Abstract
Purpose
This drug-interaction study evaluated the effect of omeprazole, a proton-pump inhibitor, on ibrutinib’s pharmacokinetics (PK) in healthy participants.
Methods
This open-label, sequential-design study included 20 healthy adults aged 18–55 years. Ibrutinib (560 mg, single dose) was administered after an overnight fast alone on day 1 and with omeprazole on day 7. Omeprazole (40 mg) alone was administered on days 3–6, 1 h before breakfast; and after an overnight fast on day 7, followed by ibrutinib 2 h later. Blood was sampled on days 1 and 7 for up to 48 h postdose, and the standard PK parameters for ibrutinib and PCI-45227 were summarized using descriptive statistics. The effect of omeprazole on ibrutinib’s PK was determined by assessing geometric mean ratios (GMRs) and 90% CIs. Mechanistic modeling was performed using the BTK-receptor occupancy (RO) model.
Results
AUC48h and AUClast of ibrutinib plus omeprazole versus ibrutinib alone showed a modest decrease (GMR [90% CI] 98.3% [83.1–116.3] and 92.5% [77.8–109.9], respectively); Cmax decreased by 62.5% (GMR [90% CI] 37.5% [26.4–53.4]), with delayed tmax (1−2 h) and terminal half-life unaffected. Mean AUC for PCI-45227 (primary metabolite) was ~ 20% lower with ibrutinib plus omeprazole versus ibrutinib alone. Model predictions showed no impact of decreased Cmax on BTK target engagement. No new safety signals were identified with the use of ibrutinib in this study.
Conclusions
The decrease in Cmax without a corresponding decrease in AUC by omeprazole was not clinically relevant for ibrutinib’s bioavailability. No dose adjustments are recommended during ibrutinib’s co-administration with omeprazole or other pH-altering agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
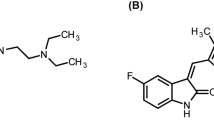
Ibrutinib (Imbruvica®) is a first-in-class, orally-administered, potent, selective and covalently binding Bruton’s tyrosine kinase (BTK) inhibitor [1, 2]. Ibrutinib covalently binds to BTK, which impairs B-cell antigen receptor signaling, the pivotal tumorigenesis pathway in most B-cell malignancies, and disrupts the proliferation and survival of malignant B-cells. Ibrutinib is currently approved in the United States, European Union, and > 80 other countries as a single agent or as part of a combination therapy for treatment-naïve or previously treated patients with chronic lymphocytic leukemia/small lymphocytic lymphoma (including patients with 17p deletion) [3,4,5], and as a single agent for previously treated patients with mantle cell lymphoma [6] and Waldenström’s macroglobulinemia [7]. Furthermore, in the US, ibrutinib has been approved for the treatment of patients with marginal zone lymphoma who require systemic therapy and have received at least one prior anti-CD20-based therapy [8], and most recently for the treatment of chronic graft-versus-host disease after failure of one or more treatments [9].
Considering daily oral administration of ibrutinib, it is critical to optimize its antitumor activity, and it is important to evaluate the factors that may impact its absorption and bioavailability, especially the steady-state exposure that modulates the efficacy in long-term treatments. Ibrutinib is a Biopharmaceutical Classification System Class 2 compound, displaying high permeability and poor solubility at physiological pH (insoluble at pH ≥ 3). It is rapidly absorbed following oral administration, and peak plasma concentrations are achieved within 1–2 h postdose [9]. The primary metabolite of ibrutinib, PCI-45227, has an inhibitory activity ~ 15 times lower than that of ibrutinib [10]. Gastric pH-altering agents, particularly long-acting ones such as proton-pump inhibitors (PPIs), may have the potential to impact the pharmacokinetics (PK) of weak bases such as ibrutinib, which show decreasing solubility at higher pH, potentially affecting its bioavailability and efficacy [10,11,12]. Physiologically-based PK modeling and simulation studies suggested that the dissolution step does not impact the bioavailability of ibrutinib [13], which was corroborated by comparing ibrutinib solution and capsule formulations (data on file). Population PK analysis suggested a delayed absorption of ibrutinib when co-administered with antacids without an impact on its exposure [14]. However, a clinical interaction study with pH-altering agents has not been performed. Since gastric pH-altering agents are commonly prescribed as well as taken as over-the-counter medications in North America and Western Europe [15], it is important to study this pH-dependent drug–drug interaction (DDI) to ascertain if PPIs can be used concurrently with weak-base drugs [16]. The present phase 1 clinical study was conducted to evaluate the potential effect of repeated dosing of omeprazole on the single-dose PK of ibrutinib in healthy adults.
Materials and methods
Study population
Healthy adults aged ≥ 18 to ≤ 55 years with a body mass index (BMI) of ≥ 18 to ≤ 30 kg/m2 and a body weight of not < 50 kg were included in the study. Key exclusion criteria were clinically significant history of (or current) cardiac, renal, hepatic, hematologic, pulmonary, neurologic, or psychiatric diseases; diabetes mellitus; infection; coagulation disorders; known hypersensitivity or intolerance to sulfonamide or beta-lactam antibiotics; known allergy to the study drugs; or other clinically significant abnormal laboratory values, physical examination findings, vital signs, or electrocardiogram (ECG) abnormalities. In addition, participants taking any prescription or non-prescription medication (including vitamins and herbal supplements), except for paracetamol and hormonal replacement therapy, within 14 days before the first dose of the study drug until completion of the study were excluded. Women had to be postmenopausal or surgically sterile.
Study design and settings
This was an open-label, sequential-design, DDI study conducted at a single study center in Belgium from February 2016 to March 2016. The study included a 21-day screening period, a 9-day open-label treatment period, and a 10-day follow-up period.
Ibrutinib 560 mg was administered as a single dose following an overnight fast on day 1. Omeprazole 40 mg was administered 1 h before breakfast on day 3 through day 6, to ensure steady-state concentrations of omeprazole when ibrutinib was administered on day 7. Participants were permitted to leave the clinic after 48 h sample collection for the PK analysis on day 2, and returned each morning on day 3 through day 6 to receive a single dose of omeprazole. Participants were readmitted on the evening of day 6. Following an overnight fast on day 7, omeprazole was administered 2 h before ibrutinib 560 mg to achieve the maximum possible impact of co-administering omeprazole. On days 1 and 7, water was allowed ad libitum beginning 2 h after administering ibrutinib, and lunch was served 4 h postdose. Participants were not allowed to consume food or beverages containing alcohol, grapefruit juice, Seville oranges, quinine, methylxanthine, poppy seeds, and nicotine; excessive use of caffeine was prohibited.
Participants were discharged after the final 48 h sample collection for the PK analysis on day 9. A follow-up visit was made approximately 10 (± 2) days after the last dose to perform safety evaluations.
Pharmacokinetic assessments
Plasma concentrations of ibrutinib, PCI-45227, and omeprazole were measured using validated liquid chromatography with tandem mass spectrometry methods. Serial blood samples for the PK analysis were collected before each ibrutinib dose, and up to 48 h (0, 0.25, 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, 16, 24, and 48 h) following dosing on days 1 and 7, and standard PK parameters for ibrutinib and PCI-45227 were calculated. Blood samples for PK analysis of omeprazole were collected on day 7 predose (before omeprazole administration), and 2 h postdose. The quantification range was 0.5–100 ng/mL for ibrutinib/PCI-45227, and 1–1000 ng/mL for omeprazole. Details of the quantification of ibrutinib/PCI-45277 have been described previously [17].
Pharmacokinetic analysis was performed using the validated computer program Phoenix™ WinNonlin® (version 6.2.1), and a non-compartmental analysis model was used. The primary PK parameters of interest were the maximum plasma concentration (Cmax) and area under the curve (AUC) of ibrutinib, which included the AUC from 0 to 48 h (AUC48h), and from 0 to the time of the last quantifiable concentration (AUClast). Truncated AUC from 0 to 24 h (AUC24h) was calculated post hoc, since concentrations at 48 h were BQL in 30% of the profiles. Other PK parameters included time to reach Cmax (tmax), metabolite-to-parent ratio (Cmax and AUCs), and the terminal elimination half-life (t1/2term). In addition, the potential impact on the efficacy of ibrutinib with continuous use of pH-increasing agents was evaluated indirectly by simulating the effect of ibrutinib when given with omeprazole on BTK engagement derived from a covalent-binding model of ibrutinib.
BTK-receptor occupancy model
A mechanistic model-based approach was followed using covalent target-binding kinetics to test the effect of the shape of ibrutinib concentration–time profiles with and without omeprazole on BTK-receptor occupancy (RO). The model was built on available covalent binding kinetics (association [kon], dissociation [koff], and covalent binding rate [kinact]) of ibrutinib to its target [BTK] in combination with BTK disposition kinetics. The BTK RO time profile was predicted based on in vitro covalent binding model parameters, PK concentration–time curves after ibrutinib administration with/without omeprazole, and a BTK half-life (turn-over rate) of 24 h. All model parameters are listed in Table S1, Supplementary Appendix.
PK profiles mimicking those observed for ibrutinib in the absence and presence of omeprazole were created using Monolix–R2016R1, Lixoft S.A.S (Paris, France). The PK parameters used to describe the profiles for ibrutinib with and without omeprazole (listed in Table S1, Supplementary Appendix) were fitted to the observed average plasma concentration (Fig. S1, Supplementary Appendix).
BTK-binding simulations were performed using Berkeley Madonna V8.3.18, CA, USA, using the covalent binding model and accompanying equations (Fig. S2, Supplementary Appendix).
The model’s robustness for comparing the treatment with and without omeprazole was tested using local sensitivity analysis of the parameters kinact, kon and the BTK half-life by assuming a tenfold up or down variation from the nominal value for kinact and kon and a threefold up or down variation for the BTK half-life. Factors for rate constants were arbitrarily chosen, while the factor 3 for half-life was based on the reported range of half-lives [18, 19]. The percent change in the average RO when using the nominal values with respect to upper or lower bounds were calculated for each parameter and for both treatments.
Safety assessments
Safety was evaluated throughout the study in terms of the incidence and type of treatment-emergent adverse events (TEAEs), and notable changes in clinical laboratory parameters, physical examination results, 12-lead ECGs, and vital sign measurements. TEAEs were coded in accordance with the Medical Dictionary for Regulatory Activities (MedDRA) version 18.1 by system organ class, and preferred term. Toxicity grading for TEAE and laboratory safety was performed in accordance with the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE Version 4.03).
Statistical methods
The sample size for the study was based on a previous study [20], where the intrasubject coefficients of variation were approximately 27 and 43% for the AUC and the Cmax of ibrutinib, respectively. Based on this, a sample size of 18 participants was considered sufficient for the point estimates of the geometric mean ratios (GMRs) of the AUC and Cmax of ibrutinib, with and without co-administration of omeprazole, falling within 86, 116, 79, and 127% of the true value of the AUC and Cmax, respectively, with 90% confidence. Assuming a 10% dropout rate, 20 participants were enrolled in the study to ensure that a minimum of 18 participants would complete the study.
The safety set included all the participants who received at least one dose of the study drug. Safety data were summarized using descriptive statistics.
The PK set included all the participants who had PK estimations of ibrutinib for both periods (ibrutinib administered alone on day 1 and in combination with omeprazole on day 7). The PK data were summarized descriptively. The effect of omeprazole on primary PK parameters of ibrutinib (Cmax and AUCs) was determined by assessing GMRs and 90% confidence intervals (CIs). The GMRs of PK parameters of ibrutinib with and without co-administration of omeprazole and the associated 90% CIs and intrasubject coefficients of variation from a mixed effects model of log-transformed PK parameters were constructed. No statistical comparisons were made for PCI-45227. Individual and mean plasma ibrutinib and PCI-45227 concentration–time profiles were plotted for each treatment. Statistical analyses were performed using SAS Version 9.3.
Results
A total of 20 participants (19 men and 1 woman; all white) received the study medication, and all of them completed the study without any protocol violation. The median age of the participants was 48 years (range 36–55 years, inclusive), and the mean (standard deviation) BMI was 25.47 (2.61) kg/m2.
Pharmacokinetics of ibrutinib
Co-administration of omeprazole reduced ibrutinib concentrations during the first 4 h compared with ibrutinib alone. Between 12 and 24 h postdose, ibrutinib concentrations were slightly higher when co-administered with omeprazole (Figs. 1a and S3, Supplementary Appendix) and the median tmax was delayed by 1 h. However, there was no apparent effect on the elimination phase of ibrutinib.
a Concentration–time curves of ibrutinib after administration of a single oral dose of ibrutinib 560 mg alone (day 1) and in combination with omeprazole 40 mg once daily (day 7). b Concentration–time curves of PCI-45227 after administration of a single oral dose of ibrutinib 560 mg alone (day 1) and in combination with omeprazole 40 mg once daily (day 7)
Repeated administration of omeprazole 40 mg (once daily) minimally affected the AUC48h and AUClast of ibrutinib after a single 560 mg dose with < 10% decrease based on GMR (98.3 and 92.5%, respectively), decreased ibrutinib mean Cmax (62.5% reduction based on GMRs) (Fig. 2). The 90% CI of the GMR of AUC48h fell within the (80–125%) interval (Table 1). The 48 h postdose concentration for ibrutinib was below the quantification limit (BQL) in six participants who received ibrutinib alone and eight participants who received ibrutinib with omeprazole. Furthermore, the truncated AUC calculations showed that GMR of AUC24h was 17% lower during initial 24 h when ibrutinib was co-administered with omeprazole (versus ibrutinib alone) compared to 1.7 and 7.5% lower AUC in the case of AUClast and AUC48h, respectively. The intrasubject variability on Cmax was 71.9%, and that on the AUC48h and AUClast was 31.5 and 32.3%, respectively.
Pharmacokinetics of PCI-45227
During the first 8 h, a reduction in the mean plasma concentrations of PCI-45227 was observed when ibrutinib was co-administered with omeprazole versus ibrutinib alone; however, the mean plasma concentrations were comparable thereafter (Fig. 1b). The mean AUC of PCI-45227 was 16% lower when ibrutinib was co-administered with omeprazole than when administered alone. The reduction in Cmax (50%) and the delay in tmax (1.5 h) caused by omeprazole for the metabolite were generally similar to those measured for ibrutinib. Co-administering omeprazole had a minimal effect on the ibrutinib metabolite-to-parent ratio (Table 2).
Pharmacokinetics of omeprazole
The average omeprazole plasma concentration at 2 h postdose was 554 ng/mL, with individual plasma concentrations ranging between BQL and 2310 ng/mL. In three participants, the 2 h postdose sample was reported as BQL (< 1.0 ng/mL). For these three participants, the individual treatment ratios of AUC or Cmax (ibrutinib co-administered with omeprazole versus ibrutinib alone) did not significantly differ from the other participants, with some showing a low treatment effect in conjunction with high omeprazole concentrations at the 2 h time point, while other participants had low omeprazole levels with a high treatment effect.
BTK-receptor occupancy model predictions
The PK model provided a good fit to the observed data for ibrutinib alone and in combination with omeprazole (Fig. S1, Supplementary Appendix). The corresponding predicted BTK binding versus the time profile at steady state for the ibrutinib 560 mg daily dose in the absence and presence of omeprazole is shown in Fig. 3. As per model predictions, the difference in average target occupancy was negligible with RO values of 0.96 (96%) and 0.94 (94%) with and without omeprazole, respectively. The RO remained above 90% during the 24 h treatment interval for both treatments. Thus, the lower ibrutinib Cmax observed with omeprazole does not seem to impact BTK target engagement. The sensitivity analysis confirmed that the impact of changing kinact, BTK half-life and kon parameters used in this model was minimal, and consistent for both treatments, with or without omeprazole (Fig. S4, Supplementary Appendix).
Safety
Overall, nine (45%) participants experienced at least one TEAE, of which six (30%) participants had TEAEs that were considered by the investigator to be related to study drug. The number of participants with TEAEs after administration of ibrutinib alone and when co-administered with omeprazole was the same (five in each group). The most commonly reported TEAEs during this period were back pain, headache, abdominal pain, and diarrhoea, which were all grade 1 in severity (Table 3). During the follow-up period, one participant experienced a grade 2 TEAE (prostatitis), however, this was considered by the investigator as not related to study drug. No clinically significant changes in laboratory safety parameters, ECG, or vital signs over time were observed in this study. No serious adverse events (SAEs) were reported, and there were no discontinuations due to adverse events (AEs).
Discussion
The present study evaluated the potential effects of repeated omeprazole dosing on single-dose PK of ibrutinib in healthy adults. Repeated administration of omeprazole with ibrutinib minimally affected the AUC of ibrutinib (≤ 10% based on the GMR for AUC48h, and AUClast) despite a 63% reduction in Cmax. The median tmax increased from 1 to 2 h when omeprazole was co-administered with ibrutinib, with increases in systemic concentrations observed as late as 24 h after ibrutinib intake. The effects of omeprazole on PCI-45227 PK parameters were generally consistent with those observed with the parent ibrutinib, with a twofold decrease in Cmax but a small change in AUC. In line with this, co-administering ibrutinib with omeprazole resulted in comparable metabolite-to-parent ratios of PCI-45227 for both treatments.
These findings are pertinent as co-administering ibrutinib with omeprazole delayed the gastrointestinal absorption but did not have an impact on ibrutinib exposure as evaluated by its AUC, which is deemed most relevant for ibrutinib’s clinical activity. Since the gastric pH-lowering effect with PPIs is more pronounced and lasts longer compared to other gastric pH-lowering agents, the impact of using H2-antagonists (e.g., ranitidine) or antacids on ibrutinib exposure can also be considered clinically irrelevant. In general, omeprazole tmax occurs approximately 1–2 h following dosing [21]. However, in this study, omeprazole plasma concentrations, determined at 2-h postdose only, varied from BQL to > 2 µg/mL.
Despite this, the majority of the participants showed a clear decrease in ibrutinib Cmax, implying that low omeprazole levels at the 2-h timepoint resulted from a delayed tmax, rather than low exposure. Support for this explanation was obtained from a retrospective evaluation of similar DDI studies conducted with other compounds, in which omeprazole PK profiles were obtained (data on file). In addition, a sustained effect of omeprazole on gastric pH was observed regardless of its short half-life, suggesting that this effect is dependent on the total AUC of the drug and not on its plasma concentration at any timepoint [22, 23].
Half-life of ibrutinib in this study ranged between 11 and 15 h, higher than the reported t1/2 of 4–6 h [9]. The PK profile of ibrutinib showed a temporary increase in concentration at the 24-h timepoint, suggesting deviation from normal linear elimination profile that was observed in other studies involving non-fasted conditions. This deviation prevented accurate determination of the terminal half-life, resulting in apparently longer t1/2 values. Furthermore, the correlation coefficient of the terminal slope failed to meet the criteria for the estimation of t1/2 (coefficient of determination r2 < 0.9, or < 3 data points could be used in the calculation) for many profiles, thus preventing its extrapolation to infinity. These profiles were excluded from the summary statistics.
Based on ibrutinib’s pharmacology and mechanism of action with covalent binding, the effect of a lower Cmax was predicted to be minimal. To confirm this assumption, a mechanistic BTK RO model was developed based on covalent target-binding kinetics, and demonstrated that the lower Cmax of ibrutinib as a result of omeprazole co-administration does not impact the extent and duration of BTK target engagement in a clinically relevant manner. A similar approach has been used by Jusko who proposed a mathematical basis for the observation that cyclophosphamide, which acts through irreversible binding, showed similar efficacy in mouse models after fractionated dosing and after a single injection [24]. When several reversibly binding ligands compete for the same binding site on the BTK target, a higher concentration (in combination with the on/off rate) is of critical importance. However, with a covalently binding ligand such as ibrutinib, in combination with its sub-nanomolar affinity for the target [0.39 nM (0.17 ng/mL)], binding can occur quickly and thereafter displacement by a ligand present at a higher concentration is not possible. The covalent ligand remains bound to the target, with the duration of response dependent on the turn-over rate of the enzyme (24 h for BTK). The model predicted high target engagement (RO > 90%) which lasted over 24 h, consistent with the exposure–RO relationship observed in patients (data on file).
The treatment regimen used in this study represents a worst-case scenario where patients receive multiple doses of PPIs over time, thereby causing a continuously elevated gastric pH. This treatment regimen did not impact the relative bioavailability of ibrutinib. A similar observation was made in a study with ponatinib, another Biopharmaceutics Classification System Class 2 tyrosine kinase inhibitor, where co-administering lansoprazole resulted in more modest, though statistically significant, reduction in the Cmax of ponatinib (25% reduction), but only a small change in the AUC [25]. However, the majority of kinase inhibitors, indeed, showed a decreased bioavailability when combined with a PPI, e.g., AUCs of dasatinib [26], erlotinib [27] and nilotinib [28] in healthy volunteers, lapatinib in women with breast cancer [29], and pazopanib in patients with solid tumors [30], were decreased by 60, 33, 34, 26, and 40%, respectively [31]. Physiologically-based PK (PBPK) modeling techniques may be used to simulate the effect of pH-altering agents on bioavailability, but due to the critical balance between dissolution, GI transport, and intestinal absorption, success has been limited. Recently, Lu et al. were able to reconcile the negative effect of PPI co-administration on the AUC of pictilisib using PBPK modeling by fine-tuning gastric emptying and motility parameters using clinical observations [32]. The extent of the decrease in AUC of these oral anticancer drugs in combination with gastric pH-altering agents is much higher than those observed in the current study. However, in most cases, these decreases were not deemed clinically relevant. Taken together, the considerable range of observations substantiates the finding that for BCS Class 2 compounds, although gastric pH may affect their dissolution, their ultimate bioavailability is determined by the drug’s intestinal permeability. For ibrutinib, complete absorption, albeit delayed, still seems to take place in these unfavorable conditions.
This study evaluated the PK of ibrutinib under fasting conditions; however, the effect of omeprazole on ibrutinib Cmax is expected to be less pronounced under fed conditions, since food intake increases ibrutinib Cmax by up to fourfold, and AUC by approximately twofold [18, 33]. Ibrutinib can be taken regardless of food intake, and repeated intake under formal fasted conditions (no food intake from 10 h prior until 4 h after drug intake) is unlikely. Population PK analysis showed that the AUC under typical clinical trial conditions (no food intake from 2 h prior to 30 min after ibrutinib administration) did not differ from the AUC in fed condition, i.e., ibrutinib administration with a high-fat breakfast. In addition, the population PK analysis [14] demonstrated that relative bioavailability of ibrutinib was not affected by co-administration of gastric pH-lowering agents, mainly PPIs. It should be noted that the conditions of this pharmacokinetic study were chosen to obtain the maximal effect. Finally, a subgroup analysis using data from four randomized trials, stratified for concomitant use of PPIs or H2 antagonists for at least 2 months, found no detrimental impact on ibrutinib efficacy in participants taking pH-altering agents chronically.
In line with the parent drug, the primary metabolite PCI-45227, which is considered to be inactive as it binds reversibly to BTK with 1/15th of ibrutinib’s affinity [9, 10], closely followed the PK of ibrutinib in the presence of omeprazole, i.e., a large decrease in the Cmax and a small change in the AUC.
The safety profile after single doses of ibrutinib 560 mg either alone or in combination with omeprazole was consistent with earlier studies, with no new safety signals identified in this study. There were no clinically significant observations on hematology, serum chemistry, physical examination, vital signs, and ECGs.
The findings of this study should be interpreted in the context of some limitations. There was a gender imbalance, which, however, did not hamper interpretation, since each subject served as its own control. In addition, it may be noted that there are no indications of gender-specific differences in clearance of ibrutinib or omeprazole [21, 33]. Finally, variability on Cmax was higher than expected, based on prior data.
In conclusion, results of this study in combination with mechanistic modeling of target-binding indicated that the observed decrease in ibrutinib Cmax caused by repeated omeprazole co-administration, without a corresponding decrease in AUC, is not clinically relevant for ibrutinib’s bioavailability. Thus, dose adjustments are not recommended during ibrutinib’s co-administration with omeprazole or other pH-altering agents.
References
de Claro RA, McGinn KM, Verdun N, Lee S-L, Chiu H-J, Saber H, Brower ME, Chang CG, Pfuma E, Habtemariam B (2015) FDA approval: ibrutinib for patients with previously treated mantle cell lymphoma and previously treated chronic lymphocytic leukemia. Clin Cancer Res 21(16):3586–3590
Roskoski R Jr (2016) Ibrutinib inhibition of Bruton protein-tyrosine kinase (BTK) in the treatment of B cell neoplasms. Pharmacol Res 113:395–408
Burger JA, Tedeschi A, Barr PM, Robak T, Owen C, Ghia P, Bairey O, Hillmen P, Bartlett NL, Li J (2015) Ibrutinib as initial therapy for patients with chronic lymphocytic leukemia. N Engl J Med 373(25):2425–2437
Byrd J, Brown J, O’Brien S, Barrientos J, Kay N, Reddy N, Coutre S, Tam C, Mulligan S, Jaeger U, Investigators R (2014) Ibrutinib versus ofatumumab in previously treated chronic lymphoid leukemia. N Engl J Med 371(3):213–223
Chanan-Khan A, Cramer P, Demirkan F, Fraser G, Silva RS, Grosicki S, Pristupa A, Janssens A, Mayer J, Bartlett NL (2016) Ibrutinib combined with bendamustine and rituximab compared with placebo, bendamustine, and rituximab for previously treated chronic lymphocytic leukaemia or small lymphocytic lymphoma (HELIOS): a randomised, double-blind, phase 3 study. Lancet Oncol 17(2):200–211
Dreyling M, Jurczak W, Jerkeman M, Silva RS, Rusconi C, Trneny M, Offner F, Caballero D, Joao C, Witzens-Harig M (2016) Ibrutinib versus temsirolimus in patients with relapsed or refractory mantle-cell lymphoma: an international, randomised, open-label, phase 3 study. Lancet 387(10020):770–778
Dimopoulos MA, Trotman J, Tedeschi A, Matous JV, Macdonald D, Tam C, Tournilhac O, Ma S, Oriol A, Heffner LT (2017) Ibrutinib for patients with rituximab-refractory Waldenström’s macroglobulinaemia (iNNOVATE): an open-label substudy of an international, multicentre, phase 3 trial. Lancet Oncol 18(2):241–250
Noy A, De Vos S, Thieblemont C, Martin P, Flowers CR, Morschhauser F, Collins GP, Ma S, Coleman M, Peles S (2017) Targeting Bruton tyrosine kinase with ibrutinib in relapsed/refractory marginal zone lymphoma. Blood 129(16):2224–2232
Imbruvica® Prescribing Information. https://www.janssenmd.com/pdf/imbruvica/imbruvica_pi.pdf. Accessed 04 Dec 2017
Parmar S, Patel K, Pinilla-Ibarz J (2014) Ibrutinib (imbruvica): a novel targeted therapy for chronic lymphocytic leukemia. Pharm Ther 39(7):483
Budha N, Frymoyer A, Smelick G, Jin J, Yago M, Dresser M, Holden S, Benet L, Ware J (2012) Drug absorption interactions between oral targeted anticancer agents and PPIs: is pH-dependent solubility the achilles heel of targeted therapy? Clin Pharmacol Ther 92(2):203–213
Howden CW (1991) Clinical pharmacology of omeprazole. Clin Pharmacokinet 20(1):38–49
de Zwart L, Snoeys J, De Jong J, Sukbuntherng J, Mannaert E, Monshouwer M (2016) Ibrutinib dosing strategies based on interaction potential of CYP3A4 perpetrators using physiologically based pharmacokinetic modeling. Clin Pharmacol Ther 100(5):548–557
Marostica E, Sukbuntherng J, Loury D, de Jong J, Woot de Trixhe X, Vermeulen A, De Nicolao G, O’Brien S, Byrd JC, Advani R (2015) Population pharmacokinetic model of ibrutinib, a Bruton tyrosine kinase inhibitor, in patients with B cell malignancies. Cancer Chemother Pharmacol 75(1):111–121
Smelick GS, Heffron TP, Chu L, Dean B, West DA, DuVall SL, Lum BL, Budha N, Holden SN, Benet LZ (2013) Prevalence of acid-reducing agents (ARA) in cancer populations and ARA drug–drug interaction potential for molecular targeted agents in clinical development. Mol Pharm 10(11):4055–4062
Zhang L, Wu F, Lee S, Zhao H (2014) pH-dependent drug–drug interactions for weak base drugs: potential implications for new drug development. Clin Pharmacol Ther 96(2):266–277
de Vries R, Huang M, Bode N, Jejurkar P, de Jong J, Sukbuntherng J, Sips L, Weng N, Timmerman P, Verhaeghe T (2015) Bioanalysis of ibrutinib and its active metabolite in human plasma: selectivity issue, impact assessment and resolution. Bioanalysis 7(20):2713–2724
Evans EK, Tester R, Aslanian S, Karp R, Sheets M, Labenski MT, Witowski SR, Lounsbury H, Chaturvedi P, Mazdiyasni H, Zhu Z (2013) Inhibition of Btk with CC-292 provides early pharmacodynamic assessment of activity in mice and humans. J Pharmacol Exp Ther 346(2):219–228
Hutchinson CV, Dyer MJ (2014) Breaking good: the inexorable rise of BTK inhibitors in the treatment of chronic lymphocytic leukaemia. Br J Haematol 166(1):12–22
De Jong J, Sukbuntherng J, Skee D, Murphy J, O’Brien S, Byrd JC, James D, Hellemans P, Loury DJ, Jiao J (2015) The effect of food on the pharmacokinetics of oral ibrutinib in healthy participants and patients with chronic lymphocytic leukemia. Cancer Chemother Pharmacol 75(5):907–916
Omeprazole Summary of Product Characteristics. https://www.medicines.org.uk/emc/medicine/24226. Accessed 17 May 2017
Prilosec® Prescribing Information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/019810s096lbl.pdf. Accessed 5 May 2018
Cederberg C, Andersson T, Skånberg I (1989) Omeprazole: pharmacokinetics and metabolism in man. Scand J Gastroenterol 24(Suppl 166):33–40
Jusko WJ (1971) Pharmacodynamics of chemotherapeutic effects: dose-time-response relationships for phase-nonspecific agents. J Pharm Sci 60(6):892–895
Narasimhan NI, Dorer DJ, Davis J, Turner CD, Sonnichsen D (2014) Evaluation of the effect of multiple doses of lansoprazole on the pharmacokinetics and safety of ponatinib in healthy subjects. Clin Drug Invest 34(10):723–729
Eley T, Luo FR, Agrawal S, Sanil A, Manning J, Li T, Blackwood-Chirchir A, Bertz R (2009) Phase I study of the effect of gastric acid pH modulators on the bioavailability of oral dasatinib in healthy subjects. J Clin Pharmacol 49(6):700–709
Kletzl H, Giraudon M, Ducray PS, Abt M, Hamilton M, Lum BL (2015) Effect of gastric pH on erlotinib pharmacokinetics in healthy individuals: omeprazole and ranitidine. Anti-Cancer Drugs 26(5):565–572
Yin OQ, Gallagher N, Fischer D, Demirhan E, Zhou W, Golor G, Schran H (2010) Effect of the proton pump inhibitor esomeprazole on the oral absorption and pharmacokinetics of nilotinib. J Clin Pharmacol 50(8):960–967
Koch KM, Im YH, Kim SB, Urruticoechea Ribate A, Stephenson J, Botbyl J, Cartee L, Holshouser J, Ridgway D (2013) Effects of esomeprazole on the pharmacokinetics of lapatinib in breast cancer patients. Clin Pharmacol Drug Dev 2(4):336–341
Tan AR, Gibbon DG, Stein MN, Lindquist D, Edenfield JW, Martin JC, Gregory C, Suttle AB, Tada H, Botbyl J (2013) Effects of ketoconazole and esomeprazole on the pharmacokinetics of pazopanib in patients with solid tumors. Cancer Chemother Pharmacol 71(6):1635–1643
Yu G, Zheng Q-S, Wang D-X, Zhou H-H, Li G-F (2014) Drug interactions between tyrosine-kinase inhibitors and acid suppressive agents: more than meets the eye. Lancet Oncol 15(11):e469-e470
Lu T, Fraczkiewicz G, Salphati L, Budha N, Dalziel G, Smelick GS, Morrissey KM, Davis JD, Jin JY, Ware JA (2017) Combining “bottom-up” and “top-down” approaches to assess the impact of food and gastric pH on pictilisib (GDC-0941) pharmacokinetics. CPT: Pharm Syst Pharmacol. https://doi.org/10.1002/psp4.12228
Imbruvica (2018) Summary of product characteristics EU. https://www.medicines.org.uk/emc/product/3414/smpc/. Accessed 03 Apr 2018
Acknowledgements
The authors thank the volunteers for their participation in this study and acknowledge the collaboration and commitment of the study staff; Payal Bhardwaj, Ph.D., and Ashwini Patil, M.S., ISMPP CMPP™ (Tata Consultancy Services, India) for medical writing assistance, and Namit Ghildyal, Ph.D. (Janssen Research & Development, LLC.) for additional editorial support.
Funding
The study was funded by Janssen Research & Development, LLC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
de Jong, Haddish-Berhane, Hellemans, Jiao, and Ouellet are employees of Janssen Research & Development and hold stock in the company. Sukbuntherng is an employee of Pharmacyclics LLC and holds AbbVie stock.
Ethical approval
This study was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and are consistent with Good Clinical Practices and applicable regulatory requirements. The study protocol was approved by the Independent Ethics Committee or Institutional Review Board at the study center. The study is registered at clinicaltrials.gov (NCT02638116).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
280_2018_3613_MOESM1_ESM.tif
Supplementary Figure S1 PK profile fits and steady-state PK profiles (bottom) for ibrutinib 560 mg alone and in combination with omeprazole (TIF 1788 KB)
280_2018_3613_MOESM3_ESM.tif
Supplementary Figure S3 Concentration–time curve (with standard deviation bars) of ibrutinib after administration of a single oral dose of ibrutinib 560 mg alone (day 1) and in combination with omeprazole 40 mg once daily (day 7) (TIF 1189 KB)
280_2018_3613_MOESM4_ESM.tif
Supplementary Figure S4 Local sensitivity analysis for BTK half-life (top), kon (middle), and kinact (bottom) (TIF 1571 KB)
Rights and permissions
About this article
Cite this article
de Jong, J., Haddish-Berhane, N., Hellemans, P. et al. The pH-altering agent omeprazole affects rate but not the extent of ibrutinib exposure. Cancer Chemother Pharmacol 82, 299–308 (2018). https://doi.org/10.1007/s00280-018-3613-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-018-3613-9