Abstract
Systemic lupus erythematosus (SLE) is a disease that affects the immune system, and it can lead to increased morbidity and mortality. The primary causes of mortality for individuals with SLE are disease activity, infections, drug toxicity, and other health conditions. The aim of this study is to estimate the mortality rate of patients with SLE who are hospitalized, describe the causes of death, and identify factors associated with mortality. The study was conducted at a referral hospital from 2009 to 2021, utilizing a nested case–control design. The records of patients with SLE who were hospitalized in the Department of Rheumatology were reviewed. Cases were identified as individuals who died during their hospitalization, while controls were those who were discharged alive during the same period. Elective hospitalizations were not included in the study. The primary causes of death were recorded, and demographic, clinical, laboratory, and immunological variables were analyzed as potential risk factors associated with in-hospital mortality. The study included 105 patients who died while hospitalized and 336 who were discharged alive. The estimated mortality rate was 10.93 deaths per 1000 hospital admissions per year. The leading causes of death were SLE activity (20%), infections (34.2%), or a combination of both (24.8%). Risk factors associated with in-hospital mortality were any infection (OR 2.5, CI 95% 1.2–5.2), nosocomial infections (OR 5.0, CI 95% 1.8–13.7), SLEDAI-2K > 2 (OR 2.0, CI 95% 1.02–3.8), lymphopenia (OR 2.1, CI 95% 1.01–4.6), anemia (OR 2.9, CI 95% 1.4–5.7), and thrombocytopenia (OR 3.3, CI 95% 1.7–6.4). Disease activity and infections, particularly nosocomial infections, are significant causes of mortality in hospitalized patients with SLE. Furthermore, hematological manifestations play a significant role in in-hospital mortality for these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is a systemic, immune-mediated disease characterized by an extensive production of autoantibodies with multiorgan involvement that results in significant morbidity and mortality [1]. Despite notable advances in the knowledge of the pathogenesis of the disease and its therapeutic approach, patients with SLE still have a higher mortality compared to the general population, adjusted for age and sex [2]. Several studies have reported standardized mortality rates (SMR) between 1.8 and 4.5 [3,4,5,6,7]. The information from Latin American countries is scarce and comes mainly from the cohort of the Grupo Latino Americano de Estudio de Lupus (GLADEL for its acronym in Spanish). In this cohort of 1480 patients with SLE, the survival rate at 4 years was found to be 94% [8] More recently, in a report on global mortality trends in systemic autoimmune diseases from 2001 to 2014, the SMR in patients with SLE was higher in Latin America (5.53) compared to North America (2.69) [9]. In Mexico, SLE is one of the main causes of death in young women (15–44 years) [10].
For several decades, it has been noted that SLE patients experience two mortality peaks. Infections and SLE activity usually cause the first peak in the short term, while the second peak is attributed to cardiovascular complications and neoplasms in the long term [11]. In developing countries, the leading causes of in-hospital death in patients with SLE are disease activity, infections, or a combination of both [12,13,14]. Neoplasms are another recognized cause of death, although less frequently reported [9]. In addition, various risk factors have been associated with mortality, such as older age at onset, male gender, high activity scores, fever, myositis, neurological, cardiovascular, premature atherosclerosis, lupus nephritis (class IV and VI), associated antiphospholipid syndrome (APS), gastrointestinal involvement, vasculitis, serum creatinine, thrombocytopenia, persistent C3 hypocomplementemia, high levels of C-reactive protein (CRP), presence of antiphospholipid antibodies (aPL) as well as high dose pulses of methylprednisolone and IV cyclophosphamide [13]. Thus, the mortality rate in patients with SLE can vary and may be influenced by various factors such as epidemiological, sociodemographic, genetic, clinical, and economic factors [2, 15,16,17,18]. Therefore, it is essential to collect local data to improve patient care and facilitate effective diagnosis and treatment for hospitalized SLE patients. Here, our aim was to determine the in-hospital mortality rate and the causes and risk factors associated with mortality in patients with SLE who were admitted to a referral hospital.
Patients and methods
We conducted a nested case–control study at the Hospital de Especialidades Dr. Antonio Fraga Mouret, Centro Médico Nacional La Raza, a national tertiary center in Mexico City, Mexico. We included patients aged > 18 years at the time of admission with the diagnosis of SLE according to the 2012 ACR/SLICC criteria admitted to the Department of Rheumatology between January 2009 and December 2020 [19]. We did not include patients admitted electively to perform a procedure (e.g., renal biopsy), for the scheduled administration of a drug (such as cyclophosphamide or rituximab) or pregnant women. Subsequently, we identified those patients who died during the hospitalization, and the primary cause of death was categorized into disease activity, infection, a combination of both, and other causes (e.g., drug toxicity, gastrointestinal bleeding, thrombosis). Patients who died (cases) were compared with those who were discharged alive (controls) in the same study period in a 1:3 ratio matched for age and sex.
For each patient, we collected demographic, clinical, biochemical, and immunological data from the medical records. Clinical variables included organ involvement in SLE, type and degree of SLE activity, and index of chronic damage. Disease activity was calculated using the SLE Disease Activity Index 2K (SLEDAI-2K) and a score equal to or greater than 4 was considered active disease. The chronic damage to the patients was calculated using the SLICC/ACR Damage Index and its presence was considered with a score equal to or greater than 1. Antiphospholipid syndrome (APS) was diagnosed using the updated 2006 Sydney criteria [20]. Patients whose symptoms began before 18 years old were classified as childhood-onset SLE. Biochemical variables included complete blood count, urea, urea nitrogen, serum creatinine, transaminases, serum lipids, general urinalysis, glomerular filtration rate (GFR), and 24-h proteinuria. Anemia was defined as Hb < 10 g/dL, lymphopenia as lymphocytes < 1000/μL, and thrombocytopenia as platelets < 100,000/μL. The immunological variables obtained were C3 and C4 serum complement (determined by nephelometry), antinuclear antibodies (ANA) by indirect immunofluorescence, anti-double-stranded DNA (anti-dsDNA) antibodies, anti-Sm antibodies, anti-SSA/Ro antibodies, anti-SSB/La antibodies (determined by ELISA), lupus anticoagulant (LA), anti-cardiolipin antibodies, and anti-β2-glycoprotein-1 antibodies. Comorbidities such as obesity, diabetes, and arterial hypertension were also recorded. Diagnosis of infection was established based on a combination of clinical characteristics, systemic inflammatory response, imaging studies, and/or isolation of the causative microorganism by the culture of the affected site. Furthermore, infections were classified as community-acquired or nosocomial. Nosocomial infections were defined according to the WHO, as those infections acquired during the hospital stay and that were not present either in the incubation period or at the time of patient admission. The duration of hospital stays, as well as the medications taken both before and during hospitalization, were documented.
Statistical analysis and ethical considerations
Categorical variables are presented in simple frequencies and percentages. Continuous variables are presented as means with standard deviations (SD) or medians with interquartile ranges, as appropriate. We compared the characteristics of SLE patients who died during hospitalization (cases) vs. those who were discharged alive (controls) using Student's t test or Wilcoxon test for continuous measures and Pearson's Chi-square or Fisher's exact test for categorical measures. A comparison of variables among the death categories was made using the Chi-square test, ANOVA test, or Kruskal–Wallis test, as appropriate. We conducted a receiver operating characteristic (ROC) curve analysis to identify the SLEDAI-2K score threshold that provides the most accurate prediction of in-hospital mortality. Additionally, we calculated both the positive predictive value (PPV) and negative predictive value (NPV). A multivariable logistic regression analysis was conducted to determine the potentially predictive variables with a p value less than 0.1 in the bivariate analysis. The dependent variables included in-hospital mortality, active disease mortality, infection mortality, and early mortality. The results from multivariable analysis and ROC curve analysis were expressed as odds ratio (OR) and its 95% confidence interval (CI). A p value < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS software (v. 25.0, IBM 2010). The Local Health Research Committee number 3501 of our hospital approved the study protocol on December 15, 2021 (registry number R-2021-3501-134), and it was conducted in accordance with the declaration of Helsinki. Informed consent was not required as patient information was anonymized before analysis. The data of the patients were treated in accordance with the General Law of Protection of Personal Data in force in our country.
Results
We identified 1109 hospital admissions of SLE patients over 11 years. Of the total number of patients admitted to the hospital, we excluded 235 of them because they had been hospitalized electively (Fig. 1). From the remaining 834 patients, we identified 105 hospitalized patients who died. The estimated mortality rate was 10.93 deaths/1000 hospital admissions/year. To compare the variables, we selected 336 hospitalized patients who were discharged alive (controls) in the same study period, with a 1:3 strategy. Of the total number of hospitalized patients included in the analysis, 17% of them had > 1 admission to the hospital.
Comparison of dead patients with those alive at hospital discharge
Of the total included patients, 82% were female with a mean age of 34 ± 12 years (Table 1). Patients who died had a shorter duration of SLE (36 vs 60 months, p = 0.03), higher SLEDAI-2K scores (4 vs. 2 points, p < 0.001), a higher percentage of active patients (61% vs. 39.6%, p < 0.001), a lower percentage of APS (13.3% vs. 24.4%, p = 0.01), and a higher proportion of chronic kidney disease (35.2% vs. 14.9%, p < 0.001) compared to those who were discharged alive (Table 1). Constitutional symptoms (39.9% vs. 20%, p < 0.001), mucocutaneous manifestations (90.8% vs. 61.9%, p < 0.001), and serositis (17.3% vs 8.6%, p = 0.03) were more frequent in patients alive at hospital discharge, while cardiovascular involvement (7.6% vs. 2.7%, p = 0.02), pulmonary manifestations (23.8% vs. 12.5%, p = 0.005), and hematological manifestations (61.9% vs. 49.7%, p = 0.005) were more common in dead patients. About 60% of patients had lupus nephritis with a similar distribution in both groups. Mesangial glomerulonephritis (class II) was more frequently observed in those patients who survived and diffuse glomerulonephritis (class IV) in those who died. According to the class of lupus nephritis confirmed by biopsy, patients with class II lupus nephritis most frequently received mycophenolate mofetil (53.8%) followed by IV cyclophosphamide (26.9%) and azathioprine (15.3%); in those with class III, mycophenolate mofetil (36.8%) followed by azathioprine (31.5%) and tacrolimus (15.7%); in those with class IV, mycophenolate mofetil (44.7%) followed by IV cyclophosphamide (32.8%) and azathioprine (30.2%); and finally in those with class V, mycophenolate mofetil (37.5%) followed by azathioprine (31.2%) and IV cyclophosphamide (25%). Considering laboratory parameters, the patients who died presented more frequently with anemia (75.7% vs. 37.5%, p < 0.001), lymphopenia (83.5% vs. 65.4%), p < 0.001, thrombocytopenia (47.6% vs. 17%, p < 0.001), elevated serum creatinine (1.5 mg/dL vs. 0.8 mg/dL, p < 0.001), decreased GFR (75% vs 43.1%, p < 0.001), and C3 hypocomplementemia (74% vs. 51.7%, p < 0.001) on hospital admission compared to those who were alive (Table 2). Interestingly, a smaller proportion of deceased patients were taking chloroquine (50.5% vs. 62.5%, p = 0.007) but received methylprednisolone pulses more frequently than those living patients (35.2% vs. 24.6%, p = 0.002). Infections (57.1% vs. 28%, p < 0.001), especially nosocomial infections (58.3% vs. 14.7%, p < 0.001), more frequently complicated patients who died compared to those who did not die, with pneumonia being the most observed infection (60% vs. 18.1%, p < 0.001) (Table 3). On the other hand, soft-tissue infections (21.3% vs. 8.3%, p < 0.001) and urosepsis (24.5% vs. 11.7%, p = 0.003) were more frequent in patients who survived compared to those who died. Of 40 patients in which the results of their cultures were obtained, a microorganism was isolated in 38, with E. coli, S. aureus, C. albicans, P. aeruginosa, K. pneumoniae, and A. faecium being the most frequently recovered microorganisms. Patients who developed a nosocomial infection had a greater number of days of hospital stay (11 vs. 8, p < 0.001), lower SLEDAI scores (4 vs. 5, p = 0.008), a higher frequency of chronic kidney disease (41.7% vs. 17.1%, p < 0.001), anemia (70.8% vs. 40.3%, p < 0.001), and thrombocytopenia (43.8% vs. 22%, p < 0.001) as well as higher CRP levels (28.7 mg/dL vs. 7.83 g/dL, p = 0.01) compared to those without it.
Analysis of mortality subgroups
According to the attributed cause of death, 36 patients (34.2%) died from infections, 21 (20%) from SLE activity, 26 (24.8%) from a combination of both, and 21 (20%) from other causes, mostly gastrointestinal hemorrhage, malignancies, drug toxicity, liver disease, and SARS-CoV2 infection. The comparison of the variables studied by the different mortality subgroups of patients is shown in Table 3. Of the total number of dead patients, 68 (64.5%) had less than 5 years of evolution (early death). In the group of patients with early death, a lower proportion of childhood SLE (8.8% vs. 40.5%, p < 0.001), higher SLEDAI scores (4 vs. 2, p = 0.01), lower proportion of accrual chronic damage (27.9% vs. 56.8%, p = 0.004), a lower frequency of arterial hypertension (19.1% vs. 32.4%, p = 0.001), and chronic kidney disease (31.3% vs. 43.2%, p = 0.01) were observed compared with the group with late death. As expected, the median SLEDAI-2K scores were higher in those patients who died due to SLE activity with and without associated infection (median of 10 and 9 points, respectively; p < 0.001). Anemia and thrombocytopenia were more frequently found in patients who died due to SLE activity with and without associated infection (80.8% and 76.2%, p < 0.001; 50% and 56.1%, p < 0.001; respectively). C3 hypocomplementemia was more frequent in patients who died due to disease activity (85.7%, p < 0.001). A lower proportion of patients who died due to SLE activity were taking chloroquine (p < 0.003) but more frequently received methylprednisolone pulses (p < 0.003) at hospital admission compared to the other subgroups.
Mortality predictors
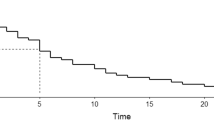
In the multivariate analysis, we found that hematological manifestations such as anemia (OR 2.9, CI 95% 1.4–5.7), lymphopenia (OR 2.1, CI 95% 1.01–4.6), and thrombocytopenia (OR 3.3, CI 95% 1.7–6.4) as well as any kind of infection (OR 2.5, CI 95% 1.2–5.2), particularly nosocomial infections (OR 5.0, CI 95% 1.8–13.7) were independent risk factors associated with in-hospital mortality (Fig. 2). ROC curve analysis showed that a SLEDAI score > 2 had a PPV of 83% and an NPV of 35% to predict in-hospital mortality (OR 2.0, CI 95% 1.02–3.8). In contrast, the presence of constitutional symptoms (OR 0.3, CI 95% 0.1–0.7), skin and joint involvement (OR 0.2, CI 95% 0.1–0.5), serositis (OR 0.1, CI 95% 0.06–0.4), and use of prednisone (OR 0.2, CI 95% 0.05–0.8) were factors associated with less in-hospital mortality. Finally, it was not possible to analyze risk factors by cause of death subgroup due to an insufficient number of subjects in the outcome group.
Discussion
We conducted a study to examine the mortality rate of SLE patients during their hospital stay and to identify the contributing factors and causes of death over an 11-year period at a reference hospital. Our findings revealed a significant mortality rate, with disease activity and infections, particularly those acquired in the hospital or a combination of both, as the primary causes of death in SLE patients. We also found that anemia, thrombocytopenia, and hospital-acquired infections were independent risk factors for mortality in SLE patients during their hospitalization.
Over the past 50 years, the survival rate of patients with SLE has significantly improved. In the 1950s, the survival rate was less than 50%, but at the beginning of the twenty-first century, it had increased to almost 95% thanks to a better understanding of the disease and advancements in diagnosis and treatment [21]. However, mortality rates still vary across different ethnicities, races, and regions. In the United States, the risk of death for hospitalized patients with SLE decreased from 2.2 to 1.5% between 2006 and 2016, but Black and Hispanic individuals were more likely to die than other ethnic groups [18, 22]. Developed countries like Canada, the UK, Denmark, and Finland have an SMR ranking of 1.48 to 4.53 [5, 23,24,25], while a Brazilian study showed a mortality rate of 4.76 deaths per 100,000 inhabitants [26]. Developing countries like Pakistan and South Africa report lower survival rates, ranging from 57 to 80% [27, 28]. Our study reported a high mortality rate of 10.93 deaths per 1000 hospital admissions annually. It should be noted that our research was conducted at a high-complexity medical center, which provides care to severe patients that probably had worse disease outcomes. Additionally, our patients are of Hispanic ethnicity and are of low socioeconomic status, factors known to impact disease outcomes, as previously reported [15,16,17,18].
Our research has found that infections, especially nosocomial infections, and SLE flare-ups (either alone or combined with infection) are the primary causes of death. This finding is consistent with similar studies conducted in other countries [29,30,31,32]. For instance, a review of 174,105 SLE hospitalizations in the United States using the National Inpatient Sample (NIS) in 2016 revealed that infections were the leading cause of death [29]. In China, a nationwide SLE cohort of 29,510 hospitalized patients between 2005 and 2014 found that infections and complications related to SLE activity were the most common causes of death [30]. In Colombia, a retrospective case series of SLE patients who died between January 2011 and June 2017 also identified disease activity and infections as the primary causes of death [31]. However, our findings differ from other researches that report cardiovascular disease and malignancy as the significant causes of death in SLE patients, especially in developed countries [33,34,35,36,37,38,39,40,41]. Generally, during the early stages of illness, infections, or complications of active disease (such as lupus nephritis) are the leading causes of death, while cardiovascular disease and cancer are the primary causes of late death in SLE patients [2]. However, in a recent British study, unexpectedly no cardiovascular causes of death were found, suggesting a change in the trend of causes of mortality in patients with SLE, similar to our results [42]. It is worth mentioning that the median evolution time in our patients was 48 months, which partly explains why we observed few cardiovascular complications, such as ischemic heart disease. Therefore, factors such as ethnicity, socioeconomic status, regional cultural background, and the availability of medical resources can influence the course and outcomes of patients with SLE.
The importance of infections as a potentially serious complication in patients with SLE should not be overlooked. Bacterial infections are the most frequent, followed by viral, fungal, and protozoan infections, with the respiratory and urinary tracts being the most affected sites [2]. SLE patients are more prone to bacteremia, which has a higher mortality rate compared to other infections [43, 44]. Mortality is also higher in those with nosocomial infections and active lupus [27, 45,46,47] which agrees with our results. SLE patients with high disease activity and intense immunosuppressive therapy are more susceptible to infections [27, 48]. Additionally, different therapeutic responses have been described with the use of immunosuppressants in different ethnicities, which may influence disease control and potential adverse effects [49]. Our study revealed that a significant number of patients had active SLE and were treated with pulse methylprednisolone and other immunosuppressants, resulting in a high incidence of infections. On the other hand, antimalarial medication has been shown to lower the risk of infections in SLE patients [49]. Antimalarials can provide protection against infections by regulating pH and post-translational protein modifications [31]. In our study, those who died had lower chloroquine use. Therefore, it is crucial to provide outpatient care, ensure adherence to treatment, identify the optimal immunosuppression treatment, and educate patients to reduce the risk of death.
Based on our analysis using both bivariate and multivariable models, we can confirm that organ involvement related to SLE significantly impacts the outlook of these patients. Hematological manifestations of the three cell lines were found to be an independent risk factor for mortality by the multivariable logistic regression analysis. Our results are consistent with previous research such as Moghazy et al.’s report, which identified lymphopenia as a risk factor for mortality in the multivariate Cox regression analysis [50]. Wo et al.’s study also found hematological abnormalities to be associated with mortality in both univariate and multivariate analyses [30]. In a case series by Aguirre-Valencia et al., patients who passed away often had lymphopenia, anemia, leukopenia, or thrombocytopenia with a frequency between 73.4 and 89.8% [31]. In a previous case–control study by Miranda-Hernandez et al. of hospitalized SLE patients, those were admitted for hematological manifestations had a higher risk of death (OR 3.8, 95% CI 1.1–8.8, p < 0.001), particularly those with thrombocytopenia, compared to those admitted for other SLE symptoms or complications [51]. Minor manifestations of SLE (serositis, skin and joint involvement) were associated with lower mortality, which may simply show less severity of the disease. In fact, higher SLEDAI scores at SLE diagnosis are associated with higher mortality. Unfortunately, we did not have this complete information to perform our analysis. Therefore, it is crucial to quickly identify any hemocytopenia in a hospital setting as it can affect the mortality risk of SLE patients.
Our study has some limitations that need to be acknowledged. First, we only included patients from a single hospital center, so our findings may not apply to other healthcare settings. Nonetheless, the insights gained from this study can help improve the care provided to these patients. Second, due to the retrospective design of our study, some relevant data may have been missed. For example, it was not possible to obtain the SLEDAI score at diagnosis or calculate the cumulative glucocorticoid dose. However, we made sure to exclude patients with incomplete information, which may have introduced some level of selection bias. Third, it was not possible to recover the isolated causative agent in all patients with infection. Lastly, our research only focused on patients admitted to the Department of Rheumatology, and therefore we may have underestimated the incidence of cardiovascular or malignant mortality in the wider hospital population.
In conclusion, infections and disease activity remain the primary causes of death among individuals with SLE. It is crucial to undertake comprehensive measures that account for varying disease severity, evaluate the effectiveness of immunosuppressants, comply with management guidelines, ensure adequate access to healthcare, and address social determinants of health to reduce the disparity in in-hospital mortality rates for SLE patients.
References
Dörner T, Furie R (2019) Novel paradigms in systemic lupus erythematosus. Lancet 393:2344–2358. https://doi.org/10.1016/S0140-6736(19)30546-X
Ocampo-Piraquive V, Nieto-Aristizábal I, Cañas CA, Tobón GJ (2018) Mortality in systemic lupus erythematosus: causes, predictors and interventions. Expert Rev Clin Immunol 14:1043–1053. https://doi.org/10.1080/1744666X.2018.1538789
Tselios K, Gladman DD, Sheane BJ, Su J, Urowitz M (2019) All-cause, cause-specific and age-specific standardised mortality ratios of patients with systemic lupus erythematosus in Ontario, Canada over 43 years (1971–2013). Ann Rheum Dis 78:802–806. https://doi.org/10.1136/annrheumdis-2018-214802
Hersh AO, Trupin L, Yazdany J, Panopalis P, Julian L, Katz P, Criswell LA, Yelin E (2010) Childhood-onset disease as a predictor of mortality in an adult cohort of patients with systemic lupus erythematosus. Arthritis Care Res (Hoboken) 62:1152–1159. https://doi.org/10.1002/acr.20179
Ambrose N, Morgan TA, Galloway J, Ionnoau Y, Beresford MW, Isenberg DA; UK JSLE Study Group (2016) Differences in disease phenotype and severity in SLE across age groups. Lupus 25:1542–1550. https://doi.org/10.1177/0961203316644333
Ingvarsson RF, Landgren AJ, Bengtsson AA, Jönsen A (2019) Good survival rates in systemic lupus erythematosus in southern Sweden, while the mortality rate remains increased compared with the population. Lupus 28:1488–1494. https://doi.org/10.1177/0961203319877947
Bultink IEM, de Vries F, van Vollenhoven RF, Lalmohamed A (2021) Mortality, causes of death and influence of medication use in patients with systemic lupus erythematosus vs matched controls. Rheumatology (Oxford) 60:207–216. https://doi.org/10.1093/rheumatology/keaa267
Pons-Estel GJ, Catoggio LJ, Cardiel MH, Bonfa E, Caeiro F, Sato E, Massardo L, Molina Restrepo JF, Toledano MG, Barile-Fabris LA, Amigo MC, Acevedo-Vásquez EM, Abadi I, Wojdyla D, Alarcón-Riquelme ME, Alarcón GS, Pons-Estel BA, GLADEL, (2015) Lupus in Latin-American patients: lessons from the GLADEL cohort. Lupus 24:536–545. https://doi.org/10.1177/0961203314567753
Scherlinger M, Mertz P, Sagez F, Meyer A, Felten R, Chatelus E, Javier RM, Sordet C, Martin T, Korganow AS, Guffroy A, Poindron V, Richez C, Truchetet ME, Blanco P, Schaeverbeke T, Sibilia J, Devillers H, Arnaud L (2020) Worldwide trends in all-cause mortality of autoimmune systemic diseases between 2001 and 2014. Autoimmun Rev 19:102531. https://doi.org/10.1016/j.autrev.2020.102531
Etchegaray-Morales I, Mendoza-Pinto C, Munguía-Realpozo P, Osorio-Peña ÁD, Ibañez-Ovando S, Pineda C, García-Carrasco M (2022) Systemic lupus erythematosus, a leading cause of death in young Mexican females: a nationwide population-based study, 2000–2020. Rheumatol Int 42:1715–1720. https://doi.org/10.1007/s00296-022-05154-9
Urowitz MB, Bookman AA, Koehler BE, Gordon DA, Smythe HA, Ogryzlo MA (1976) The bimodal mortality pattern of systemic lupus erythematosus. Am J Med 60:221–225. https://doi.org/10.1016/0002-9343(76)90431-9
Vega-Morales D, Hernández-Galarza IJ, Galarza-Delgado DÁ (2018) Causes of hospital mortality in patients with rheumatoid arthritis and systemic lupus erythematosus in a university hospital: 1998–2015 analysis. J Rheumatol 45:583–584. https://doi.org/10.3899/jrheum.170735
Pattanaik SS, Muhammed H, Chatterjee R, Naveen R, Lawrence A, Agarwal V, Misra DP, Gupta L, Misra R, Aggarwal A (2020) In-hospital mortality and its predictors in a cohort of SLE from Northern India. Lupus 29:1971–1977. https://doi.org/10.1177/0961203320961474
Adwan MH, Qasem U, Mustafa KN (2020) In-hospital mortality in patients with systemic lupus erythematosus: a study from Jordan 2002–2017. Rheumatol Int 40:711–717. https://doi.org/10.1007/s00296-020-04538-z
Lim SS, Helmick CG, Bao G, Hootman J, Bayakly R, Gordon C, Drenkard C (2019) Racial disparities in mortality associated with systemic lupus erythematosus - Fulton and DeKalb Counties, Georgia, 2002-2016. MMWR Morb Mortal Wkly Rep 68:419–422. https://doi.org/10.15585/mmwr.mm6818a4
Gianfrancesco MA, Dall'Era M, Murphy LB, Helmick CG, Li J, Rush S, Trupin L, Yazdany J (2021) Mortality Among Minority Populations with Systemic Lupus Erythematosus, Including Asian and Hispanic/Latino Persons - California, 2007–2017. MMWR Morb Mortal Wkly Rep 70:236–239. https://doi.org/10.15585/mmwr.mm7007a2
Guo Q, Liang M, Duan J, Zhang L, Kawachi I, Lu TH (2021) Age differences in secular trends in black-white disparities in mortality from systemic lupus erythematosus among women in the United States from 1988 to 2017. Lupus 30:715–724. https://doi.org/10.1177/0961203321988936
Taylor T, Anastasiou C, Ja C, Rush S, Trupin L, Dall’Era M, Katz P, Barbour KE, Greenlund KJ, Yazdany J, Gianfrancesco MA (2023) Causes of death among individuals with systemic lupus erythematosus by race and ethnicity: a population-based study. Arthritis Care Res (Hoboken) 75:61–68. https://doi.org/10.1002/acr.24988
Petri M, Orbai AM, Alarcón GS, Gordon C, Merrill JT, Fortin PR, Bruce IN, Isenberg D, Wallace DJ, Nived O, Sturfelt G, Ramsey-Goldman R, Bae SC, Hanly JG, Sánchez-Guerrero J, Clarke A, Aranow C, Manzi S, Urowitz M, Gladman D, Kalunian K, Costner M, Werth VP, Zoma A, Bernatsky S, Ruiz-Irastorza G, Khamashta MA, Jacobsen S, Buyon JP, Maddison P, Dooley MA, van Vollenhoven RF, Ginzler E, Stoll T, Peschken C, Jorizzo JL, Callen JP, Lim SS, Fessler BJ, Inanc M, Kamen DL, Rahman A, Steinsson K, Franks AG Jr, Sigler L, Hameed S, Fang H, Pham N, Brey R, Weisman MH, McGwin G Jr, Magder LS (2012) Derivation and validation of the systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 64:2677–2686. https://doi.org/10.1002/art.34473
Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, Derksen RH, de Groot PG, Koike T, Meroni PL, Reber G, Shoenfeld Y, Tincani A, Vlachoyiannopoulos PG, Krilis SA (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 4:295–306. https://doi.org/10.1111/j.1538-7836.2006.01753.x
Fors Nieves CE, Izmirly PM (2016) Mortality in systemic lupus erythematosus: an updated review. Curr Rheumatol Rep 18:21. https://doi.org/10.1007/s11926-016-0571-2
Anastasiou C, Trupin L, Glidden DV, Li J, Gianfrancesco M, Shiboski S, Schmajuk G, Yazdany J (2021) Mortality among hospitalized individuals with systemic lupus erythematosus in the US between 2006 and 2016. Arthritis Care Res 73:1444–1450. https://doi.org/10.1002/acr.24356
Urowitz MB, Gladman DD, Tom BD, Ibañez D, Farewell VT (2008) Changing patterns in mortality and disease outcomes for patients with systemic lupus erythematosus. J Rheumatol 35:2152–2158. https://doi.org/10.3899/jrheum.080214
Voss A, Laustrup H, Hjelmborg J, Junker P (2013) Survival in systemic lupus erythematosus, 1995–2010. A prospective study in a Danish community. Lupus 22:1185–1191. https://doi.org/10.1177/0961203313498796
Elfving P, Puolakka K, Kautiainen H, Virta LJ, Pohjolainen T, Kaipiainen-Seppänen O (2014) Mortality and causes of death among incident cases of systemic lupus erythematosus in Finland 2000–2008. Lupus 23:1430–1434. https://doi.org/10.1177/0961203314543919
Costi LR, Iwamoto HM, Neves DCDO, Caldas CAM (2017) Mortality from systemic erythematosus lupus in Brazil: evaluation of causes according to the government health database. Rev Bras Reumatol Engl Ed 57:574–582. https://doi.org/10.1016/j.rbre.2017.09.001
Rabbani MA, Habib HB, Islam M, Ahmad B, Majid S, Saeed W, Shah SM, Ahmad A (2009) Survival analysis and prognostic indicators of systemic lupus erythematosus in Pakistani patients. Lupus 18:848–855. https://doi.org/10.1177/0961203309103410
Wadee S, Tikly M, Hopley M (2007) Causes and predictors of death in South Africans with systemic lupus erythematosus. Rheumatology 46:1487–1491. https://doi.org/10.1093/rheumatology/kem180
Dhital R, Pandey RK, Poudel DR, Oladunjoye O, Paudel P, Karmacharya P (2020) All-cause hospitalizations and mortality in systemic lupus erythematosus in the US: results from a national inpatient database. Rheumatol Int 40:393–397. https://doi.org/10.1007/s00296-019-04484-5
Wu XY, Yang M, Xie YS, Xiao WG, Lin J, Zhou B, Guan X, Luo CN, Che N, Liu XZ, Wang C, Teng JL, Cheng XB, Ye JN, Su YT, Shi H, Yin YF, Liu MR, Sun Y, Hu QY, Zhou ZC, Chi HH, Liu Y, Zhang X, Chen JW, Zhang MJ, Zhao DB, Yang CD, Wu LJ, Liu HL (2019) Causes of death in hospitalized patients with systemic lupus erythematosus: a 10-year multicenter nationwide Chinese cohort. Clin Rheumatol 38:107–115. https://doi.org/10.1007/s10067-018-4259-z
Aguirre-Valencia D, Suárez-Avellaneda A, Ocampo-Piraquive V, Posso-Osorio I, Naranjo-Escobar J, Nieto-Aristizábal I, Tobón GJ, Cañas CA (2019) Mortality in patients with systemic lupus erythematosus in Colombia: a case series. Clin Rheumatol 38:1865–1871. https://doi.org/10.1007/s10067-019-04546-w
Lertwises S, Rattanasupar A, Chang A (2023) Factors predictive of in-hospital mortality in patients with systemic lupus erythematosus: a single-centre retrospective analysis. Acta Med Acad 52:37–46. https://doi.org/10.5644/ama2006-124.400
Rees F, Doherty M, Grainge MJ, Lanyon P, Davenport G, Zhang W (2016) Mortality in systemic lupus erythematosus in the United Kingdom 1999–2012. Rheumatology (Oxford) 55:854–860. https://doi.org/10.1093/rheumatology/kev424
Thomas G, Mancini J, Jourde-Chiche N, Sarlon G, Amoura Z, Harlé JR, Jougla E, Chiche L (2014) Mortality associated with systemic lupus erythematosus in France assessed by multiple-cause-of-death analysis: mortality and systemic lupus erythematosus. Arthritis Rheum 66:2503–2511. https://doi.org/10.1002/art.38731
Yen EY, Shaheen M, Woo JMP, Mercer N, Li N, McCurdy DK, Karlamangla A, Singh RR (2017) 46-year trends in systemic lupus erythematosus mortality in the United States, 1968 to 2013: a nationwide population-based study. Ann Intern Med 167:777–785. https://doi.org/10.7326/M17-0102
Li D, Yoshida K, Feldman CH, Speyer C, Barbhaiya M, Guan H, Solomon DH, Everett BM, Costenbader KH (2020) Initial disease severity, cardiovascular events and all-cause mortality among patients with systemic lupus erythematosus. Rheumatology (Oxford) 59:495–504. https://doi.org/10.1093/rheumatology/kez288
Segura BT, Bernstein BS, McDonnell T, Wincup C, Ripoll M, V, Giles I, Isenberg D, Rahman A, (2020) Damage accrual and mortality over long-term follow-up in 300 patients with systemic lupus erythematosus in a multi-ethnic British cohort. Rheumatology (Oxford) 59:524–533. https://doi.org/10.1093/rheumatology/kez292
Hernández-Rodríguez JC, Durán-Romero AJ, Muñoz-Jiménez A, Conejo-Mir J, Pereyra-Rodríguez JJ (2020) Trends in mortality from lupus in Spain from 1980 to 2018. Lupus 29:1719–1726. https://doi.org/10.1177/0961203320952864
Elfving P, Kariniemi S, Kautiainen H, Virta LJ, Kaipiainen-Seppänen O, Puolakka K (2021) Mortality in SLE patients compared with population controls in Finland in years 2000–2015. Rheumatology (Oxford) 60:4238–4244. https://doi.org/10.1093/rheumatology/keaa917
Lorenzo-Vizcaya A, Isenberg D (2021) Analysis of trends and causes of death in SLE patients over a 40-years period in a cohort of patients in the United Kingdom. Lupus 30:702–706. https://doi.org/10.1177/0961203320988607
Moghaddam B, Marozoff S, Li L, Sayre EC, Zubieta JAA (2021) All-cause and cause-specific mortality in systemic lupus erythematosus: a population-based study. Rheumatology (Oxford) 61:367–376. https://doi.org/10.1093/rheumatology/keab362
Anver H, Dubey S, Fox J (2019) Changing trends in mortality in systemic lupus erythematosus? An analysis of SLE inpatient mortality at University Hospital Coventry and Warwickshire NHS Trust from 2007 to 2016. Rheumatol Int 39:2069–2075. https://doi.org/10.1007/s00296-019-04450-1
Cuchacovich R, Gedalia A (2009) Pathophysiology and clinical spectrum of infections in systemic lupus erythematosus. Rheum Dis Clin North Am 35:75–93. https://doi.org/10.1016/j.rdc.2009.03.003
Singh JA, Cleveland JD (2021) Hospitalized infections in Lupus: a nationwide study of types of infections, time trends, health care utilization, and in-hospital mortality. Arthritis Rheumatol 73:617–630. https://doi.org/10.1002/art.41577
Navarro-Zarza JE, Alvarez-Hernández E, Casasola-Vargas JC, Estrada-Castro E, Burgos-Vargas R (2010) Prevalence of community-acquired and nosocomial infections in hospitalized patients with systemic lupus erythematosus. Lupus 19:43–48. https://doi.org/10.1177/0961203309345776
Kedves M, Kósa F, Kunovszki P, Takács P, Szabó MZ, Karyekar C, Lofland JH, Nagy G (2020) Large-scale mortality gap between SLE and control population is associated with increased infection-related mortality in lupus. Rheumatology (Oxford) 59:3443–3451. https://doi.org/10.1093/rheumatology/keaa188
Oud L, Garza J (2023) The association of systemic lupus erythematosus with short-term mortality in sepsis: a population-level analysis. J Investig Med 71:419–428. https://doi.org/10.1177/10815589221150641
Yin P, Li J, Wen Q, Qiu Y, Liang W, Wang J, Yu J, Zhong Z, Yang X, Yu X, Ye Q, Huang F (2020) Infection-related hospitalization after intensive immunosuppressive therapy among lupus nephritis and ANCA glomerulonephritis patients. Ren Fail 42:474–482. https://doi.org/10.1080/0886022X.2020.1763400
Gatto M, Saccon F, Zen M, Bettio S, Iaccarino L, Punzi L, Doria A (2016) Success and failure of biological treatment in systemic lupus erythematosus: a critical analysis. J Autoimmun 74:94–105. https://doi.org/10.1016/j.jaut.2016.06.014
Moghazy A, Ibrahim AM (2021) Mortality in a cohort of Egyptian systemic lupus erythematosus patients: retrospective two-center study. Egypt Rheumatol Rehabil 48:14. https://doi.org/10.1186/s43166-021-00062-5
Miranda-Hernández D, Cruz-Reyes C, Monsebaiz-Mora C, Gómez-Bañuelos E, Ángeles U, Jara LJ, Saavedra MÁ (2017) Active haematological manifestations of systemic lupus erythematosus lupus are associated with a high rate of in-hospital mortality. Lupus 26:640–645. https://doi.org/10.1177/0961203316672926
Funding
The authors did not receive any funding to carry out this study.
Author information
Authors and Affiliations
Contributions
All authors meet the ICMJE criteria for authorship. MAS, NZZ, and MAC were involved in drafting or revising this article critically for important intellectual content. DMH, RBG, and AEGR made substantial contributions to the conception or design of the work. AEGR and MÁS drafted the work or revised it critically for important intellectual content. MAC, GMD, DTR, and BLZ contributed to the data collection and analysis. MPCD and MÁS revised the data analysis and the final manuscript. All authors approved the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Congress abstract publications: This study was accepted as a plenary session in LI Mexican Congress of Rheumatology. Colegio Mexicano de Reumatología (2023) LI Congreso Mexicano de Reumatología. Reumatol Clin 19 (Supl Congr 1):1–14. https://www.reumatologiaclinica.org/es-vol-19-num-sc1-sumario-X1699258X23X00C10.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arrucha-Cozaya, M., Zamora-Zúñiga, N.C., Miranda-Hernández, D. et al. In-hospital mortality and associated factors in patients with systemic lupus erythematosus: analysis over more than 11 years in a reference hospital center. Rheumatol Int 43, 2221–2231 (2023). https://doi.org/10.1007/s00296-023-05469-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-023-05469-1