Abstract
The purpose of this study was to evaluate chest CTA protocol using retrospective ECG-gating and triphasic IV contrast regimen for comprehensive evaluation of patients with acute non-specific chest pain. ECG-triggered dose modulation was used with a 64-MDCT scanner in 56 non-critically ill patients with acute nonspecific chest pain using triphasic IV regimen: 50 ml contrast followed by 50 ml 60% contrast/saline and 30 ml normal saline. Lungs, aorta, pulmonary and coronary arteries were graded on a 5-point scale (5, best). Aorta and pulmonary artery attenuation was measured and three coronary artery groups were evaluated. Comparison with invasive coronary angiography was obtained in nine patients on a per segment (16 total) basis. Dosimetry values were obtained. Studies were satisfactory in all patients (score >3). Aorta and pulmonary artery attenuation was >200 HU in 90.5%. Lung or pleura, non-cardiac vascular and coronary arteries disease were detected in 20, 11 and 16 patients, respectively. Median coronary angiography (grade 5) was significantly higher than acceptable for diagnosis grade 4 (p < 0.001). Per segment, weighted kappa statistic was 0.79 indicating substantial agreement with catheter angiography (p<0.001). Average DLP was 1,490 ± 412 mGy-cm. Gated 64-MDCT angiography with triphasic IV contrast is a robust multipurpose technique for patients with acute non-specific chest pain.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In patients with chest pain, scanning CT protocols vary to facilitate visualization of various major vascular components in the chest, such as pulmonary arteries, aorta or coronary arteries and their branches. However, precise differentiation of chest pain etiology based only on clinical signs is not always clear-cut due to non-vascular or vascular factors such as pneumonia, pleural or chest wall problems, aortic dissection, pulmonary embolism and coronary artery disease [1]. For these cases, an inclusive protocol is needed, and if evaluation of the coronary arteries is to be included, ECG gating is essential. ECG gating has also been shown to improve quality by reducing artifacts of the thoracic aorta and improving visualization of pulmonary vessels and parenchyma [2–5].
Disadvantages of ECG gating include an increase in scan time and higher radiation exposure [6, 7]. Thinner collimation and higher tube power used by 64 MDCT may cause an even higher radiation dose. Decreasing the tube current during the systolic phase (ECG pulsing) has been shown to reduce exposure by up to 50% depending on patient heart rate [8]. Low kilovoltage setting in slim and pediatric populations has the potential to reduce exposure even more [9, 10] and can be obtained with 64-slice CT technology in routine clinical practice [11].
We have been using a retrospective ECG-gated CTA protocol for the evaluation of thoracic aorta in patients with suspected aortic dissection and in emergency department (ED) patients with non-specific chest pain, in whom dissection was a possibility [2]. Using 16-row MDCT the image quality of the aorta, pulmonary arteries and the lungs was satisfactory, but there was a large number of suboptimal or non-interpretable coronary artery results [12]. With the installation of a 64-row MDCT in our ED and bi-phasic IV contrast injection regimen evaluation of coronary arteries improved. However, this did not achieve the desired clearance of contrast from the superior vena cava (SVC) and right heart in the presence of maximum contrast opacification of the pulmonary arteries and left heart, coronary tree and aorta [12].
The purpose of this study is to evaluate a chest CTA protocol using retrospective ECG-gating on 64-row MDCT with ECG pulsing and triphasic IV contrast injection regimen for comprehensive evaluation of ED patients with acute non-specific chest pain including assessment of parenchymal and vascular abnormalities involving the pulmonary arteries, the thoracic aorta and the coronary arteries.
Materials and methods
Patient selection
Starting from December 2005, ECG-gated chest CTA done with 64-row MDCT was offered as a clinical chest CTA protocol to patients with acute chest pain with normal or inconclusive ECG and negative initial cardiac enzymes. Other available chest pain CTA protocols included specific protocols for pulmonary embolism, aortic dissection and non-specific chest pain CTA. We used a previous clinical scanning protocol based on 16-row MDCT and adapted it for the 64-row scanner. Review of the results performed initially for quality assurance purposes and analysis of the study data were performed after approval by our Institutional Review Board (IRB) and was conducted in compliance with the Health Insurance Portability and Accountability Act (HIPAA) guidelines. Informed consent was waived by IRB as this was a clinical diagnostic protocol. Patients with no suspected acute myocardial infarction or definite angina pectoris were selected. Further selection criteria were limited by time: patients referred from our Emergency Department (ED) between 8 am and 3 pm on weekdays. An age limitation was also set (50 to 80 years old) as the prevalence of coronary disease is low under age 50. However, if an aortic dissection was clinically suspected, patients younger than 50 years old (four in this series) were included to evaluate the origin of the coronary arteries and rule out type A dissection. Patients with tachypnea, tachycardia greater than 100 beats per minute (bpm), high clinical suspicion for pulmonary embolism or those with contraindications for receiving beta-blockers were excluded. Other exclusion criteria were cardiac arrhythmia of any sort, pacemaker, compromised renal function and allergies to contrast media. Using the above criteria 56 patients were selected (see “Results”). The ED physician ordered chest CTA in each case as part of the conventional workup, and this was done early in the clinical evaluation of the patient in the interval after the ECG and blood samples were done and before a final diagnosis or patient disposition was made. For radiation dose comparisons, two control groups were used: one group of 56 patients undergoing non-gated chest CTA and a second group of 12 patients undergoing non-ECG-dose modulated coronary CTA.
Scanning technique protocol
The following protocol was adapted for 64-row MDCT:
Patient preparation
For patients not already on a beta-block regimen (either through their regular medications or as a part of ED treatment) administration of beta blockade started once eligibility for ECG gating was established and provided that the pulse rate was greater than 65 bpm and the systolic blood pressure was not lower than 110 mmHg. Patients were given 50 mg metoprolol, orally, to decrease the pulse rate by the time of the scan (usually 45–60 min later, which in our practice is an average delay between the request for chest CTA and the start of the scan). If scanning was required to be done sooner and the pulse rate was greater than 65 bpm, intravenous beta blocking was administered on the CT table immediately before the exam: 5 mg every 5 min up to a total of 25 mg. ECG-gating protocol was aborted if pulse rate did not drop below 72 bpm.
IV contrast timing and injection
To maximally opacify the pulmonary arteries, aorta and coronary arteries with minimal IV contrast remaining in the superior vena cava and right ventricle, exact timing is required as the scanning temporal window is very narrow. Using a dual-head power injector (Stellant, Medrad, Indianola, PA) a test IV bolus determined the scanning delay, and a tri-phasic injection of IV contrast was used for data collection. A test IV bolus of 25 ml of contrast agent was followed by 20 ml of normal saline flush at a rate of 4.5 ml/s. The delay was determined by temporal monitoring, with low dose, 50 mA, technique, of the attenuation of the pulmonary artery, ascending and descending aorta. Scan delay was calculated as time to peak at the ascending aorta +2 s or at the descending aorta at the level of the main pulmonary artery. Chest CT angiography was performed with a tri-phasic consecutive injection sequence beginning with 50 ml nonionic IV contrast material (Optiray 350, Mallinckrodt, St. Louis, MO) injected at a rate of 4.5 ml followed by 50 ml of a mixture of 60% contrast and normal saline and ended with a 30-ml flush of normal saline. If the pulmonary artery to descending aorta time was greater than 8 s, an additional 20 ml IV contrast was used for the exam (consisting of 10 ml full strength and 10 ml 60% dilution). Contrast was injected through an 18- to 20-gauge angiocatheter in an antecubital vein.
This regimen was adapted to create a tight contrast column based on a 9-s scan duration. Rather than organ enhancement, we sought full contrast opacification of pulmonary vessels, aorta and coronary arteries combined with unenhanced blood in the superior vena cava and right heart as our goal of CT angiography.
Data acquisition
A 64-MDCT scanner (Lightspeed VCT, General Electric Healthcare Technologies, Milwaukee, WI) was used in the ED. Scanning started at the level of the thoracic inlet and continued to below the diaphragm (Fig. 1). The following imaging and reconstruction parameters were applied: data acquisition collimation 0.625 mm ×64=4 cm; 140 kVp; 300–600 mAs; pitch 0.18–0.24 (depending on heart rate); rotation time 0.35 s; slice width 0.625 mm; field of view 50 cm; matrix 512×512. Overall the scanning time for the whole chest was less than 9 s, with variations depending on patient size and heart rate.
ECG-gated chest CTA of a 58-year-old man with atypical chest pain. Volume rendering shows span of scan from the thoracic inlet to the cardiac apex that includes the origins of the brachiocephalic vessels, the thoracic aorta, pulmonary arteries, heart and lungs. There are no motion artifacts in the ascending aorta or pulmonary artery. LAD (arrow) and LCx (arrowhead) arteries are clearly seen with the obtuse marginal crossing over the mid LCx (asterisk)
ECG-triggered dose modulation was applied in each case with 400–600 mA in 60–80% R-R interval and 250–350 mA for the rest of the cardiac cycle (81% to 59% of the next cycle). A report of the radiation dose, with volume Computed Tomography Dose Index (CTDIvol) measured in mGy and dose-length product (DLP) measured in mGy-cm, was provided by the scanner for every case and stored in PACS.
Study display protocol
Chest, pulmonary arteries and aorta
Axial, coronal and sagittal images of the chest were reconstructed using soft-tissue algorithm to evaluate pulmonary arteries, aorta and lung parenchyma at 2.5-mm slice thickness and sent to PACS. The images were then interpreted using appropriate window settings for soft tissues, vessels and lung.
Heart and coronary arteries
Retrospective gating was applied to the heart images. Cardiac data were reconstructed at 60%, 65%, 70%, 75% and 80% of the R-R interval at 0.625 mm and sent to a workstation. Additional phases from 0% to 90% were reconstructed at 2.5-mm slice thickness for evaluation of the ejection fraction. Coronary vessels were reviewed on the workstation using commercial cardiac volume models (AW Volume Share™, GE Medical Systems, Milwaukee, WI). Volume renderings and curved reformations were done as well as interactive double oblique orthogonal 2–4-mm views of the vessels. Maximum intensity projection thick slabs (10–20 mm) were obtained for broader views of vessel orientation and anatomic relationships. Selected images and series were saved to PACS from the workstation.
Vessel assessment
Coronary arteries
Two radiologists (DL and GAZ) assessed the pulmonary, aortic and coronary arteries by consensus. The coronary arteries were divided into three groups: group 1: left main coronary artery (LMCA), left anterior descending artery (LAD) and diagonal branches; group 2: left circumflex (LCx) and obtuse marginal branches; group 3: right coronary artery (RCA), acute marginal branches, posterior descending artery (PDA) and posterior lateral branch (PLB). Left or right dominance was determined as well as the presence of ramus intermedius, myocardial bridge and other anatomical coronary variants. Motion artifacts and vessel attenuation of each coronary artery group was graded using a 5-point scale: 1, poor; 2, fair; 3, good (some artifacts in less than half of the vessel group); 4, very good (few artifacts in less than one-third of the vessel group); 5, excellent (no artifacts). A total of 168 coronary artery groups (56 studies ×3 coronary groups) were graded. The same grading scale was used to grade the coronary angiograms per patient. The studies or vessels with overall grades of 4 or 5 were considered as diagnostic.
CT coronary angiographic images were reformatted using curved multiplanar reformations through the lumen of the coronary vessel. The minimal diameter of stenotic artery lesions was measured using manually positioned electronic calipers and compared with the maximal diameter of the closest proximal normal arterial segment, based on established cardiology practice [13]. The coronary arteries were segmented according to American Heart Association guidelines [14], based on 16-segment classifications for evaluation of coronary artery stenosis (including ramus intermedius). Each vessel segment was assessed as 0= no stenosis, 1= 1–49% stenosis, 2= 50–74% stenosis, 3= 75–99% stenosis and 4= occlusion. Each segment was also classified as being significantly stenosed (diameter reduction of >50%) or not. Vessels 1.5 mm in diameter or larger were assessed.
In nine patients who had selective coronary catheterization within 3 months (±1.2 months) following MDCT, detailed segment-by-segment comparison of MDCT arteriography with catheterization was made. Segments were classified according to the same AHA classification and were subjectively classified as significantly stenosed (diameter reduction of >50%) or not (same criteria as in CTA).
Aorta and pulmonary artery opacification
Enhancement of the pulmonary artery and aorta was measured using the region of interest (ROI) technique. Aortic and pulmonary artery attenuation higher than 200 HU was adequate. For pulmonary artery attenuation, measurements were taken at four levels: the main pulmonary trunk, left and right pulmonary arteries and left lower lobe pulmonary artery, each just above the bifurcation. Attenuation of the thoracic aorta was also measured at four levels: ascending aorta and descending aorta at the level of the main pulmonary artery, descending aorta at the level of the mid-left atrium and at the level of the diaphragm. Homogeneity of the contrast column in the aorta and the pulmonary arteries of each patient were assessed by calculating the contrast homogeneity index (CHI) for the aorta and pulmonary artery as follows:
where HUmax, HUmin and HUmean were the highest, the lowest and the mean value of the four attenuation measurements in each vessel, respectively. A higher CH index indicates greater contrast column homogeneity in the vessel.
Chest CT assessment
The appearance of pulmonary parenchyma and chest wall was evaluated for adequacy of image quality and abnormalities detected. Motion artifacts, bands, counter pulsation of the ascending aorta and stepladder cardiac pulsation artifacts of the distal lower lobes in the pulmonary arteries were assessed. The overall appearance of the chest CT was subjectively graded on the following 5-point scale: 1, not interpretable study; 2, poor, probably not interpretable; 3, moderate, some artifacts in less than half of the chest; 4, adequate, few artifacts in less than one-third of the chest; 5, superior, no artifacts.
Dosimetry
Mean computed tomography dose index, CTDIvol (mGy) and dose-length product (DLP) (mGy-cm), were calculated from the radiation dose report provided for each study. The estimate of effective dose calculation was based on the European Guidelines on Quality Criteria on Computed Tomography using the following formula:
Where E = effective dose in mSv, E DLP = 0.017 (dose length co-efficient for chest) and DLP = dose length product in mGy-cm [15]. The mean dose value was compared to that of the control group with an equal number of patients (n = 56) matched for age and gender, scanned within the same time period on the same GE 64-row MDCT scanner using non-gated chest CTA protocol: fixed 50-mA non-contrast enhanced scan followed by chest CT angiography. In these scans, x-y-z modulation was applied using a range of 150–500 mA and noise index of 11.57. In addition, the DLP was measured in 12 consecutive patients who had coronary CT angiography with 64-MDCT, but without ECG modulation.
Statistical analysis
Descriptive statistics of patient sex, age, heart rate, and vessel artifacts were calculated. Numerical data are reported as the mean ± the standard deviation. Ordinal data are presented as the median and the 25th and 75th percentiles. Categorical data are presented as counts and percentages. The adequacy of the chest CT quality was tested with the Wilcoxon signed rank test, considering grade 4 (adequate study) as the hypothetical adequate-for-diagnosis grade. The same test was also used to assess whether the coronary angiograms received a diagnostic grade, designating grade 4 as the adequate-for-diagnosis grade for the coronary artery group and for patient study. Finally regression analysis was made comparing the heart rate with the elements measuring the scan quality as indicated by coronary arteries and chest CT grades.
Comparison of the agreement between CTA and invasive selective coronary angiography was done by segments graded 0 to 4 for stenosis using kappa statistics. In addition, the five grades were further divided into two categories of 0–49% and 50% and above stenosis. For this comparison we used Fisher’s exact test to identify sensitivity, specificity, negative and positive predictive value using selective invasive coronary angiography as the gold standard.
Results
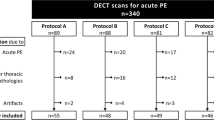
Of 113 patients referred to this study by our ED physicians, 33 did not match the inclusion criteria. Twenty-four additional patients were excluded due to inability to achieve the desired heart rate after use of beta blockers. The remaining 56 patients completed the MDCT angiography study without complications. The mean age of the 56 scanned patients was 59.2 ± 10.6 years. Four patients younger than 50 years were scanned to exclude aortic dissection. The mean heart rate was 56.5 ± 5 bpm. In 46 (82.1%) patients the heart rate was less than 65 bpm. The mean scan range was 221 ± 35 mm.
Abnormalities detected
Of 56 ECG-gated chest CT angiograms, the scans were normal in 20 (34.2%) patients. Vascular, non-coronary abnormalities were diagnosed in 11 (19.5%): PE in 4, aortic dissection in 3 and aortic aneurysm in 4. In 20 (35%) patients, a lung or pleural abnormality was found that explained the patient’s symptoms, including pulmonary consolidations suggesting pneumonia, pulmonary edema, pleural effusion, atelectasis and emphysema. On coronary CT angiography 16 (28.5%) of 56 patients showed evidence of coronary artery disease, with both calcified and non-calcified plaques detected (Figs. 2 and 3). One patient had spontaneous dissection of mid LAD with CT showing evidence of myocardial hypoperfusion (Fig. 4). Nine of the 16 patients underwent conventional selective invasive coronary angiography. Of 144 segments, 130 were evaluated (90.2%) based on vessel diameter greater then 1.5 mm. Per segment comparison was done and the weighted kappa statistic by segments was 0.79 indicating substantial agreement between two tests (p<0.001). Using the same per-segment data based on below or above 50% stenosis, Fisher’s exact test shows a sensitivity of 81% (95% CI 54–95%) and specificity of 93% (95% CI 87–98%), with a positive predictive value of 68% (95% CI 43–87%) and negative predictive value of 96% (95% CI 91–99%).
Curved reconstruction of ECG-gated chest CTA showing calcified plaque in proximal (black line) and non-calcified plaques in mid LAD (white line) producing mild (less than 50%) stenosis (a). Cross images at the long axis of the vessel (at the black and white lines) provide means for assessing the lumen and characterizing the plaque, the proximal (b) being mixed calcified-soft, and the mid-vessel plaque (c) being purely soft
Axial (a) and curved reformatted (b) images from ECG-gated chest CTA of a 52-year-old woman with atypical chest pain showing severe (greater than 70%) stenosis in proximal LAD, confirmed at subsequent coronary angiogram (arrows) (c). Axial image of the ascending aorta (d) shows no artifacts. Coronal reformation (e) of the chest viewed with lung windows show normal parenchyma and no pulsation or other motion artifacts
Curved reformatted and axial images of a 39-year-old 4-week postpartum woman with persistent chest pain demonstrate severe stenosis in proximal LAD (a) (arrows) and related perfusion defect (b) (arrowheads) involving the anterior wall of the left ventricle and the anterior septum corresponding to diagnosed severe stenosis in proximal LAD due to spontaneous coronary dissection (c) (white arrow)
In addition to atherosclerotic plaques, MDCT demonstrated findings not mentioned on the written interpretation report of catheter coronary angiography: ramus intermedius was seen in four patients, myocardial bridge in five patients and anomalous origin of the right coronary artery from the left coronary sinus of Valsalva in one patient.
Functional data were obtained with the dose modulation, and dose modulation did not affect Functional Data acquisition.
Aorta and pulmonary arteries
Except for one exam, no motion or pseudodissection artifacts were diagnosed in the pulmonary arteries, aorta and pulmonary parenchyma (Fig. 4). Vessel attenuation was measured in 448 predetermined points (224 in the aorta and 224 in the pulmonary arteries). By vessel, the mean attenuations of the pulmonary artery and the thoracic aorta were 321 ± 103 HU and 316.70 ± 88.83 HU, respectively. Forty-three of 448 (9.6%) individual measurements in the aorta and pulmonary arteries had attenuation values lower than 200 HU (Fig. 5). By patient, the mean of four predetermined attenuation measurements of the aorta was greater than 200 HU in all but two exams (161 HU and 187 HU, respectively). The mean of four predetermined attenuation measurements of the pulmonary artery was greater than 200 HU in all but six exams: in five the mean attenuation ranged between 160 and 181 HU. In one patient, a non-ECG-gated pulmonary CT angiogram was repeated because of poor pulmonary artery opacification: mean attenuation was 123 HU. A minor timing adjustment was made to the original protocol after the 16th patient that resulted in higher levels of opacification in aorta and pulmonary arteries (mean: 340 HU and 315 HU, respectively, with no attenuation measurements below 200 HU) in the remaining 40 patients.
Box plot of median (mid-line) and 25–75 quartiles of attenuation of specific locations in the aorta (Ao) and pulmonary arteries (PA) ⊗, indicates mean. There is little variation in mean and median attenuation values along the two vessels, ~300 HU, indicating homogeneity of the contrast column, and the vessel attenuation is satisfactory, mostly greater than 200 HU. Ao1 and Ao2: ascending aorta and descending aorta at the level of main pulmonary artery. Ao3 and Ao4: descending aorta at the level of the mid-left atrium and diaphragm, respectively. PA1: main pulmonary trunk. PA2 and PA3: left and right pulmonary arteries. PA4: left lower lobe pulmonary artery
The contrast column in the aorta and pulmonary arteries showed overall little variation in attenuation (Fig. 5). The contrast homogeneity index was 0.79 for the aorta and 0.87 for the pulmonary artery.
With the triphasic injection of IV contrast, the attenuation of the superior vena cava and right ventricle was low enough to eliminate streak artifacts while the pulmonary arteries, left ventricle, aorta and coronary arteries were opacified adequately for CT angiography (Fig. 6). The mean attenuation of the right ventricle was significantly lower that of the left ventricle: 275 ± 126 HU compared to 325 ± 71 (p = 0.01, paired t-test). In 24 of 55 patients the attenuation in the right ventricle was less then 200 HU. In contrast, the attenuation in the left ventricle was less than 200 HU in only two of the same 55 patients.
Coronary arteries
Satisfactory visualization was achieved in 51 out of 56 patients (grade 4 or 5) (Table 1). In the remaining five patients the overall grades were: grade 1 in one patient, grade 2 in two patients and grade 3 in two patients (Table 1). The overall mean coronary angiography grade was 4.44 ± 0.93 and the median was 5 (quartiles 4–5). This is statistically significantly higher than the presumed adequate-for-diagnosis grade of 4 (p = 0.0012). Similarly the LM and LCA group and the RCA each received a median grade of 5 (quartiles 4–5), which is statistically superior to the presumed adequate-for-diagnosis grade 4 (p<0.001 for both groups). There was no statistical difference between the LCx group grade of 4 (quartiles 4–5) and the presumed adequate-for-diagnosis grade of 4. Moderate to marked bands and coronary artery motion artifacts were noted in 6 of 10 patients with heart rates >65 bpm (60%). Linear regression analysis showed a statistically significant correlation of higher grades with lower pulse rates for all elements of the coronary study (p < 0.001). Beam-hardening artifacts from the superior vena cava, right atrium and ventricle were seen in five patients, though not severe enough to affect visualization of the right coronary artery.
Lungs and thorax
High quality images of the lungs, pleura and chest wall were produced. The mean chest CT grade was 4.16 ± 1.04, and the median was 4 (quartiles 4–5). This is not statistically significantly different from the presumed acceptable-for-diagnosis grade of 4 (p = 0.158). Stepladder cardiac pulsation artifacts of the ascending aorta and distal pulmonary arteries were noted in the patients with bands and coronary artery motion artifacts and were more pronounced in patients with faster pulse rates. Linear regression analysis showed a trend towards a relationship of lower grades with higher pulse rates (p < 0.056).
Dosimetry
Dose modulation technique based on ECG-gating was applied in each case. In our patients the average DLP was 1,490 ± 412 mGy-cm. After conversion into effective dose using the normalized effective dose, EDLP coefficient, the effective dose was 25 ± 7 mSv. By comparison, the average dose received by the 56 control patients who had non-gated chest CT angiogram was 710 ± 171 mGy-cm, (12 ± 3 mSv), about half that of the gated technique. Conversely, the mean DLP of 12 consecutive non ECG-modulated coronary CT angiograms, where only the heart was scanned, was 1,670 ± 390 mGy-cm (28 ± 7 mSv).
Discussion
Combined evaluation of the pulmonary arteries, thoracic aorta and coronary arteries along with lung parenchyma, pleura and chest wall using a single acquisition technique was done. Routine use of such a protocol in clinical practice may provide fast and precise information, facilitating a more expeditious triage of patients with chest pain.
In our study the contrast column was homogeneous in both the pulmonary arteries and aorta, showing small attenuation differences among measurements made in the upper, middle and lower chest. Note that the latter 40 patients demonstrated better opacification of the major arteries following a minor adjustment to the protocol; however, we analyzed the results for the entire group of 56 patients, which affected the mean values of the entire study population.
In addition, vascular attenuation values were high (mean levels greater than 300 HU) while with the tri-phasic injection, attenuation in superior vena cava and right heart decreased to levels that did not produce streak artifacts. Coronary artery visualization surpassed expectations for adequate quality study, although evaluation of coronary artery stenosis was performed on an observational basis only. Both calcified and non-calcified coronary artery plaques were noted, although precise calcium scoring was not assessed. With gating, pseudodissection artifact in the ascending aorta was eliminated, as shown by Roos et al. [2]. This, along with the high quality of coronary artery imaging would have an important application in the evaluation of type A aortic dissection and assessment of extension to the coronary arteries.
With the triphasic protocol, scanning time of the whole chest is fast, less than 9 s, making it a comfortable test and applicable even in patients with mild shortness of breath. The use of the triphasic injection protocol, with combined contrast and saline injection in the second phase, reduced the IV contrast amount to 80 ml instead of the 100 ml normally used for non-gated chest CT angiography or the 120–130 ml used for gated studies with 16-row MDCT [16]. In addition, the triphasic injection achieved the goal of high attenuation in the pulmonary arteries, aorta and coronary arteries and low attenuation in the superior vena cava and right ventricle. Finally, the use of ECG-based dose modulation technique reduced radiation dose by about 30%, to an average effective dose of approximately 1,500 mGy-cm compared to the approximately 1,700 mGy-cm received on ECG-gated non-dose modulated dedicated coronary CT exams. This dose is no more than twice that of non-gated chest CT angiograms, while providing considerably more information.
Our results showed direct connection between heart rate and image quality, represented by fewer bands or motion artifacts. The highest quality was assessed when the heart rate was less than 65 bpm for both vascular and non-vascular structures. The best approach to achieve this was by using oral beta-blockage, about 1 h before the study and, if needed, supplemented by intravenous beta-blockage with the patient on the table. Use of beta blockers might be inappropriate in a small minority of ED patients, especially those suffering from asthma, allergy or low blood pressure. In our practice, individual decision for their use was made in consultation with the patient’s clinician and was widely supported by our ED colleagues. In addition, the 40–60 min prep delay may be too long for some patients, but our study group did not include critically ill patients.
In our study of 56 patients with non-specific chest pain, not suspected to be caused by coronary artery disease, 16 patients had severe or moderate coronary stenosis on MDCT, and 9 of them had catheterization based on subsequent cardiac evaluation. Although the high percentage of patients with coronary artery disease we encountered may be coincidental, it shows that choice of disease-specific MDCT protocol based on clinical evaluation alone is inadequate. Furthermore, the high correlation of the gated MDCT findings with coronary catheter angiography in our small series is comparable to the results of dedicated coronary 64-MDCT angiography [17]. Our results were also comparable to a recent study evaluating the role of ECG-gated 64-MDCT angiography in the differential diagnosis of acute chest pain [18]; however, our study demonstrated consistent emptying of contrast in the right heart. Another recent study demonstrated good coronary artery enchancement [12], but provided no direct comparison between MDCT and invasive coronary arteriography as we were able to obtain. Our triphase protocol also allows obtainment of pulmonary arteries, aorta and coronary arteries enhancement with significantly smaller (up to 30%) amounts of IV contrast compared to the above-mentioned studies.
The ECG-gated chest CTA protocol has a number of limitations, including the need to slow heart rate and appropriate training of radiology technologists and radiologists.
Another limitation is the relatively high radiation exposure, increased by retrospective ECG-gating because of the low pitch used. This high radiation exposure was reduced by 30% through dose modulation, but this still remains high and raises the issue of using gated protocols when clinical suspicion for PE, aortic dissection or coronary artery disease is very low. Radiation limitations may decrease considerably with the recently released dual-source MDCT (Siemens Medical Solutions, Malvern, PA) or the upcoming 256-row non-spiral MDCT (Toshiba Medical Systems, Tokyo, Japan) with prospective ECG gating [19–22].
An additional consideration is the relatively low sensitivity of this exam to diagnose chest pain due to musculoskeletal problems and gastroesophageal reflux disease. Thus, although many life-threatening diseases could be diagnosed or excluded, not every cause of chest pain can be diagnosed with this protocol.
This study has a number of biases related to selection criteria. The large number of drop-outs we experienced was at least partially due to the strict selection criteria. Verification bias is related to coronary artery evaluation because not all the results of our test have been compared with a reference test Finally, for all non-cardiac components the results of the test were incorporated as evidence of the final diagnosis (given the well-accepted accuracy of chest CTA for pulmonary, aortic and pulmonary artery abnormalities), thus leading to incorporation bias [23].
Our preliminary results suggest that the ECG-gated chest pain protocol using 64-slice MDCT can be used as a single technique for evaluation of acute chest pain in the Emergency Department setting, allowing superior pulmonary vessel, aortic and coronary artery contrast medium delivery along with all the advantages of a tailored CTA for evaluation of the pulmonary arteries, aorta, coronary arteries, lungs and the rest of the thorax. A commonly used term for the technique is “triple rule out,” while in actuality the technique assesses at least four major components of the thorax. Consequently, we believe the term “ECG-gated chest CTA” is more appropriate.
References
Raptopoulos VD, Boiselle PB, Michailidis N (2006) MDCT angiography of acute chest pain: evaluation of ECG-gated and nongated techniques. AJR 186:S346–S356
Roos JE, Willmann JK, Weishaupt D, Lachat M, Marincek B, Hilfiker PR (2002) Thoracic aorta: motion artifact reduction with retrospective and prospective electrocardiography-assisted multi-detector row CT. Radiology 222:271–277
Marten K, Engelke C, Funke M, Obenauer S, Baum F, Grabbe E (2003) ECG-gated multislice spiral CT for diagnosis of acute pulmonary embolism. Clin Radiol 58:862–868
Schoepf UJ, Becker CR, Bruening RD (1999) Electrocardiographically gated thin-section CT of the lung. Radiology 212:649–654
Boehm T, Willmann JK, Hilfiker PR (2003) Thin-section CT of the lung: does electrocardiographic triggering influence diagnosis? Radiology 229:483–491
Morin RL, Gerber TC, McCollough CH (2003) Radiation dose in computed tomography of the heart. Circulation 18(107):917–922, Feb
Bae KT, Hong C, Whiting BR (2004) Radiation dose in multidetector row computed tomography cardiac imaging. J Magn Reson Imaging 19:859–863, Jun
Jakobs TF, Becker CR, Ohnesorge B, Flohr T, Suess C, Schoepf UJ, Reiser MF (2002) Multislice helical CT of the heart with retrospective ECG gating: reduction ofradiation exposure by ECG-controlled tube current modulation. Eur Radiol 12:1081–1086
Sigal-Cinqualbre AB, Hennequin R, Abada HT, Chen X, Paul JF (2004) Low-kilovoltage multi-detector row chest CT in adults: feasibility and effect on image quality and iodine dose. Radiology 231:169–174
Abada HT, Larchez C, Daoud B, Sigal-Cinqualbre A, Paul JF (2006) MDCT of the coronary arteries: feasibility of low-dose CT with ECG-pulsed tubecurrent modulation to reduce radiation dose. AJR 186:S387–S390
d’Agostino AG, Remy-Jardin M, Khalil C, Delannoy-Deken V, Flohr T, Duhamel A, Remy J (2006) Low-dose ECG-gated 64-slices helical CT angiography of the chest: evaluation of image quality in 105 patients.Eur Radiol 16(10):2137–2146, Oct
Vrachliotis TG, Bis KG, Haidary A, Kosuri R, Balasubramaniam M, Gallagher M, Raff G, Ross M, O’neil B, O’neill W (2007) Atypical chest pain: coronary, aortic, and pulmonary vasculature enhancement atbiphasic single-injection 64-section CT angiography. Radiology 243(2):368–376, May
Ghersin E, Litmanovich D, Dragu R (2006) 16-MDCT coronary angiography versus invasive coronary angiography in acute chest pain syndrome: a blinded prospective study. AJR 186:177–184
Austen W, Edwards J, Frye R et al (1975) A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association 51(4 Suppl):5–40, Apr
European Guidelines on Quality Criteria for Computed Tomography. Available at: http://www.drs.dk/guidelines/ct/quality/index.htm. Accessed June 26, 2002
White CS, Kuo D, Kelemen M. Chest pain evaluation in the emergency department: can MDCT provide a comprehensive evaluation? AJR 185:533–540
Leber AW, Knez A, von Ziegler F, Becker A, Nikolaou K, Paul S, Wintersperger B, Reiser M, Becker CR, Steinbeck G, Boekstegers P (2005) Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol 46(1):147–154
Johnson TR, Nikolaou K, Wintersperger BJ, Knez A, Boekstegers P, Reiser MF, Becker CR (2007) ECG-gated 64-MDCT angiography in the differential diagnosis of acute chest pain. AJR Am J Roentgenol 188(1):76–82, Jan
Flohr TG, McCollough CH, Bruder H, Petersilka M, Gruber K, Suss C, Grasruck M, Stierstorfer K, Krauss B, Raupach R, Primak AN, Kuttner A, Achenbach S, Becker C, Kopp A, Ohnesorge BM (2006) First performance evaluation of a dual-source CT (DSCT) system. Eur Radiol 16(2):256–68, Feb, Epub 2005 Dec 10. Erratum in: Eur Radiol 16(6):1405, Jun
Scheffel H, Alkadhi H, Plass A, Vachenauer R, Desbiolles L, Gaemperli O, Schepis T, Frauenfelder T, Schertler T, Husmann L, Grunenfelder J, Genoni M, Kaufmann PA, Marincek B, Leschka S (2006) Accuracy of dual-source CT coronary angiography: first experience in a high pre-test probability population without heart rate control. Eur Radiol 16(12):2739–2747, Dec
Johnson TR, Nikolaou K, Wintersperger BJ, Leber AW, von Ziegler F, Rist C, Buhmann S, Knez A, Reiser MF, Becker CR (2006) Dual-source CT cardiac imaging: initial experience. Eur Radiol 16(7):1409–1415, Jul
Johnson TR, Nikolaou K, Fink C, Becker A, Knez A, Rist C, Reiser MF, Becker CR (2007) Dual-source CT in chest pain diagnosis. Radiologe 47(4):301–309, Apr
Sica GT (2006) Bias in research studies. Radiology 239:780–789
Acknowledgements
The authors are grateful to (Donna Wolfe) for editorial assistance and to (Clotell Forde) for secretarial, data formatting and literature search assistance and (Iryna Rastorhuyeva) for assistance with data collection.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00330-007-0791-y
Rights and permissions
About this article
Cite this article
Litmanovitch, D., Zamboni, G.A., Hauser, T.H. et al. ECG-gated chest CT angiography with 64-MDCT and tri-phasic IV contrast administration regimen in patients with acute non-specific chest pain. Eur Radiol 18, 308–317 (2008). https://doi.org/10.1007/s00330-007-0739-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-007-0739-2