex and the focus of attention in prospective memory. Cereb Cortex 22:1876–1886
Walton ME, Devlin JT, Rushworth MF (2004) Interactions between decision making and performance monitoring within prefrontal cortex. Nat Neurosci 7:1259–1265
Gläscher J, Adolphs R, Damasio H et al (2012) Lesion mapping of cognitive control and value-based decision making in the prefrontal cortex. Proc Natl Acad Sci U S A 109:14681–14686
McNamee D, Rangel A, O’Doherty JP (2013) Category-dependent and category-independent goal-value codes in human ventromedial prefrontal cortex. Nat Neurosci 16:479–485
Galynker II, Eisenberg D, Matochik JA et al (2007) Cerebral metabolism and mood in remitted opiate dependence. Drug Alcohol Depend 90:166–174
Crews FT, Braun CJ, Hoplight B, Switzer RC 3rd, Knapp DJ (2000) Binge ethanol consumption causes differential brain damage in young adolescent rats compared with adult rats. Alcohol Clin Exp Res 24:1712–1723
Squeglia LM, Jacobus J, Tapert SF (2009) The influence of substance use on adolescent brain development. Clin EEG Neurosci 40:31–38
Ritz MC, Lamb RJ, Goldberg SR, Kuhar MJ (1987) Cocaine receptors on dopamine transporters are related to self-administration of cocaine. Science 237:1219–1223
Volkow ND, Fowler JS, Wang GJ (1999) Imaging studies on the role of dopamine in cocaine reinforcement and addiction in humans. J Psychopharmacol 13:337–345
Gogtay N, Giedd JN, Lusk L et al (2004) Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci U S A 101:8174–8179
Volkow ND, Fowler JS, Wang GJ, Goldstein RZ (2002) Role of dopamine, the frontal cortex and memory circuits in drug addiction: insight from imaging studies. Neurobiol Learn Mem 78:610–624
Tisserand DJ, Pruessner JC, Sanz Arigita EJ et al (2002) Regional frontal cortical volumes decrease differentially in aging: an MRI study to compare volumetric approaches and voxel-based morphometry. Neuroimage 17:657–669
Raz N, Lindenberger U, Rodrigue KM et al (2005) Regional brain changes in aging healthy adults: general trends, individual differences and modifiers. Cereb Cortex 15:1676–1689
Sowell ER, Thompson PM, Tessner KD, Toga AW (2001) Mapping continued brain growth and gray matter density reduction in dorsal frontal cortex: inverse relationships during postadolescent brain maturation. J Neurosci 21:8819–8829
Sowell ER, Thompson PM, Leonard CM, Welcome SE, Kan E, Toga AW (2004) Longitudinal mapping of cortical thickness and brain growth in normal children. J Neurosci 24:8223–8231
Volkow ND, Fowler JS, Wang GJ, Swanson JM (2004) Dopamine in drug abuse and addiction: results from imaging studies and treatment implications. Mol Psychiatry 9:557
Volkow ND, Wang GJ, Tomasi D, Baler RD (2013) Unbalanced neuronal circuits in addiction. Curr Opin Neurobiol 23:639–648
Hester R, Nestor L, Garavan H (2009) Impaired error awareness and anterior cingulate cortex hypoactivity in chronic cannabis users. Neuropsychopharmacology 34:2450–2458
Garavan H (2010) Insula and drug cravings. Brain Struct Funct 214:593–601
Clark L, Bechara A (2015) Commentary on Abdolahi et al (2015): Isolating the role of the insula in drug cravings. Addiction 110:2004–2005
Menon V, Uddin LQ (2010) Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct 214:655–667
Contreras M, Ceric F, Torrealba F (2007) Inactivation of the interoceptive insula disrupts drug craving and malaise induced by lithium. Science 318:655–658
Naqvi NH, Rudrauf D, Damasio H, Bechara A (2007) Damage to the insula disrupts addiction to cigarette smoking. Science 315:531–534
Sridharan D, Levitin DJ, Menon V (2008) A critical role for the right fronto-insular cortex in switching between central-executive and default-mode networks. Proc Natl Acad Sci U S A 105:12569–12574
Palaniyappan L, Liddle PF (2012) Does the salience network play a cardinal role in psychosis? An emerging hypothesis of insular dysfunction. J Psychiatry Neurosci 37:17–27
Naqvi NH, Bechara A (2010) The insula and drug addiction: an interoceptive view of pleasure, urges, and decision-making. Brain Struct Funct 214:435–450
Haldane M, Cunningham G, Androutsos C, Frangou S (2008) Structural brain correlates of response inhibition in bipolar disorder I. J Psychopharmacol 22:138–143
Jiang GH, Qiu YW, Zhang XL et al (2011) Amplitude low-frequency oscillation abnormalities in the heroin users: a resting state fMRI study. Neuroimage 57:149–154
Chang L, Yakupov R, Cloak C, Ernst T (2006) Marijuana use is associated with a reorganized visual-attention network and cerebellar hypoactivation. Brain 129:1096–1112
Im K, Lee JM, Seo SW, Kim SH, Kim SI, Na DL (2008) Sulcal morphology changes and their relationship with cortical thickness and gyral white matter volume in mild cognitive impairment and Alzheimer’s disease. Neuroimage 43:103–113
Kochunov P, Mangin JF, Coyle T et al (2005) Age-related morphology trends of cortical sulci. Hum Brain Mapp 26:210–220
Kochunov P, Thompson PM, Coyle TR et al (2008) Relationship among neuroimaging indices of cerebral health during normal aging. Hum Brain Mapp 29:36–45
Thatcher DL, Pajtek S, Chung T, Terwilliger RA, Clark DB (2010) Gender differences in the relationship between white matter organization and adolescent substance use disorders. Drug Alcohol Depend 110:55–61
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Guihua Jiang.
Conflict of interest
The authors declare that they have no competing interests.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional review board approval was obtained.
Study subjects or cohorts overlap
No study subjects or cohorts have been previously reported.
Methodology
• prospective
• cross-sectional study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, M., Hua, K., Li, S. et al. Cortical morphology of chronic users of codeine-containing cough syrups: association with sulcal depth, gyrification, and cortical thickness. Eur Radiol 29, 5901–5909 (2019). https://doi.org/10.1007/s00330-019-06165-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06165-0