Abstract
Objectives
To evaluate right ventricle (RV) function by coronary computed tomography angiography (CTA) using a novel automated three-dimensional (3D) RV volume segmentation tool in comparison with clinical reference modalities.
Methods
Twenty-six patients with severe end-stage heart failure [left ventricle (LV) ejection fraction (EF) <35%] referred to CTA were enrolled. A specific individually tailored biphasic contrast agent injection protocol was designed (80%/20% high/low flow) was designed. Measurement of RV function [EF, end-diastolic volume (EDV), end-systolic volume (ESV)] by CTA was compared with tricuspid annular plane systolic excursion (TAPSE) by transthoracic echocardiography (TTE) and right heart invasive catheterisation (IC).
Results
Automated 3D RV volume segmentation was successful in 26 (100%) patients. Read-out time was 3 min 33 s (range, 1 min 50s–4 min 33s). RV EF by CTA was stronger correlated with right atrial pressure (RAP) by IC (r = -0.595; p = 0.006) but weaker with TAPSE (r = 0.366, p = 0.94). When comparing TAPSE with RAP by IC (r = -0.317, p = 0.231), a weak-to-moderate non-significant inverse correlation was found. Interobserver correlation was high with r = 0.96 (p < 0.001), r = 0.86 (p < 0.001) and r = 0.72 (p = 0.001) for RV EDV, ESV and EF, respectively. CT attenuation of the right atrium (RA) and right ventricle (RV) was 196.9 ± 75.3 and 217.5 ± 76.1 HU, respectively.
Conclusions
Measurement of RV function by CTA using a novel 3D volumetric segmentation tool is fast and reliable by applying a dedicated biphasic injection protocol. The RV EF from CTA is a closer surrogate of RAP than TAPSE by TTE.
Key Points
• Evaluation of RV function by cardiac CTA by using a novel 3D volume segmentation tool is fast and reliable.
• A biphasic contrast agent injection protocol ensures homogenous RV contrast attenuation.
• Cardiac CT is a valuable alternative modality to CMR for the evaluation of RV function.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Right ventricular (RV) function is a key parameter for management of patients with severe heart failure, especially if scheduled for heart transplantation, artificial heart implantation or other novel valvular devices such as percutaneous tricuspid valves (e.g. CorMatrix® by Aziyo Biologics, Richmond, CA, USA).
In clinical practice, the severity of RV dysfunction is estimated from a variety of surrogate parameters obtained from transthoracic echocardiography (TTE), including tricuspid annular plane systolic excursion (TAPSE), which reflects the magnitude of movement of the tricuspid annulus between end-diastole and end-systole [1]. Further TTE parameters comprise the fractional area change (FAC), right ventricular contraction pressure index (RVCPI), defined as TAPSE × tricuspid regurgitation, the estimated right atrial pressure (eRAP) [2] and the TEI index [3].
Invasive right heart invasive catheterisation (IC) is the reference standard for accurate measurement of right ventricular and atrial pressure load. Given its invasive nature and associated risks, an accurate and non-invasive technique for estimating RV pressure would be desirable.
Cardiac magnetic resonance imaging (CMR) is a valuable non-invasive tool for the assessment of RV volumes and function. However, in patients with severe heart failure non-CMR compatible cardiac devices such as cardiac pacemakers are frequently implanted. In contrast, ECG-gated computed tomography (CT) does not preclude such patients. Studies utilising CT for assessment of RV function and volume are scarce but have shown a good correlation between CT and CMR [4,5,6], respectively.
Imaging the RV by CT is challenging. Accurate measurement of RV function requires a homogenous contrast attenuation of the RV to ensure precise contour tracing and the separation of the RV cavity from the myocardium. Homogenous attenuation of the right chambers by CT angiography (CTA) is difficult to obtain to due beam hardening, streak and flow-related artefacts resulting from mixing of high-attenuation contrast agent from the superior vena cava with unenhanced blood from the inferior vena cava. Precise injection inflow and contrast volume timing is necessary in order to ensure homogenous attenuation of the RV, and there is lack of consensus on which protocol performs best—both biphasic and triphasic injection protocols have been proposed [7, 8].
Therefore, the primary aim of our study was to evaluate measurement of RV function by CT using a novel, automated 3D RV volume segmentation tool and by using a dedicated biphasic “personalised” (individually tailored) contrast injection protocol. Our second major aim was to validate CT in comparison with the other clinical reference modalities such as TTE (TAPSE) and invasive right atrial pressure (RAP) by IC.
Methods and materials
Study population
Twenty-six patients [58.0 ± 13.6 years (mean ± SD), 11.5% females] with severe end-stage heart failure (LV EF <35%), referred to coronary CT angiography (CTA) for clinical indications were enrolled into this retrospective study. Ischaemic cardiomyopathy (CMP), n = 10; non-ischaemic dilated CMP, n = 9; hypertrophic obstructive cardiomyopathy (HOCM), n = 1; severe valvular heart disease causing ventricular dilatation and heart failure, n = 2; arrhythmogenic right ventricular dysplasia (ARVD), n = 1; mixed CMP (HOCM/ischaemic CMP/ toxic), n = 2; CMP caused by scleroderma, n = 1.
Clinical indications for cardiac CT were: patients were listed either for evaluation prior to heart transplantation (HTX), artificial ventricular assist devices (VAD) or scheduled for transcatheter tricuspid valve intervention, or the assessment of RV function was required for other clinical management decisions (e.g. medication), or coronary artery disease.
Cardiac CTA was compared with right heart invasive catheterisation (IC) and TTE. All examinations were performed within 2 weeks.
Cardiac computed tomography angiography (CTA)
A 128-slice dual source CT (Somatom Definition FLASHTM; Siemens Healthineers, Erlangen, Germany) scanner was used with the following scan parameters: 2 × 64 × 0.6 mm detector collimation, rotation time 0.28 s. Tube voltage settings were adapted to body mass index (BMI) (80 kV < 20 BMI, 100kV < 25 BMI, 120 kV > 25 BMI kg/m2, and 140 kV if > BMI 35). Based on the patient’s individual heart rate, ECG-gating in retrospective spiral (pitch, 0.2-0.5) or, if heart rate was regular and <80 bpm, sequential prospective dual-step ECG-gated mode was applied. [9]
Axial images were reconstructed with 1 mm slice width (increment 0.7), a smooth-medium kernel and at every 5% increments of R-to-R interval during one entire cardiac cycle for the creation of a multiphase dataset.
A biphasic iodine contrast agent (370 mg/ml iodine concentration) injection protocol was designed (Iopromide, Ultravist 370™; Bayer Healthcare, Leverkusen, Germany):
-
1.
The total contrast volume was split into 80% at a high-flow of 5 ml/s and 20% at reduced flow of 3.5 ml/s, followed by a saline solution chaser of 30 ml at 3.5 ml/s.
-
2.
Total contrast agent volume ranged between 80 to 110 ml and was calculated mainly depending on the patient’s body weight (<65 kg = 80 ml; 65-85 kg = 90 ml; 85-105 kg = 100 ml; >105 kg = 110 ml).
The iodine contrast agent was triggered into arterial phase by using automated bolus tracking, after reaching a 100 HU threshold in the ascending aorta.
Exclusion criteria for CTA were: renal dysfunction (serum GFR <30 ml/min/1.73 m2), iodine allergy without pre-medication, hyperthyroidism and pregnancy.
Image analysis
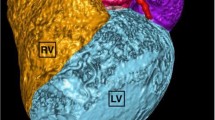
Image analyses were performed with dedicated automated server-based software (SyngoVIATM; Siemens Healthineers) using the CT Cardiac Workflow, which allows RV- function measurements. The RV was segmented automatically using 3D segmentation of the blood volume of the RV while sparing the RV myocardium, myocardial trabecula and the moderator band. RV outer contours were further defined by tricuspid valve and pulmonary valve level until to the apex (Fig.1). The software created a volume dataset for each phase at 5 % increments. The maximal end-systolic and end-diastolic volumes were selected automatically. RV contours were adjusted manually if deemed inaccurate and aligned with the inner contour of the RV blood pool volume and/or adjusted to tricuspid or pulmonary valve level, or the RV myocardial trabecula.
Automated right ventricular (RV) 3D volume segmentation by CTA (SyngoVIA; Siemens Healthineers). Yellow contours denote the inner RV volume delineation, which was extracted automatically. Minor adaptions of the yellow lines are feasible manually, to ensure correct tracing of irregular RV morphology and myocardial trabecula. Table upper right shows right ventricular ejection fraction (RV-EF), end-diastolic volume (EDV) and end-systolic volume (ESV), which were calculated based on the individual selection of the smallest ESV and largest EDV
The RV function parameters of ejection fraction (EF), end-diastolic volume (EDV) and end-systolic volume (ESV) were calculated by two observers [one with 10 years of cardiac CT experience and one with less (>6 months) experience]. RF EF was computed automatically based on automated selection of the smallest ESV and largest EDV during the entire cardiac cycle (RR interval).
The time for image analysis was recorded for one of the two observers, from uploading the patient dataset into the CT Cardiac Workflow, until the completion of the final results. After automated RV volume segmentation was completed, the contours of the RV were reviewed for alignment. The inner RV contours were adjusted manually by both observers if deemed inaccurate. Then, the final results of the RV function analysis (Table 1) were recorded and then, the “total read out time” was recorded. (Time from uploading images until results.)
CTA image quality analysis
-
1.
CTA image quality of the RV and right atrium (RA) was rated as sufficient for 3D volume segmentation with “yes” or “no”.
-
2.
Qualitative CTA analysis: image quality was graded subjectively for the presence of streak/flow-mixing artefacts in the RA and RV as 5 = no artefacts, homogenous enhancement; 4 = minimal artefacts, homogenous enhancement; 3 = moderate artefacts, relatively homogenous; 2 = severe artefacts, inhomogeneous; 1 = very severe artefacts, inhomogeneous/insufficient for segmentation.
-
3.
Quantitative CTA analysis (Fig. 2): assessment of RV and RA enhancement was performed by placing a region of interest (ROI) during end-diastolic phase, chosen as large as possible and by avoiding inclusion of papillary muscles, myocardial walls, or the tricuspid valve apparatus, on axial slices into the RV and RA. The CT attenuation values (HU) and image noise (SD of HU) were recorded.
Transthoracic echocardiography (TTE)
All measurements were performed using a sonography unit (Sequoia 256, Acuson; Siemens Healthineers) equipped with a 3.5- to 1.75-MHz transducer by experienced observers.
In a four-chamber view, the tricuspid annular plane systolic excursion (TAPSE)—defined as the amount of longitudinal displacement of the annulus at peak systole in apical direction—was measured, using an M-mode cursor passed through the tricuspid lateral annulus.
The severity of tricuspid regurgitation was classified semi-quantitatively according to the report of the American Society of Echocardiography as grade 1–3 (i.e. mild, moderate or severe, respectively) by jet-length, width and area according to ASE [10], and optionally by incorporating the PISA method.
Invasive right-heart catheterisation (IC)
Right heart catheterisation was performed in a dedicated interventional angiography suite by advancing the intravascular guidewire to the right atrium through a puncture of a central or peripheral vein. By using a Swan-Ganz catheter, right atrial pressures (RAP) were measured and the mean calculated. The cardiac output was measured by thermodilution.
Statistical analysis
Statistical analysis was performed using SSPS™ software (V17.0; SPSS, Chicago, IL,USA) and MedCalc® (V12.5; MedCalc Software, Mariakerke, Belgium). Quantitative variables are expressed as the mean ± standard deviation (SD), whereas categorical variables are presented as the absolute value and percentage. Correlation coefficients were determined with linear regression analysis and plots were created, and the Pearson correlation coefficient calculated. A p value of less than 0.05 was considered as significant.
Results
Assessment of RV function by CTA
Automated RV 3D volume segmentation was successful completed in 26 of 26 (100%) study patients, and after checking the segmentation results, major manual RV contour edits were not necessary in 24 of 26 (92.3%) patients, with only minor adjustments done occasionally. Ten subjects (38.5 %) had undergone previous RV pacemaker implantation.
Qualitative RA and RV image quality results are shown in Table 2 and quantitative results in Table 3.
Interobserver correlation was high, r = 0.956 (p < 0.001), r = 0.86 (p < 0.001) and r = 0.72 (p = 0.001) for RV EDV, ESV and EF, respectively.
CT attenuation of the right atrium (RA) and RV was 196.9 HU ± 75.3 and 217.5 HU ± 76.1, respectively.
Total read-out time (including image post-processing and RV function parameter calculation) was mean 3 min 33 s (range, 1 min 50 s–4 min 33 s).
Correlation of RV-function by cardiac CTA compared to TTE and invasive right heart catheter (IC) (Table 4)
Figure 3 shows that RV EF by CT was strongest and significantly correlated with right atrial pressure (RAP) by IC (r = -0.595; p = 0.006). A weaker but positive correlation between RV EF by CT and TAPSE by TTE (r = 0.366; p = 0.94) was found.
When comparing TAPSE by TTE with RAP by IC (r = -0.317; p = 0.231), similarly, a weak-to-moderate non-significant negative correlation was found (Fig. 4).
The correlation of RV-EDV with TAPSE was not significant (r = 0.07; p = 0.734).
The cardiac index (CI) was not correlated with RV-EF by CT (r = 0.04, p = 0.087) (mean, 2.86 ± 0.37; range, 1.2-2.8).
Severity of tricuspid regurgitation (TR) by TTE was inversely moderately correlated with RV EF by CT (r = -0.44; p = 0.04) and stronger correlated with RAP (r = 0.58; p = 0.02), while TAPSE compared to TR was weaker and non-significant (r = 0.292; p = 0.199).
The majority of patients had moderate-to-severe TR (moderate, n = 11, severe TR, n = 13, mild or minimal, n = 2).
Creatinine values were 1.3 ± 0.38 SD mg/dl (range, 0.55–2.22 mg/dl).
Table 1 shows the RV function parameters by CT, TTE and RAP by IC. LV-EF in our cohort was mean 24.5% (range, 13–34%).
Discussion
Our study shows that evaluation of RV function by cardiac CTA in clinical practice using a fully automate 3D RV volume segmentation approach is fast (within approximately 3 min) and reliable. Our dedicated biphasic contrast agent injection protocol (80%/20%, adjusted to body weight) ensured homogenous RV contrast attenuation and automated RV volume segmentation.
While sufficient enhancement of the left heart chambers by CTA is commonly obtained using a monophasic contrast agent injection protocol, as recommended for coronary CTA [11], this protocol frequently results in lack of RV contrast attenuation (“RV washout”). Consecutively, a weak or absent delineation of the myocardial septum from the RV occurs in up to 25% [12] or above. Other studies utilised a similar (70:30%) contrast agent mixing protocol [13]. Vrachioloitis et al. [14] applied a fixed volume of 130 mL (100 mL at 5 mL/s and 30 mL at 3 mL/s) for a triple-rule-out scan protocol [15]. Litmanovitch et al. [16] employed a triphasic protocol (50 ml contrast, 50 ml 60% contrast/saline and 30 ml normal saline) for the comprehensive evaluation of lungs, aorta, pulmonary and the coronary arteries.
Our protocol is also appropriate for the planning of transcatheter or minimal invasive tricuspid valve intervention, or other interventional procedures requiring a morphological assessment of the RV, e.g. right atrial catheter ablation (isthmus), or other indications for CTA requiring a delineation of the interventricular myocardium septum such as the evaluation of patients with asymmetric midventricular hypertrophic CMP for planning of myomectomy. Further, in patients with suspected arrhythmogenic right ventricular dysfunction (ARVD), CT serves as a valuable alternative modality to CMR if non-CMR compatible pacemakers are implanted. Furthermore, patients with unclear cardiac masses in the right heart may undergo CT for further evaluation. Beyond, our protocol is also suitable for acute chest pain evaluation (triple rule protocol [14,15,16,17,18]) and the evaluation of CT myocardial perfusion [16, 19, 20], which relies as well on the delineation of the interventricular myocardial septum.
Since the morphology of the RV is complex, multitrabecular and irregular, multiple time-consuming manual contour edits are usually required when using currently commercially available post-processing techniques, resulting in tedious long readout times of up to 30 min.
Thus, we explored a novel 3D RV segmentation tool which permits fast automated RV segmentation from a CTA dataset without extensive manual contour tracking edits by the observer. This technique is highly efficient and saves valuable time. Manual RV contour edits were necessary in only minority of patients and quickly performed, and despite minor inaccuracies (see Fig. 1), the correlation was good.
Second, our study showed that RV EF by CT is a closer surrogate of right atrial pressure than TAPSE by TTE; the RV EF provides the clinical heart failure team a valuable supportive non-invasive parameter for clinical and therapeutic decision-making in patients with severe end-stage heart failure and avoids the burden of repeating an invasive procedure.
Such indications include follow-up exams for monitoring of RV dysfunction under medication in terms of treatment response and dose adjustments, or clinical management decision-making in terms of defining a patient’s appropriateness for novel artificial heart systems—ventricular assist device (VAD) versus the final decision of scheduling heart transplantation.
CTA could be also applied in patients, in which the evaluation of RV function with TAPSE by TTE is technically limited or inappropriate, such as in those after surgical tricuspid valve reconstruction.
We acknowledge the following study limitations. Our cohort comprises a relatively small sample size of patients with various aetiologies of end-stage severe heart failure and moderate-to-severe tricuspid valve regurgitation. Further, the application of an iodine contrast agent may be contraindicated if severe renal dysfunction is present.
Finally, we would like to emphasise that our study consisted of patients with end-stage heart failure; therefore, total contrast volume was kept as low as possible to prevent a further decline of kidney function [21].
Conclusions
Measurement of RV function by CTA using an automated 3D RV volume segmentation tool and our dedicated contrast flow injection protocol is reliable in clinical practice, with short readout times. Second, RV EF by CTA is a more accurate non-invasive surrogate parameter for invasive right atrial pressure (RAP) than TAPSE obtained by TTE.
In summary, CT is a useful alternative non-invasive modality to CMR in patients with end-stage heart failure, and CTA offers the advantage of simultaneous coronary artery disease evaluation.
Abbreviations
- ARVD:
-
Arrhythmogenic right ventricular dysfunction
- CMP:
-
Cardiomyopathy
- EDV:
-
End-diastolic volume
- EF:
-
Ejection fraction
- ESV:
-
End-systolic volume
- LV:
-
Left ventricle
- PASP:
-
Pulmonary artery systolic pressure
- RAP:
-
Right atrial pressure
- rIC:
-
Right heart invasive catheterisation
- RA:
-
Right atrium
- RV:
-
Right ventricle
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TTE:
-
Transthoracic echocardiogram
- TR:
-
Tricuspid regurgitation
- VAD:
-
Ventricular assist device
References
Rudski LG, Lai WW, Afilalo J et al (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713
Frea S, Pidello S, Bovolo V et al (2016) Prognostic incremental role of right ventricular function in acute decompensation of advanced chronic heart failure. Eur J Heart Fail 18:564-572
Guazzi M, Bandera F, Pelissero G et al (2013) Tricuspid annular plane systolic excursion and pulmonary arterial systolic pressure relationship in heart failure: an index of right ventricular contractile function and prognosis. Am J Physiol Heart Circ Physiol 305:H1373–H1381
Guo YK, Gao HL, Zhang XC, Wang QL, Yang ZG, Ma ES (2010) Accuracy and reproducibility of assessing right ventricular function with 64-section multi-detector row CT: comparison with magnetic resonance imaging. Int J Cardiol 139:254–262
Maffei E, Messalli G, Martini C et al (2012) Left and right ventricle assessment with cardiac CT: validation study vs. cardiac MR. Eur Radiol 22:1041–1049
Lembcke A, Dohmen PM, Dewey M et al (2005) Multislice computed tomography for preoperative evaluation of right ventricular volumes and function: comparison with magnetic resonance imaging. Ann Thorac Surg 79:1344–1351
Saremi F, Ho SY, Cabrera JA, Sanchez-Quintana D (2013) Right ventricular outflow tract imaging with CT and MRI: Part 1, Morphology. AJR Am J Roentgenol 200(1):W39–W50
Saremi F, Hassani C, Millan-Nunez V, Sanchez-Quintana D (2015) Imaging evaluation of tricuspid valve: analysis of morphology and function with CT and MRI. AJR Am J Roentgenol 204:W531–W542
Feuchtner G, Goetti R, Plass A et al (2010) Dual-step prospective ECG-triggered 128-slice dual-source CT for evaluation of coronary arteries and cardiac function without heart rate control: a technical note. Eur Radiol 20:2092–2099
Zoghbi WA, Enriquez-Sarano M, Foster E et al (2003) Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and doppler echocardiography. J Am Soc Echocardiogr 16:777–802
Cademartiri F, Luccichenti G, Marano R, Gualerzi M, Brambilla L, Coruzzi P (2004) Comparison of monophasic vs biphasic administration of contrast material in non-invasive coronary angiography using a 16-row multislice computed tomography. Radiol Med 107:489-496
Raman SV, Shah M, McCarthy B, Garcia A, Ferketich AK (2006) Multi-detector row cardiac computed tomography accurately quantifies right and left ventricular size and function compared with cardiac magnetic resonance. Am Heart J 151:736–744
Kerl JM, Ravenel JG, Nguyen SA et al (2008) Right heart: split-bolus injection of diluted contrast medium for visualization at coronary CT angiography 1. Radiology 247:356–364
Vrachliotis TG, Bis KG, Haidary A et al (2007) Atypical chest pain: coronary, aortic, and pulmonary vasculature enhancement at biphasic single-injection 64-section CT angiography. Radiology 243:368–376
Haidary A, Bis K, Vrachiolitis T, Kosuri R, Balasubramaniam M (2007) Enhancement performance of a 64-slice triple rule-out protocol vs 16-slice and 10-slice multidetector CT-angiography protocols for evaluation of aortic and pulmonary vasculature. J Comput Assist Tomogr 31:917–923
Litmanovitch D, Zamboni GA, Hauser TH et al (2008) ECG-gated chest CT angiography with 64-MDCT and tri-phasic IV contrast administration regimen in patients with acute non-specific chest pain. Eur Radiol 18:308–317
Dedic A, Lubbers MM, Schaap J et al (2016) Coronary CT angiography for suspected ACS in the era of high-sensitivity troponins: randomized multicenter study. J Am Coll Cardiol 67:16–26
Hulten E, Pickett C, Bittencourt MS et al (2013) Outcomes after coronary computed tomography angiography in the emergency department: a systematic review and meta-analysis of randomized, controlled trials. Am Coll Cardiol 61:880–892
Cannaò PM, Schoepf UJ, Muscogiuri G et al (2015) Technical prerequisites and imaging protocols for dynamic and dual energy myocardial perfusion imaging. Eur J Radiol 84:2401–2410
Feuchtner GM, Plank F, Pena C et al (2012) Evaluation of myocardial CT perfusion in patients presenting with acute chest pain to the emergency department: comparison with SPECT-myocardial perfusion imaging. Heart 98:1510–1517
Subramaniam RM, Suarez-Cuervo C, Wilson RF et al (2016) Effectiveness of prevention strategies for contrast-induced nephropathy: a systematic review and meta-analysis. Ann Intern Med 164:406–416
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Ao.Univ.-Prof. Dr. Gudrun Feuchtner.
Conflict of interest
The authors of this manuscript declare relationships with the following companies: Gudrun M. Feuchtner—research collaboration with Siemens, SyngoVIA; no financial, no grant.
Statistics and biometry
One of the authors has significant statistical expertise.
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was not required because of specific regulations for retrospective studies in Innsbruck, Austria.
Methodology
• retrospective
• diagnostic study
• performed at one institution
Rights and permissions
About this article
Cite this article
Burghard, P., Plank, F., Beyer, C. et al. Evaluation of right ventricular function by coronary computed tomography angiography using a novel automated 3D right ventricle volume segmentation approach: a validation study. Eur Radiol 28, 5129–5136 (2018). https://doi.org/10.1007/s00330-018-5523-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5523-y