Abstract
Introduction/objectives
Recognising systemic lupus erythematosus (SLE) patients at higher risk for hospitalization, aiming at developing tailored management strategies, may help minimize admissions and improve long-term health outcomes. Our study aimed to identify predictors for hospitalization in patients with SLE.
Method
Cohort study of SLE patients followed in a referral centre. All hospitalizations from study baseline up to 120 months were identified, and the primary indication for admission was categorized as follows: (1) SLE disease activity; (2); infection; and (3) other conditions. Demographic, clinical, and laboratory parameters at baseline were sought as predictors of hospitalization for (i) any cause, (ii) disease activity, and (iii) infection using survival analysis with Kaplan–Meier curves and log-rank tests. Potential predictors were further tested using multivariate Cox proportional hazards regression models.
Results
We included 398 patients (median follow-up: 120 months). The incidence rate of hospitalization was 17.7 per 100 patient-years. The most frequent indications for hospitalization were SLE disease activity (29.4%) and infection (23.4%). In multivariate analysis, male gender, age > 50 years, antiphospholipid antibodies positivity (aPL), SLEDAI-2 K > 5, organ damage, and prednisone daily dose (PDN) predicted hospitalization for any cause. SLEDAI-2 K > 5, aPL, PDN, and IS medication predicted hospitalization for active SLE. Male gender, prior biopsy-proven lupus nephritis, aPL, organ damage, and ongoing treatment with high-risk IS predicted hospitalization for infection. Treatment with antimalarials was associated with a lower risk of hospitalization for any cause and for infection.
Conclusions
Positive aPL identifies SLE patients presenting a higher risk of hospitalization, while medication with antimalarials was associated with a lower risk.
Key Points |
• Positive aPL is predictive of hospitalization for any medical condition, disease activity, and infection • Organ damage is predictive of hospitalization for any condition and infection • Antimalarials are predictive of a lower risk of hospitalization for any condition and infection |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The long-term survival of patients with systemic lupus erythematosus (SLE) improved over the last decades, following earlier diagnosis, improved management strategies, and novel treatment approaches [1]. Nevertheless, these patients have a wide gap in health outcomes compared to the general population, including a higher risk of hospitalization, with a significant proportion of patients with SLE being hospitalized during their disease course [1,2,3,4]. The requirement for hospitalizations identifies a subgroup of SLE patients with worse health outcomes, including higher morbidity and mortality [4,5,6,7,8,9], while carrying high direct and indirect costs [10, 11]. Disease activity and infection are consistently reported as the leading causes of hospitalization in these patients [4,5,6,7,8,9, 12,13,14,15,16,17].
Previous studies assessed data collected from national and hospital registries, allowing an extensive portrayal of admission rates, length of stay, causes for admission, costs, and in-hospital mortality [4, 6, 12, 13, 15,16,17,18]. However, they lack individual patient-level clinical information and rely on physician-reported diagnoses of SLE at hospital discharge, which may be inaccurate. Conversely, studies in well-characterized unicentric SLE cohorts were performed to evaluate the incidence, causes, predictors of hospitalization, and predictors of increased length of stay on admission [5, 7, 8, 14, 19], although with smaller sample sizes and shorter follow-up periods. Accounting for the follow-up time until hospitalization with survival analysis may be more suitable to predict which patients have the highest risk for hospitalization, thus allowing risk stratification and its use to optimise patient-level management to reduce admissions and improve long-term health outcomes.
This study aims to identify clinical predictors of hospitalization in SLE patients for any reason and, specifically, for disease activity and infection.
Methods
Study design and population
This single-centre retrospective cohort study included adult SLE patients followed at a tertiary referral centre (CHUC Lupus Clinic) [20,21,22], which provides assistance to a wide geographical area, with more than 50,000 patients hospitalized yearly at this institution. Fulfilment of the revised 1997 American College of Rheumatology (ACR’97) [23] or the Systemic Lupus International Collaborating Clinics (SLICC) [24] classification criteria and compliance with regular follow-up (defined as at least two outpatient visits, no longer than 12 months apart, during the study period) were required for inclusion. This project adhered to the principles of the Declaration of Helsinki and has been approved by the Local Ethics Committee (protocol number CHUC04618). All patients provided written informed consent before inclusion.
Patient assessments and outcomes
The study baseline for each patient was set at their first scheduled outpatient visit during the study period (January 1, 2009, to December 31, 2020). The follow-up period was completed at their last clinical observation up to 120 months from baseline. The electronic database of the CHUC Lupus Clinic cohort and individual medical records from our hospital database were reviewed to characterize each patient at the study baseline and to identify all hospitalizations occurring in our hospital during the inclusion period.
Baseline characteristics assessed for each patient at study baseline included demographic features, SLE cumulative manifestations and immunological features, SLE disease activity, cumulative organ damage, and ongoing medication for SLE, including hydroxychloroquine (HCQ), immunosuppressants (IS), and prednisone (PDN). Positivity to antiphospholipid antibodies (aPL) was considered when medium-to-high levels of immunoglobulin G (IgG) or immunoglobulin M (IgM) anticardiolipin or anti-beta-2-glycoprotein I or positive lupus anticoagulant were measured on at least two occasions, at least 12 weeks apart. Antiphospholipid syndrome (APS) was defined according to classification criteria [25]. Disease activity was scored with the SLE Disease Activity Index 2000 (SLEDAI-2 K) [26] and organ damage with the SLICC/ACR-damage index (SDI) [27].
The primary causes for hospitalization were determined by review of the discharge summary record and categorized as follows: (1) SLE disease activity, (2) infection, or (3) other conditions. Only one primary cause for inpatient admission was considered for each hospitalization event. Hospitalizations for SLE disease activity were further classified according to the main organ manifestation motivating the inpatient admission. Hospitalizations for programmed intravenous administration of therapy or pregnancy, labour, or childbirth complications were excluded from the analysis. The co-primary outcomes of the study included time-to-first hospitalization, up to 120 months from baseline, for (i) any condition; (ii) SLE disease activity; and (iii) infection.
Statistical analysis
Descriptive statistics were performed, with continuous data presented as mean and standard deviation (SD) or median with interquartile range (IQR), as appropriate, and categorical variables presented using frequencies and absolute counts. Comparison of categorical variables among subgroups of patients was performed by applying chi-squared tests, adjusting the significance level according to the number of variables in multiple comparisons with the Bonferroni correction. The incidence rate of hospitalizations was calculated by dividing the number of hospitalizations by the number of patients and observation time at risk.
Survival analyses with Kaplan–Meier curves and log-rank test were applied to test for associations between potential univariate categorical predictors of each outcome. The set of pre-specified candidate variables evaluated at study baseline included gender; age at SLE diagnosis (≤25 vs > 25 years old); age at baseline (≤50 vs > 50 years old); disease duration (≤2 vs > 2 years); SLE classification criteria (fulfilment of ACR’97 vs SLICC criteria alone); SLEDAI-2 K score (≤5 vs > 5); cumulative SLE manifestations (yes/no for each feature); cumulative organ damage (SDI = 0 vs ≥ 1); and ongoing medication with HCQ, IS, or PDN > 7.5 mg/day (yes/no for each class). Regarding time-to-first hospitalization for infection, IS were further categorized as low-risk (methotrexate, sulfasalazine, belimumab) or high-risk (azathioprine, mycophenolate mofetil, calcineurin inhibitors, cyclophosphamide, rituximab) [9].
In a second step, variables with p < 0.1 on the log-rank test for the outcome of interest were included in multivariate analysis applying Cox proportional hazards regression models (backward stepwise method, Wald-based) with estimation of hazard ratios (HR) and 95% confidence intervals (95%CI). Although the PDN daily dose was categorized (≤ 7.5 vs > 7.5 mg/day) according to the 2019 update of the EULAR recommendations for the management of SLE [28] for allowing univariate analysis, it was analysed as a continuous variable in the multivariable analysis. The proportional hazards assumption was verified with log-minus-log plots. Independent variables with p < 0.05 were considered significant. The analysis was performed using IBM SPSS Statistics, version 26.0.
Results
Study population
The baseline characteristics of the 398 patients included are described in Table 1.
Incidence rate and causes for hospitalizations during follow-up
Over a median follow-up of 120 months (IQR = 57.7–120.0) and a total of 3018.6 patient-years, 615 hospitalizations were recorded. After excluding 35 admissions due to pregnancy, labour, or childbirth and 46 for programmed administration of parenteral medication, 534 hospitalizations were included in the analysis.
The incidence rate of hospitalizations was 17.7 per 100 patient-years of follow-up. The median follow-up time until the first admission was 27.2 months (IQR = 9.1–57.8). The most frequent causes for hospitalization were SLE disease activity (29.4%) and infections (23.4%). The exact causes for hospitalization are shown in Supplementary Table S1. Among causes for admission due to SLE disease activity, lupus nephritis was the most frequent (48.4%), followed by haematologic (19.1%) and neuropsychiatric (7.0%) involvement. Pneumonia (28.0%) and urosepsis (26.4%) were the most common infections motivating hospital admission. Almost one-half of the admissions (47.2%) were due to conditions other than SLE disease activity or infection, mainly for elective surgery (27.0%). Admissions potentially related to lupus complications or morbidity, including cardiovascular disease (11.9%), malignancy (7.5%), and renal transplant grafting procedure or complications (7.5%), were also observed. Of note, thrombosis, namely cardiovascular and cerebrovascular events, including myocardial infarction (7), ischaemic stroke (3), and pulmonary embolism (3), motivated 13 (2.4%) admissions.
Predictors of hospitalization for any condition
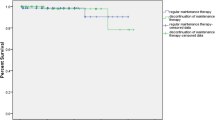
Of the 398 patients participating in the study, 184 (46.2%) were hospitalized for any condition at least once during follow-up. In Supplementary Table S2 and Table 2, results of univariate and multivariate survival analyses of potential risk factors for hospitalization are summarized. In univariate analysis, putative predictors (p < 0.1) at baseline included male gender, age over 50 years, moderate-to-high disease activity with SLEDAI-2 K > 5, ongoing treatment with PDN > 7.5 mg/day, IS medication, organ damage with SDI ≥ 1, and positive aPL. Patients receiving therapy with HCQ presented a lower risk. In the multivariate Cox regression analysis, independent predictors of hospitalization for any condition included (Table 2, Fig. 1) male gender, age > 50 years, aPL positivity, SLEDAI-2 K > 5, SDI ≥ 1, and PDN daily dose. Medication with HCQ was associated with a lower risk for the outcome.
Patients receiving HCQ at study baseline presented previous mucocutaneous lupus more frequently than those not treated with HCQ, without any other significant differences among these subgroups (Supplementary Table S3).
Predictors of hospitalization for SLE disease activity
Of the 398 patients, 94 (23.6%) were hospitalized for SLE disease activity at least once during the follow-up. In univariate analysis (Supplementary Table S2), putative predictors at baseline were: fulfilment of ACR’97 classification criteria; SLEDAI-2 K > 5; previous neuropsychiatric lupus; SDI ≥ 1; aPL positivity; ongoing treatment with PDN > 7.5 mg/day; and IS medication.
In multivariate analysis (Table 2), after adjusting for the other variables in the model, SLEDAI-2 K > 5, positive aPL, PDN daily dose, and IS medication (Table 3, Fig. 2) were confirmed independent predictors.
Predictors of hospitalization for infection
Regarding infections, 69 (17.3%) patients were hospitalized at least once for this cause. In univariate analysis, potential baseline predictors of hospitalization for infection included (Supplementary Table S2) male gender, prior biopsy-proven lupus nephritis, previous neuropsychiatric lupus, serositis, positive aPL, SDI ≥ 1, and ongoing treatment with high-risk IS. Patients receiving HCQ presented a lower risk.
In multivariate Cox regression analysis, male gender, prior biopsy-proven lupus nephritis, positive aPL, SDI ≥ 1, and ongoing treatment with high-risk IS were confirmed independent predictors. Medication with HCQ at baseline was associated with a lower risk for the outcome (Table 2, Fig. 3).
Discussion
In this cohort study, including 398 SLE patients over a median follow-up of 10 years, positive aPL and markers of severe SLE predicted hospitalization, whereas antimalarials were protective. Importantly, positive aPL was predictive of admissions for any condition, SLE disease activity, and infection, regardless of antiphospholipid syndrome criteria fulfilment. Among markers of severe SLE, patients with higher disease activity (SLEDA-2 K > 5), those requiring treatment with higher prednisone daily doses or those receiving IS for severe organ involvement presented an increased risk of hospitalization, as expected. Additionally, patients with lupus nephritis or treated with high-risk IS presented an increased risk of admission for infection. Irreversible organ damage (SDI ≥ 1) was predictive of hospitalization for any condition and infection. Conversely, treatment with antimalarials was associated with 36% and 45% lower risks of hospitalization for any condition and infection, respectively. However, standard-of-care (SOC) treatment with antimalarials or IS was insufficient to abrogate the higher risk of admission for disease activity of patients with severe SLE.
The incidence of hospitalizations was lower than reported in most cohort studies [5, 8, 14], which is in accordance with the study population, comprising primarily Caucasian European patients, with a less severe disease phenotype and inferior damage accrual compared to other ethnicities and geographical areas [29].
Disease activity and infection were the leading causes of hospitalization in SLE patients, as previously reported [3,4,5,6,7,8,9, 12,13,14,15,16,17]. Among hospitalizations for active disease, the primary organ involvements motivating the admission were similar to previous reports [3, 5, 6, 12,13,14, 16, 17, 19]. The most frequent infections leading to admission were also comparable to those of other studies [5, 16]. Notably, a considerable proportion of hospitalizations for other conditions were motivated by complications and morbidity potentially related to SLE and its medication, including cardiovascular disease, malignancy, renal transplantation, and osteoporotic fractures [5, 6, 8, 13, 14, 16, 17, 19].
Remarkably, positivity to aPL, regardless of antiphospholipid syndrome, was predictive of hospitalization for any condition, disease activity, and infection. Although APS has been associated with hospitalization in ICU and mortality [16], an association between aPL positivity and hospitalization has not been previously described. Prior studies suggest that secondary APS and positive aPL in SLE patients imply a more severe disease phenotype regarding non-thrombotic and non-pregnancy-related manifestations, with higher damage accrual and mortality [30,31,32,33]. Since in our cohort few hospitalizations for thrombotic events were observed, with a lower frequency than previously reported [6, 16], and obstetric events were excluded, these causes do not explain the higher risk of admission associated with aPL. Hence, identifying aPL positivity as a predictor of hospitalizations suggests that aPL-related non-thrombotic phenomena may significantly impact health outcomes in SLE patients. Further research is warranted to assess whether these putative effects of aPL are relevant or a surrogate for an underlying variable that may be directly linked to hospitalizations.
Several predictors of hospitalization identified in this study were previously described in other cohort studies, including markers of severe SLE, namely high disease activity [5, 7, 19], daily prednisone dose [5, 7, 13, 16], and SDI, either as a categorical (SDI ≥ 1) [15] or continuous variable [7, 16]. While some studies found an association between shorter disease duration and hospitalization for disease activity [7, 13, 15, 16], in our cohort, disease duration (analysed either as a categorical or continuous variable) did not attain statistical significance after adjusting for confounders, probably because a prevalent cohort and not an inception cohort was analysed. The requirement for IS treatment is a marker of a more severe SLE subset and is associated with a higher risk of flares [21]. Thus, as expected, IS were found to predict hospitalizations for disease activity. Of note, we did not find an association between PDN and hospitalization for infection, which can probably be explained because a single baseline value and not the average corticosteroid dose along the follow-up time was considered.
The effect of antimalarials in reducing disease activity, preventing lupus flares, lowering damage accrual, and improving survival is well established [34,35,36]. Antimalarial use was also associated with reduced cardiovascular risk [37] and reduced infections [15, 16, 38, 39], in either the outpatient or inpatient settings. Our finding that antimalarials were associated with a lower risk of hospitalization for any condition is also consistent with previous evidence [15, 16]. Of note, we compared the subgroups of patients receiving HCQ or not receiving this medication, and there were no relevant differences regarding disease severity or other types of SLE drugs.
A significant strength of our study is that it is based on a large and well-characterized SLE cohort followed over 10 years in a referral lupus clinic. Detailed information regarding each hospitalization episode was available from the patients’ clinical charts and electronic clinical files. Our centre is the primary provider of hospital healthcare for this population, making it unlikely that information regarding hospitalizations is missing. Furthermore, as these patients are enrolled in a SLE prospective cohort study of outcomes, baseline characteristics were systematically collected in the cohort database. Finally, survival analysis is the most appropriate methodologic approach in an open cohort study, where participants are enrolled and can be lost to follow-up over time. However, our study also has some limitations. Variables tested as predictors were set at baseline, although some may be time-varying. This option can facilitate the applicability of the study results in the clinical setting. However, it may have limited the accuracy of the risk estimates associated with SLEDAI-2 K and SLE medications. Secondly, the generalizability of our findings to different ethnic populations and other geographical settings should be carefully considered, especially bearing in mind that patients in this cohort mainly presented low disease activity at baseline.
In conclusion, we newly identified aPL as biomarkers that may be predictive of a higher risk of hospitalization, in addition to other clinical predictors that can be helpful to stratify SLE patients regarding the risk of hospitalizations. These can help clinicians adopt new and tailored management approaches to maintain patients under good control and prevent the need for admissions.
Data availability
The data underlying this article will be shared at reasonable request to the corresponding author.
References
Urowitz MB, Gladman DD, Tom BD, Ibañez D, Farewell VT (2008) Changing patterns in mortality and disease outcomes for patients with systemic lupus erythematosus. J Rheumatol 35(11):2152–2158. https://doi.org/10.3899/jrheum.080214
Arnaud L, Tektonidou MG (2020) Long-term outcomes in systemic lupus erythematosus: trends over time and major contributors. Rheumatology (Oxford) 59(Suppl5):v29–v38. https://doi.org/10.1093/rheumatology/keaa382
Aldarmaki R, Al Khogali HI, Al Dhanhani AM (2021) Hospitalization in patients with systemic lupus erythematosus at Tawam Hospital, United Arab Emirates (UAE): rates, causes, and factors associated with length of stay. Lupus 30(5):845–851. https://doi.org/10.1177/0961203321990086
Krishnan E (2006) Hospitalization and mortality of patients with systemic lupus erythematosus. J Rheumatol 33(9):1770–1774
Petri M, Genovese M (1992) Incidence of and risk factors for hospitalizations in systemic lupus erythematosus: a prospective study of the Hopkins Lupus Cohort. J Rheumatol 19(10):1559–1565
Edwards CJ, Lian TY, Badsha H, Teh CL, Arden N, Chng HH (2003) Hospitalization of individuals with systemic lupus erythematosus: characteristics and predictors of outcome. Lupus 12(9):672–676. https://doi.org/10.1191/0961203303lu452oa
Legge A, Kirkland S, Rockwood K, Andreou P, Bae SC, Gordon C et al (2020) Prediction of hospitalizations in systemic lupus erythematosus using the Systemic Lupus International Collaborating Clinics Frailty Index (SLICC-FI). Arthritis Rheumatol Hoboken, N.J. 72(4):658–666. https://doi.org/10.1002/art.41144
Busch RW, Kay SD, Voss A (2018) Hospitalizations among Danish SLE patients: a prospective study on incidence, causes of admission and risk factors in a population-based cohort. Lupus 27(1):165–171. https://doi.org/10.1177/0961203317734919
Li D, Madhoun HM, Roberts WN Jr, Jarjour W (2018) Determining risk factors that increase hospitalizations in patients with systemic lupus erythematosus. Lupus 27(8):1321–1328. https://doi.org/10.1177/0961203318770534
Anandarajah AP, Luc M, Ritchlin CT (2017) Hospitalization of patients with systemic lupus erythematosus is a major cause of direct and indirect healthcare costs. Lupus 26(7):756–761. https://doi.org/10.1177/0961203316676641
Slawsky KA, Fernandes AW, Fusfeld L, Manzi S, Goss TF (2011) A structured literature review of the direct costs of adult systemic lupus erythematosus in the US. Arthritis Care Res (Hoboken) 63(9):1224–1232. https://doi.org/10.1002/acr.20502
Teh CL, Ling GR (2013) Causes and predictors of mortality in hospitalized lupus patient in Sarawak General Hospital, Malaysia. Lupus 22(1):106–111. https://doi.org/10.1177/0961203312465780
Lee J, Dhillon N, Pope J (2013) All-cause hospitalizations in systemic lupus erythematosus from a large Canadian referral centre. Rheumatology (Oxford) 52(5):905–909. https://doi.org/10.1093/rheumatology/kes391
Lee JW, Park DJ, Kang JH, Choi SE, Yim YR, Kim JE et al (2016) The rate of and risk factors for frequent hospitalization in systemic lupus erythematosus: results from the Korean lupus network registry. Lupus 25(13):1412–1419. https://doi.org/10.1177/0961203316640916
Gu K, Gladman DD, Su J, Urowitz MB (2017) Hospitalizations in patients with systemic lupus erythematosus in an academic health science center. J Rheumatol 44(8):1173–1178. https://doi.org/10.3899/jrheum.170072
Rosa GPD, Ortega MF, Teixeira A, Espinosa G, Cervera R (2019) Causes and factors related to hospitalizations in patients with systemic lupus erythematosus: analysis of a 20-year period (1995–2015) from a single referral centre in Catalonia. Lupus 28(9):1158–1166. https://doi.org/10.1177/0961203319861685
Levy O, Markov A, Drob Y, Maslakov I, Tishler M, Amit-Vazina M (2018) All-cause hospitalizations in systemic lupus erythematosus from a single medical center in Israel. Rheumatol Int 38(10):1841–1846. https://doi.org/10.1007/s00296-018-4147-5
Chakravarty EF, Bush TM, Manzi S, Clarke AE, Ward MM (2007) Prevalence of adult systemic lupus erythematosus in California and Pennsylvania in 2000: estimates obtained using hospitalization data. Arthritis Rheum 56(6):2092–2094. https://doi.org/10.1002/art.22641
Lee J, Peschken CA, Muangchan C, Silverman E, Pineau C, Smith CD et al (2013) The frequency of and associations with hospitalization secondary to lupus flares from the 1000 Faces of Lupus Canadian cohort. Lupus 22(13):1341–1348. https://doi.org/10.1177/0961203313505689
Jesus D, Matos A, Henriques C, Zen M, Larosa M, Iaccarino L et al (2019) Derivation and validation of the SLE Disease Activity Score (SLE-DAS): a new SLE continuous measure with high sensitivity for changes in disease activity. Ann Rheum Dis 78(3):365–371. https://doi.org/10.1136/annrheumdis-2018-214502
Inês L, Duarte C, Silva RS, Teixeira AS, Fonseca FP, da Silva JA (2014) Identification of clinical predictors of flare in systemic lupus erythematosus patients: a 24-month prospective cohort study. Rheumatology (Oxford) 53(1):85–89. https://doi.org/10.1093/rheumatology/ket322
Inês L, Rodrigues M, Jesus D, Fonseca FP, Silva JAP (2018) Risk of damage and mortality in SLE patients fulfilling the ACR or only the SLICC classification criteria. A 10-year, inception cohort study. Lupus 27(4):556–563. https://doi.org/10.1177/0961203317731534
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40(9):1725. https://doi.org/10.1002/art.1780400928
Petri M, Orbai AM, Alarcón GS, Gordon C, Merril JT, Fortin PR et al (2012) Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 64(8):2677–2686. https://doi.org/10.1002/art.34473
Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R et al (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 4(2):295–306. https://doi.org/10.1111/j.1538-7836.2006.01753.x
Gladman DD, Ibañez D, Urowitz MB (2002) Systemic lupus erythematosus disease activity index 2000. J Rheumatol 29(2):288–291
Gladman DD, Urowitz MB (1999) The SLICC/ACR damage index: progress report and experience in the field. Lupus 8(8):632–637. https://doi.org/10.1191/096120399680411335
Fanouriakis A, Kostopoulou M, Alunno A, Aringer M, Bajema I, Boletis J et al (2019) 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis 78:736–745. https://doi.org/10.1136/annrheumdis-2019-215089
Lewis MJ, Jawad AS (2017) The effect of ethnicity and genetic ancestry on the epidemiology, clinical features and outcome of systemic lupus erythematosus. Rheumatology (Oxford) 56(suppl_1):i67–i77. https://doi.org/10.1093/rheumatology/kew399
Ruiz-Irastorza G, Egurbide MV, Ugalde J, Aguirre C (2004) High impact of antiphospholipid syndrome on irreversible organ damage and survival of patients with systemic lupus erythematosus. Arch Intern Med 164(1):77–82. https://doi.org/10.1001/archinte.164.1.77
Riancho-Zarrabeitia L, Martínez-Taboada V, Rúa-Figueroa I, Alonso F, Galindo-Izquierdo M, Ovalles J et al (2020) Antiphospholipid syndrome (APS) in patients with systemic lupus erythematosus (SLE) implies a more severe disease with more damage accrual and higher mortality. Lupus 29(12):1556–1565. https://doi.org/10.1177/0961203320950477
Deák M, Bocskai M, Burcsár S, Dányi O, Fekete Z, Kovács L (2014) Non-thromboembolic risk in systemic lupus erythematosus associated with antiphospholipid syndrome. Lupus 23(9):913–918. https://doi.org/10.1177/0961203314531839
İlgen U, Yayla ME, Ateş A, Okatan IE, Yurteri EU, Torgutalp M et al (2018) Antiphospholipid antibodies and non-thrombotic manifestations of systemic lupus erythematosus. Lupus 27(4):665–669. https://doi.org/10.1177/0961203317734924
Bruce IN, O’Keeffe AG, Farewell V, Hanly JG, Manzi S, Li Su et al (2015) Factors associated with damage accrual in patients with systemic lupus erythematosus: results from the Systemic Lupus International Collaborating Clinics (SLICC) Inception Cohort. Ann Rheum Dis 74:1706–1713. https://doi.org/10.1136/annrheumdis-2013-205171
Alarcón GS, McGwin G, Bertoli AM, Fessler BJ, Calvo-Alén J, Bastian HM et al (2007) Effect of hydroxychloroquine on the survival of patients with systemic lupus erythematosus: data from LUMINA, a multiethnic US cohort (LUMINA L). Ann Rheum Dis 66(9):1168–1172. https://doi.org/10.1136/ard.2006.068676
Ruiz-Irastorza G, Ramos-Casals M, Brito-Zeron P, Khamashta MA (2010) Clinical efficacy and side effects of antimalarials in systemic lupus erythematosus: a systematic review. Ann Rheum Dis 69(1):20–28. https://doi.org/10.1136/ard.2008.101766
Liu D, Li X, Zhang Y, Kwong JSW, Li L, Zhang Y et al (2018) Chloroquine and hydroxychloroquine are associated with reduced cardiovascular risk: a systematic review and meta-analysis. Drug Des Devel Ther 12:1685–1695. https://doi.org/10.2147/DDDT.S166893
Rúa-Figueroa Í, López-Longo J, Galindo-Izquierdo M, Calvo-Alén J, Del Campo V, Olivé-Marqués A et al (2017) Incidence, associated factors and clinical impact of severe infections in a large, multicentric cohort of patients with systemic lupus erythematosus. Semin Arthritis Rheum 47(1):38–45. https://doi.org/10.1016/j.semarthrit.2017.01.010
Prata AR, Luís M, Assunção H, da Silva JAP, Inês LS (2021) Antimalarial treatment and minimizing prednisolone are associated with lower risk of infection in SLE: a 24-month prospective cohort study. Clin Rheumatol 41(4):1069–1078. https://doi.org/10.1007/s10067-021-05988-x
Author information
Authors and Affiliations
Contributions
HA was involved in the bibliographic research, data collection, statistical analysis, interpretation of the data, and manuscript drafting. MR was involved in the data collection and manuscript review. ARP, ML, and JAP da Silva were involved in the manuscript review. LI was involved in the bibliographic research, conception, and design of the study, statistical analysis, interpretation of the data, and manuscript review. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This project was conducted according to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of Centro Hospitalar e Universitário de Coimbra (protocol number CHUC04618). All patients signed an informed consent form before the inclusion in this study.
Consent for publication
Not applicable.
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Assunção, H., Rodrigues, M., Prata, A.R. et al. Predictors of hospitalization in patients with systemic lupus erythematosus: a 10-year cohort study. Clin Rheumatol 41, 2977–2986 (2022). https://doi.org/10.1007/s10067-022-06251-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-022-06251-7