Abstract
Objectives
To identify CT findings in chronic hypersensitivity pneumonitis (cHP) associated with survival.
Material and methods
Two thoracic radiologists assessed CT scans for specific imaging findings and patterns in 132 subjects with cHP. Survival analyses were performed.
Results
The majority of subjects had an inconsistent with usual interstitial pneumonitis pattern on CT (55.3%,73/132). Hypersensitivity pneumonitis (HP) diagnosis on CT was less common in those with fibrosis (66.1%, 74/112) than those without fibrosis (85%,17/20). Smoking was associated with a lower prevalence of HP on CT (p=0.04). CT features of pulmonary fibrosis, especially traction bronchiectasis (HR 8.34, 95% CI 1.98–35.21) and increased pulmonary artery (PA)/aorta ratio (HR 2.49, 95% CI 1.27–4.89) were associated with worse survival, while ground-glass opacity (HR 0.31, 95% CI 0.12–0.79) was associated with improved survival. Survival association with imaging was less pronounced after adjustment for gender, age and physiology score.
Conclusions
A substantial proportion of cHP cases have a non-HP-like appearance. Ground-glass opacity, pulmonary fibrosis features and elevated PA/aorta ratio on CT likely reflect varying degrees of disease severity in cHP and may inform future clinical prediction models.
Key Points
• A substantial proportion of subjects with chronic HP have a UIP-like pattern.
• A UIP pattern in HP may be potentiated by smoking.
• A diagnosis of HP should not be excluded based solely on CT appearance.
• CT fibrosis and increased PA/aorta ratio signal worse survival.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hypersensitivity pneumonitis (HP) is caused by inhalation of organic and/or inorganic antigens that results in lung inflammation. While a two-category cluster classification system for HP has been proposed based on clinical presentation, pulmonary function and imaging, it has not been validated and the classic three-tier classification (acute, subacute and chronic) is still commonly used in clinical practice [1]. With recurrent or chronic exposure, patients may develop pulmonary fibrosis, including CT imaging findings consistent with usual interstitial pneumonia (UIP). While the patterns associated with subacute disease are well established, heterogeneity exists among the reported imaging patterns of chronic HP [2,3,4,5,6,7]. Such heterogeneity may reflect differences in how HP diagnosis was achieved and/or how chronic HP was defined as no consensus guidelines have been established [2, 6, 8]. While the presence of pulmonary fibrosis has been shown to predict early mortality in chronic HP, other imaging variables associated with survival have been incompletely characterised [2, 9,10,11,12].
Among imaging findings with potential clinical relevance are those commonly observed in the presence of pulmonary hypertension. This co-morbid condition is a well-described complication of pulmonary fibrosis. Recent studies showed that pulmonary hypertension complicates HP in a substantial minority (20–50%) of symptomatic patients and was associated with worse survival [8, 9]. The impact of CT findings of pulmonary hypertension (specifically, pulmonary artery [PA] size and PA/aorta size ratio) on survival in patients with chronic HP are unknown. Though a seemingly trivial issue, as PA enlargement on CT has long been associated with pulmonary hypertension, previous studies have failed to show an association between PA size and pulmonary hypertension in the setting of pulmonary fibrosis [13,14,15].
The purposes of this study were to:
-
1.
Evaluate the imaging patterns of chronic HP in a large cohort of patients,
-
2.
Assess whether pulmonary imaging findings were associated with survival, and
-
3.
Assess whether CT findings of pulmonary hypertension were associated with survival.
We hypothesised that among subjects with chronic HP, imaging findings of pulmonary fibrosis, UIP pattern and increased PA size and PA/aorta ratio would be associated with worse survival.
Methods
Study population
We searched our interstitial lung disease registry for patients with chronic HP from 2006–2015. This registry is approved by our Institutional Review Board (#14163A) and informed consent was obtained from all subjects included in the study. The diagnosis of chronic HP was achieved through a multidisciplinary approach including input from pulmonologists, dedicated chest radiologists and pathologists, all with expertise in the diagnosis of interstitial lung diseases, according to American Thoracic Society criteria [16].
Clinical data
We collected all pertinent clinical data from the first clinic visit using electronic medical records (EMRs). Patient demographics, surgical and medical history, tobacco use, occupational history, environmental antigen exposure history, medications, physical examination findings, pertinent laboratory results, thoracic pathology findings, echocardiographic data and pulmonary functional data were abstracted.
HRCT evaluation
The earliest available chest CT of diagnostic quality for each subject was scored by two thoracic radiologists (JHC and SMM, 11 and 32 years of imaging experience, respectively) by consensus. Outside hospital CT scans were also eligible for scoring if they were of diagnostic quality. CT scans were considered of diagnostic quality if they included all of the lung, were free of motion artifact severe enough to obscure underlying pulmonary architecture and were of thin-slice reconstruction or acquisition (1.5 mm or less); axial acquisition or helical CT acquisition were both considered adequate. The extent of reticulation, ground-glass opacity, honeycombing, traction bronchiectasis and mosaic attenuation (on inspiration) or air-trapping (on expiratory images) were scored to the closest 5%. The predominant axial (central or peribronchovascular, peripheral or diffuse) and zonal (upper, mid, lower or diffuse) distributions were abstracted. The lungs were considered fibrotic if there was presence of reticulation with traction bronchiectasis, traction bronchiolectasis and/or honeycombing [17]. The largest main PA diameter was also measured in the axial plane at the level of the right pulmonary artery bifurcation [18]; the ascending aorta was also measured on the same image orthogonal to the oblique course of the ascending aorta.
The UIP pattern on CT was scored according to recent guidelines: UIP, possible UIP and inconsistent with UIP (Figs. 1, 2 and 3) [19]. If the CT pattern was not definitively UIP, the most likely CT interstitial pneumonia pattern was also recorded (with level of confidence) including but not exclusive to HP, nonspecific interstitial pneumonitis (NSIP), sarcoidosis, obliterative bronchiolitis and pleuroparenchymal fibroelastosis. Level of confidence in diagnosis was scored as possible, probable or definite depending on the likelihood of the diagnosis (possible: 1–50% likelihood of diagnosis, probable: 51–89% likelihood of diagnosis, and definite: greater than 90% likelihood of diagnosis). Given the focus on HP subjects, we specifically defined the confidence of HP patterns based on CT appearance [6]. A definite HP pattern was defined as profuse centrilobular nodules or widespread mosaic attenuation and air trapping with relative basal sparing. Probable HP was defined as a moderate degree of centrilobular nodularity, mosaic attenuation or air-trapping in all lobes. Possible HP was defined as any combination of the CT findings associated with a definite or probable HP pattern but not meeting the criteria for probable or definite disease.
A 53-year-old woman with chronic hypersensitivity pneumonitis and an inconsistent with usual interstitial pneumonitis (UIP) pattern on CT. Axial (A) and coronal (B) images from chest CT demonstrate axially central and zonally upper lung preponderant disease characterised by ground-glass opacity, mosaic attenuation and reticulation. Findings are diagnostic of an inconsistent with UIP pattern given substantial ground-glass opacity and central/upper lung preponderance
A 42-year-old woman with chronic hypersensitivity pneumonitis and a possible usual interstitial pneumonitis (UIP) pattern on CT. Axial (A) and coronal (B) images from chest CT demonstrate peripheral and basilar predominant pulmonary fibrosis characterised by reticulation and traction bronchiolectasis without subpleural honeycombing consistent with a possible UIP pattern
A 49-year-old woman with chronic hypersensitivity pneumonitis and a usual interstitial pneumonitis (UIP) pattern on CT. Axial (A) and coronal (B) images from chest CT demonstrate peripheral and basilar predominant pulmonary fibrosis characterised by reticulation, traction bronchiectasis, traction bronchiolectasis and subpleural honeycombing consistent with UIP
Statistical analysis
Continuous data were presented as means with standard deviation and categorical data as counts with percentage. Means were compared using a two-tailed Student’s t-test and proportions were compared using a Chi-square test. Correlation assessments were pursued using a general linear model. Survival analysis was performed using univariable and multivariable Cox proportional hazard regression and unadjusted log rank testing. Iterative multivariable Cox regression models were constructed to assess individual components of UIP, including reticulation, traction bronchiectasis and honeycombing, as these variables are collinear and cannot be assessed together in a single model. The first model was adjusted for independent CT predictors of mortality in univariate analysis, while the second model included CT predictors plus gender, age and physiology (GAP) score. Survival was displayed graphically using the Kaplan-Meier survival estimator and was defined as time from diagnosis to lung transplantation or death. Statistical evaluation was performed using Stata (StataCorp. 2015. Release 14. College Station, TX, USA).
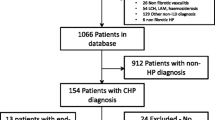
Results
Of the 1,250 patients in our ILD registry, there were 132 subjects who were diagnosed with HP based on a multidisciplinary ILD evaluation. The average age of the cohort was 62.1 (±11.5) years (Table 1) with a slight female predominance (60.6%). Most of the cohort was comprised of non-Hispanic whites (84.8%) with fewer Hispanic (7.6%), African American (5.3%) and Asian (2.2%) subjects. Approximately half of the subjects were ‘ever smokers’ (56.1%). The likely antigen could not be identified in approximately one-third of the subjects.
CT findings
Most subjects (112/132, 84.8%) had findings of fibrotic disease on CT. Those with fibrosis were older than those without fibrosis (64.0 ± 10.8 years vs. 52.2 ± 9.1 years; p<0.001), but groups were similar with regard to sex or smoking history (Table 2). In those with reticulation, an average of 22 ± 12.4% of the lung was involved. In those with non-fibrotic disease, ground-glass opacity was present in half (10/20) with 27.4 ± 30.0% of lung involvement, and air-trapping was present in 80% (16/20) of subjects with 19.6 ± 9.0% of lung involvement. There was no difference in prevalence or extent of lung involvement with regard to ground-glass opacity or air-trapping among fibrotic subjects as compared to the non-fibrotic subjects. In those with fibrotic disease, ground-glass opacity was present in 29.5% (33/112) with 23.9 ± 18.5% of lung involvement and air-trapping was present in 63.4% (71/112) of subjects with 16.8 ± 11.1% of lung involvement.
Centrilobular nodularity was more common in those without fibrosis (9/20, 45.0%) as compared to those with fibrosis (13/112, 11.6%) [p=0.001]. In those with fibrosis, honeycombing was present in 57/112 with an average of 4.2 ± 5.5% of lung involvement; traction bronchiectasis was ubiquitous in those with fibrosis, affecting 12.8 ± 8.4% of the bronchial tree.
Distribution of disease varied between those with and without fibrotic disease (p<0.001 for both axial and zonal distribution). In those without fibrosis, the axial distribution was always diffuse and the zonal distribution was most often diffuse (14/20, 70.0%). In those with fibrosis, axially peripheral (58/112, 51.8%) and zonally lower (60/112, 53.6%) distributions were most common, followed by diffuse axial (43/112, 38.4%) and zonal (30/112, 26.8%) distributions. Only a small proportion of subjects had an upper lung preponderant distribution in the fibrotic setting (19/112, 17.0%). There was no significant difference in the size of the PA or PA/aorta ratio in those with and without fibrosis (PA diameter 29.1 ± 4.4 mm vs. 28.4 ± 4.2 mm, PA/aorta ratio 0.866 ± 0.111 vs. 0.872 ± 0.156, respectively).
HP pattern on CT relative to UIP diagnosis in those with pulmonary fibrosis
The majority of our subjects with pulmonary fibrosis had an inconsistent with UIP pattern (65.2%, 73/112); however, a substantial minority of subjects had a UIP (18.8%, 21/112) or possible UIP (9.8%, 11/112) pattern on CT. In 6.3% of subjects (7/112), the CT pattern could not be scored within the confines of current UIP classification guidelines. The most common finding on CT scans considered inconsistent with UIP was the presence of air-trapping (78.1%, 57/73) followed by the presence of ground-glass opacity (49.3%, 36/73), diffuse nodules (21.9%, 16/73), and upper lung preponderance (24.7%, 18/73).
Single best imaging pattern in HP cases
With regard to the single best diagnosis based on imaging pattern, those without fibrotic disease had an HP pattern in the majority of cases (85%, 17/20), with the remainder demonstrating a CT pattern that was nonspecific (15%, 3/20). Those with fibrosis most often had an HP CT pattern (66.1%, 74/112), followed by a UIP pattern (25.0%, 28/112). There was no significant difference in subjects with an HP CT pattern as compared to those without an HP pattern relative to smoking history, age or sex (Table 2). However, when only considering those with a high confidence CT pattern (probable or definite), there was a higher proportion of never smokers with an HP pattern on CT as compared to smokers or former smokers with an HP pattern on CT (81.1% (30/37) vs. 60.5% (26/43); p=0.04) (Table 2).
Survival and CT findings
On univariate analysis (Table 4), the presence of ground-glass opacity was associated with improved survival (HR 0.31, 95% CI 0.12–0.79). Each increase of 5% in reticulation was associated with a 6% increase in mortality risk (HR 1.06, 95% CI 1.03–1.08). Other CT characteristics that were associated with an increase in mortality risk included the presence of traction bronchiectasis (HR 8.34, 95% CI 1.98–35.21), honeycombing (HR 2.47, 95% CI 1.25–4.87), UIP CT pattern (HR 1.36, 95% CI 1.01–1.82) and PA/aorta ratio greater than 0.9 (HR 2.49, 95% CI 1.27–4.89) (Table 3, Figs. 4 and 5). PA dilation (not corrected for aortic size) and distribution of lung disease were not significant predictors of survival.
Kaplan-Meier survival curves for CT findings of pulmonary fibrosis. (A) Kaplan-Meier survival curves for presence and absence of reticulation show that those with reticulation had significantly worse survival than those without reticulation (log rank test p-value 0.016). (B) Kaplan-Meier survival curves for presence and absence of traction bronchiectasis show that those with traction bronchiectasis had significantly worse survival than those without traction bronchiectasis (log rank test p-value <0.001). (C) Kaplan-Meier survival curves for presence and absence of honeycombing show that those with honeycombing had significantly worse survival than those without honeycombing (log rank test p-value 0.007)
Increasing reticulation (HR 1.04; 95% CI 1.02–1.07) and traction bronchiectasis (HR 5.88; 95% CI 1.39–24.90) were independent predictors of reduced survival after adjustment for the presence of ground-glass opacities and PA/aorta ratio, while the presence of honeycombing was not (HR1.51; 95% 0.74–3.07) (Table 4). In the same model, PA/aorta ratio remained an independent predictor of reduced survival (HR 2.36; 95% CI 1.20–4.63). None of the UIP components nor the PA/aorta ratio remained independent predictors of survival after GAP score was added to the multivariable model. However, GAP score was consistently associated with survival regardless of which finding of fibrosis (reticulation, traction bronchiectasis or honeycombing) was included in the model (HR 1.44–1.53, 95% CI 1.14–1.86).
Correlation of PA/aorta ratio with parameters associated with pulmonary hypertension
In regard to clinical or laboratory parameters that are associated with pulmonary hypertension, 120 of the 132 subjects had N-terminal pro b-type natriuretic peptide (NT-proBNP) values. In 95 of the 132 subjects, right heart catheter angiography, echocardiography or both were performed. Of these 95 subjects, in only 38 subjects could right ventricle systolic pressure (RVSP) values be quantitatively estimated on echocardiography, and in only nine of these 38 subjects was mean pulmonary artery pressure (mPAP) estimated on cardiac catheter angiography. There was a positive but weak correlation between elevated NT-proBNP (>125) and CT measurement of PA/Aorta (>0.9) in our cohort (r=0.232; p=0.011). There was no statistically significant correlation between elevated echocardiography measurement of RVSP (>40 mmHg) and CT measurement of PA/Aorta (>0.9) (r=0.167; p=0.331). Due to the small number of subjects with mPAP, further analysis in regard to this variable was not possible.
Discussion
The main goals of this study were to determine the imaging patterns of chronic HP and assess whether pulmonary parenchymal and arterial imaging findings were associated with survival. The main findings of this study were as follows: (1) a substantial minority (approximately 1/4th) of subjects with chronic HP had a UIP or possible UIP pattern on CT; (2) in the setting of high-confidence CT patterns, smoking history was associated with a 20% lower rate of an HP pattern on CT; (3) those with fibrotic disease most often had a peripheral and basilar distribution as opposed to the near universal axially and zonally diffuse distributions that were present in those without fibrosis; and (4) findings of pulmonary fibrosis and increased PA/aorta ratio were associated with worse survival, but this association was less pronounced after adjustment for GAP score.
Many previous studies have evaluated the CT pattern in chronic HP; ground-glass opacity, centrilobular nodularity and air-trapping or mosaic attenuation are well-known findings in HP [6, 17, 20, 21]. However, there is a substantial proportion of cases in which chronic HP cannot be differentiated from other types of pulmonary fibrosis based on CT [6]. Many cases of chronic HP have been shown to mimic UIP on imaging, and differentiation from idiopathic pulmonary fibrosis (IPF) must be achieved based on multidisciplinary review [6, 17, 22]. Our study was in agreement with the literature; one-fifth of subjects with chronic HP had a UIP pattern on CT.
The association between smoking history and a lower prevalence of an HP pattern on CT was not entirely surprising. Previous evidence suggests that smoking is protective against the development of HP, unlike the association between smoking and an increased risk of IPF [10, 23]. Many have postulated that this is due to the mildly immunosuppressive nature of cigarette smoke on the lungs, likely due to nicotine [24, 25]. However, there is evidence that suggests that smokers who do develop HP are more likely to develop chronic disease with worse survival as compared to non-smokers [26]. The modest immunosuppressant effect of cigarette smoke may not be able to alter the natural disease course in patients who are genetically predisposed to develop severe, fibrotic HP, but may mitigate the inflammatory changes in those less predisposed to developing severe disease. Alternatively, smoking may have a bitemporal effect based on the chronicity of exposure: early on, smoking may protect from HP, but with prolonged exposure, it may potentiate the fibrosis, as suggested in a study using a murine model [27]. Our results raise a third possibility: chronic HP cases in smokers may be misdiagnosed as IPF. Smoking in HP may lead to a CT pattern that is not typical for HP, increasing the risk of misdiagnosis. Given that lung biopsy is becoming less common and that the causative antigen is not identified in up to half of HP cases, an atypical HP pattern on CT could result in an incorrect diagnosis even if achieved using multidisciplinary discussion [19, 28].
The distribution of disease in chronic HP has not been definitively established, with conflicting reports in the literature [2, 6, 29]. Upper zone parenchymal lung disease is commonly associated with HP and is one of the most helpful findings to differentiate HP from UIP/IPF [6]. However, the current study and previous work show that only a small proportion of chronic HP cases have upper lung zone preponderance [2, 6, 29]. One study showed that only 11% of those with fibrotic HP had upper lung preponderant disease [6]. An older study showed that the distribution of HP was most often basilar and peripheral preponderant, though relative basilar sparing of the lower lung zone was present in approximately half of subjects [8]. Others showed an almost ubiquitously diffuse axial and zonal distribution in HP independent of chronicity [2]. The variability in the reported distribution of chronic HP on CT is likely due to diverse inclusion criteria in the different studies. Chronic HP is often defined either as disease of prolonged duration (6–12 months) or in which frank fibrosis is evident on imaging or pathology. The current study implies that disease distribution may evolve as inflammatory HP progresses to fibrotic disease, though our study was not optimized to explore this possibility. Other interstitial processes can also change from a non-UIP imaging pattern into a more UIP-like pattern, and underlines the need to examine the earliest CT scan available to accurately diagnose interstitial lung disease [6, 30,31,32].
We also found that CT findings of pulmonary fibrosis and UIP CT pattern were associated with worse survival in HP, with traction bronchiectasis having the greatest effect size. Previous data have also shown that fibrosis on CT predicts worse survival [2, 9,10,11,12]. Ground-glass opacity on CT was also associated with improved survival and may be a marker for reversible lung inflammation as opposed to end-stage lung fibrosis. Our findings likely reflect varying disease severity, as survival associations for reticulation, traction bronchiectasis and PA/aorta ratio were no longer significant after adjustment for GAP score. The presence of ground-glass opacity and PA/aorta ratio did retain a marginal survival association after GAP score adjustment, suggesting these variables may inform future clinical prediction models derived using larger cohorts.
We postulate that the association between PA enlargement and mortality in our study is due transitively to the well-established relationship between PA size on CT and chronic pulmonary hypertension [33, 34]. However, there is poor correlation between pulmonary hypertension and PA size on CT in patients with pulmonary fibrosis [13,14,15]. Therefore, one must be cautious in assuming that PA enlargement is simply a marker of pulmonary hypertension given the high prevalence of pulmonary fibrosis in the current study. Our study showed a significant but weak correlation between PA/aorta ratio and serum NT-proBNP values, but no correlation between PA/aorta ratio and elevated RVSP on echocardiography, suggesting that though PA size may partially affect survival by its transitive association with pulmonary hypertension, there may be other pathophysiological factors associated with PA size that alter survival.
Our study was limited by its retrospective design and could only assess association, not causation. Also, though our study included a larger chronic HP cohort compared to other studies in the literature, the power of the study remains limited. Third, we were unable to standardise CT protocols, as some scans were not performed at our medical centre. However, we only included CT scans of high diagnostic quality for assessment of ILD in this study. Finally, our study was performed at a referral centre for ILD, which may limit the generalisability of our findings.
In conclusion, we showed that a UIP pattern on CT was not uncommon in chronic HP. This suggests that a diagnosis of HP should not be excluded based solely on imaging. Smoking may also augment the CT appearance of chronic HP. More research is necessary to explain the sometimes paradoxical, effect of smoking in HP. Our study also showed that the distribution of lung disease in those with and without CT fibrosis were different (diffuse in non-fibrotic disease with a peripheral and basilar distribution in fibrotic disease); we postulate inflammation in HP may be diffuse early in disease but that recurrent inflammation may affect the lungs more asymmetrically as HP progresses. A study that systematically assesses the pattern of HP over time in individual patients is necessary before any definitive conclusions can be made in this regard. Finally, CT findings of pulmonary fibrosis, ground-glass opacity and increased PA/aorta ratio were associated with differential survival risk and likely reflect varying degrees of disease severity based on multivariable modelling. The relationship between survival and CT features of HP, along with PA size and pulmonary hypertension, should be explored in larger studies with adequate power to detect smaller differences in survival risk.
References
Lacasse Y, Selman M, Costabel U et al (2009) Classification of hypersensitivity pneumonitis: a hypothesis. Int Arch Allergy Immunol 149:161–166
Tateishi T, Ohtani Y, Takemura T et al (2011) Serial high-resolution computed tomography findings of acute and chronic hypersensitivity pneumonitis induced by avian antigen. J Comput Assist Tomogr 35:272–279
Remy-Jardin M, Remy J, Wallaert B, Muller NL (1993) Subacute and chronic bird breeder hypersensitivity pneumonitis: sequential evaluation with CT and correlation with lung function tests and bronchoalveolar lavage. Radiology 189:111–118
Chung MH, Edinburgh KJ, Webb EM, McCowin M, Webb WR (2001) Mixed infiltrative and obstructive disease on high-resolution CT: differential diagnosis and functional correlates in a consecutive series. J Thorac Imaging 16:69–75
Franquet T, Hansell DM, Senbanjo T, Remy-Jardin M, Muller NL (2003) Lung cysts in subacute hypersensitivity pneumonitis. J Comput Assist Tomogr 27:475–478
Silva CI, Muller NL, Lynch DA et al (2008) Chronic hypersensitivity pneumonitis: differentiation from idiopathic pulmonary fibrosis and nonspecific interstitial pneumonia by using thin-section CT. Radiology 246:288–297
Selman M (2004) Hypersensitivity pneumonitis: a multifaceted deceiving disorder. Clin Chest Med 25:vi
Lynch DA, Newell JD, Logan PM, King TE Jr, Muller NL (1995) Can CT distinguish hypersensitivity pneumonitis from idiopathic pulmonary fibrosis? AJR Am J Roentgenol 165:807–811
Hanak V, Golbin JM, Hartman TE, Ryu JH (2008) High-resolution CT findings of parenchymal fibrosis correlate with prognosis in hypersensitivity pneumonitis. Chest 134:133–138
Mooney JJ, Elicker BM, Urbania TH et al (2013) Radiographic fibrosis score predicts survival in hypersensitivity pneumonitis. Chest 144:586–592
Vourlekis JS, Schwarz MI, Cherniack RM et al (2004) The effect of pulmonary fibrosis on survival in patients with hypersensitivity pneumonitis. Am J Med 116:662–668
Oliveira RK, Pereira CA, Ramos RP et al (2014) A haemodynamic study of pulmonary hypertension in chronic hypersensitivity pneumonitis. Eur Respir J 44:415–424
Devaraj A, Wells AU, Meister MG, Corte TJ, Wort SJ, Hansell DM (2010) Detection of pulmonary hypertension with multidetector CT and echocardiography alone and in combination. Radiology 254:609–616
Zisman DA, Karlamangla AS, Ross DJ et al (2007) High-resolution chest CT findings do not predict the presence of pulmonary hypertension in advanced idiopathic pulmonary fibrosis. Chest 132:773–779
Tan RT, Kuzo R, Goodman LR, Siegel R, Haasler GB, Presberg KW (1998) Utility of CT scan evaluation for predicting pulmonary hypertension in patients with parenchymal lung disease Medical College of Wisconsin Lung Transplant Group. Chest 113:1250–1256
Travis WD, Costabel U, Hansell DM et al (2013) An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med 188:733–748
Sahin H, Brown KK, Curran-Everett D et al (2007) Chronic hypersensitivity pneumonitis: CT features comparison with pathologic evidence of fibrosis and survival. Radiology 244:591–598
Truong QA, Massaro JM, Rogers IS et al (2012) Reference values for normal pulmonary artery dimensions by noncontrast cardiac computed tomography: the Framingham Heart Study. Circ Cardiovasc Imaging 5:147–154
Raghu G, Collard HR, Egan JJ et al (2011) An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 183:788–824
Hansell DM, Wells AU, Padley SP, Muller NL (1996) Hypersensitivity pneumonitis: correlation of individual CT patterns with functional abnormalities. Radiology 199:123–128
Patel RA, Sellami D, Gotway MB, Golden JA, Webb WR (2000) Hypersensitivity pneumonitis: patterns on high-resolution CT. J Comput Assist Tomogr 24:965–970
Adler BD, Padley SP, Muller NL, Remy-Jardin M, Remy J (1992) Chronic hypersensitivity pneumonitis: high-resolution CT and radiographic features in 16 patients. Radiology 185:91–95
Hanak V, Golbin JM, Ryu JH (2007) Causes and presenting features in 85 consecutive patients with hypersensitivity pneumonitis. Mayo Clin Proc 82:812–816
Nizri E, Irony-Tur-Sinai M, Lory O, Orr-Urtreger A, Lavi E, Brenner T (2009) Activation of the cholinergic anti-inflammatory system by nicotine attenuates neuroinflammation via suppression of Th1 and Th17 responses. J Immunol 183:6681–6688
Blanchet MR, Israel-Assayag E, Cormier Y (2004) Inhibitory effect of nicotine on experimental hypersensitivity pneumonitis in vivo and in vitro. Am J Respir Crit Care Med 169:903–909
Ohtsuka Y, Munakata M, Tanimura K et al (1995) Smoking promotes insidious and chronic farmer's lung disease, and deteriorates the clinical outcome. Intern Med 34:966–971
Furuiye M, Miyake S, Miyazaki Y et al (2007) Effect of cigarette smoking on the development of murine chronic pigeon breeder's lung The difference between a short-term and a long-term exposure. J Med Dent Sci 54:87–95
Fernandez Perez ER, Swigris JJ, Forssen AV et al (2013) Identifying an inciting antigen is associated with improved survival in patients with chronic hypersensitivity pneumonitis. Chest 144:1644–1651
Kazerooni EA, Chow LC, Whyte RI, Martinez FJ, Lynch JP (1995) Preoperative examination of lung transplant candidates: value of chest CT compared with chest radiography. AJR Am J Roentgenol 165:1343–1348
Craig PJ, Wells AU, Doffman S et al (2004) Desquamative interstitial pneumonia, respiratory bronchiolitis and their relationship to smoking. Histopathology 45:275–282
Kawabata Y, Takemura T, Hebisawa A et al (2012) Desquamative interstitial pneumonia may progress to lung fibrosis as characterized radiologically. Respirology 17:1214–1221
Lee HY, Lee KS, Jeong YJ et al (2012) High-resolution CT findings in fibrotic idiopathic interstitial pneumonias with little honeycombing: serial changes and prognostic implications. AJR Am J Roentgenol 199:982–989
Alhamad EH, Al-Boukai AA, Al-Kassimi FA et al (2011) Prediction of pulmonary hypertension in patients with or without interstitial lung disease: reliability of CT findings. Radiology 260:875–883
Edwards PD, Bull RK, Coulden R (1998) CT measurement of main pulmonary artery diameter. Br J Radiol 71:1018–1020
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jonathan H. Chung, MD.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Funding
The authors state that this work has not received any funding.
Statistics and biometry
Two of the authors have significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Rights and permissions
About this article
Cite this article
Chung, J.H., Montner, S.M., Adegunsoye, A. et al. CT findings associated with survival in chronic hypersensitivity pneumonitis. Eur Radiol 27, 5127–5135 (2017). https://doi.org/10.1007/s00330-017-4936-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4936-3