Abstract
The aim of this study was to determine the causes of mortality in patients with systemic lupus erythematosus (SLE) at the University Hospital Coventry and Warwickshire (UHCW) NHS Trust over a 10 year period. This was a retrospective study of patients who had died in UHCW NHS Trust between 2007 and 2016, where SLE or lupus was mentioned on the death certificate. Ethics approval was obtained from the Research and Development. We identified 22 patients out of 1979 admissions with SLE who had died during the period between 2007 and 2016, 7 of these patients were under 50 years of age. The leading cause of death was infection with pneumococcus being associated with two deaths. Active disease was associated with younger age at death. Median age at death was 58.5 years, with median duration of disease of 14.5 years. Constitutional and mucocutaneous features were the most common items scoring on disease activity, seen in 68.2% and 45.45%, respectively. We identified three patients with biopsy proven lupus nephritis and one patient with CNS lupus. Surprisingly, none of the patients died because of vascular problems. The study suggests a changing trend in SLE mortality with none of the deaths in this cohort being due to cardiovascular or cerebrovascular disease. Infection continues to be the biggest reason for mortality in this cohort and greater emphasis is needed on vaccination for preventable infections like pneumococcus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is a chronic multi-system autoimmune disease with involvement of multiple organs either simultaneously or at different time points. There is often significant organ damage in these patients. A number of studies over the years have suggested increased mortality in this group of patients [1]. Older studies had indicated an increase in 5 year mortality of up to 50% [2] compared to the general population. Advances in treatment of patients with lupus led to a significant improvement in this figure, based on more recent studies [1, 2]. However, this improvement in mortality appears to have plateaued since the 2000s, as demonstrated by Jorge et al. [3], and premature mortality remains significantly higher in SLE patients when compared to the general population. The causes for this increased mortality have been analysed in multiple studies and suggest that on average a patient with SLE loses 2 decades of their life [5]. There are multiple causes for this due to its chronicity and multitude of organs involved; nonetheless increased SLE disease activity is considered an important contributory factor [2,3,4,5,6,7]. Some mortality studies have shown ‘double peak’ with increased mortality higher in early disease, due to infection or active disease and later in the disease course (due to cardiovascular, cerebrovascular, malignancy, infection and disease flares) [4,5,6,7,8]. Essentially, increased morbidity and mortality could be due to disease itself, complications of disease, complications of treatment, or unrelated events.
A recent cohort study by Rees et al. [8] suggested a 67% increase of all-cause mortality in patients with SLE when compared to age- and sex-matched controls in the United Kingdom. This study used clinical data from the United Kingdom GP research database which represents approximately 20% of the total UK population. However, although the study identified similar causes for increased SLE mortality to previous studies, it showed differences in the contributions of these causes to the overall increased mortality risk. Since this study collected data that had been coded on the GP database, details about SLE and organ involvement in particular were not available.
The last couple of decades have seen very significant changes in NHS management with improvement in outcomes following renal transplant (currently over 90% for matched transplants [9]); better pharmacological management of atherosclerosis and vascular problems and also the advent of primary angioplasty. We have seen changes in vascular risk in Rheumatoid Arthritis and TRACE RA study was closed early due to reduced CV events in the control arm [10].
University Hospital Coventry and Warwickshire NHS Trust is a secondary care provider with a catchment area of ~ 500,000 covering predominantly Rugby and Coventry, but also some parts of Nuneaton, Leicestershire and Northamptonshire. The lupus cohort that we would provide for in 2016 would be around 250–300 patients.
Our study aimed to analyse the factors involved with SLE mortality at a more local level to better understand local trends and improve the management of patients. This study helps us to discern regional and temporal variations. Here we look at the mortality data for inpatients with SLE at University Hospital Coventry and Warwickshire NHS Trust (UHCW) to determine the main causes of death and compare the data to previously published studies.
Methods
We performed a retrospective study looking at mortality from SLE at UHCW NHS Trust between 2006 and 2016.
The coding department was asked to provide us with data relating to ‘SLE’ or ‘lupus’ being included on death certificates for any patients that had died in hospital between 2007 and 2016. All patients with a diagnosis of SLE or lupus on the death certificate were included in our study. Patient notes were reviewed, and diagnosis was ascertained. Patient notes were also interrogated for more details relating to their final illness and the previous problems with SLE as well as concurrent treatment. SLE was considered active if the treating physician deemed it so.
Further clinical information including duration of illness, treatment history and positive antibodies was obtained through the use of patients’ records and the hospital Clinical Results Reporting Service (CRRS). Disease activity was determined from the clinical assessments recorded in patient notes, based on SELENA-SLEDAI composite score [11]. We also classified patients based on systemic involvement by grouping symptoms as per the British Isles Lupus Assessment Group (BILAG 2004) classification system [12].
Ethical approval was obtained from the Research and development department of UHCW NHS Trust (GF0075) and also University of Warwick (REGO-2015-1682). Descriptive statistical analysis was performed using Microsoft Excel 2010.
Results
There were 1,350,520 admissions during this period of which 39,588 patients died (2.75%). In total, we identified 23 patients with SLE or lupus on death certificate who died at UHCW NHS Trust in this 10 year period, of which one was subsequently excluded as we could not find confirmation of SLE diagnosis. Number of SLE admissions during this period was 1979 (0.14%) with 22 deaths (1.1%). If day case admissions are discounted, there were 1055 admissions in SLE patients leading to death rate of 2.08%.
Demographic data showed 18 of 22 cases were females, with 4 male SLE patients dying in this period. The ethnicity of the patient population was predominantly Caucasian, accounting for 16 out of 22 patients (15 White British, 1 White of other nationality). 4 patients were of South Asian descent (3 Asian Indian and 1 Asian Bangladeshi), 1 patient was from an Afro-Caribbean background and 1 patient was Chinese.
Less than half of these patients [9 of the 22 patients (42%)] were thought to have active disease during the spell of hospitalisation that ended with their death. The youngest patient at death was 23 (2 patients) and the oldest was 85. 15 of 22 patients were above the age 50 at death and 7 patients were under 50.
The overall median age at diagnosis was 41.5 years, ranging from 17 to 72 years. The median age at death was 58.5 years. In patients with active disease the median age at death was 5 years lower than those with inactive disease, at 55.5 versus 60.5 years.
In two cases, SLE was thought to be drug-induced—omeprazole and paclitaxel being the responsible drugs. We were unable to determine the duration of illness in two patients, but we found a median disease length of 14.5 years in the remaining 20 patients. This was dramatically shorter in patients determined to have active disease during their final spell of hospitalisation with median disease duration of 5.5 years.
A number of different causes of death were identified (Table 1). The most common cause of death in this study was infection, with 5 out of 10 infections attributed to pneumonia. Of these, two patients were diagnosed with hospital-acquired pneumonia (one of these grew Streptococcus pneumoniae in the blood, other did not grow any organisms although Staphylococcus aureus was grown from wound swab). 1 patient developed varicella pneumonia, another patient was found to have streptococcal pneumonia and we were unable to determine the type of pneumonia in the last patient. Other infections included one patient with cholecystitis, one patient with peritonitis, one patient with gall bladder empyema, one patient with neutropenic sepsis (neutropenia was attributed to paclitaxel) and one patient with sepsis of uncertain cause. One of these patients had recently received Rituximab to treat SLE. We do not have details of their vaccination status, particularly pneumococcal vaccination.
Pancreatitis was associated with three deaths. In one instance this was related to alcohol, in a second case it was related to surgery and in the third case due to hyperparathyroidism and hypocalcemia. Other causes of death included subdural haemorrhage although no overt previous risk factors for bleeding in the presence of active SLE (one patient), malignancy or malignancy treatment-related complications (three patients), one patient where death resulted from pneumonitis secondary to SLE Vasculitis and three patients with pulmonary disease (chronic obstructive pulmonary disease and interstitial lung disease—which was deemed to be unrelated to SLE). We did not find any deaths related to renal, cardiovascular or thrombotic disease in this cohort (Table 1).
In younger patients (under 50 at death) the main cause of mortality was infection, which was seen in 5 out of 8 patients (62.5%). Other causes of mortality were subdural haemorrhage (1 case), malignancy (1 case) and secondary to radiotherapy for cerebral lymphoma (1 case). Infection was also the main cause of death in patients above the age of 50, deemed to be the cause of death in 6 out of 14 patients (42%). Other causes in this age group included pancreatitis (3 cases or 21%), pulmonary disease (2 cases or 14%), and malignancy (1 case). The remaining patient in this age group was deemed to have died as a result of vasculitis secondary to active SLE.
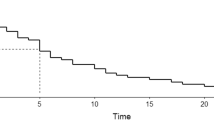
Assessment of system involvement using the BILAG 2004 classification demonstrated that the most common system involved prior to the death of the patients was constitutional symptoms (see Fig. 1), seen in 15 out of the 22 patients (68.2%). Other systems affected were mucocutaneous (10 out of 22), renal (6 out of 22), musculoskeletal (6 out of 22), cardio-respiratory (3 out of 22), neuropsychiatric (1 out of 22) and haematological (2 out of 22). Renal biopsy had been performed in five patients previously, with three of these showing lupus nephritis (1 patient with type 3, 1 patient with type 5, and the last patient with both types 3 and 5) and two others showing tubulointerstitial fibrosis and inflammation. Liver biopsy had been performed in two patients and showed portal and lobular hepatitis in one patient and non-specific findings in the other. Significant renal impairment (CKD 3 or worse) was present in five patients, four of these had biopsies.
Complement levels were found to be low in 6 out of the 22 patients. 14 patients had normal complement levels and 2 patients did not have complement levels checked during their hospital admission. In the nine patients determined to have active SLE, four had low complement levels (44.4%). Hypertension was the most common co-morbidity, seen in 5 patients. 3 patients were diagnosed with epilepsy and three patients had previous cerebrovascular incidents. Rheumatoid arthritis, hypothyroidism, type 2 diabetes, and chronic obstructive pulmonary disease were listed as co-morbidities in two patients each. Other co-morbidities listed included osteoporosis (1 patient), osteoarthritis (3 patients), diverticular disease (1 patient), polycythaemia (1 patient) and ischaemic heart disease (1 patient).
We were able to confirm the antibody profile for 20 of 22 patients, as 2 patients did not have these results available on CRRS. 19 of these 20 patients had positive anti-nuclear antibodies.
The most common antibodies present in these patients were Ro antibodies present in 12/19 patients. DsDNA was positive in 11/19 patients by ELISA and eight patients by Crithidia.
La antibodies were present in nine patients and anti-Smith antibody and u1snRNP antibodies were present in five cases each. We noted that anti phospholipid syndrome was diagnosed in 4 patients (2 additional patients were noted to have positive antiphospholipid antibodies).
Of the 22 cases, 20 were on some form of SLE treatment, where one patient was undergoing chemotherapy for breast cancer and was thought to have drug-induced SLE (paclitaxel).
Most patients were on prednisolone at death with a median dose of 10 mg per day. The second most common drug was hydroxychloroquine which was used at the time of death in 7 patients. Another 7 patients were on Mycophenolate. No patients were on Azathioprine, Methotrexate, Ciclosporin A or Tacrolimus at death. 2 patients had received Rituximab in the past. Cyclophosphamide had previously been used in 2 patients, 3 had been on methotrexate, 6 had been on Azathioprine 1 had previously been on Mycophenolate and Ciclosporin.
Discussion
The study confirms that death in patients with SLE is common, and patients with active disease die younger. In this cohort six patients were less than 50 years of age. However, our mortality data raise some interesting questions when compared with data from recent studies. The study by Rees et al. [8] identified 15 deaths in patients in SLE in the West Midlands during a period from 1999 to 2012. This is significantly lower than the number of patients with diagnosed SLE who died during a shorter period of 2007–2016 at UHCW NHS Trust alone (which is a small part of West Midlands). One possible explanation could be that our study did not exclude patients who had a disease interval of lower than 1 year. There were three patients in our study who would not have met their criteria. Therefore, even accounting for this, it would suggest that SLE is under represented in most clinical data records. A study from London identified 44 patient deaths in their cohort of patients with at least 10 years of follow-up from 1978 to 2004 amongst 401 patients [9]. Our study suggests that a higher number of patients with SLE may have died in hospital than community-based studies indicate and may reflect the inconsistencies in sharing of information between primary and secondary care. It is also important to point out that only a small proportion of GP surgeries is a part of the GPRD, this includes about 20% of the population.
Infection was found to be the most common cause of mortality in our study. It had been identified as a major cause of SLE mortality in a number of previous studies. The reasons for such observations may be due to increased risk of infection from clinically active disease or the use of immunosuppressive agents [15,16,17]. Steroids continue to be used regularly for management of SLE, and may be contributing significantly to this risk. Although steroid-sparing regimes with Rituximab have been trialled [18], this has not yet become standard practice, and the majority of patients with SLE continue to be treated with steroids in some form.
The observation that we did not find any deaths caused by cardiovascular, renal or thrombo-embolic disease was surprising, as previous studies suggested these were a major cause for the increased mortality in patients with SLE [8, 19]. Although cardiovascular disease has been identified as the major cause of mortality in several European and American studies [1, 20], some studies in Korea and China also did not show any mortality from cardiovascular disease [21, 22]. However, renal and thrombo-embolic disease feature highly in mortality data of published studies [1, 19,20,21,22,23]. Changes to NHS practice in terms of waiting times and outcomes of organ transplantation, better management of vascular risk factors and primary coronary interventions may have contributed to this improvement in outcome.
We detected some variation in causes of mortality between the younger and older patients. Whilst infection, malignancy, and subdural haemorrhage were deemed to be responsible for mortality in both cohorts, pancreatitis and pulmonary disease were causes of death only in older patients. Pneumococcal infections were relatively common, and it is unclear whether pneumococcal vaccination might have been able to prevent these infections. For the last 4 years, all rheumatology letters to general practitioners for patients on immunosuppression have included recommendation on pneumococcal and flu vaccination. However, we do not have data regarding how widely it has been utilised.
Malignancy was a major cause of mortality in our patient group, accounting for 3 out of 19 deaths. Of these, 2 patients had primary cancers affecting the brain and the remaining patient died from metastatic breast cancer. This was surprising as studies do not appear to show a significant association between SLE and brain cancer or breast cancer [24]. Different studies have looked into cancer risk in SLE patients, with variable results [25]. A large multicentre prospective cohort study by Bernatsky et al. from 2005 showed an increased overall cancer risk when compared to the general population. This study revealed a significant risk of haematological malignancies but also an increased risk of lung and hepatobiliary cancers [26].
Comparative population data from the UK national statistics show that cancer accounts for 34% of avoidable deaths [27]. Although our data suggest that cancer accounts for 16% of our cohort, the relatively small number of patients may make direct comparison difficult. Brain cancers are the ninth most common cancers in the UK, accounting for 3% of cancer incidences. However, it is associated with high mortality, with an estimated 14% 5 year survival [28].
Anti-Ro antibodies were detected in 57% of our patient group. This is disproportionately high when compared to epidemiological data of prevalence of anti-Ro antibodies in SLE [29, 30]. As expected, low complement levels were found in the majority of patients determined to have active lupus. This may be due to the fact that this is one of the markers used in determining disease activity [19, 29, 31].
The high number of patients on prednisolone and hydroxychloroquine is consistent with current guidelines for management of SLE, with these agents considered first-line therapy and hydroxychloroquine has the added advantage of being relatively safe in the context of acute infection [4]. Steroid use has been associated with a higher risk of infections [32] and there is an urgent need for better drugs that would help manage SLE without the dependence on steroids.
Overall life expectancy for patients with SLE appears to be reduced when compared with the general population. The median age at death in our study was found to be 57.1 years. The average regional life expectancy in the general population during a similar period was 82.4 in females and 74.8 in males [13]. This study was not designed to determine the average life expectancy in patients with SLE, and we are not able to provide accurate estimates of life expectancy in SLE patients in Coventry. Nonetheless, the data we have are consistent with previous studies suggesting a significant reduction in life expectancy [14]. Disease activity is an important factor and our study would indicate that higher disease activity is associated with increased mortality as it was seen to result in a younger age at death and shorter disease duration. This is consistent with previously published results [5,6,7] and continues to highlight the challenges in appropriate management of SLE patients.
Further studies to evaluate average age of death of patients with SLE compared to that of the general population in the region will give a more accurate measure of mortality risk. Previously, Standardised mortality rate (SMR) of 4.6 has been quoted in a Danish study [33]. Management of SLE and improving mortality requires the control of active disease and the prevention or management of long-term sequelae associated with the condition [34]. Further research is needed to investigate changes in SMR with changing times. As more SLE mortality data are revealed in different centres throughout the globe, we may be able to better understand regional trends in mortality of SLE patients in the twenty-first century. This should then allow for a more targeted approach to long-term management of patients with SLE to further improve survival rates.
Limitations
Small numbers of patients in our study population make generalisation difficult
Most retrospective studies are reliant on death certificates to identify patients with SLE [35]. Information in death certificates is subject to systemic biases in reporting (co-morbidities are often under reported) and this may have led to some discrepancies in results. This could have also been the case in our study and it is possible that the study may have omitted some patients with a co-morbid diagnosis of SLE.
Conclusions
Mortality associated with SLE is relatively common in bigger hospitals; in UHCW in Coventry, we have been seeing approximately two deaths a year. Active disease contributing to death is still relatively common. We surprisingly did not find any evidence of deaths from cardiovascular, or thrombo-embolic complications of SLE. Infections were the main cause of mortality in patients with SLE at UHCW and more emphasis on pneumococcal vaccinations is necessary. Regional variations in mortality data may exist in different centres and detailed analyses of these data are important to gain insight into long-term management of patients with SLE.
References
Bernatsky S, Bolvin JF, Joseph L et al (2006) Mortality in systemic lupus erythematosus. Arthritis Rheum 54(8):2550–2557
Uramoto KM, Michet CJ, Thumboo J, Sunko J, O’Fallon WM, Gabriel SE (1999) Trends in the incidence and mortality of systemic lupus erythematosus, 1950–1992. Arthritis Rheum 42(1):46–50
Jorge AM, Lu N, Zhang Y, Rai SK, Choi HK (2018) Unchanging premature mortality trends in systemic lupus erythematosus: a general population-based study (1994–2014). Rheumatology 57(2):337–344
Gordon C, Amissah-Arthur M-B, Gayed M et al (2018) The British Society of Rheumatology guidelines for the management of systemic lupus erythematosus in adults. Rheumatology 57(1):14–18
Chambers SA, Allen E, Rahman A, Isenberg D (2009) Damage and mortality in a group of British patients with systemic lupus erythematosus followed up for over 10 years. Rheumatology 48(6):673–675
Urowitz MB, Gladmann DD (1999) Evolving spectrum of mortality and morbidity in SLE (editorial). Lupus 8:253–255
Yee CS, Su L, Toescu V, Hickman R, Situnayake D, Bowman S, Farewell V, Gordon C (2015) Birmingham SLE cohort: outcomes of a large inception cohort followed up for 21 years. Rheumatology 54(5):836–843
Rees F, Doherty M, Grainge MJ, Lanyon P, Davenport G, Zhang W (2016) Mortality in systemic lupus erythematosus in the United Kingdom 1999-2012. Rheumatology 55(5):854–860
Organ Donation and Transplantation website. https://www.odt.nhs.uk/statistics-and-reports/organ-specific-reports/. Accessed 18 Nov 2018
Kitas G, Nightingale P, Armitage J et al (2015) SAT0105 Trial of atorvastatin for the primary prevention of cardiovascular events in patients with rheumatoid arthritis (TRACE RA). Ann Rheum Dis 74:688
Petri M, Kim MY, Kalunian KC, Grossman J, Hahn BH, Sammaritano LR, Lockshin M, Merrill JT, Belmont HM, Askanase AD, McCune WJ, Hearth-Holmes M, Dooley MA, Von Feldt J, Friedman A, Tan M, Davis J, Cronin M, Diamond B, Mackay M, Sigler L, Fillius M, Rupel A, Licciardi F, Buyon JP (2005) Combined oral contracpetives in women with systemic lupus erythematosus. N Engl J Med 353(24):2550–2558
Isenberg DA, Rahman A, Allen E, Farewell V, Akil M, Bruce IN, D’Cruz D, Griffiths B, Khamashta M, Maddison P, McHugh N, Snaith M, Teh LS, Yee CS, Zoma A, Gordon C, BILAG 2004 (2005) Development and initial validation of an updated version of the British Isles Lupus Assessment Group’s disease activity index for patients with systemic lupus erythematosus. Rheumatology 44(7):902–906. https://doi.org/10.1093/rheumatology/keh624
Public Health England, public health outcomes framework. http://www.phoutcomes.info. Accessed on 20 Nov 2017
Gordon C (2002) Long-term complications of systemic lupus erythematosus. Rheumatology 41(10):1095–1100
Mosca M, Tani C, Aringer M et al (2010) European League Against Rheumatism recommendations for monitoring patients with systemic lupus erythematosus in clinical practice and in observational studies. Ann Rheum Dis 69(7):1269–1274
Nived O, Sturfelt G, Wollheim F (1985) Systemic lupus erythematosus and infection: a controlled and prospective study including an Epidemiological Group. Q J Med 55(218):271–287
Petri M, Genovese M (1992) Incidence of and risk factors for hospitalization in systemic lupus erythematosus: a prospective study of the Hopkins Lupus Cohort. J Rheumatol 19(10):1559–1565
Condon MB, Ashby D, Pepper RJ, Cook HT, Levy JB, Griffith M, Cairns TD, Lightstone L (2013) Prospective observational single-centre cohort study to evaluate the effectiveness of treating lupus nephritis with rituximab and mycophenolate mofetil but no oral steroids. Ann Rheum Dis 72(8):1280–1286
Ho A, Barr SG, Magder LS et al (2001) A decrease in complement is associated with increased renal and haematological activity in patients with systemic lupus erythematosus. Arthritis Rheum 44(10):2350–2357
Manger K, Manger B, Repp R, Geisselbrecht M, Geiger A, Pfahlberg A, Harrer T, Kalden J (2002) Definition of causes for death, end stage renal disease and thromboembolic events in a monocentric cohort of 338 patients with systemic lupus erythematosus. Ann Rheum Dis 61(12):1065–1070
Kim WU, Min JK, Lee SH, Park SH, Cho CS, Kim HY (1999) Causes of death in Korean patients with systemic lupus erythematosus: a single centre retrospective study. Clin Exp Rheumatol 17(5):539–545
Mok CC, Lee KW, Ho CT, Lau CS, Wong RW (2000) A prospective study of survival and prognostic indicators of systemic lupus erythematosus in a southern Chinese population. Rheumatology (Oxford) 39(4):399–406
Moss KE, Ioannou Y, Sultan SM, Haq I, Isenberg D (2002) Outcome of a cohort of 300 patients with systemic lupus erythematosus attending a dedicated clinic for over two decades. Ann Rheum Dis 61(5):409–413
Song L, Wang Y, Zhang J et al (2018) The risks of cancer development in systemic lupus erythematosus (SLE) patients: a systematic review and meta-analysis. Arthritis Res Ther. 20:270. https://doi.org/10.1186/s13075-018-1760-3(Published online 2018 Dec 6)
Dey D, Kenu E, Isenberg DA (2013) Cancer complicating systemic lupus erythematosus—a dichotomy emerging from a nested case-control study. Lupus 22(9):919–927. https://doi.org/10.1177/0961203313497118
Bernatsky S, Bolvin JF, Joseph L (2005) An international cohort study of cancer in systemic lupus erythematosus. Arthritis Rheum 52(5):1481–1490. https://doi.org/10.1002/art.21029
Office for National Statistics. Avoidable mortality in the UK 2016. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/datasets/avoidablemortalityintheuk. Accessed July 2019
Cancer Research UK. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/brain-other-cns-and-intracranial-tumours/survival. Accessed July 2019
Cervera R, Khamashta MA, Font J et al (1993) Systemic lupus erythematosus: clinical and immunological patterns of disease expression in a cohort of 1000 patients. Medicine (Baltimore) 72(2):113–124
Praprotnik S, Bozic B, Kveder T, Rozman B (1999) Fluctuation of anti-Ro/SS antibody levels in patients with systemic lupus erythematosus and sjogren’s syndrome: a prospective study. Clin Exp Rheumatol 17(1):63–68
Kasitanon N, Magder LS, Petri M (2006) Predictors of survival in systemic lupus erythematosus. Medicine (Baltimore) 85(3):147–156
Bosch X, Guilabert A, Pallarés L, Cervera R et al (2006) Infections in systemic lupus erythematosus: a prospective and controlled study of 110 patients. Lupus 15:584–589
Jaconsen S, Petersen J, Ullman S et al (1999) Mortality and causes of death of 513 Danish patients with systemic lupus erythematosus. Scand J Rheum 28:75–80
Urowitz MB, Gladman DD (2000) How to improve mortality and morbidity in patients with systemic lupus erythematosus. Rheumatology 39(3):238–244
Abu-Shakra M, Novack V (2012) Mortality and multiple causes of death in systemic lupus erythematosus- role of the death certificate. J Rheumatol 39(3):458–460
Author information
Authors and Affiliations
Contributions
All three authors have contributed to study design, data collection, data analysis, and write-up. SD and JF led the initial study design and data collection and SD and HA then led the analysis and write-up. All authors fulfil the ICMJE criteria for authorship.
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest and no relevant disclosures.
Ethics approval
Formal ethics approval was obtained from Research and Development department within UHCW NHS Trust.
Informed consent
Written consent has not been obtained from individual patients, as this was not needed as per the ethics approval. No personal identifiable information has been collected for the study. As this is a retrospective study about patients who have died, informed consent is not possible.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anver, H., Dubey, S. & Fox, J. Changing trends in mortality in systemic lupus erythematosus? An analysis of SLE inpatient mortality at University Hospital Coventry and Warwickshire NHS Trust from 2007 to 2016. Rheumatol Int 39, 2069–2075 (2019). https://doi.org/10.1007/s00296-019-04450-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-019-04450-1