Abstract
Streptococcus agalactiae (GBS) is a colonizing agent in pregnant women, the main cause of invasive neonatal infections, and the reason of serious diseases in non-pregnant adults. Several virulence determinants are involved in the pathogenesis. These include capsular polysaccharide, surface-localized proteins, and toxins. Penicillin is considered the first choice antibiotic for the treatment and prophylaxis; erythromycin, clindamycin and fluoroquinolones are recommended alternatives for penicillin-allergic GBS carriers or patients. Our objective was to investigate the virulence genetic characteristics and the antimicrobial susceptibility of 162 GBS colonizing and infective isolates recovered in Argentina. Serotypes Ia and III were the most prevalent ones, followed by Ib, II, V, IV and non-typeable. In relation to the 13 virulence genes screened, cpsA, cylE, hylB, lmb, and scpB were the most prevalent and could be postulated as vaccine epitopes; bca, rib, bac, hvgA, spb1, PI, PI-2a, and PI-2b were detected in lesser frequencies. No significant association was found between serotypes or virulence genes and colonizing or infective isolates but, on the contrary, significant association was observed between some genes and the most prevalent serotypes, la and III. The cluster analysis showed 52 virulence profiles and, antimicrobial resistance tests, 16 profiles, some with up to 4 resistances. Tetracycline resistance was significantly associated with colonizing isolates. Genes tetM and ermB conferring resistance to tetracyclines and macrolides, respectively, were the most commonly identified. Our findings show that GBS colonizing and infective isolates circulating in Argentina share similar features in terms of serotype and virulence genes and show a high level of antimicrobial resistance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Streptococcus agalactiae, or Group B Streptococcus (GBS), is the leading cause of neonatal sepsis and meningitis and an important cause of infections in pregnant and nonpregnant adults, particularly among the elderly and those with underlying comorbidities [1, 2]. On the other hand, GBS is part of the normal gastrointestinal or genitourinary flora of healthy adults.
Asymptomatic colonization of pregnant women is the leading source of neonatal GBS infection, and has also been associated with an increased risk of prematurity and stillbirth. The vaginal colonization rate in pregnant women is not equal between different geographical areas. The estimated maternal GBS colonization worldwide average is 18%, with a range between 11 and 35% [3]. In Argentina, although information regarding national GBS colonization rate is scarce, regional data show that between 1.4 and 18% of pregnant women are colonized by GBS [4]. In order to prevent this route of transmission, universal screening for recto- vaginal GBS colonization is recommended for pregnant women between 35 and 37 weeks of gestation and carriers receive intrapartum antibiotic prophylaxis (IAP). In Argentina, the search for GBS in all pregnant women is mandatory since 2008, according to the National Law N° 26369. IAP has reduced the incidence of early onset neonatal disease without a notable impact on the incidence of late-onset neonatal disease [5].
Beta-lactams remain appropriate for first line treatment and prophylaxis as GBS is still sensitive to penicillin but isolates with reduced susceptibility have been reported [6, 7]. Erythromycin, clindamycin and fluoroquinolones are recommended alternatives for penicillin-allergic GBS carriers or patients or when therapeutic failure is suspected. Increased frequency of resistance to these non-beta-lactam antibiotics has been observed, therefore continued monitoring of antimicrobial resistance (AMR) is essential [8].
GBS has a variety of virulence factors that facilitate its ability to cause disease. Several virulence determinants are involved in the adhesion and invasion of host cells, as well as in evasion from the immune system [9]. These include capsular polysaccharide (CPS), regulatory proteins, surface-localized proteins, and toxins. The CPS is an antigenic determinant and a major virulence factor as it interferes with complement mediated killing [10]. GBS can be classified into ten serotypes based on CPS types (Ia–Ib, II–IX) [11]. CPS is presented in combination with different surface proteins including α-C and ß-C, Rib, Lmb, C5a peptidase, HylB, and β-haemolysin, among others [9]. Vaccines targeting capsule polysaccharides and common proteins are under development. The frequency of the genes that encode them varies by origin of the strains, geographic location as well as serotypes [12].
Our hypothesis is that GBS is differentiated into subpopulations according to whether they are infective or colonizing strains. This study aimed to analyse the virulence profiles and antimicrobial resistance of Streptococcus agalactiae isolates from the Argentina Pampa region.
Materials and Methods
Isolates Collection
Between 2010 and 2020, we received 189 S. agalactiae isolates obtained and identified using standard biochemical criteria and sent from health centers (three hospitals and three biochemical laboratories) of the Argentinean Pampa region of Argentina. The isolates identified by routine diagnostics as GBS were classified as infective or colonizing strains. Sources of the infective isolates were symptomatic non-pregnant people. This group included mostly adults of different ages (with the exception of three infants), both females and males, with symptomatic disease. We received infective isolates recovered from blood, soft tissue, urinary and vaginal infections. Sources of the colonizing isolates were pregnant women tested between 35 and 37 weeks of pregnancy. The isolates were recovered from vaginal swabs (according to the Argentinean regulation 26369/2008). Of 189 isolates received, 162 could be confirmed by amplifying a region of the monocopy regulatory gene dltR, specific to S. agalactiae [13].
Serotyping and Detection of Virulence-Associated Genes
The capsular type identification, Ia, Ib, II–IX, was determined by PCR according to Imperi et al. [14]. A total of thirteen virulence genes associated with adhesion and colonization, invasion, tissue damage and/or immune evasion were amplificated by PCR. The genes encoding virulence factors analysed were: bca and bac (alpha and beta subunits of protein C), lmb (laminin-binding protein), rib and spb1 (surface proteins), cpsA (capsule component, survival of the pathogen in the host), scpB (peptidase C5a), cylE (pore-forming toxin β-haemolysin), hylB (enzyme, degradation hyaluronic acid) [15,16,17,18] and PI1, PI2a and PI2b (pilus structures, colonization and invasion of host tissues and formation of biofilms) [19]. Also, a 210 bp genetic region encoding the S10 domain of the HvgA surface protein, from the gbs2018 allele, described as specific for ST-17 was amplified [13]. The primers used to amplify DNA regions specific to virulence genes in GBS isolates are listed in Suppl. Mat. Table 1. The DNA template for PCR assays was obtained by boiling frozen bacteria suspended in sterile water for 10 min. The PCR products were visualized in 2% agarose gel stained by ethidium bromide.
Antimicrobial Susceptibility
Antimicrobial susceptibility to clindamycin (CLI), erythromycin (ERY), levofloxacin (LEV), penicillin (PEN) and tetracycline (TET), was tested in 93 isolates by disc diffusion method according to Clinical and Laboratory Standards Institute [20]. The interpretation of results for NOR was performed following the recommendations of the Clinical and Laboratory Standards Institute [21] (Suppl. Mat. Table 2). A bacterial suspension in sterile saline solution from an overnight pure culture, adjusted to a turbidity of 0.5 on the McFarland scale, was inoculated on a Muller-Hinton agar (Britania) plate, supplemented with 5% ovine blood. Antibiotic discs (Britania) were placed on the agar surface and plates were incubated overnight (16–18 h) at 37 °C in an atmosphere with 5% CO2. Antimicrobial resistance (AMR) was defined as non-susceptibility to a given antimicrobial by combining intermediate (or susceptible with increased exposure) and resistant categories into a single category. On the other hand, AMR genes were investigated. The macrolide resistance gene ermB, was amplified by PCR according to Zhou et al. [22], tetracycline resistance genes tetM and tetO, according to Lopardo et al. [23], lincosamide resistance gene linB, according to Bozdogan et al. [24] (Suppl. Mat. Table 1).
Data Analysis
The statistical associations between serotypes, virulence genes, antimicrobial resistance and isolates source, and between serotypes and virulence genes were analysed by 2 × 2 contingency tables, chi-square test (χ2), and Fisher exact test, with a confidence level of 95%, using the software Epi Info™ 7.1.5.2.
Taking into account the combinations of the genes detected in the present study, virulence profiles were defined. A cluster analysis was carried out using the UPGMA clustering method. The dendrogram was generated using the BioNumerics v.6.6 software.
Results
Molecular Identification, Virulence and Serotypes of S. agalactiae
Among the 162 isolates, the percentages of colonizing and infective isolates were 78% and 22%, respectively. Six serotypes and non-typeable isolates were detected. Serotypes Ia and III were the most prevalent ones (38% and 30%, respectively) followed by Ib, II, and V (Fig. 1a). Also, among colonizing isolates a serotype IV isolate was detected, meanwhile among infective isolates, an isolate was non-typeable. No significant association was found between the serotypes and colonizing or infective GBS isolates (p > 0.05) (Fig. 1b).
In relation with virulence-associated genes screened, cpsA, cylE, hylB (100%), lmb (98%), and scpB (91%) were the most prevalent, meanwhile, the other ones were detected in lesser frequencies, PI-2a (73%), bca (66%), PI-1 (50%), rib (32%), bac (23%), PI-2b (14%) and spb1 (12%). The genes bac, rib and PI-2a predominated in colonizing isolates over infective ones, and on the contrary, spb1, PI-1 and PI-2b predominated in infective isolates. However, no significant association was found between virulence genes and colonizing or infective strains (p > 0.05) (Table 1).
The genes rib and PI-2b were detected only in serotypes III, Ia, and II, meanwhile spb1, in III and Ia isolates (Fig. 2). The hvgA gene (reported as specific for the ST-17) was detected in 33 isolates (20%). The majority (82%) of the hvgA-positive strains were from colonizing samples. Surprisingly, in addition to amplifying in serotype III isolates (73%), it was detected in some Ia and Ib colonizing isolates. On the other hand, hvgA-positive infective isolates belonged only to serotype III.
Significant association was observed between the presence of virulence genes and the most prevalent serotypes, la and III. The bca and PI-2a genes were significantly associated with serotype Ia (OR 2.54, p < 0.05; OR 3.61, p < 0.05, respectively) compared to isolates of serotype III; and, rib, spb1, PI-1 and PI-2b were significantly associated with serotype III, compared to serotype Ia (OR 56, p < 0.05; OR 15.93, p < 0.05; OR 3.75, p < 0.05; OR 19, p < 0.05, respectively). The bac gene was not significantly associated with either serotype.
The cluster analysis taking into account the virulence genes showed 52 profiles, being 31 of them unique and the remaining 21 shared by 2 to 24 isolates. Each profile comprised 4 to 12 genes. The principal profile was bca-lmB-hylB-cylE-scpB-PI-2a-cpsA (n = 24, 15%), followed by bca-bac-lmb-hylB-cylE-scpB-PI2a-cpsA/bca-bac-lmb-hylB-cylE-scpB-PI-1-PI-2a-cpsA (n = 13, 8% each one), lmb-hylB-cylE-scpB-PI2a-cpsA (n = 12, 7%), and bca-lmb-hylB-cylE-scpB-PI-1-PI-2a-cpsA (n = 11, 7%). No one of these mentioned profiles could be associated with a particular serotype (Fig. 3).
Cluster analysis of GBS isolates from Argentina based on virulence-associated genes profiles. The presence (black) or absence (white) of genes, the isolate name, serotype, source, and isolation date of the isolates are shown. The antimicrobial resistance profiles are indicated on the right. The dendrogram was carried out by the UPGMA clustering method, and was generated using the BioNumerics v.6.6 software. NT non-typeable, CLI clindamycin, ERY erythromycin, LEV levofloxacin, ND no data, PEN penicillin, S susceptible to all tested antimicrobial agents, TET tetracycline
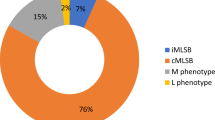
Antimicrobial Susceptibility
Regarding antimicrobial resistance (AMR), 93 isolates could be tested using a disc diffusion method. All analysed isolates were susceptible to penicillin. The resistance rates measured for clindamycin, erythromycin, norfloxacin, levofloxacin, and tetracycline were 14, 22, 41, 13, and 76% of the isolates, respectively (Table 2). No significant association was found between penicillin, clindamycin, erythromycin, norfloxacin, and levofloxacin resistances and colonizing or infective strains. On the contrary, tetracycline resistance was significantly associated with colonizing isolates (OR 4.5, p < 0.05). Norfloxacin resistance was present in all the serotypes, except in NT. Serotype Ia isolates presented mostly resistance to TET (30/36) and NOR (13/36); serotype III isolates, to TET (26/32), ERY (9/32) and CLI (7/32), and serotype Ib, to LEV (8/19), NOR (12/19), TET (11/19), ERY (3/19) and CLI (1/19). All isolates resistant to levofloxacin were resistant, also, to norfloxacin (N = 12).
Results showed 16 AMR profiles, some of them with resistance to up to 4 antibiotics and only four isolates were susceptible to 100% of the tested antibiotics. Among colonizing isolates, the profile TET-resistance (44%), followed by the profile NOR-TET-resistance (18%) predominated. Among the infective isolates, TET-resistance and LEV-NOR-resistance profiles (19% each one) predominated, followed by NOR-TET-resistance, CLY-ERY-TET- resistance, and NOR-resistance (13% each one) (Suppl. Mat. Table 3).
Detection of Antimicrobial Resistance Genes
In order to investigate genetic resistance mechanisms, all isolates (N = 162) were screened by PCR for some genes accounting for resistance to several antibiotics. In relation to erythromycin resistance, the ermB gene was detected in 27% of the total isolates (43/162) and in 80 and 77%, of ERY and CLI-resistant isolates (according to phenotypic analysis), respectively. The gene linB was not detected in clindamycin-resistant isolates. In relation to tetracycline resistance, the ribosomal protection genes tetM and tetO were detected in 51% (83/162) and in 9% (15/162) of the total isolates, respectively, and in the 96% and 13% among TET-resistant isolates (according to phenotypic analysis), respectively.
Discussion
GBS colonizes the lower genital tract of approximately 18% of women globally as an asymptomatic member, but established in other host niches, however, GBS is highly pathogenic [3]. Also, this pathogen is able to colonize mammary glands and cause bovine mastitis [25]. The present study characterizes circulating GBS isolates that predominate among colonized pregnant mothers as well as infective cases in a region of Argentina.
GBS is encased by a capsular polysaccharide, based on which ten serotypes are distinguished. Among the Argentinean GBS isolates studied, six serotypes (Ia, III, Ib, II, IV, and V) were detected. Serotypes Ia and III together comprised almost 70% of the total number of isolates. Only one colonizing isolate showed serotype IV. Our results are somewhat similar to a recent study carried out on strains from pregnant women of Misiones province but not in terms of the frequencies of each one of them. The authors detected serotype Ia (33%) as the most frequent one followed by III (19%), Ib (15%), II (14%), V (7%), and IX [4]. A previous study, also in strains from Misiones pregnant women, showed a serotype distribution of Ia (40%), III, V, II, Ib, and IX [26]. On the other hand, in Argentinean multi-center studies, serotypes Ia, III and Ib (85% of the total) were the most frequently recorded serotypes among GBS strains from urinary infections [27], meanwhile Ia and III followed by serotypes II and IV were recorded among strains from invasive diseases [28]. A recently published study [29], with emphasis on Argentinean invasive strains collected during 1 year (2014–2015), reported results concordant with ours in relation in that serotypes Ia and III were the most frequent ones in colonizing and invasive isolates recovered from neonates; in invasive isolates from adults, on the other hand, serotypes Ib and Ia prevailed.
A characteristic of GBS strains is that most of the genes associated with the virulence encode proteins necessary for bacteria-host-cell interaction in the process of pathogenicity [30]. In relation to the virulence genes screened in this study, all of them were detected in some percentage. All isolates possessed cpsA, hylB, and cylE, at least one variant or a combination of the two pili island and nearly all isolates possessed lmb, scpB. These would suggest that these factors are crucial for colonization in humans.
The GBS hyaluronate lyase (HylB) degrades hyaluronic acid, the main component of human connective tissue, facilitating bacterial spread and immunity evasion [31]. This gene and cylE were detected in 100% of the strains, both infective and colonizing ones. Haemolytic activity in GBS is produced by the gene products of the cyl operon, and cylE, which encodes an N-acyl transferase, is necessary for pigment production [32]. This β-haemolysin is, also, a pore-forming toxin, involved in tissue damage, balance the pro- and anti-inflammatory responses of the infected host and the systemic spread of bacteria [33, 34].
The major strategy that GBS employs to colonize the lower genital tract is adherence to epithelial cells via surface-associated adhesins. A common ability conferred by these adhesins is GBS binding to components of the extracellular matrix. The laminin-binding protein (Lmb) mediates the union to laminin, a major component of the basement membrane in human tissues [35]. The peptidase C5a, encoded by the gene scpB, interferes with the recruitment of leukocytes at infection sites and binds to fibronectin to promote bacterial invasion of epithelial cells [36].
GBS encodes pili encoded in islands-1 and -2, (PI-1 and PI-2, respectively), with PI-2 comprising 2 variants [37]. The most common pilus here detected was PI-2a, agreeing with results from other groups [38].
The hypervirulent GBS adhesin (HvgA) is a critical virulence trait of neonatal GBS-associated-disease and serotype III has been found to exhibit specific neurotropism through expression of it [39] Gene hvgA was mostly present but not restricted to serotype III. It was also detected in Ia and Ib serotypes meanwhile McGee et al. [40] detected it in serotype IV isolates.
No significant association was found between virulence genes and colonizing or infective strains but, on the other hand, significant association was observed between some virulence genes and the most prevalent serotypes, la and III. The bca and PI-2a genes were significantly associated with serotype Ia (compared to isolates of serotype III) meanwhile rib, spb1, PI-1, and PI-2b were significantly associated with serotype III. The gene bca encodes the α-C surface protein, which plays an important role in virulence when the bacterium joins the eukaryotic cell [41].
In order to have a global view of antimicrobial susceptibility occurrence, some isolates were tested against six antimicrobial agents. In Argentina, according to our results and previous information [27, 29, 42], GBS continues to be susceptible to penicillin. However, an important level of RAM for other antibiotics, in both colonizing and infective strains, was detected. Macrolide and lincosamide antibiotics are often used as an alternative in penicillin-allergic patients, and the emergence of resistance among GBS is an increasing problem in many parts of the world [8]. Recent reports on ERY and CLI susceptibility among isolates from infections in Argentina informed resistance rates between 17 and 24% and between 16 and 18%, respectively [29, 42]. In relation to resistance detected in colonizing isolates from Misiones, a recent publication revealed ERY and CLI-resistance rates of 6% and 5%, respectively [43]. Our results taking into account the total number of strains show similar average resistance rates (22 and 14%, respectively); considering only colonizing ones, our data are similar (18 and 12%, respectively) to those obtained from other geographical areas in South America [17, 44].
Resistance against macrolides and lincosamides among GBS may be occurring through two mechanisms, target site modification encoded by erm gene and through an active efflux pump [45]. In this study the ermB gene was detected in 80% of ERY-resistant isolates and, 77% of CLY-resistant isolates, explaining, at least partially, the resistance by a ribosome methylase which alter the binding of the antibiotic target site. The detection of linB (among other resistance determinants) in clindamycin-resistant isolates would explain the resistance observed to lincosamides, not explained by macrolides, however the linB gene was not detected in this study.
In relation to fluoroquinolones, an important therapeutic alternative, Arias et al. [29, 46] detected a LEV-resistance rate of approximately 15% in invasive GBS isolates. The authors discussed that the resistance percentage detected was higher than the latest reports from Argentina and the rest of the world, except Korea, China and Japan. In this study, the general percentage of resistance found was similar (13%).
No significant association was found between penicillin, clindamycin, erythromycin, norfloxacin, and levofloxacin resistances and colonizing or infective strains. On the contrary, tetracycline resistance was significantly associated with colonizing isolates. Resistance to tetracycline could be attributed, at least partially, to tetM and, tetO, genes encoded ribosome protection. High rates of tetracycline have been found previously in Argentinean infective GBS isolates [23], and rates even higher than those found by us have been detected for other geographical areas [47]. It is known that tetracycline resistance in GBS is ubiquitously high, and has been proposed that the acquisition of resistance genes tetO and tetM by a subset of GBS clones has led to their selection and expansion [48]. According to our data, those tetracycline resistant clones would have spread mainly among the colonizing strains.
GBS leads a double life as both an asymptomatic colonizer and a potent pathogen. Although most people who are colonized with GBS do not experience invasive disease, invasion of GBS into host niches outside of the gastrointestinal and/or vaginal mucosa causes severe damage to the host, resulting in severe outcomes, especially in new-borns [49]. Our findings show that both colonizing and infective isolates share similar features in terms of capsular serotype and virulence genes, suggesting that there are no a GBS subpopulation with a particular propensity to cause disease in adults. This research contributes to epidemiological surveillance in public health and provides data of interest about GBS strains circulating in Argentina. Data on serotypes and virulence genes, particularly those encoding surface proteins, can be useful to evaluate the effectiveness in the region of a GBS vaccine; data on antimicrobial resistance are necessary to evaluate which would be the best prophylactic/therapeutic option.
Conclusions
This is the first time that the virulence profiles of GBS colonizing and infective Argentinean strains have been investigated and compared. Genes cpsA, cylE, hylB, lmb, and scpB were the most prevalent and could be postulated as vaccine epitopes. Also, this work highlights the genetic diversity of GBS isolates circulating in the Pampean region of Argentina.
Penicillin-resistant GBS was not found, but resistance levels to tetracycline, fluoroquinolones, macrolides, and lincosamides were high. Our and worldwide reports on emerging multi-drug resistant GBS isolates reinforce the need for continued surveillance.
Data Availability
All data generated or analysed during this study are included in this published article (and its supplementary information file).
Code Availability
Not applicable.
References
Johri AK, Paoletti LC, Glaser P et al (2006) Group B Streptococcus: global incidence and vaccine development. Nat Rev Microbiol 4:932–942. https://doi.org/10.1038/nrmicro1552
Skoff TH, Farley MM, Petit S et al (2009) Increasing burden of invasive Group B Streptococcal disease in nonpregnant adults, 1990–2007. Clin Infect Dis 49:85–92. https://doi.org/10.1086/599369
Russell NJ, Seale AC, O’Driscoll M et al (2017) Maternal colonization with Group B Streptococcus and serotype distribution worldwide: systematic review and meta-analyses. Clin Infect Dis 65:S100–S111. https://doi.org/10.1093/cid/cix658
Bobadilla FJ, Novosak MG, Cortese IJ et al (2021) Prevalence, serotypes and virulence genes of Streptococcus agalactiae isolated from pregnant women with 35–37 weeks of gestation. BMC Infect Dis 21:73. https://doi.org/10.1186/s12879-020-05603-5
Raabe VN, Shane AL (2019) Group B Streptococcus: Streptococcus agalactiae. Microbiol Spectr. https://doi.org/10.1128/microbiolspec.gpp3-0007-2018
Kimura K, Suzuki S, Wachino JI et al (2008) First molecular characterization of group B streptococci with reduced penicillin susceptibility. Antimicrob Agents Chemother 52:2890–2897. https://doi.org/10.1128/AAC.00185-08
Nagano N, Nagano Y, Toyama M et al (2012) Nosocomial spread of multidrug-resistant group B Streptococci with reduced penicillin susceptibility belonging to clonal complex 1. J Antimicrob Chemother 67:849–856. https://doi.org/10.1093/jac/dkr546
Francois Watkins LK, McGee L, Schrag SJ et al (2019) Epidemiology of invasive Group B Streptococcal infections among nonpregnant adults in the United States, 2008–2016. JAMA Intern Med 179:479–488. https://doi.org/10.1001/jamainternmed.2018.7269
Lindahl G, Stålhammar-Carlemalm M, Areschoug T (2005) Surface proteins of Streptococcus agalactiae and related proteins in other bacterial pathogens. Clin Microbiol Rev 18:102–127
Brochet M, Couvé E, Zouine M et al (2006) Genomic diversity and evolution within the species Streptococcus agalactiae. Microbes Infect 8:1227–1243. https://doi.org/10.1016/j.micinf.2005.11.010
Slotved HC, Kong F, Lambertsen L et al (2007) Serotype IX, a proposed new Streptococcus agalactiae serotype. J Clin Microbiol 45:2929–2936. https://doi.org/10.1128/JCM.00117-07
Manning SD, Ki M, Marrs CF et al (2006) The frequency of genes encoding three putative group B streptococcal virulence factors among invasive and colonizing isolates. BMC Infect Dis. https://doi.org/10.1186/1471-2334-6-116
Lamy MC, Dramsi S, Billoët A et al (2006) Rapid detection of the “highly virulent” group B Streptococcus ST-17 clone. Microbes Infect 8:1714–1722. https://doi.org/10.1016/j.micinf.2006.02.008
Imperi M, Pataracchia M, Alfarone G et al (2010) A multiplex PCR assay for the direct identification of the capsular type (Ia to IX) of Streptococcus agalactiae. J Microbiol Methods 80:212–214. https://doi.org/10.1016/j.mimet.2009.11.010
Bidet P, Brahimi N, Chalas C, Aujard Y, Bingen E (2003) Molecular characterization of serotype III group B-streptococcus isolates causing neonatal meningitis. J Infect Dis 188(8):1132–1137. https://doi.org/10.1086/378517
Duarte RS, Bellei BC, Miranda OP et al (2005) Distribution of antimicrobial resistance and virulence-related genes among Brazilian group B Streptococci recovered from bovine and human sources. Antimicrob Agents Chemother 49:97–103. https://doi.org/10.1128/AAC.49.1.97-103.2005
Otaguiri ES, Belotto Morguette AE, Reis Tavares E et al (2013) Commensal Streptococcus agalactiae isolated from patients seen at University Hospital of Londrina, Paraná, Brazil: capsular types, genotyping, antimicrobial susceptibility and virulence determinants. BMC Microbiol 13:297. https://doi.org/10.1186/1471-2180-13-297
Smith TC, Roehl SA, Pillai P et al (2007) Distribution of novel and previously investigated virulence genes in colonizing and invasive isolates of Streptococcus agalactiae. Epidemiol Infect 135:1046–1054. https://doi.org/10.1017/S0950268806007515
Martins ER, Melo-Cristino J, Ramirez M (2010) Evidence for rare capsular switching in Streptococcus agalactiae. J Bacteriol 192:1361–1369. https://doi.org/10.1128/JB.01130-09
Clinical and Laboratory Standards Institute (CLSI) (2019) Performance standards for antimicrobial susceptibility testing, 29th edn. CLSI supplement M100, Wayne, PA
European Committee on Antimicrobial Susceptibility Testing - Committee of the Antibiogram of the French Society of Microbiology (2019) Breakpoint tables for interpretation of MICs and zone diameters version 9.0. CA-SFM Recommendations 2019
Zhou L, Yu SJ, Gao W et al (2011) Serotype distribution and antibiotic resistance of 140 pneumococcal isolates from pediatric patients with upper respiratory infections in Beijing, 2010. Vaccine 29:7704–7710. https://doi.org/10.1016/j.vaccine.2011.07.137
Lopardo HA, Vidal P, Jeric P et al (2003) Six-month multicenter study on invasive infections due to group B streptococci in Argentina. J Clin Microbio 41:4688–4694. https://doi.org/10.1128/JCM.41.10.4688-4694.2003
Bozdogan B, Berrezouga L, Kuo M-S et al (1999) A new resistance gene, linB, conferring resistance to lincosamides by nucleotidylation in Enterococcus faecium HM1025. Antimicrob Agents Chemother 43:925–929. https://doi.org/10.1128/AAC.43.4.925
Hernandez L, Bottini E, Cadona J et al (2021) Multidrug resistance and molecular characterization of Streptococcus agalactiae isolates from dairy cattle with mastitis. Front Cell Infect Microbiol 11:647324. https://doi.org/10.3389/fcimb.2021.647324
Oviedo P, Pegels E, Laczeski M et al (2013) Phenotypic and genotypic characterization of Streptococcus agalactiae in pregnant women. First study in a province of Argentina. Braz J Microbiol 44:253–258. https://doi.org/10.1590/S1517-83822013005000030
Vigliarolo L, Arias B, Suárez M et al (2019) Argentinian multicenter study on urinary tract infections due to Streptococcus agalactiae in adult patients. J Infect Dev Ctries 13:77–82. https://doi.org/10.3855/jidc.10203
Perez J, Limansky A, Toresani I et al (2004) Streptococcus agalactiae en Argentina Distribución de tipo capsular y sensibilidad antimicrobiana de Streptococcus agalactiae productores de infecciones en Argentina. Rev Argent Microbiol 36:63–67
Arias B, Kovacec V, Vigliarolo L et al (2022) Epidemiology of invasive infections caused by Streptococcus agalactiae in Argentina. Microb Drug Resist 28:322–329. https://doi.org/10.1089/mdr.2021.0071
Laczeski M, Novosak M, Giolito RC et al (2015) Study of serotypes, susceptibility to macrolide and virulence and resistance molecular profiles in invasive strains of Streptococcus agalactiae in two Argentine Provinces. Adv Microbiol 05:230–243. https://doi.org/10.4236/aim.2015.54021
Baker JR, Pritchard DG (2000) Action pattern and substrate specificity of the hyaluronan lyase from group B streptococci. Biochem J 348(Pt 2):465–471
Pritzlaff CA, Chang JCW, Kuo SP et al (2001) Genetic basis for the b-haemolytic/cytolytic activity of group B Streptococcus. Mol Microbiol 39:236–247. https://doi.org/10.1046/j.1365-2958.2001.02211.x
Reiss A, Braun JS, Jäger K et al (2011) Bacterial pore-forming cytolysins induce neuronal damage in a rat model of neonatal meningitis. J Infect Dis 203:393–400. https://doi.org/10.1093/infdis/jiq047
Randis TM, Gelber SE, Hooven TA et al (2014) Group B Streptococcus β-hemolysin/cytolysin breaches maternal-fetal barriers to cause preterm birth and intrauterine fetal demise in vivo. J Infect Dis 210:265–273. https://doi.org/10.1093/infdis/jiu067
Tenenbaum T, Spellerberg B, Adam R et al (2007) Streptococcus agalactiae invasion of human brain microvascular endothelial cells is promoted by the laminin-binding protein Lmb. Microbes Infect 9:714–720. https://doi.org/10.1016/j.micinf.2007.02.015
Beckmann C, Waggoner JD, Harris TO et al (2002) Identification of novel adhesins from group B streptococci by use of phage display reveals that C5a peptidase mediates fibronectin binding. Infect Immung 70:2869–2876. https://doi.org/10.1128/IAI.70.6.2869-2876.2002
Rosini R, Rinaudo CD, Soriani M et al (2006) Identification of novel genomic islands coding for antigenic pilus-like structures in Streptococcus agalactiae. Mol Microbiol 61:126–141. https://doi.org/10.1111/j.1365-2958.2006.05225.x
Martins ER, Andreu A, Melo-Cristino J, Ramirez M (2013) Distribution of pilus islands in Streptococcus agalactiae that cause human infections: Insights into evolution and implication for vaccine development. Clin Vaccine Immunol 20:313–316. https://doi.org/10.1128/CVI.00529-12
Tazi A, Disson O, Bellais S et al (2010) The surface protein HvgA mediates group B Streptococcus hypervirulence and meningeal tropism in neonates. J Exp Med 207:2313–2322. https://doi.org/10.1084/jem.20092594
McGee L, Chochua S, Li Z et al (2021) Multistate, population-based distributions of candidate vaccine targets, clonal complexes, and resistance features of invasive group B Streptococci within the United States, 2015–2017. Clin Infect Dis 72:1004–1013. https://doi.org/10.1093/cid/ciaa151
Baron MJ, Bolduc GR, Goldberg MB et al (2004) Alpha C protein of group B Streptococcus binds host cell surface glycosaminoglycan and enters cells by an actin-dependent mechanism. J Biol Chem 279:24714–24723. https://doi.org/10.1074/jbc.M402164200
Servicio de Antimicrobianos. INEI-ANLIS “Dr. Carlos G Malbrán" (2019) Resistencia a los Antimicrobianos en Aislamientos de Origen Comunitario, RED WHONET- Argentina 2019. http://antimicrobianos.com.ar/ATB/wp-content/uploads/2021/01/Datos-resistencia-comunitarios-2019-VF.pdf
Novosak M, Bobadilla F, Delgado O et al (2020) Phenotypic and genotypic characterization of resistance to macrolides and lincosamides in Streptococcus agalactiae isolated from pregnant women in Misiones, Argentina. Microb Drug Resist 26:1472–1481. https://doi.org/10.1089/mdr.2019.0328
Abarzúa CF, Arias EA, García CP et al (2011) Aumento de resistencia de Streptococcus agalactiae vaginal-anal en el tercer trimestre de gestación a eritromicina y clindamicina al cabo de una década de tamizaje universal. Rev Chilena Infectol 28:334–337. https://doi.org/10.4067/S0716-10182011000500005
Gygax SE, Schuyler JA, Kimmel LE et al (2006) Erythromycin and clindamycin resistance in group B streptococcal clinical isolates. Antimicrob Agents Chemother 50:1875–1877. https://doi.org/10.1128/AAC.50.5.1875-1877.2006
Arias B, Kovacec V, Vigliarolo L et al (2019) Fluoroquinolone-resistant Streptococcus agalactiae invasive isolates recovered in Argentina. Microb Drug Resist 25:739–743. https://doi.org/10.1089/mdr.2018.0246
Bergal A, Loucif L, Benouareth DE et al (2015) Molecular epidemiology and distribution of serotypes, genotypes, and antibiotic resistance genes of Streptococcus agalactiae clinical isolates from Guelma, Algeria and Marseille, France. Eur J Clin Microbiol Infect Dis 34:2339–2348. https://doi.org/10.1007/s10096-015-2487-6
Hayes K, O’Halloran F, Cotter L (2020) A review of antibiotic resistance in Group B Streptococcus: the story so far. Crit Rev Microbiol 46:253–269. https://doi.org/10.1080/1040841X.2020.1758626
Armistead B, Oler E, Adams Waldorf K, Rajagopal L (2019) The double life of Group B Streptococcus: asymptomatic colonizer and potent pathogen. J Mol Biol 431:2914–2931. https://doi.org/10.1016/j.jmb.2019.01.035
Acknowledgements
The authors sincerely thank all participating health centers, particularly members of hospitals and laboratories members who collaborated with this study. A special thanks to Cristina Monteavaro, Gladys Baz, Roxana Perez, and Rebecca Monterfano.
Funding
This work was supported by Grant from Agencia Nacional de Promoción Científica y Tecnológica (PICT 1139/17).
Author information
Authors and Affiliations
Contributions
LH: Formal analysis, Investigation, Methodology, Writing—Original Draft. JC: Formal analysis, Visualization. FT, SA: Resources, Investigation. AB: Conceptualization, Methodology, Investigation. MS: Conceptualization, Writing—Review & Editing, Supervision, Project administration, Management.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics Approval
The research was adjusted to the principles of Good Clinical Research Practices and adheres to the precepts established by the Declaration of Helsinki. The study followed the regulations stated in the Guide for Research in Human Health (Resolution 1480/11, Health Ministry of Presidency of the Argentine Nation, and Buenos Aires Province law No. 11,044 with its Regulatory Decree 3385/08 related to research on human beings). The data obtained were analysed anonymously, ensuring the patients’ confidentiality who were assigned an alphanumeric code. The confidentiality rules were respected according to Law 25326 (Protection of Personal Data) and articles 51 and 52 of the Civil and Commercial Code of the Argentine Nation.
Informed Consent
Not applicable.
Consent for Publication
Not applicable.
Something about Declaration of Deposition in Repositories
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hernandez, L.B., Cadona, J.S., Traverso, F. et al. Virulence Profiles and Antimicrobial Resistance of Streptococcus agalactiae Infective and Colonizing Strains from Argentina. Curr Microbiol 79, 392 (2022). https://doi.org/10.1007/s00284-022-03050-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00284-022-03050-w