Abstract
Adolescence is a unique period in neurodevelopment. Dextromethorphan (DXM)-containing cough syrups are new addictive drugs used by adolescents and young adults. The effects of chronic DXM abuse on neurodevelopment in adolescents and young adults are still unknown. The aim of this study was to investigate the differences in cortical thickness and subcortical gray matter volumes between DXM-dependent adolescents and young adults and healthy controls, and to explore relationships between alternations in cortical thickness/subcortical volume and DXM duration, initial age of DXM use, as well as impulsive behavior in DXM-dependent adolescents and young adults. Thirty-eight DXM-dependent adolescents and young adults and 18 healthy controls underwent magnetic resonance imaging scanning, and cortical thickness across the continuous cortical surface was compared between the groups. Subcortical volumes were compared on a structure-by-structure basis. DXM-dependent adolescents and young adults exhibited significantly increased cortical thickness in the bilateral precuneus (PreC), left dorsal lateral prefrontal cortex (DLPFC. L), left inferior parietal lobe (IPL. L), right precentral gyrus (PreCG. R), right lateral occipital cortex (LOC. R), right inferior temporal cortex (ITC. R), right lateral orbitofrontal cortex (lOFC. R) and right transverse temporal gyrus (TTG. R) (all p < 0.05, multiple comparison corrected) and increased subcortical volumes of the right thalamus and right pallidum. There was a significant correlation between initial age of DXM use and cortical thickness of the DLPFC. L and PreCG. R. A significant correlation was also found between cortical thickness of the DLPFC. L and impulsive behavior in patients. This was the first study to explore relationships between cortical thickness/subcortical volume and impulsive behavior in adolescents dependent on DXM. These structural changes might explain the neurobiological mechanism of impulsive behavior in adolescent DXM users.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescence is a unique period in neurodevelopment that includes synaptic refinement and myelination (Russell 1968). While the developing brain may be more vulnerable to neurotoxic effects (Spear 2002), addiction during adolescence may interrupt the natural course of brain maturation and key processes of brain development. Dextromethorphan (DXM)/codeine-containing cough syrups have been used recently by adolescents and young adults and have resulted in addiction (Darboe et al. 1996; Miller 2005; Wu et al. 2016). Our previous studies have demonstrated white matter myelination dysplasia (Qiu et al. 2015) and orbitofrontal cortex neural cell shrinkage (Qiu et al. 2014) in adolescents and young adults addicted to codeine-containing cough syrups. However, the effects of chronic DXM abuse on the neurodevelopment in adolescents and young adults are still unknown.
Although there are no studies investigating the effects of adolescent DXM abuse on gray matter development, previous studies of adolescent addiction to other substances (or alcohol) have presented inconsistent findings (De Bellis et al. 2005; Medina et al. 2008; Medina et al. 2007; Squeglia et al. 2009). Heavy adolescent marijuana users have shown larger posterior, prefrontal cortex, hippocampus, and global gray matter volume than control subjects. Increased marijuana use predicts increased volume and poorer verbal and attention performance, which indicates that adolescent marijuana use may subtly interfere with synaptic pruning processes, resulting in larger gray matter volumes (Medina et al. 2008; Medina et al. 2007). However, studies have found that heavy drinkers have smaller prefrontal cortical and hippocampal volumes than non-drinkers. This was especially pronounced in females and might be attributed to pathological processes involved in neuronal death or atrophy (Squeglia et al. 2009). Whether and how adolescent DXM abuse can affect neurodevelopment, especially the synaptic refinement is still unknown.
To address this question, we used high resolution structural magnetic resonance imaging (MRI) and surface-based morphometry analysis to investigate cortical and subcortical gray matter changes related to DXM-containing cough syrup abuse in adolescents and young adults. Given that synaptic pruning is a hallmark of the brain transformations during adolescence (Russell 1968), we hypothesized that adolescent DXM abuse may interfere with the synaptic pruning process, which may result in increased cortical thickness and subcortical gray matter volume. Because synaptic pruning occurs primarily in the prefrontal and temporal cortex and in subcortical structures such as the striatum, thalamus, and nucleus accumbens, with frontal lobes being the final areas of the brain to complete development during adolescence (Giedd 2004; Sowell et al. 1999), we expected cortical thickness changes mainly in these regions, especially the prefrontal cortex. We also expected that cortical thickness and subcortical volume would be related to duration of DXM abuse, initial age of DXM use, as well as the impulsivity behavior in DXM-dependent individuals.
Material and methods
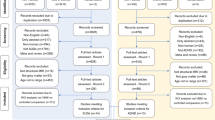
Subjects
This prospective study was approved by the local ethics committee. After receiving a written and oral description of the aim of this study, all participants gave written informed consent statements before inclusion. Fifty-six right-handed male volunteers, including 18 control subjects and 38 DXM-dependent individuals participated in this study. All DXM-dependent individuals were randomly selected from patients seeking treatment at the Addiction Medicine Division of Guangdong No.2 Provincial People’s Hospital. Patients were screened based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria using medical history, a urine test, and an interview. They regularly smoked cigarettes and denied any use of other psychotropic agents in the month prior to undergoing the MRI scan. Patients were excluded from participation if they had any other history of substance abuse. Inclusion criteria for the control subjects were lack of diagnosis of substance abuse or dependence. Exclusion criteria for all participants included neurological illness, schizophrenia or bipolar disorder, prior significant head trauma, positive HIV status, diabetes, hepatitis C, other major medical illness and left-handedness.
Impulsivity assessment
Impulsivity was assessed using the Barratt Impulsiveness Scale (BIS.11) (Patton et al. 1995), which is one of the oldest and most widely used self-report measures of impulsive personality traits. It includes 30 items that are scored according to the following 3 oblique factors: 1) attentional/cognitive impulsivity, which measures tolerance for cognitive complexity and persistence, 2) motor impulsivity, which measures the tendency to act in the spur of the moment, and 3) non-planning impulsivity, which measures the lack of sense of the future. Items are rated from 1 (rarely/never) to 4 (almost always/always). To determine the overall impulsiveness scores, all items were summed, with higher scores indicating greater impulsivity (Patton et al. 1995). BIS.11 is a valid and reliable instrument for healthy and psychiatric Chinese populations (Yao et al. 2007).
MRI scanning
MRI data were obtained on a Philips Achieva 1.5 T Nova dual MR scanner (Philips, Netherlands) using a 16-channel NV coil in the Department of Medical Imaging, Guangdong No.2 Provincial People’s Hospital. None of the subjects were taking any medications at the time of the scans. Tight but comfortable foam padding was used to minimize head motion, and earplugs were used to reduce scanner noise. Sagittal structural images (160 sagittal slices, TR = 25 ms, TE = 4.1 ms, thickness = 1.0 mm, no gap, in-plane resolution =231 × 232, FOV = 230 × 230 mm, flip angle =30°) were acquired using a fast field echo (FFE) three-dimensional T1 weighted sequence.
Data analysis
Prior to processing, all scans were visually examined by a trained rater for motion artifacts or other distortions, and only scans without visible distortion were included in the sample.
Cortical reconstruction and volumetric segmentation of the whole brain were performed using the FreeSurfer software package (Version 5.3.0, http://surfer.nmr.mgh.harvard.edu), which is a widely documented and automated program for reconstructing brain cortical surfaces (Fischl et al. 1999a; Fischl et al. 1999b). The technical details of these procedures have been described previously (Li et al. 2014). Briefly, we processed the T1-weighted 3-dimensional brain structural images by removing the non-brain tissue, transforming the brain into a Talairach-like space, and performing a segmentation to obtain the brain gray and white matters. The boundary or interface between the brain white and gray matters was tessellated, and the topological defects in the gray-white estimate were fixed automatically. After performing intensity normalization and determining the transitions between the brain gray matter and white matter, we identified the boundary between the pia and gray matter by detecting the greatest shift in intensity through cortical surface deformation. Thus, we produced a linked mesh surface that was covered by the triangles. We took each point shared by adjacent triangles on the cortical surface as a vertex. For each subject, the entire cortex was then visually inspected for any inaccuracies in segmentation and manually corrected if necessary. Cortical thickness was measured as follows. We estimated the shortest distance between a given point on the estimated pial surface and the gray-white matter boundary and the shortest distance between a given point on the gray-white matter boundary and the estimated pial surface at each vertex. We then averaged these 2 values to estimate the cortical thickness. The surface of the gray-white matter boundary was inflated, and between-subject differences in the cortical folding patterns of the gyri and sulci were normalized. The reconstructed brain of each subject was morphed and registered to an average spherical surface using a spherical transformation. A thickness measurement at each vertex on the cortical surface was mapped for each subject on a common spherical coordinate system using a spherical transformation. The normalized cortical thickness was smoothed using a Gaussian kernel with a full-width-half-maximum (FWHM) of 10 mm.
The subcortical volumes were obtained from the automated procedure for volumetric measures of brain structures implemented in Freesurfer. Twenty-seven volumetric measures were investigated, and we extracted 7 subcortical structures (accumbens, caudate, thalamus, pallidum, putamen, hippocampus, and amygdala) from each hemisphere. Reliability studies on measuring cortical thickness and subcortical volumes reported that within-scanner variability of cortical thickness and subcortical volume measurements using Freesurfer were estimated to be <0.03 mm and 4.3 %, respectively (Han et al. 2006; Jovicich et al. 2009).
Statistical analyses
Comparisons of demographics and clinical characteristics
Assumptions for normality were tested for all continuous variables. Normality was tested using the Kolmogorov-Smirnov test. All variables were normally distributed. Two-sample t-tests were performed to assess differences in age, education, cigarette smoking and impulsive behavior (BIS total scores, attentional impulsivity scores, motor impulsivity score and non-plan impulsivity scores) between the DMX-dependent individuals and healthy control (HC) groups using SPSS 23.0. All statistical analyses had a two-tailed α level of <0.05 for defining statistical significance.
Comparisons of brain morphometry
For each vertex, a general linear model (GLM) was used to detect significant differences in cortical thickness between the adolescent DXM abusers and the HC using the QDEC utility. The left and right hemispheres were analyzed separately. We regressed out the effects of age, nicotine usage, education, and total intracranial volume (TIV). A Monte Carlo simulation cluster analysis with 10,000 iterations and a cluster threshold of p < 0.05 was performed to resolve the problem of multiple comparisons. Only the surviving cluster is shown in this study.
The 7 subcortical structure volumes (i.e., accumubens, thalamus, caudate nucleus, putamen, pallidum, hippocampus, and amygdala) were imported into the SPSS 23.0 software for statistical analyses. To assess group differences (adolescent DXM abuse vs control) in volumes of subcortical structures, univariate analysis with each volume of subcortical structures as dependent variable, group as fixed factor and TIV, education, nicotine usage, and age as nuisance variables was performed. Results were reported at the significance level of p < 0.05 with Bonferroni correction (7 structures × 2 hemispheres).
Association between brain measurements and clinical characteristics: Based on the results of the vertex-wise analysis, we estimated the partial correlations between the cortical thickness of each significant cluster and the duration of DXM use, initial age of DXM use, as well as impulsive behavior for the DXM abuse participants. First, we determined significant clusters on a statistical parametric map of the between-group differences in cortical thickness, mapped each of these clusters onto each individual cortical surface and extracted the mean cortical thickness. Then, we used SPSS to calculate the partial correlation between the mean cortical thickness of each significant cluster and the duration of DXM use, initial of DXM use and impulsive behavior while taking age, nicotine usage, education, and TIV as covariates within the DXM-dependent adolescents and young adults. In addition, we performed the same correlation analysis (mean cortical thickness of each significant cluster and impulsive behavior) in the HC group. Results were reported at the significance level of p < 0.05 with Bonferroni correction.
In addition, regression analyses were performed to determine the contribution of clinical variables (duration of illness, initial age of DXM use and impulsive behavior) to subcortical structural volumes.
Results
Demographics and clinical characteristics
There were no significant differences in age, formal years of education, or number of cigarettes smoked per day between the DXM-dependent adolescents and young adults and the HC groups. The mean duration of DXM use was 5.15 years, and mean age of first use of DXM was 18.9 years (Table 1). DXM-dependent adolescents and young adults had significantly higher attentional impulsivity, motor impulsivity, non-plan impulsivity, and total scores than the HC group (Fig. 1).
Impulsivity differences between DXM-dependent individuals and healthy controls. DXM-dependent individuals had higher BIS total scores, attentional impulsivity scores, motor impulsivity scores and non-plan impulsivity scores than the control group. DXM, Dextromethorphan. s  p < 0.01 (multiple comparison correction with Bonferroni)
p < 0.01 (multiple comparison correction with Bonferroni)
Increased cortical thickness in DXM-dependent adolescents and young adults
We found significant increases in cortical thickness in 9 clusters, 3 in the left hemisphere and 6 in the right hemisphere, in the DXM-dependent adolescents and young adults compared with the HC (p < 0.05, corrected, Table 2, Fig. 2). Figure 2 shows the location of these clusters on the cortical surface, and Table 2 lists detailed information of these clusters. The clusters with increased thickness were located primarily in the bilateral precuneus (PreC. L and PreC. R), left dorsal lateral prefrontal cortex (DLPFC. L), left inferior parietal lobe (IPL. L), right lateral occipital cortex (LOC. R), right inferior temporal cortex (ITC. R), right lateral orbitofrontal cortex (lOFC. R), right transverse temporal gyrus (TTG. R) and right precentral gyrus (PreCG. R).
Cross-cohort comparisons of cortical thickness between DXM-dependent adolescents and young adults and healthy controls. Controlling for age, education, total intracranial volume and nicotine usage, DXM-dependent individuals had significantly increased cortical thickness in the bilateral precuneus (PreC. L and PreC. R), left dorsal lateral prefrontal cortex (DLPFC. L), left inferior parietal lobe (IPL. L), right lateral occipital cortex (LOC. R), right inferior temporal cortex (ITC. R), right lateral orbitofrontal cortex (lOFC. R), right transverse temporal gyrus (TTG. R) and right precentral gyrus (PreCG. R). Color bars indicate the T value. (p < 0.05, Alphasim corrected)
Increased right thalamus and right pallidum volume in DXM-dependent adolescents and young adults
DXM-dependent adolescents and young adults had significantly increased right thalamus and right pallidum volume compared with HC (Fig. 3). Other subcortical structures did not show significant differences between the2 groups.
Increased right thalamus and right pallidum volume in DXM-dependent adolescents and young adults compared with controls. Controlling for age, education, nicotine usage and total intracranial volume (TIV), DXM-dependent adolescents and young adults had significantly increased right thalamus and right pallidum volumes compared with healthy controls. DXM, Dextromethorphan; R, right; THAL, thalamus.  denote p < 0.05 (multiple comparison correction with Bonferroni)
denote p < 0.05 (multiple comparison correction with Bonferroni)
Cortical thickness correlated with initial age of DXM use in patients
Pearson correlation analysis demonstrated significantly negative correlations between mean cortical thicknesses in the DLPFC. L, PreCG. R and initial age of DXM use (Fig. 4), and a significant positive correlation between mean cortical thicknesses in the DLPFC. L and BIS total scores in DXM-dependent adolescents and young adults (Fig. 5). Notably, we also found a significant negative correlation between the thickness in the DLPFC. L and the initial age of DXM use (Supplementary Fig. 1), and a significant positive correlation between the thickness in the DLPFC. L and the BIS total scores (Supplementary Fig. 2) in the DXM-dependent adolescents and young adults using a voxel-based manner (Supplementary Figs. 1 and 2). However, we did not find significant correlations between mean cortical thickness and the initial age of DXM use or BIS total scores in the other clusters listed in Table 2. In addition, we did not find significant correlations between cortical thickness, subcortical volume and the duration of DXM use as well as the BIS subscales in DXM-dependent adolescents and young adults. Within the HC, we also did not find significant correlations between the cortical thickness, subcortical volume and impulsive behavior.
Cortical thickness of the DLPFC. L and the PreCG. R correlated with the age of initial DXM use in DXM-dependent adolescents and young adults. Pearson correlation analysis demonstrated significant negative correlations between cortical thicknesses of the DLPFC. L a, the PreCG. R b and age of initial DXM use in DXM-dependent adolescents and young adults.
Discussion
Combining cortical thickness analysis and subcortical volume measurement, our study mainly verified the following: 1) The DXM-dependent adolescents and young adults had significantly increased cortical thickness and increased subcortical gray matter (right thalamus and right pallidum) volume compared with HC. 2) The cortical thicknesses of DLPFC. L and PreCG. R were associated with the initial age of DXM use. 3) The cortical thickness of DLPFC. L positively correlated with the BIS total scores in DXM-dependent adolescents and young adults. Synaptic refinement is a hallmark of brain transformation during adolescence and involves reductions of gray matter by eliminating unnecessary neural connections (Gogtay et al. 2004). The increased cortical thickness and subcortical volume observed in the present study may represent unpruned synapses in adolescent DXM addicts. Thus, we suggest that adolescent DXM use may interfere with synaptic pruning processes, especially in the prefrontal and occipital cortices, right thalamus and pallidum. Moreover, interruption of synaptic refinement may underlie impulsive behavior and correlate with initial age of DXM use, with greater impact when exposure occurs during early life.
We found significantly increased cortical thickness in 9 clusters, 3 in the left hemisphere and 6 in the right hemisphere, in the DXM-dependent adolescents and young adults compared with the HC (Fig. 1 and Table 2). These regions are mainly located in the bilateral frontal and occipital lobes, especially in bilateral frontal cortices. We also found significantly increased right thalamic and pallidum volumes in addicted individuals compared with HC. These findings are consistent with the fact that synaptic pruning occurs primarily in the prefrontal and temporal cortices as well as in subcortical structures such as the striatum, thalamus, and nucleus accumbens, with frontal lobes being the final areas of the brain to complete development during adolescence (Gogtay et al. 2004).
The DLPFC is thought to play an important role in coding external events into internal representations and volitional scanning, which enables contents of consciousness to be selected deliberately rather than reflexively, be they events in the environment (Mesulam 2002). The lOFC is involved in stimulus-outcome associations and evaluation and possibly reversal of behavior (Walton et al. 2010). Both regions have been implicated in drug addiction in previous studies. Studies have demonstrated that addicts have lower gray matter volume/density (Alia-Klein et al. 2011; Filbey et al. 2014; Gallinat et al. 2006; Qiu et al. 2013) and lower cortical thickness (Makris et al. 2008) in the DLPFC and lOFC compared with control subjects, which may be attributed to neural cell death or shrinkage. In adolescent addicts, some studies showed reduced gray matter volume or cortical thickness in the DLPFC (Medina et al. 2008), lOFC (Yuan et al. 2013), while others showed opposite changes (Kuhn et al. 2014). This disparity may be due to the following: 1) Different addictive substances may have diverse neurotoxic effects. Some may lead to neural cell death and shrinkage (Crews et al. 2000), while others may interfere with synaptic refinement (Medina et al. 2007; Squeglia et al. 2009). 2) Addiction effects on the brain may have a nonlinear trajectory. For example, marijuana use during adolescence increases the size of the hippocampus (Squeglia et al. 2009). However, after long-term heavy marijuana use, the size of the hippocampus eventually decreases by 12 % (Yücel et al. 2008). In the present study, we found significantly increased cortical thickness in the left DLPFC and the right lOFC, which may represent interference with neural refinement in DXM-dependent adolescents and young adults at this particular stage. However, the long-term effects of DXM abuse must be clarified in a longitudinal follow-up.
We also found an increased volume in the right thalamus and right pallidum in DXM addicts. The thalamus and pallidum play vital roles in substance addiction. The thalamus receives input from the prefrontal cortex and the limbic system and in turn relays signals to the prefrontal association cortex. As a result, it plays a crucial role in attention, planning, decision-making, organization, abstract thinking, multitasking, and active memory (Alcaraz et al. 2015). The pallidum is a brain region reciprocally innervated by the ventral tegmental area and the nucleus accumbens, and it is a critical mediator of drug-induced behavioral sensitization. The ventral pallidum is also a central convergent point for input from the orbitofrontal, prefrontal and infralimbic cortices, the amygdala, the lateral hypothalamus, the ventral tegmental area, the parabrachial nucleus, the subthalamic nucleus, and other structures related to reward (Mickiewicz et al. 2009). The thalamus and pallidum are subcortical gray matters frequently reported to show structural abnormalities in addicts. However, the findings have been inconsistent across studies. Increased thalamic gray matter volume and fractional anisotropy (FA) have been reported in adolescents and young adults addicted to online games, and the increase in thalamic FA was shown to correlate positively with Young’s Internet Addiction Scale (YIAS) scores (Dong et al. 2012; Han et al. 2012). While reduced thalamic gray matter volume was reported in heroin dependent individuals, thalamic gray matter was significantly influenced by alcohol use (Reid et al. 2008). Consistent with previous studies on adolescents addicted to online games, our finding also revealed significant increases in right thalamic and right pallidum gray matter volume in adolescents and young adults addicted to DXM, which may represent unpruned synapsis in these regions. Unpruned synapses in the DLPFC and pallidum are also consistent with the addition model of impaired response inhibition and salience attribution (I-RISA) (Goldstein and Volkow 2011). In this model, balances between the prefrontal cortex, such as the DLPFC involved in higher-order control, and subcortical structures such as the striatum involved in more automatic emotion-related processes, are impaired. Thus, the unpruned synapses in these regions may represent an imbalance of cognitive control and emotional processes, which fits well with the I-RISA model.
Interestingly, we found a significantly negative correlation between the thickness of the DLPFC. L, PreCG. R and the initial age of DXM use, which means that DXM use at a younger age leads to thicker DLPFC and PreCG. It also suggests a greater impact when exposure occurs early in life. This finding may demonstrate that young adolescents are more prone to the deleterious effects of DXM use. We also found a positive correlation between thicknesses of DLPFC. L and BIS total scores in adolescent and young adult DXM abusers, which means that increased thickness of the DLPFC. L is associated with higher impulsivity of the DXM abuser. This finding is consistent with a recent study of healthy young adults, which demonstrated that reductions in both gray matter volume and cortical folding in the ventromedial PFC, ventrolateral PFC, and DLPFC predicted better common executive function, shifting-specific, and updating-specific performance, respectively (Smolker et al. 2014). This correlation is also in agreement with a study related to training with a commercial video game, which revealed that a video gaming training group that was trained for 2 months for at least 30 min per day with a platform game had significantly increased gray matter volume in the right hippocampal formation, right DLPFC and bilateral cerebellum relative to control subjects. Furthermore, they found that gray matter increases in the hippocampus and DLPFC correlated with participants’ desire for video gaming, which suggests that volume change plays a role in predicting desire (Kuhn et al. 2014).
Limitations
We acknowledge that our present study has several limitations. First, the present study is a cross-sectional case-control design study that revealed increased cortical thickness and larger subcortical gray matter volume in adolescent and young adult DXM addicts, but the trajectory of the DXM effects on brain development is unclear. A longitudinal study is needed to elucidate this issue. Second, the sample size is not large, which may reduce the statistical power. Enrollment of more subjects would resolve this issue. Third, the pathology-imaging correlation is not clear, but we postulate that increased cortical thickness and subcortical gray matter volume is due to unpruned synapses. The exact pathological mechanism should be verified in future animal model studies. Fourth, we only enrolled male participants, so females must be included in future studies to fully understand DXM effects on brain development. Finally, we did not evaluate withdrawal symptoms in the present study. Evidences from a previous study showed that severity of opioid withdrawal correlated with local and remote cortical functional connectivity (Fingelkurts et al. 2007). Thus, potential effects of withdrawal symptoms may exist in the present study.
Conclusion
This is the first study to demonstrate the structural alternations in cortical and subcortical gray matter in DXM-dependent adolescents and young adults. DXM-dependent adolescents and young adults had increased cortical thickness of several brain regions and larger subcortical gray matter volume of the right thalamus and right pallidum. Increased cortical thickness of the DLPFC. L and PreCG. R correlated with the age of initial DXM use, and increased cortical thickness of the DLPFC. L also correlated with the BIS total scores. These findings provide novel insight into the impact of DXM on brain structural alternations in adolescents and young adults. Moreover, these findings may also provide targets for intervention methods or medical treatments that restore the abnormally thick regions to normal and potentially reduce symptoms or severity of addiction.
References
Alcaraz, F., Marchand, A. R., Vidal, E., Guillou, A., Faugère, A., Coutureau, E., & Wolff, M. (2015). Flexible use of predictive cues beyond the orbitofrontal cortex: role of the Submedius thalamic nucleus. The Journal of Neuroscience, 35, 13183–13193.
Alia-Klein, N., Parvaz, M. A., Woicik, P. A., Konova, A. B., Maloney, T., Shumay, E., Wang, R., Telang, F., Biegon, A., & Wang, G.-J. (2011). Gene × disease interaction on orbitofrontal gray matter in cocaine addiction. Archives of General Psychiatry, 68, 283–294.
Crews, F. T., Braun, C. J., Hoplight, B., Switzer, R. C., Knapp, D. J., & Darin, J. (2000). Binge ethanol consumption causes differential brain damage in young adolescent rats compared with adult rats. ALCOHOLISM-NEW YORK THEN BALTIMORE, 24, 1712–1723.
Darboe, M. N., Keenan Jr., G. R., & Richards, T. K. (1996). The abuse of dextromethorphan-based cough syrup: a pilot study of the community of Waynesboro, Pennsylvania. Adolescence, 31, 633.
De Bellis, M. D., Narasimhan, A., Thatcher, D. L., Keshavan, M. S., Soloff, P., & Clark, D. B. (2005). Prefrontal cortex, thalamus, and cerebellar volumes in adolescents and young adults with adolescent-onset alcohol use disorders and comorbid mental disorders. Alcoholism-clinical and experimental. Research, 29, 1590–1600.
Dong, G., DeVito, E., Huang, J., & Du, X. (2012). Diffusion tensor imaging reveals thalamus and posterior cingulate cortex abnormalities in internet gaming addicts. Journal of Psychiatric Research, 46, 1212–1216.
Filbey, F. M., Aslan, S., Calhoun, V. D., Spence, J. S., Damaraju, E., Caprihan, A., & Segall, J. (2014). Long-term effects of marijuana use on the brain. Proceedings of the National Academy of Sciences, 111, 16913–16918.
Fingelkurts, A. A., Fingelkurts, A. A., Kivisaari, R., Autti, T., Borisov, S., Puuskari, V., Jokela, O., & Kähkönen, S. (2007). Opioid withdrawal results in an increased local and remote functional connectivity at EEG alpha and beta frequency bands. Neuroscience Research, 58, 40–49.
Fischl, B., Sereno, M. I., & Dale, A. M. (1999a). Cortical surface-based analysis. II: inflation, flattening, and a surface-based coordinate system. NeuroImage, 9, 195–207.
Fischl, B., Sereno, M. I., Tootell, R. B., & Dale, A. M. (1999b). High-resolution intersubject averaging and a coordinate system for the cortical surface. Human Brain Mapping, 8, 272–284.
Gallinat, J., Meisenzahl, E., Jacobsen, L. K., Kalus, P., Bierbrauer, J., Kienast, T., Witthaus, H., Leopold, K., Seifert, F., & Schubert, F. (2006). Smoking and structural brain deficits: a volumetric MR investigation. European Journal of Neuroscience, 24, 1744–1750.
Giedd, J. N. (2004). Structural magnetic resonance imaging of the adolescent brain. Annals of the New York Academy of Sciences, 1021, 77–85.
Gogtay, N., Giedd, J. N., Lusk, L., Hayashi, K. M., Greenstein, D., Vaituzis, A. C., Nugent, T. F., Herman, D. H., Clasen, L. S., & Toga, A. W. (2004). Dynamic mapping of human cortical development during childhood through early adulthood. Proceedings of the National Academy of Sciences of the United States of America, 101, 8174–8179.
Goldstein, R. Z., Volkow, N. D. (2011). Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nature Reviews Neuroscience, 12, 652–669.
Han, X., Jovicich, J., Salat, D., van der Kouwe, A., Quinn, B., Czanner, S., Busa, E., Pacheco, J., Albert, M., & Killiany, R. (2006). Reliability of MRI-derived measurements of human cerebral cortical thickness: the effects of field strength, scanner upgrade and manufacturer. NeuroImage, 32, 180–194.
Han, D. H., Lyoo, I. K., & Renshaw, P. F. (2012). Differential regional gray matter volumes in patients with on-line game addiction and professional gamers. Journal of Psychiatric Research, 46, 507–515.
Jovicich, J., Czanner, S., Han, X., Salat, D., van der Kouwe, A., Quinn, B., Pacheco, J., Albert, M., Killiany, R., & Blacker, D. (2009). MRI-derived measurements of human subcortical, ventricular and intracranial brain volumes: reliability effects of scan sessions, acquisition sequences, data analyses, scanner upgrade, scanner vendors and field strengths. NeuroImage, 46, 177–192.
Kuhn, S., Gleich, T., Lorenz, R. C., Lindenberger, U., & Gallinat, J. (2014). Playing super Mario induces structural brain plasticity: gray matter changes resulting from training with a commercial video game. Molecular Psychiatry, 19, 265–271.
Li, M., Tian, J., Zhang, R., Qiu, Y., Wen, X., Ma, X., Wang, J., Xu, Y., Jiang, G., & Huang, R. (2014). Abnormal cortical thickness in heroin-dependent individuals. NeuroImage, 88, 295–307.
Makris, N., Gasic, G. P., Kennedy, D. N., Hodge, S. M., Kaiser, J. R., Lee, M. J., Kim, B. W., Blood, A. J., Evins, A. E., & Seidman, L. J. (2008). Cortical thickness abnormalities in cocaine addiction—a reflection of both drug use and a pre-existing disposition to drug abuse? Neuron, 60, 174–188.
Medina, K. L., Schweinsburg, A. D., Cohen-Zion, M., Nagel, B. J., & Tapert, S. F. (2007). Effects of alcohol and combined marijuana and alcohol use during adolescence on hippocampal volume and asymmetry. Neurotoxicology and Teratology, 29, 141–152.
Medina, K. L., McQueeny, T., Nagel, B. J., Hanson, K. L., Schweinsburg, A. D., & Tapert, S. F. (2008). Prefrontal cortex volumes in adolescents with alcohol use disorders: unique gender effects. Alcoholism: Clinical and Experimental Research, 32, 386–394.
Mesulam, M.-M. (2002). The human frontal lobes: Transcending the default mode through contingent encoding. Principles of Frontal Lobe Function, 8–30.
Mickiewicz, A. L., Dallimore, J. E., & Napier, T. C. (2009). The ventral pallidum is critically involved in the development and expression of morphine-induced sensitization. Neuropsychopharmacology, 34, 874–886.
Miller, S. (2005). Dextromethorphan psychosis, dependence and physical withdrawal. Addiction Biology, 10, 325–327.
Patton, J. H., Stanford, M. S., & Barratt, E. S. (1995). Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology, 51, 768–774.
Qiu, Y. W., Jiang, G. H., Su, H. H., Lv, X. F., Tian, J. Z., Li, L. M., & Zhuo, F. Z. (2013). The impulsivity behavior is correlated with prefrontal cortex gray matter volume reduction in heroin-dependent individuals. Neuroscience Letters, 538, 43–48.
Qiu, Y. W., Lv, X. F., Jiang, G. H., Su, H. H., Yu, T., Tian, J. Z., Zhang, X. L., & Zhuo, F. Z. (2014). Reduced ventral medial prefrontal cortex (vmPFC) volume and impaired vmPFC-default mode network integration in codeine-containing cough syrups users. Drug and Alcohol Dependence, 134, 314–321.
Qiu, Y. W., Su, H. H., Lv, X. F., & Jiang, G. H. (2015). Abnormal white matter integrity in chronic users of codeine-containing cough syrups: a tract-based spatial statistics study. AJNR. American Journal of Neuroradiology, 36, 50–56.
Reid, A. G., Daglish, M. R., Kempton, M. J., Williams, T. M., Watson, B., Nutt, D. J., & Lingford-Hughes, A. R. (2008). Reduced thalamic grey matter volume in opioid dependence is influenced by degree of alcohol use: a voxel-based morphometry study. Journal of Psychopharmacology, 22, 7–10.
Russell, R. W. R. (1968). Regional development of the brain in early life. Proceedings of the Royal Society of Medicine, 61, 326–326.
Smolker, H., Depue, B., Reineberg, A., Orr, J., & Banich, M. (2014). Individual differences in regional prefrontal gray matter morphometry and fractional anisotropy are associated with different constructs of executive function. Brain Structure and Function, 220, 1291–1306.
Sowell, E. R., Thompson, P. M., Holmes, C. J., Jernigan, T. L., & Toga, A. W. (1999). In vivo evidence for post-adolescent brain maturation in frontal and striatal regions. Nature Neuroscience, 2, 859–861.
Spear, L. P. (2002). Alcohol’s effects on adolescents. Alcohol Research and Health, 26, 287–291.
Squeglia, L. M., Jacobus, J., & Tapert, S. F. (2009). The Influence of Substance Use on Adolescent Brain Development. Clinical EEG and Neuroscience : Official Journal of the EEG and Clinical Neuroscience Society (ENCS), 40, 31–38.
Walton, M. E., Behrens, T. E., Buckley, M. J., Rudebeck, P. H., & Rushworth, M. F. (2010). Separable learning systems in the macaque brain and the role of orbitofrontal cortex in contingent learning. Neuron, 65, 927–939.
Wu, Q., Yu, J., Yang, C., Chen, J., Yang, L., Zhang, H., Teng, S., Li, J., Yan, D., Cao, J., Zhao, Y., & Wang, Z. (2016). Nonmedical use of cough syrup among secondary vocational school students: a National Survey in China. Medicine, 95, e2969.
Yao, S., Yang, H., Zhu, X., Auerbach, R. P., Abela, J. R., Pulleyblank, R. W., & Tong, X. (2007). An examination of the psychometric properties of the Chinese version of the Barratt Impulsiveness Scale, 11th version in a sample of Chinese adolescents. Perceptual and Motor Skills, 104, 1169–1182.
Yuan, K., Cheng, P., Dong, T., Bi, Y., Xing, L., Yu, D., Zhao, L., Dong, M., von Deneen, K. M., & Liu, Y. (2013). Cortical thickness abnormalities in late adolescence with online gaming addiction. PloS One, 8, e53055.
Yücel, M., Solowij, N., Respondek, C., Whittle, S., Fornito, A., Pantelis, C., & Lubman, D. I. (2008). Regional brain abnormalities associated with long-term heavy cannabis use. Archives of General Psychiatry, 65, 694–701.
Acknowledgments
This work was supported by grants from the Natural Scientific Foundation of China (Grant No. 81201084, 81560283), and the Natural Scientific Foundation of Jiangxi Province, China (Grant No. 20151BAB205049). We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no financial interests or potential conflicts of interest.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, and the applicable revisions at the time of the investigation.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Electronic supplementary material
ESM 1
(DOCX 775 kb)
Rights and permissions
About this article
Cite this article
Qiu, Yw., Lv, Xf., Jiang, Gh. et al. Potential gray matter unpruned in adolescents and young adults dependent on dextromethorphan-containing cough syrups: evidence from cortical and subcortical study. Brain Imaging and Behavior 11, 1470–1478 (2017). https://doi.org/10.1007/s11682-016-9628-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-016-9628-0