Abstract
Purpose of Review
The purpose of this review is to summarize the recent technical and scientific advancements in cardiac computed tomography (CT) assessment of ventricular function and valvular heart disease.
Recent Findings
With improvement in scanner technology and protocols, cardiac CT can be used to assess cardiac function and chamber volumes with excellent accuracy and interobserver reproducibility. CT is a reliable adjunct modality to assess most valvular heart diseases when other modalities are not adequate or provide discrepant data. CT is now the standard of care in planning transcatheter valve interventions.
Summary
Cardiac CT can be reliably used to assess right and left ventricular function albeit with radiation exposure. CT is also helpful as a tiebreaker in complex valvular heart disease when other modalities are discrepant or limited. Further improvement in temporal resolution and reduction of radiation dose will increase utilization of cardiac CT with the goal of comprehensive cardiac assessment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiac computed tomography (CT) is now an established tool for the assessment of patients with different suspected cardiac pathologies [1]. It is primarily used in the assessment of coronary arteries given its high diagnostic accuracy [2] and has been shown to be best utilized in patients with low to intermediate probability of coronary artery disease [3,4,5]. However, this tool can also be utilized as a second-line test in patients with other cardiac pathologies to provide an assessment of right and left ventricular function and size as well as valvular function. In this review, we will provide a detailed review of these applications of cardiac CT.
Assessment of Left Ventricular Function
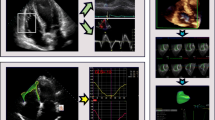
Echocardiography is often the initial tool in the assessment of left and right ventricular function. It is portable, quick, and cheap and can provide accurate assessment when the echo windows are adequate [6]. Cardiac magnetic resonance imaging (CMR) is an alternative when echocardiography is not adequate. It has high spatial resolution, good temporal resolution, unrestricted view of the heart, and high reproducibility [6]. These strengths are also shared by cardiac CT which has the highest spatial resolution, acceptable temporal resolution (but lower than echo and CMR), unrestricted view of the heart, and high reproducibility. Cardiac CT calculates the ejection fraction (EF) by true volumetric evaluation without geometric assumptions (Fig. 1), resulting in accurate EF calculation irrespective of the degree of left ventricular (LV) remodeling or systolic dysfunction [7]. The inter- and intraobserver reproducibility of LVEF by cardiac CT is high. This correlation has even improved as the temporal resolution of the CT systems improved [8••].
In a study of 79 patients who underwent both cardiac CT and CMR, CT and CMR images showed good agreement: LVEF (52 ± 14% for CT vs. 52 ± 14% for CMR; r = 0.73; p > 0.05); RVEF (47 ± 12% for CT vs. 47 ± 12% for CMR; r = 0.74; p > 0.05). The intra- and interobserver variabilities were good, and the performance of CT was maintained for different EF subgroups. Thus, cardiac CT provides accurate and reproducible LV and RV ejection fractions and volumes compared with CMR [9]. Using a dual-source CT system which has the highest temporal resolution showed similar findings in a study of 15 patients. The mean left ventricular EF was 61.6 ± 12.4% in cardiac CT and 57.9 ± 9.0% in CMR, resulting in an overestimation of EF by 3.8% [10]. It is possible that the observed differences in the measured ejection fractions may be due to different post-processing methods and physiological reactions to contrast material injection without beta-blocker medication.
A meta-analysis of 12 studies showed no significant difference in LVEF between cardiac CT and CMR with a difference of only − 0.11 (− 1.48 and 1.26, respectively; 95% CI), p = 0.88. Thus, these newer generation dual-source CT systems provide accurate LVEF measurement compared with CMR [11].
LV dysfunction and volumes measured with cardiac CT can also provide prognostic value by augmenting risk prediction and discrimination for future mortality. In a study of 7758 patients, worsening LVEF measured by cardiac CT was independently associated with mortality for moderately (hazard ratio = 3.14, p < .001) and severely (hazard ratio = 5.19, p < .001) abnormal ejection fraction. Similarly, LV end-systolic volumes and LV end-diastolic volumes demonstrated improved discrimination when compared with coronary artery disease risk factors or extent and severity [12, 13].
However, one should keep in mind that the main limitation of using CT to calculate cardiac functional parameters is the high level of radiation [14]. This is considered a quality measure that operators always try to reduce [15]. To determine the systolic and diastolic volumes, the patient will receive radiation through the entire cardiac cycle to determine systole and diastole. This is often referred to as retrospective gating and is the mode of scanning associated with the highest radiation exposure [16]. Radiation exposure can be lowered if other modes are used in image acquisition, but these modes (prospective gating, high-pitch scanning) do not allow for accurate left ventricular volumes and ejection fraction assessment [17]. This would be possible only if wide padding is used. A recent study of 77 patients suggested that a low-dose CT LVEF protocol is feasible, accurate, and fast with a good correlation (r = 0.863) [18••].
Assessment of Right Ventricular Function
The same rational used for the left ventricle can also be applied to the right ventricle (RV). The right ventricle has complex geometry which makes it difficult to image by echocardiography. It is triangular from the side and crescentic in cross section [19, 20]. Its posterior wall is formed by the ventricular septum, which is concave towards the LV in both systole and diastole. Compared with the LV, the RV has a larger volume [19].
CMR is considered the gold standard for RVEF given its complex 3D and highly variable shape [21, 22]. Cardiac CT serves as an alternative to echocardiography and MRI for quantification of RV and LV volume and function [23] when echocardiography and CMR are inadequate [24]. This might be of utmost importance when primary or secondary pathologies of the RV are suspected like arrhythmogenic right ventricular dysplasia and RV failure secondary to pulmonary hypertension [25, 26]. CT imaging has been used to evaluate arrhythmogenic right ventricular dysplasia and has the ability to depict the characteristic abnormalities in attenuation correction (AC) such as abnormal RV morphology and fat infiltration [27]. Given all the above, the 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death recommend that CMR or cardiac CT should be considered in patients with ventricular arrhythmias when echocardiography does not provide accurate assessment of left or right ventricular function and/or evaluation of structural changes.
Assessment of Valvular Heart Disease
Although echocardiography remains the first-line tool in assessment of valvular heart disease (VHD), cardiac CT has emerged a powerful imaging modality with numerous clinical applications where echocardiography is limited or discrepancies of clinical and diagnostic findings exist. Multiphase retrospectively gated CT was traditionally utilized to assess the valvular structure and function but at the cost of higher radiation exposure compared with prospective triggered imaging. The improvement in temporal resolution of CT systems improved the role of the use of CT in VHD. Prospective imaging with wide intervals to capture diastolic and systolic phases may also be sufficient for valvular assessment, depending on the clinical scenario.
In structural heart interventions, CT is widely adopted and essential for preoperative planning and valve sizing, particularly in transcatheter aortic and mitral valve interventions. CT is also now used in prosthetic valve dysfunction and complicated infective endocarditis with critical implications for treatment strategies such as detection of aortic root abscess. These and other indications were acknowledged in the 2017 Appropriate Use Criteria for Multimodality Imaging in Valvular Heart Disease document [28]. CT is also considered an appropriate modality to exclude coronary artery disease in patients with an intermediate pretest probability undergoing cardiac valve surgery. Due to its superior spatial resolution, CT is frequently the optimal imaging study to use for 3D printing and fusion imaging during structural interventions.
The Aortic Valve
The development of transcatheter aortic valve replacement (TAVR) led to greater understanding of the aortic valve and annulus dynamic nature. Appropriate electrocardiographic gating of CT allows superior visualization of the aortic valve leaflets in systole and diastole by reconstructing the dataset at different phases of the R-R interval. Generally, maximal opening of the aortic valve is at 20–30% of the R-R interval, and closure in diastole is captured at the 70% phase. CT studies also demonstrate that the aortic annulus is elliptical (and becomes more circular in systole) with larger dimensions compared with 2D echocardiographic dimensions.
In aortic stenosis assessment, planimetry of the aortic valve area (AVACT) correlates well with echocardiographic-based measurements (AVAecho) in most reports but systematically—slightly—overestimates the valve area [29, 30]. This is due to the fact that AVAecho calculated using the continuity equation measures the effective orifice area (or vena contracta) as opposed to the anatomic orifice area planimetered on CT. Visualization of the leaflet tips particularly in deformed valves or suboptimal studies can be challenging and can result in an erroneous calculation of AVA. As a result, AVA planimetry by CT is not routinely recommended when echocardiography is available.
Hybrid calculation of AVA by measuring the left ventricular outflow tract (LVOT) area by CT and entering it into the continuity equation systematically measure larger AVAs by approximately 0.2 cm2. Hybrid calculation of AVA can be useful in cases with paradoxical low-gradient aortic stenosis and where echo assessment of the LVOT is limited (Fig. 2.).
Aortic stenosis. Contrast-enhanced gated cardiac CT in a 70-year-old woman with aortic stenosis. Minimal-intensity projection and slice thickness of 2.4 mm are used to optimize measurements. The aortic valve is trileaflet with mild calcification (arrow) (a). Planimetered aortic valve area is 1.1 cm2 (b). Echocardiography performed on the same day yielded an aortic valve area of 1.0 cm2 with peak velocity of 2.8 m/s and mean gradient of 21 mmHg
New emerging data also emphasized the role AV calcium load (AVC) by non-contrast CT in patients with low-gradient aortic stenosis [31]. Measurement of AVC is now well established with prognostic data and recommended with well-delineated cutoffs for men (> 2000 arbitrary units) and women (> 1200 arbitrary units) for severe AS [32, 33••, 34••, 35••, 36••].
In patients referred for TAVR, the use of CT is essential to determine the annular size and access. The reconstruction-based measurements of the aortic annulus were shown to reduce the incidence of greater than mild paravalvular aortic regurgitation compared with 2D transesophageal echocardiographic measurements. Furthermore, CT quantitation of calcium location and burden in the LVOT is another important predictor of paravalvular regurgitation [37, 38].
In aortic regurgitation (AR), it is feasible to measure the anatomic regurgitant orifice area (AROA) by CT. A recent study showed good correlation with phase-contrast cardiovascular magnetic resonance, with an r = 0.83 between AROA and AR severity measured by CMR. Discrimination of AR severity (mild vs. moderate and moderate vs. severe) with dual source CT was best with cutoff AROAs of 15 mm2 and 23 mm2 [39]. However, other studies described different cutoffs, and it is likely that AROA measurement is highly operator dependent, with caveats in deformed bicuspid valves with eccentric jets and studies with suboptimal imaging protocols (Fig. 3).
Aortic regurgitation. Contrast-enhanced gated cardiac CT in a 74-year-old man with AR. Minimal-intensity projection and slice thickness of 1.95 mm are used to optimize measurements after alignment coaxial to the coaptation defect. A trileaflet aortic valve with poor coaptation is shown in the 70% phase (a). The AROA is measured at 0.4 cm2 (b). The left ventricle is severely enlarged with an end-diastolic volume of 319 ml. Echocardiography confirmed severe AR with a regurgitant volume of 61 ml and regurgitant fraction of 51% (RC right cusp, LC left cusp, NC non-coronary cusp)
The Mitral Valve
The mitral valvular apparatus is a complex structure with a saddle-shaped highly dynamic annulus. The anterior mitral leaflet is intricately linked to the LVOT and aortic valve through the aortomitral curtain. Due to dynamic changes in anatomical configuration of the mitral apparatus, LVOT, and left ventricle, CT data acquisition for mitral valve (MV) assessment should preferably include the entire cardiac cycle. The mitral apparatus is best evaluated by standard views mimicking those obtained using echocardiography (commissural, 3-chamber, 4-chamber, and short-axis views). However, visualization of the dataset in a cine format improves the reader’s ability to detect structural abnormalities such as restricted motion, mitral valve prolapse, or flail leaflets.
Mitral valve stenosis (MS) management depends on accurate assessment of the mitral valve orifice area (MVA) by 2D/3D echocardiography and Doppler assessment. Calcific MS due to mitral annular calcification (MAC) is now the most common cause of MS in developed countries and represents a diagnostic and therapeutic challenges [40, 41]. Echocardiographic assessment can be limited by shadowing and poor acoustic windows. Furthermore, delineation of the extent and severity of MAC is subjective and often limited. Cardiac CT allows accurate quantitation of MVA by experienced operators with good correlation against echocardiography. Training and experience are critical to obtain an en face view correctly. CT also provides a non-obstructed view of the mitral valvular and subvalvular apparatus. In transcatheter mitral valve interventions, CT now plays a key role in valve sizing, predicting the risk of LVOT obstruction, optimizing fluoroscopy angles for implantation, and planning transapical access routes among other uses [42]. Cardiac CT can also help in excluding left atrial appendage clots in patients with severe mitral valve disease prior to intervention [43]. For these, a delayed scan is often needed to avoid poor mixing artifacts [44].
In the diagnosis and assessment of mitral regurgitation (MR) severity, CT performed well in relatively small studies. In a small case-control study of 23 patients with MR and 20 controls, CT-derived AROA correlated well (r = 0.89) against echocardiographic grading of mild, moderate, and severe MR. However, it only had modest correlation against vena contracta and effective ROA [45]. In isolated MR, quantitation can be performed using volumetric methods by comparing the stroke volume of the LV and the stroke volume of the RV. Although not the first-line method to assess MR severity, a relatively small study of 49 patients with isolated MR showed good correlation of CT-derived regurgitant volume/fraction vs. that of CMR [46] (Fig. 4).
Myxomatous mitral valve disease. Contrast-enhanced prospective cardiac CT in a 50-year-old woman. The patient had primary degenerative MR and no risk factors for coronary disease. Coronary CT showed minimal atherosclerosis and no coronary stenosis. Reconstructions of a 5-chamber view (a) and a 2-chamber view (b) demonstrate severe prolapse of the posterior leaflet (black arrow) with flail P2 (white arrow). This was confirmed intraoperatively (LAA indicates left atrial appendage)
In clinical practice, CT is now most important in planning transcatheter interventions for MR, with diagnosis and quantitation largely dependent on echocardiography and CMR.
The Tricuspid Valve
Assessment of tricuspid valve regurgitation (TR) is no longer forgotten with the recognition of the impact of secondary TR on outcomes. The tricuspid valve is generally more difficult to visualize with CT because of relatively thin leaflets and contrast mixing artifacts. A key step in the imaging is to follow a “right-sided” protocol, an example of which is when the contrast bolus is chased with a 50/50 contrast-saline flush to opacify the right side of the heart. Despite the limitations mentioned, CT often better describes anatomic features of tricuspid valve disease compared with MRI and echocardiography, particularly in the setting of cardiac devices (Fig. 5). CT well delineates tricuspid valve (TV) anomalies such as Ebstein’s anomaly. Reflux of contrast into the inferior vena cava and hepatic veins indicates TR almost invariably but has only modest correlation with TR severity [47, 48].
Tricuspid regurgitation. Contrast-enhanced retrospectively gated cardiac CT in a 79-year-old woman with TR and a pacemaker. The clinical question was whether the pacemaker leads are impinging on the TV leaflets. There was poor coaptation of the tricuspid valve (arrow) (video 1) (a). An AROA of 1.5 cm2 was measured in the 30% phase without clear impingement of the pacemaker lead (b) (video 2). Cardiac MRI confirmed a severely dilated tricuspid annulus with malcoaptation of the TV leaflets with severe (torrential) secondary TR (regurgitant volume 100 ml, regurgitant fraction 63%)
The tricuspid valve is the next frontier in transcatheter valve interventions but device development and imaging guidance is challenging. CT offers complementary information during the preprocedural planning such as the tricuspid annular structure and dimensions, the annulus’ relationship with the right coronary artery, and the sizing of the inferior vena cava [48, 49••].
The Pulmonic Valve
Similar to the tricuspid valve, the pulmonic valve (PV) can be challenging to image with transesophageal and transthoracic echocardiography due to its anterior location and limited views. Cardiac CT can be a complimentary modality to assess pulmonic stenosis etiology (supravalvular, valvular, and subvalvular), rule out other congenital malformations, and study the effects of PV disease on right ventricular size and function. In adult congenital heart disease patients and particularly tetralogy of Fallot patients, pulmonic regurgitation (PR) is an important entity with long-term deleterious effects. CT allows accurate quantitation of right ventricular size and function, albeit with radiation exposure, making it less suitable for serial follow-up. Echocardiography and MRI remain the modalities of choice to quantify PV stenosis or regurgitation.
Prosthetic Valves
CT has revolutionized the investigative workup for prosthetic valve dysfunction, particularly in mechanical valves and valves in the aortic position (Fig. 6) where echocardiography is limited by acoustic shadowing. CT is best suited for measurement of mechanical valve opening angles and retrospective acquisition yields cine images with good temporal resolution to assess occluder motion. CT also can diagnose and potentially differentiate pannus from thrombus (Fig. 7) in patients with mechanical or bioprosthetic valves. In a study of 62 patients with suspected mechanical prosthetic valve dysfunction, a definitive diagnosis could be achieved in 37 patients with 39 CT masses (22 thrombus and 17 pannus). A cutoff point of Hounsfield units ≥ 145 provided high sensitivity (87.5%) and specificity (95.5%) in discriminating pannus from thrombus. Complete lysis was more common for masses with Hounsfield units (HU) < 90 compared with those with HU 90 to 145 (100% versus 42.1%; p = 0.007) [50]. A recent meta-analysis of 17 studies in 229 patients suggested that CT and 3D transesophageal echocardiography (TEE) have higher sensitivity than do TTE and 2D TEE to detect masses causing prosthetic valve obstruction. Moreover, CT was found to more accurately differentiate the cause of prosthetic valve obstruction than does TEE [51].
Mechanical aortic valve dysfunction. An 81-year-old woman with prior aortic valve replacement 12 years earlier who presented with new dyspnea with exertion. Physical exam was significant for a diminished mechanical click. Echocardiography was consistent with prosthetic valve dysfunction with central aortic regurgitation and severely elevated mean gradient. Retrospectively gated cardiac CT was performed and showed a frozen posterior leaflet and a restricted anterior leaflet with a reduced opening angle during systole (a) (video 3). There was a hypodense mass on the aortic side of the valve with HU of 67 suggestive of thrombus (b). Thrombolytics were administered and echocardiography showed reduction of gradient. Repeated CT showed a persistently frozen posterior leaflet (c) but an improved opening angle of the anterior leaflet (video 4). Further inspection showed probable pannus on the ventricular side of the posterior leaflet with HU of 245 (d). The patient did well clinically with resolution of symptoms so surgery was not pursued but anticoagulation was intensified
Paravalvular leak (PVL) occurs in 2–12% of patients after mitral valve replacement and in 1–5% after aortic valve replacement and can cause heart failure and/or hemolytic anemia. Cardiac CT provides accurate anatomical description of the size and path of PVL and can be helpful in preoperative planning for redo surgery or percutaneous closure. In a recent study of 46 patients with PVL, the location of PVLs on CT was well matched with that noted on echocardiography and surgical inspection. PVL size measured on CT was also correlated with the regurgitant grade on echocardiography with good interobserver variability [51].
Conclusion
In conclusion, we have reviewed the role of cardiac CT in the assessment of the right and left ventricular function and size as well as valvular heart diseases. It is often a secondary and confirmatory role, when echo and CMR do not provide definite diagnosis. However, in the era of transcatheter therapeutics, there are often clear class I indications for cardiac CT in valvular heart disease, primarily in TAVR and TMVR planning as well as low-gradient low-flow aortic stenosis.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Al-Mallah MH, Aljizeeri A, Villines TC, Srichai MB, Alsaileek A. Cardiac computed tomography in current cardiology guidelines. J Cardiovasc Comput Tomogr. 2015;9:514–23.
Raff GL, Gallagher MJ, O’Neill WW, Goldstein JA. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552–7.
Al-Mallah MH, Ahmed AMJCCIR. Controversies in the use of fractional flow reserve form computed tomography (FFRCT) vs. coronary angiography. 2016;9:34.
Nakazato R, Arsanjani R, Achenbach S, Gransar H, Cheng VY, Dunning A, et al. Age-related risk of major adverse cardiac event risk and coronary artery disease extent and severity by coronary CT angiography: results from 15 187 patients from the International Multisite CONFIRM Study. Eur Heart J Cardiovasc Imaging. 2014;15:586–94.
Dowsley T, Al-Mallah M, Ananthasubramaniam K, Dwivedi G, McArdle B, Chow BJ. The role of noninvasive imaging in coronary artery disease detection, prognosis, and clinical decision making. Can J Cardiol. 2013;29:285–96.
Aljizeeri A, Sulaiman A, Alhulaimi N, Alsaileek A, Al-Mallah MH. Cardiac magnetic resonance imaging in heart failure: where the alphabet begins! Heart Fail Rev. 2017;22:385–99.
Rizvi A, Deano RC, Bachman DP, Xiong G, Min JK, Truong QA. Analysis of ventricular function by CT. J Cardiovasc Comput Tomogr. 2015;9:1–12.
•• Tabari A, Lo Gullo R, Murugan V, Otrakji A, Digumarthy S, Kalra M. Recent advances in computed tomographic technology: cardiopulmonary imaging applications. 2017;32:89–100. This study of 79 patients showed that cardiac CT provides accurate and reproducible LV and RV volume parameters compared with MR and can be considered a reliable alternative for patients who are not suitable to undergo MR.
Maffei E, Messalli G, Martini C et al. Left and right ventricle assessment with cardiac CT: validation study vs. cardiac MR. 2012;22:1041–1049.
Busch S, Johnson TRC, Wintersperger BJ et al. Quantitative assessment of left ventricular function with dual-source CT in comparison to cardiac magnetic resonance imaging: initial findings. 2008;18:570–575.
Asferg C, Usinger L, Kristensen TS, Abdulla J. Accuracy of multi-slice computed tomography for measurement of left ventricular ejection fraction compared with cardiac magnetic resonance imaging and two-dimensional transthoracic echocardiography: a systematic review and meta-analysis. Eur J Radiol. 2012;81:e757–62.
Arsanjani R, Berman DS, Gransar H et al. Left ventricular function and volume with coronary ct angiography improves risk stratification and identification of patients at risk for incident mortality: results from 7758 patients in the prospective multinational CONFIRM observational cohort study. 2014;273:70–77.
Gebhard C, Buechel RR, Stahli BE, et al. Impact of age and sex on left ventricular function determined by coronary computed tomographic angiography: results from the prospective multicentre CONFIRM study. Eur Heart J Cardiovasc Imaging. 2017;18:990–1000.
Ooijen PM van, Jonge GJ de, Oudkerk M. Informatics in radiology: postprocessing pitfalls in using CT for automatic and semiautomatic determination of global left ventricular function. 2012;32:589–599.
Chinnaiyan KM, Peyser P, Goraya T, Ananthasubramaniam K, Gallagher M, DePetris A, et al. Impact of a continuous quality improvement initiative on appropriate use of coronary computed tomography angiography. Results from a multicenter, statewide registry, the Advanced Cardiovascular Imaging Consortium. J Am Coll Cardiol. 2012;60:1185–91.
Al-Mallah MH, Aljizeeri A, Alsaileek A, Alharthi M. Routine low-radiation-dose coronary computed tomography angiography. European Heart Journal Supplements. 2014;16:B12–6.
Nakazato R, Tamarappoo BK, Smith TW, Cheng VY, Dey D, Shmilovich H, et al. Assessment of left ventricular regional wall motion and ejection fraction with low-radiation dose helical dual-source CT: comparison to two-dimensional echocardiography. J Cardiovasc Comput Tomogr. 2011;5:149–57.
•• Yang Y, Yam Y, Chen L, Aljizeeri A, Aliyary Ghraboghly S, al-Harbi I, et al. Assessment of left ventricular ejection fraction using low radiation dose computed tomography. J Nucl Cardiol. 2016;23:414–21 The results of our study suggest that low-dose CT LVEF protocol is feasible, accurate, and fast while delivering a lower radiation dose than traditional RNA.
Gopalan D. Right heart on multidetector CT. Br J Radiol 2011;84 Spec No 3:S306-S323.
Voges I, Al-Mallah MH, Scognamiglio G, Di Salvo G. Right heart-pulmonary circulation unit in congenital heart diseases. Heart Fail Clin. 2018;14:283–95.
Karamitsos TD, Hudsmith LE, Selvanayagam JB, Neubauer S, Francis JM. Operator induced variability in left ventricular measurements with cardiovascular magnetic resonance is improved after training. J Cardiovasc Magn Reson. 2007;9:777–83.
Mahrholdt H, Wagner A, Holly TA, Elliott MD, Bonow RO, Kim RJ, et al. Reproducibility of chronic infarct size measurement by contrast-enhanced magnetic resonance imaging. Circulation. 2002;106:2322–7.
Valente AM, Cook S, Festa P, et al. Multimodality imaging guidelines for patients with repaired tetralogy of fallot: a report from the AmericanSsociety of Echocardiography: developed in collaboration with the Society for Cardiovascular Magnetic Resonance and the Society for Pediatric Radiology. J Am Soc Echocardiogr. 2014;27:111–41.
Al-Mallah M, Kwong RY. Clinical application of cardiac CMR. Rev Cardiovasc Med. 2009;10:134–41.
Jamiel A, Ebid M, Ahmed AM, Ahmed D, Al-Mallah MH. The role of myocardial viability in contemporary cardiac practice. Heart Fail Rev. 2017;22:401–13.
Al-Mallah MH, Shareef MN. The role of cardiac magnetic resonance imaging in the assessment of non-ischemic cardiomyopathy. Heart Fail Rev. 2011;16:369–80.
Tandri H, Calkins H. MR and CT imaging of arrhythmogenic cardiomyopathy. Cardiac electrophysiology clinics. 2011;3:269–80.
Doherty JU, Kort S, Mehran R, Schoenhagen P, Soman P. ACC/AATS/AHA/ASE/ASNC/HRS/SCAI/SCCT/SCMR/STS 2017 Appropriate Use Criteria for Multimodality Imaging in Valvular Heart Disease. J Am Coll Cardiol. 2017;70:1647 LP–1672.
Habis M, Daoud B, Roger VL, Ghostine S, Caussin C, Ramadan R, et al. Comparison of 64-slice computed tomography planimetry and Doppler echocardiography in the assessment of aortic valve stenosis. The Journal of heart valve disease. 2007;16:216–24.
Ropers D, Ropers U, Marwan M, Schepis T, Pflederer T, Wechsel M, et al. Comparison of dual-source computed tomography for the quantification of the aortic valve area in patients with aortic stenosis versus transthoracic echocardiography and invasive hemodynamic assessment. Am J Cardiol. 2009;104:1561–7.
Nasir K, Katz R, Al-Mallah M, et al. Relationship of aortic valve calcification with coronary artery calcium severity: the Multi-Ethnic Study of Atherosclerosis (MESA). J Cardiovasc Comput Tomogr. 2010;4:41–6.
Bonow RO, Brown AS, Gillam LD et al. ACC/AATS/AHA/ASE/EACTS/HVS/SCA/SCAI/SCCT/SCMR/STS 2017 Appropriate Use Criteria for the Treatment of Patients With Severe Aortic Stenosis. J Am Coll Cardiol 2017:24131.
•• Clavel M-A, Malouf J, Messika-Zeitoun D, Araoz PA, Michelena HI, Enriquez-Sarano M. Aortic valve area calculation in aortic stenosis by CT and Doppler echocardiography. JACC Cardiovasc Imaging. 2015;8:248–57 The study showed that computed tomography is superior to echocardiography for measuring the left ventricular outflow tract and calculating the aortic valve area with regard to hemodynamic correlations and survival outcome prediction after a diagnosis of aortic stenosis.
Clavel M-A, Messika-Zeitoun D, Pibarot P, Aggarwal SR, Malouf J, Araoz PA, et al. The complex nature of discordant severe calcified aortic valve disease grading: new insights from combined Doppler echocardiographic and computed tomographic study. J Am Coll Cardiol. 2013;62:2329–38.
Delgado V, Clavel M-A, Hahn RT, et al. How do we reconcile echocardiography, computed tomography, and hybrid imaging in assessing discordant grading of aortic stenosis severity? JACC Cardiovasc Imaging. 2019;12:267–82.
Pawade T, Clavel M-A, Tribouilloy C, et al. Computed tomography aortic valve calcium scoring in patients with aortic stenosis. Circulation Cardiovascular imaging. 2018;11:e007146.
Binder RK, Webb JG, Willson AB, Urena M, Hansson NC, Norgaard BL, et al. The impact of integration of a multidetector computed tomography annulus area sizing algorithm on outcomes of transcatheter aortic valve replacement: a prospective, multicenter, controlled trial. J Am Coll Cardiol. 2013;62:431–8.
Khalique OK, Hahn RT, Gada H et al. Quantity and location of aortic valve complex calcification predicts severity and location of paravalvular regurgitation and frequency of post-dilation after balloon-expandable transcatheter aortic valve replacement. J Am Coll Cardiol Intv 2014.
Ko SM, Park JH, Shin JK, Kim JS. Assessment of the regurgitant orifice area in aortic regurgitation with dual-source CT: comparison with cardiovascular magnetic resonance. Journal of Cardiovascular Computed Tomography. 2015;9:345–53.
Lembcke A, Durmus T, Westermann Y, Geigenmueller A, Claus B, Butler C, et al. Assessment of mitral valve stenosis by helical MDCT: comparison with transthoracic Doppler echocardiography and cardiac catheterization. Am J Roentgenol. 2011;197:614–22.
Messika-Zeitoun D, Serfaty J-M, Laissy J-P, Berhili M, Brochet E, Iung B, et al. Assessment of the mitral valve area in patients with mitral stenosis by multislice computed tomography. J Am Coll Cardiol. 2006;48:411–3.
Guerrero M, Dvir D, Himbert D, Urena M, Eleid M, Wang DD, et al. Transcatheter mitral valve replacement in native mitral valve disease with severe mitral annular calcification: results from the first multicenter global registry. J Am Coll Cardiol Intv. 2016;9:1361–71.
Cavalcante JL, Al-Mallah M, Arida M, Garcia-Sayan E, Chattahi J, Ananthasubramaniam K. The relationship between spontaneous echocontrast, transesophageal echocardiographic parameters, and blood hemoglobin levels. J Am Soc Echocardiogr. 2008;21:868–72.
Romero J, Husain SA, Kelesidis I, Sanz J, Medina HM, Garcia MJ. Detection of left atrial appendage thrombus by cardiac computed tomography in patients with atrial fibrillation. 2013;6:185–194.
Arnous S, Killeen RP, Martos R, Quinn M, McDonald K, Dodd JD. Quantification of mitral regurgitation on cardiac computed tomography. J Comput Assist Tomogr. 2011;35:625–30.
Guo Y-K, Yang Z-G, Ning G, Rao L, Dong L, Pen Y, et al. Isolated mitral regurgitation: quantitative assessment with 64-section multidetector CT—comparison with MR imaging and echocardiography. Radiology. 2009;252:369–76.
Groves AM, Win T, Charman SC, Wisbey C, Pepke-Zaba J, Coulden RA. Semi-quantitative assessment of tricuspid regurgitation on contrast-enhanced multidetector CT. Clin Radiol. 2004;59:715–9.
Hahn RT, George I, Kodali SK et al. Early single-site experience with transcatheter tricuspid valve replacement. JACC Cardiovasc Imaging 2018:2784.
•• Praz F, Khalique OK, Dos Reis Macedo LG, Pulerwitz TC, Jantz J, Wu IY, et al. Comparison between three-dimensional echocardiography and computed tomography for comprehensive tricuspid annulus and valve assessment in severe tricuspid regurgitation: implications for tricuspid regurgitation grading and transcatheter therapies. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2018;31:1190–1202.e3 This study showed that in patients with severe tricuspid regurgitation, semiautomated indirect planimetry results in high agreement between TEE and CT for TA sizing and measurement of the tricuspid valve area.
Gündüz S, Özkan M, Kalçik M, Gürsoy OM, Astarcioğlu MA, Karakoyun S, Aykan AÇ, Biteker M, Gökdeniz T, Kaya H, Yesin M, Duran NE, Sevinç D, Güneysu T Sixty-four-section cardiac computed tomography in mechanical prosthetic heart valve dysfunction: thrombus or pannus. Circulation: Cardiovascular Imaging 2015.
Kim JY, Suh YJ, Han K, Kim YJ, Choi BW. Diagnostic value of advanced imaging modalities for the detection and differentiation of prosthetic valve obstruction: a systematic review and meta-analysis. JACC Cardiovasc Imaging 2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiac Computed Tomography
Rights and permissions
About this article
Cite this article
Malahfji, M., Al-Mallah, M.H. Cardiac CT Assessment of Right and Left Ventricular and Valvular Function. Curr Cardiovasc Imaging Rep 12, 23 (2019). https://doi.org/10.1007/s12410-019-9495-3
Published:
DOI: https://doi.org/10.1007/s12410-019-9495-3