Abstract
Medication adherence is a crucial part in the management of rheumatic diseases, especially with many such patients requiring long-term medications. In this paper, we aim to systematically review the literature for the factors associated with medication adherence in the rheumatic patient population. We carried out a systematic literature search using PubMed®, PsychInfo® and Embase ® with relevant keywords and employed the PRISMA® criteria. We included English peer-reviewed articles that studied the factors affecting medication adherence in patients with rheumatic diseases, which were assessed by two independent reviewers. Hand searches were conducted and relevant factors were extracted and classified using the World Health Organization (WHO)’s five dimensions of medication adherence. A simple diagram was drawn to summarise the factors extracted. 1977 articles were identified and reviewed and 90 articles were found to be relevant. A total of 17 factors and 38 sub-factors were identified and categorized based on the WHO’s five dimensions of medication adherence. A hand model for medication adherence was developed to succinctly summarise these dimension to remind clinicians the importance of medication adherence in daily practice. We conducted a systematic review on the various factors including patient, therapy, condition, health system and socioeconomic-related factors that affected medication adherence in rheumatic patients. We found 17 factors and 38 sub-factors that affected medication adherence in this population. This systematic review can facilitate future focused research in unexplored dimensions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatic disease is an umbrella term that encompasses the spectrum of musculoskeletal, arthritic and connective tissue disorders, which include conditions such as inflammatory bowel disease (IBD), psoriasis (PS), rheumatoid arthritis (RA), ankylosing spondylitis (AS), and psoriatic arthritis (PsA) [1]. Rheumatic diseases are a huge burden on the healthcare system worldwide. This group of diseases accounts for reduction in productivity, significant disability and affects quality of life [3]. A systematic review published in 2014 revealed that about 3% of worldwide population is suffering from inflammatory arthritis [4]. This group of diseases is commonly treated with disease-modifying anti-rheumatic drugs (DMARDs), corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs) [5]. Thus, adherence to the prescribed drugs is important in the prognosis of the disease.
Adherence is defined as a patient’s agreement with the recommendations from physician. It is closely linked with the effectiveness of all pharmacological therapies. As such it is particularly crucial for medications prescribed for chronic diseases. Of all medication-related hospitalizations in the United States, around one-third to two-thirds are the result of poor medication adherence [2]. Non-adherence not only causes therapeutic failure but may also worsen the disease state. Hence, it is believed that increasing adherence may have a far greater impact on health outcomes than advances in medical treatments [6, 7].
According to Arthritis Research UK, drugs that are used for rheumatic diseases are broadly classified into two groups: drugs that treat the symptoms of arthritis (NSAIDs, steroids) and treatments that suppress inflammatory disease and may improve the outcome (DMARDs and Biologics). As biologics are newer class of drugs, it is commonly used in the treatment when other types of DMARDs have not been effective. Owing to these two reasons, adherence to DMARDs and NSAIDs is of utmost importance in order to slow down the progression of the disease, saving patient’s money as well as minimizing risk of side effects.
Adherence is influenced by many factors [8]. The most commonly studied factors are medication characteristic, perceptions and cognitions about illness and medication, socioeconomic and demographic factors, disease features and doctor–patient relationship [9]. As such, we based our factors on the WHO model of medication adherence; this model forms the basis of out theoretical framework and anchor. The variety of factors makes it difficult to understand the complex problems and formulate recommendations or to develop interventions that could help to increase adherence in patients.
Currently, there are systematic reviews looking at adherence rates of DMARDs in various rheumatic diseases [10, 11]. However, there is no succinct summary that seeks to identify, group and present factors affecting medication adherence in Rheumatology as a group. Therefore, the aim of this paper is to identify factors influencing adherence and to assess the association between these factors and adherence.
Methods
A search of literature was performed in online databases: PubMed®, PsychINFO® and Embase®. Keywords used for the search were: (adherence OR compliance OR persistence) AND (rheumatic OR rheumatism OR rheum* OR rheumatology OR lupus OR ankylosing spondylitis OR rheumatoid arthritis OR psoriatic arthritis OR scleroderma OR systemic sclerosis) AND factors AND (drugs OR medication OR medicine). Further hand searches were conducted using references of related articles. The literature review was current as of October 2016 and the start date for articles was unrestricted.
Two independent reviewers (H GOH and YH KWAN) independently reviewed the articles for inclusion and discussed when discrepancies arose.
Inclusion/exclusion criteria: We included full-text original studies published in English-language articles and included patients more than 18 years old with a diagnosis of any rheumatic conditions. Meta analysis, case series, case reports and reviews were excluded.
Subsequently, we identified relevant factors associated with medication adherence and the identified factors were then clustered according to World Health Organization (WHO) recommendations [10]. This includes patient-related factors, therapy-related factors, condition-related factors, health system factors and socioeconomic factors. Finally, a hand model of treatment adherence in rheumatic patients was proposed to help clinicians to better visualize these five categories that affected treatment adherence.
Results
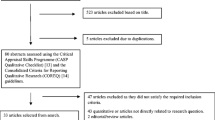
In total, 1977 articles were retrieved from title and abstract screen. After removing 1840 articles that do not fulfill inclusion criteria from full article review and removing 32 duplicates, the final number of articles reviewed was 90 as shown in Fig. 1. The percentage agreement between Goh and Kwan was 90%. A total of 17 factors (38 sub-factors) were identified; we presented statistically significant factors and factors that are not statistically significant, separately and categorized, based on WHO’s five dimensions of adherence. In addition, the types and number of studies that support or do not support a particular factor were also identified. The characteristics of each study are presented in Supplementary Table 1.
Patient-related factors
A total of four main factors were identified under the patient-/caregiver-related category. A total of 29 studies (19 cohort studies, 7 cross-sectional studies, 3 qualitative studies) supported these four factors [12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46]. The number of studies and the types of studies that supported each factor are shown in Table 1.
The most cited factor in this category was ‘Patient’s Demographic Factors’, which encompassed patient’s age, gender, ethnicity and education level. ‘Patient’s Personality Factors’ includes forgetfulness, patient’s coping behaviours, personality traits and quality of life. ‘Patient’s Disease and Treatment Perceptions’ includes disease perception and knowledge, belief for the need of medication and perception towards diagnosis/treatment. ‘Caregiver Issues’ includes caregiver’s personality, dependence on caregiver and caregiver’s negligence.
Therapy-related factors
A total of five main factors were identified under the “Therapy-related factors” category. A total of 31 studies (22 cohort studies, 7 cross-sectional studies, 2 qualitative studies) supported these factors [13, 25, 30, 31, 42, 47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68]. The number of studies and the types of studies that supported each factor are shown in Table 2.
The most cited factor in this category was ‘Choice of drugs’, which encompassed the dosage form of the drugs, properties of the drugs (taste, colour, smell, side) and how to administer the drugs. ‘Side Effects of Therapy’ includes the side effects experienced by patients during the course of treatment which lead to the discontinuation of drugs prescribed. ‘Length and Complexity of Treatment’ includes the duration of treatment, the number of drugs prescribed to the patients as well as dosing regimen. ‘Signs and Symptoms Severity’ suggests that patients would only take the medication regularly when there were worsening of signs and symptoms but will not take them when the signs and symptoms were insignificant. Lastly, ‘Changing of Medical Treatment’ refers to switching the current therapy that the patient was already receiving to another therapy. Patients might not be accustomed to the new therapy and hence were unable to follow the treatment plan completely.
Condition-related factors
A total of two main factors were identified under the “Condition-related factors” category. A total of 8 studies (5 cohort studies, 1 cross-sectional study, 2 qualitative studies) supported these two factors [29, 57, 61, 69,70,71,72]. The number of studies and the types of studies that supported each factor are shown in Table 3. The most cited factor in this category was ‘Depression’.
Health-system-related factors
A total of four main factors were identified under the “Health-system-related factors” category. A total of 10 studies (6 cohort studies, 3 cross-sectional studies, 1 qualitative study) supported these four factors [13, 16, 43, 51, 73,74,75,76,77,78,79]. The number of studies and the types of studies that supported each factor are shown in Table 4. The most cited factor in this category was ‘Poor healthcare provider communication and patient counseling’.
Socioeconomic-related factors
A total of two main factors were identified under the “Condition-related factors” category. A total of 12 studies (9 cohort studies, 2 cross-sectional studies, 1 qualitative study) supported these two factors [16, 25, 78,79,80,81,82,83,84]. The number of studies and the types of studies that supported each factor are shown in Table 5. The most cited factor in this category was ‘Cost issues’.
Hand model of medication adherence in patients with rheumatic diseases
Through these five general categories of factors affecting adherence in rheumatic patients, we propose the hand model as shown in Fig. 2 to allow clinicians to remember these factors better and to apply these factors in their daily practice with rheumatic patients.
Hand model of medication adherence in rheumatic factors based on WHO recommendation [10]
Discussion
This is a systematic review that involved a comprehensive review of literature involving factors affecting medication adherence in population suffering from rheumatological diseases. Although there are numerous studies done on various patient populations, the last systematic review on rheumatology patients was carried out about 7 years back [81]. The present review gives an overview of the types and the number of studies that supported or disagreed with the factors investigated.
There were five categories of factors presented in this hand model of adherence. Each finger represents a domain of factors that clinicians should take note of when assessing adherence in this group of patients. Hand model was designed to incorporate the five categories of factors identified in this review. During their daily practice, clinicians should focus and remember the five domains and apply this model as much as possible so that all factors of adherence can be addressed sufficiently.
In the “Patient-related factors” category, ‘Patient’s Demographic Factors’ was one of the common factors that was reported to cause non-adherence among patients in this category. It was stated that compliance with medication was higher in the older population and younger patients were at a higher risk of non-adherence [17,18,19,20, 35, 37, 38, 40, 41, 85,86,87]. Younger patients were more likely to experience non-adherence especially with regard to procedure-based therapies such as mouth care and central line care. It was also shown that older adolescents were less adherent to treatment as compared to younger adolescents, with the adolescent population defined as between 10 and 18 years old. Possible reasons include that adolescents were undergoing changes and face many problems such as autonomy, independence and separation. This could result in a transfer of medication responsibility between parent and children, thus resulting in disagreements on who was responsible for treatment adherence. It was also found out that different ethnic groups have a different compliance rate with the medication. This could be due to different perceptions on the necessity of medication. For example, three studies concluded that Whites have a higher compliance rate as compared to African American and Chinese [18, 29, 39]. However, as these studies were conducted in different settings, it was possible that there were other confounding factors (such as socioeconomic background) that were not well addressed. Lastly, patients’ belief in the need for medication was supported by ten studies and reinforces the importance of adequate patient education on the pathophysiology of disease, mechanism of action of therapeutics and most importantly patients buy-into adherence.
In the “Therapy-related factors” category, ‘Choice of Drugs and Route of Administration’ was one of the common factors that was reported to cause non-adherence among patients. It was found out adherence to drugs was higher when methotrexate (MTX) was prescribed as compared to treatment plan without methotrexate. A study revealed that concomitant MTX was associated with improved treatment continuation of biologics when compared with both TNF blockers as monotherapy and TNF blockers combined with other DMARDs [64]. We postulate that this was related to dosing frequency, side effects and ease of administration of the drugs. For example, side effects experienced during treatment were supported by nine studies to affect treatment compliance. Another study revealed that replacing hydrochloroquine and sulfasalazine in triple therapy with etanercept and MTX combination increases medication adherence [58]. Hence, these studies support that choice of drugs has a direct impact on affecting patient’s adherence to medication. As most of the biologic DMARDs were parenteral injection, it was found out that medication adherence in patients using subcutaneous injection was high due to ease in administration [64]. This suggests that self-injectable form was effective and well tolerated and was certainly a good addition to the therapeutic armamentarium for carefully selected patients with rheumatic diseases.
In the Condition related factors category, all of the studies we have identified support depression as an important reason behind medication adherence issues and difficulties with adherence were highly correlated with the severity of mental illnesses in which the patient was suffering from [57, 61, 69, 70]. For example, one study suggests that in general, depressed patient was 2.3 times more likely to self-report poor medication adherence than those who were non-depressed. As depression was a recognised comorbidity of people with rheumatic diseases, healthcare professionals supporting people with rheumatic diseases should have awareness of anxiety and depression and refer or screen as appropriate.
In the “Health-system-related factors” category, the majority of educational interventions have focused heavily on provision of information. However, raising the patient's level of understanding on the disease was not associated with increased medication adherence [88]. In fact these studies suggest that the goal of education should be to provide clear and comprehensible information to patients to allow them to make informed healthcare decisions [37]. This could be done by improving the communication between the physician and the patient. Once good rapport was established with the patient, it was more likely for him/her to follow the physician’s instruction. Clear and avoidance of medical jargons during patient counseling allow the patient to better understand the treatment regimen and drug usage [43, 74,75,76,77]. Hence, educational interventions should incorporate more clinician-patient interaction and include read-back to ensure patient understanding.
The “Socioeconomic-related factors” category highlighted that inability to afford the medications for long term has been a major and often neglected concern. One of the studies revealed the average annual cost of some commonly used biologics that a patient needs to pay yearly: adalimumab (US $25,960), abatacept (US $35,581), infliximab (US $36,107) [76]. Therefore, cost of medication was a profound issue that will affect adherence to medication, as most of the patients would require the use of these medications for a long period, if not throughout their remaining lifespan. In addition, multiple drug combinations were commonly used in treating rheumatic diseases, which will further increase the burden of cost of medications to the patient [84]. As such, patients who were at the borderline of poverty have the highest risk of discontinuing the medications due to financial constraints [16, 25, 78,79,80,81,82]. Thus, clinicians should discuss this issue with the patient so as to assess his financial capabilities and refer him for appropriate help when needed.
In terms of the types of studies, we found out that quantitative studies comprised of about 79% of the literature found, the rest being qualitative studies. A wide variety of study designs were used, including but not limited to case control studies, cohort studies, cross sectional studies and qualitative studies. Future studies should include quantitative components to measure the magnitude of effect that each factor has on medication adherence, in order to identify major causes and optimize resource allocation to improve adherence in those areas showing larger magnitude effect.
A weakness in this study was that this was a systematic review and not a meta-analysis of the various effects of factors on adherence. Although there were 17 factors in five categories and 38 sub-factors identified in this review, we do not know the aggregate magnitude of each factor on adherence rate in rheumatic patients. However, in our review, we have summarized as much as possible the available literature and presented the various factors succinctly into five major categories in order to allow clinicians to better understand the complex nature of adherence.
In conclusion, 17 factors in five categories and 38 sub-factors were found to be associated with the adherence in rheumatic patients. Clinicians would need to be cognizant of the complex nature of medication adherence in this population, and systematically address these risk factors in the patient in order to optimize therapeutic outcomes.
References
Greenstein B, Greenstein A (2007) Concise clinical pharmacology. Pharmaceutical Press, London, p 102
Brown M, Bussell J (2011) Medication adherence: WHO cares? Mayo Clin Proc 86(4):304–314
Sangha O (2000) Epidemiology of rheumatic diseases. Rheumatology 39(Suppl 2):3–12
Hoving JL, Lacaille D, Urquhart DM, Hannu TJ, Sluiter JK, Frings-Dresen MH (2014) Non-pharmacological interventions for preventing job loss in workers with inflammatory arthritis. The Cochrane database of systematic reviews. Cd010208
Smolen JS, Breedveld FC, Burmester GR et al (2016) Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Ann Rheum Dis 75:3–15
Zomahoun HT, Guenette L, Gregoire JP et al (2016) Effectiveness of motivational interviewing interventions on medication adherence in adults with chronic diseases: a systematic review and meta-analysis. Int J Epidemiol 46(2):589–602
Krueger KP, Berger BA, Felkey B (2005) Medication adherence and persistence: a comprehensive review. Adv Ther 22:313–356
De Geest S, Sabate E (2003) Adherence to long-term therapies: evidence for action. Eur J Cardiovasc Nurs 2:323
Wabe N, Lee A, Wechalekar M, McWilliams L, Proudman S, Wiese M (2017) Adherence to combination DMARD therapy and treatment outcomes in rheumatoid arthritis: a longitudinal study of new and existing DMARD users. Rheumatol Int 6(37):897–904
de Achaval S, Suarez-Almazor ME (2010) Treatment adherence to disease-modifying antirheumatic drugs in patients with rheumatoid arthritis and systemic lupus erythematosus. Int J Clin Rheumatol 5:313–326
Burkhart PV, Sabate E (2003) Adherence to long-term therapies: evidence for action. J Nurs Scholarsh 35:207
Bernatsky S, Ehrmann Feldman D (2008) Discontinuation of methotrexate therapy in older patients with newly diagnosed rheumatoid arthritis: analysis of administrative health databases in Québec, Canada. Drugs Aging 25:879–884
Brandstetter S, Hertig S, Loss J, Ehrenstein B, Apfelbacher C (2016) The lesser of two evils…’—views of persons with rheumatoid arthritis on medication adherence: a qualitative study. Psychol Health 31:675–692
Bruera S, Barbo AG, Lopez-Olivo MA (2016) Use of medication reminders in patients with rheumatoid arthritis. Rheumatol Int 36:1543–1548
Brus H, van de Laar M, Taal E, Rasker J, Wiegman O (1999) Determinants of compliance with medication in patients with rheumatoid arthritis: the importance of self-efficacy expectations. Patient Educ Couns 36:57–64
Bugni VM, Ozaki LS, Okamoto KY et al (2012) Factors associated with adherence to treatment in children and adolescents with chronic rheumatic diseases. J Pediatria 88:483–488
Choi JY, Cho SK, Choi CB et al (2014) The risk factors for nonadherence to anti-rheumatic treatment in patients with rheumatoid arthritis. Ann Rheumatic Dis 73(Suppl 2):913
Chu LH, Kawatakar AA (2012) Long term medication adherence of adalimumab and etanercept among rheumatoid arthritis patients in Kaiser Permanente Southern California. Value Health 15:A40
Dalbeth N, Petrie KJ, House M et al (2011) Illness perceptions in patients with gout and the relationship with progression of musculoskeletal disability. Arthritis Care Res 63:1605–1612
De Cuyper E, De Gucht V, Maes S, Van Camp Y, De Clerck LS (2016) Determinants of methotrexate adherence in rheumatoid arthritis patients. Clin Rheumatol 35:1335–1339
Denoeud L, Mazieres B, Payen-Champenois C, Ravaud P (2005) First line treatment of knee osteoarthritis in outpatients in France: adherence to the EULAR 2000 recommendations and factors influencing adherence. Ann Rheum Dis 64:70–74
Ekşioǧlu E, Çakir B, Gürçay E, Çakci A (2005) Factors affecting medical treatment compliance in one-year follow up of rheumatoid arthritis patients. J Rheumatol Med Rehabil 16:177–182
Elliott RA (2008) Poor adherence to medication in adults with rheumatoid arthritis: reasons and solutions. Dis Manag Health Outcomes 16:13–29
Gadallah MA, Boulos DN, Gebrel A, Dewedar S, Morisky DE (2015) Assessment of rheumatoid arthritis patients’ adherence to treatment. Am J Med Sci 349:151–156
Gross R, Graybill J, Wahezi D, Jordan NC, Putterman C, Blanco I (2014) Increased education is associated with decreased compliance in an urban multi-ethnic lupus cohort. J Clin Cell Immunol 5:215–230
Hromadkova L, Soukup T, Vlcek J (2015) Quality of life and drug compliance: their interrelationship in rheumatic patients. J Eval Clin Prac 21:919–924
Koneru S, Kocharla L, Higgins GC et al (2008) Adherence to medications in systemic lupus erythematosus. J Clin Rheumatol 14:195–201
Kumar K, Gordon C, Barry R, Shaw K, Horne R, Raza K (2011) ‘It’s like taking poison to kill poison but I have to get better’: a qualitative study of beliefs about medicines in Rheumatoid arthritis and Systemic lupus erythematosus patients of South Asian origin. Lupus 20:837–844
Kumar K, Raza K, Nightingale P et al (2015) Determinants of adherence to disease modifying anti-rheumatic drugs in White British and South Asian patients with rheumatoid arthritis: a cross sectional study. BMC Musculoskelet Disord 16:396
Li P, Blum MA, Von Feldt J, Hennessy S, Doshi JA (2010) Adherence, discontinuation, and switching of biologic therapies in medicaid enrollees with rheumatoid arthritis. Value Health 13:805–812
Loew L, Brosseau L, Kenny GP et al (2016) Factors influencing adherence among older people with osteoarthritis. Clin Rheumatol 35:2283–2291
Marchesoni A, Zaccara E, Gorla R et al (2009) TNF-alpha antagonist survival rate in a cohort of rheumatoid arthritis patients observed under conditions of standard clinical practice. Ann NY Acad Sci 1173:837–846
Morgan C, McBeth J, Cordingley L et al (2015) The influence of behavioural and psychological factors on medication adherence over time in rheumatoid arthritis patients: a study in the biologics era. Rheumatology 54:1780–1791
Müller R, Kallikorm R, Põlluste K, Lember M (2012) Compliance with treatment of rheumatoid arthritis. Rheumatol Int 32:3131–3135
Neame R, Hammond A (2005) Beliefs about medications: a questionnaire survey of people with rheumatoid arthritis. Rheumatology 44:762–767
Pascual-Ramos V, Contreras-Yanez I, Villa AR, Cabiedes J, Rull-Gabayet M (2009) Medication persistence over 2 years of follow-up in a cohort of early rheumatoid arthritis patients: associated factors and relationship with disease activity and with disability. Arthritis Res Ther 11:R26
Pasma A, van’t Spijker A, Hazes JM, Busschbach JJ, Luime JJ (2013) Factors associated with adherence to pharmaceutical treatment for rheumatoid arthritis patients: a systematic review. Semin Arthritis Rheum 43:18–28
Pavelka K, Forejtova S, Stolfa J et al (2009) Anti-TNF therapy of ankylosing spondylitis in clinical practice. Results from the Czech national registry ATTRA. Clin Exp Rheumatol 27:958–963
Salaffi F, Carotti M, Di Carlo M, Farah S, Gutierrez M (2015) Adherence to anti-tumor necrosis factor therapy administered subcutaneously and associated factors in patients with rheumatoid arthritis. J Clin Rheumatol 21:419–425
Tesher MS, Onel KB (2012) The clinical spectrum of juvenile idiopathic arthritis in a large urban population. Curr Rheumatol Rep 14:116–120
Tuncay R, Eksioglu E, Cakir B, Gurcay E, Cakci A (2007) Factors affecting drug treatment compliance in patients with rheumatoid arthritis. Rheumatol Int 27:743–746
van den Bemt BJ, van den Hoogen FH, Benraad B, Hekster YA, van Riel PL, van Lankveld W (2009) Adherence rates and associations with nonadherence in patients with rheumatoid arthritis using disease modifying antirheumatic drugs. J Rheumatol 36:2164–2170
Viller F, Guillemin F, Briancon S, Moum T, Suurmeijer T, van den Heuvel W (1999) Compliance to drug treatment of patients with rheumatoid arthritis: a 3 year longitudinal study. J Rheumatol 26:2114–2122
Wong M, Mulherin D (2007) The influence of medication beliefs and other psychosocial factors on early discontinuation of disease-modifying anti-rheumatic drugs. Musculoskelet Care 5:148–159
Zandman-Goddard G, Amital H, Shamrayevsky N, Raz R, Shalev V, Chodick G (2013) Rates of adherence and persistence with allopurinol therapy among gout patients in Israel. Rheumatology 52:1126–1131
Zwikker HE, van Dulmen S, den Broeder AA, van den Bemt BJ, van den Ende CH (2014) Perceived need to take medication is associated with medication non-adherence in patients with rheumatoid arthritis. Patient Preference Adherence 8:1635–1645
Agarwal S, Zaman T, Handa R (2009) Retention rates of disease-modifying anti-rheumatic drugs in patients with rheumatoid arthritis. Singapore Med J 50:686–692
Bendtsen P, Bjurulf P, Trell E, Lindstrom F, Larsson JE (1994) Treatment perspectives in rheumatoid arthritis: a descriptive study in a Swedish healthcare district. PharmacoEconomics 5:399–407
De Cuyper E, De Gucht V, Maes S, Van Camp Y, De Clerck LS (2016) Determinants of methotrexate adherence in rheumatoid arthritis patients. Clin Rheumatol 35:1335–1339
Doddapaneni S, Shetty R, Sabih I, Maddali K, Khera K (2014) Assessment of medication adherence in rheumatoid arthritis patients in a tertiary care hospital. Value Health 17:A774
Kumar K, Raza K, Gill P, Greenfield S (2016) The impact of using musculoskeletal ultrasound imaging and other influencing factors on medication adherence in patients with rheumatoid arthritis: a qualitative study. Patient Preference Adherence 10:1091–1100
Mjaavatten MD, Radner H, Yoshida K et al (2014) Inconsistent treatment with disease-modifying antirheumatic drugs: a longitudinal data analysis. J Rheumatol 41:2370–2378
Chu LH, Kawatkar AA, Gabriel SE (2015) Medication adherence and attrition to biologic treatment in rheumatoid arthritis patients. Clin Ther 37(660–66):e8
de Thurah A, Norgaard M, Johansen MB, Stengaard-Pedersen K (2010) Methotrexate compliance among patients with rheumatoid arthritis: the influence of disease activity, disease duration, and co-morbidity in a 10-year longitudinal study. Scand J Rheumatol 39:197–205
Li LM, Tessier-Cloutier B, Wang Y et al (2013) Assessing process of care in rheumatoid arthritis at McGill University hospitals. J Clin Rheumatol 19:175–179
Rashid N, Coburn BW, Wu YL et al (2015) Modifiable factors associated with allopurinol adherence and outcomes among patients with gout in an integrated healthcare system. Journal Rheumatol 42:504–512
Xia Y, Yin R, Fu T et al (2016) Treatment adherence to disease-modifying antirheumatic drugs in Chinese patients with rheumatoid arthritis. Patient Preference Adherence 10:735–742
Bonafede M, Johnson BH, Tang DH, Shah N, Harrison DJ, Collier DH (2015) Etanercept-methotrexate combination therapy initiators have greater adherence and persistence than triple therapy initiators with rheumatoid arthritis. Arthritis Care Res 67:1656–1663
Contreras-Yanez I, Ponce De Leon S, Cabiedes J, Rull-Gabayet M, Pascual-Ramos V (2010) Inadequate therapy behavior is associated to disease flares in patients with rheumatoid arthritis who have achieved remission with disease-modifying antirheumatic drugs. Am J Med Sci 340:282–290
de Vlam K, Boone C, The Prove Study Group A (2015) Treatment adherence, efficacy, and safety of etanercept in patients with active psoriatic arthritis and peripheral involvement in Belgium for 66 months (PROVE study). Clin Exp Rheumatol 33:624–631
Drenkard C, Dunlop-Thomas C, Easley K, Bao G, Brady T, Lim SS (2012) Benefits of a self-management program in low-income African-American women with systemic lupus erythematosus: results of a pilot test. Lupus 21:1586–1593
Hetland ML, Christensen IJ, Tarp U et al (2010) Direct comparison of treatment responses, remission rates, and drug adherence in patients with rheumatoid arthritis treated with adalimumab, etanercept, or infliximab: results from eight years of surveillance of clinical practice in the nationwide Danish DANBIO registry. Arthritis Rheum 62:22–32
Kim G, Barner JC, Rascati K, Richards K (2016) Examining time to initiation of biologic disease-modifying antirheumatic drugs and medication adherence and persistence among texas medicaid recipients with rheumatoid arthritis. Clin Ther 38:646–654
Kristensen LE, Saxne T, Nilsson JA, Geborek P (2006) Impact of concomitant DMARD therapy on adherence to treatment with etanercept and infliximab in rheumatoid arthritis. Results from a six-year observational study in southern Sweden. Arthritis Res Ther 8:R174
Malaviya AP, Ostor AJ (2012) Drug adherence to biologic DMARDS with a special emphasis on the benefits of subcutaneous abatacept. Patient Preference Adherence 6:589–596
Wong PK (2016) Medication adherence in patients with rheumatoid arthritis: why do patients not take what we prescribe? Rheumatol Int 36:1535–1542
Prudente LR, Diniz Jde S, Ferreira TX et al (2016) Medication adherence in patients in treatment for rheumatoid arthritis and systemic lupus erythematosus in a university hospital in Brazil. Patient Preference Adherence 10:863–870
Aaltonen KJ, Turunen JH, Sokka T, Puolakka K, Valleala H (2016) A survey on the medication adherence to methotrexate among rheumatoid arthritis patients treated with self-administered biologic drugs. Clin Exp Rheumatol 34:694–697
Cabrera-Marroquin R, Contreras-Yanez I, Alcocer-Castillejos N, Pascual-Ramos V (2014) Major depressive episodes are associated with poor concordance with therapy in rheumatoid arthritis patients: the impact on disease outcomes. Clin Exp Rheumatol 32:904–913
Julian LJ, Yelin E, Yazdany J et al (2009) Depression, medication adherence, and service utilization in systemic lupus erythematosus. Arthritis Rheum 61:240–246
Abobului M, Berghea F, Vlad V et al (2015) Evaluation of adherence to anti-osteoporosis treatment from the socio-economic context. Journal of medicine and life 8:119–123 (spec issue)
Flower C, Hambleton I, Campbell M (2016) The effect of psychosocial and neuropsychiatric factors on medication adherence in a cohort of women with systemic lupus erythematosus. J Clin Rheumatol 22:411–417
Iudici M, Russo B, Mitidieri M, Cuomo G, Valentini G (2015) Glucocorticoids in systemic sclerosis: patients’ beliefs and treatment adherence. Scand J Rheumatol 44:229–237
Arshad N, Ahmad NM, Saeed MA, Khan S, Batool S, Farman S (2016) Adherence to Methotrexate therapy in Rheumatoid Arthritis. Pak J Med Sci 32:413–417
Broderick JE, Stone AA, Smyth JM, Kaell AT (2004) The feasibility and effectiveness of an expressive writing intervention for rheumatoid arthritis via home-based videotaped instructions. Ann Behav Med 27:50–59
Durcan L, Clarke WA, Magder LS, Petri M (2015) Hydroxychloroquine blood levels in systemic lupus erythematosus: clarifying dosing controversies and improving adherence. J Rheumatol 42:2092–2097
Geryk LL, Blalock S, DeVellis RF, Morella K, Carpenter DM (2016) Associations between patient characteristics and the amount of arthritis medication information patients receive. J Comm 21:1122–1130
Abdul-Sattar AB, Abou El Magd SA (2015) Determinants of medication non-adherence in Egyptian patients with systemic lupus erythematosus: Sharkia Governorate. Rheumatol Int 35:1045–1051
Pascual-Ramos V, Contreras-Yanez I (2013) Motivations for inadequate persistence with disease modifying anti-rheumatic drugs in early rheumatoid arthritis: the patient’s perspective. BMC Musculoskelet Disord 14:336
Bonafede M, Johnson BH, Princic N, Shah N, Harrison DJ (2015) Cost per patient-year in response using a claims-based algorithm for the 2 years following biologic initiation in patients with rheumatoid arthritis. J Med Econ 18:376–389
Nasser-Ghodsi N, Harrold LR (2015) Overcoming adherence issues and other barriers to optimal care in gout. Curr Opin Rheumatol 27:134–138
Solomon DH, Tonner C, Lu B et al (2014) Predictors of stopping and starting disease-modifying antirheumatic drugs for rheumatoid arthritis. Arthritis Care Res 66:1152–1158
Wan SW, He HG, Mak A et al (2016) Health-related quality of life and its predictors among patients with rheumatoid arthritis. Appl Nurs Res 30:176–183
Carter EE, Barr SG, Clarke AE (2016) The global burden of SLE: prevalence, health disparities and socioeconomic impact. Nat Rev Rheumatol 12:605–620
Yap Angela Frances, Thiru Thirumoorthy Yu, Kwan Heng (2016) Medication adherence in the elderly. J Clin Gerontol Geriatrics 2016(10):1016
Yap Angela Frances, Thiru Thirumoorthy Yu, Kwan Heng (2015) Systematic review of the barriers affecting medication adherence in older adults. Geriatrics Gerontol Int 2015(10):1111
Goh XTW, Tan YB, Thirumoorthy T, Kwan YH (2016) A systematic review of factors that influence treatment adherence in paediatric oncology patients. J Clin Pharm Ther 42:1–7
Joplin S, van der Zwan R, Joshua F, Wong PKK (2015) Medication adherence in patients with rheumatoid arthritis: the effect of patient education, health literacy, and musculoskeletal ultrasound. Biomed Res Int 2015:150658
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
No potential conflicts of interest were disclosed.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Funding
No funding was involved in this study.
Additional information
Co-first authors: Hendra Goh, Yu Heng Kwan and Yi Seah.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Goh, H., Kwan, Y.H., Seah, Y. et al. A systematic review of the barriers affecting medication adherence in patients with rheumatic diseases. Rheumatol Int 37, 1619–1628 (2017). https://doi.org/10.1007/s00296-017-3763-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-017-3763-9