Abstract
Background
Everolimus, an mTOR inhibitor, is active in refractory lymphomas. However, toxicity with flat dosing limits its usage. Speculatively, pharmacokinetically-targeted dosing could improve tolerability. Therefore, we studied serum-trough dosing with rituximab as maintenance after high-dose cyclophosphamide (HDC) consolidation in lymphoma patients.
Patients/methods
After HDC, everolimus was dosed to serum trough levels (goal 3–15 ng/mL), with quarterly rituximab infusions for 1 year while maintaining < grade II non-hematologic and < grade III hematologic toxicities. Adult patients in first PR/CR with: mantle cell, transformed, double-hit, or high risk chronic lymphocytic leukemia or in second PR for any relapsed B cell lymphoma were eligible. Prophylaxis was given for encapsulated organisms, HSV and PCP. Serum IgG levels were maintained > 500 mg/dL.
Results
49 patients, median age: 59.0 years enrolled; MCL (26), CLL (10), transformed lymphoma (7), and other histologies (6). During the life of the study, the most frequent everolimus dosing has been 2.5 mg daily or 2.5 mg every other day; at these doses, serum levels are within the therapeutic range and non-hematologic toxicity is rare. At a median follow-up of 27.1 months, three patients remain on active therapy. Two patients withdrew secondary to potentially-attributable adverse events including a bacterial pneumonia and a viral pneumonia; this low rate of discontinuation compares well to other long-term everolimus trials. While a 58 and 76% EFS at 30 months for the entire cohort and MCL cohort, respectively, compares similarly to previously published HDC/rituximab data, longer follow-up is required.
Conclusions
Pharmacokinetically-targeted dosing appears to increase everolimus tolerability. This finding may be applicable to other patient populations.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
The mammalian target of rapamycin (mTOR) is a kinase vital to numerous intracellular signaling pathways, including those regulating cell growth and proliferation [1]. The oral rapalog everolimus inhibits the TORC1 (mTOR/raptor protein complex) pathway [2]. While everolimus is active in relapsed refractory lymphomas [3,4,5], the toxicities associated with prolonged, flat-fixed dosing schedules limit its use [6]. Safety reports, often based on everolimus use as an immunosuppressive agent in solid organ transplants indicate that serum everolimus ranges 3–15 ng/mL maximizes activity and levels > 15 ng/mL are associated with high rates of toxicity [7,8,9]. Therefore, in this safety trial, the same therapeutic target range was adopted. We hypothesized that dosing targeted to achieve serum concentrations in the therapeutic range might lessen toxicity while maintaining efficacy.
We evaluated 1-year of everolimus maintenance after consolidation with high-dose cyclophosphamide (HDC) [10] in B-cell lymphoma patients. Given evidence that rituximab augments everolimus in vitro we also included rituximab in the maintenance regimen [11, 12]. The HDC consolidation platform was chosen to evaluate this maintenance strategy in hopes that therapy at the time of maximum cytoreduction might augment benefit. We suspect that assessment of efficacy and toxicity of novel therapies in patients with refractory disease may lead to confounding that overestimates toxicity and underestimates efficacy. Here, we present our toxicity and early outcome data.
Methods
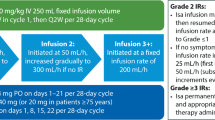
This study was designed to determine the safety of maintenance rituximab and prolonged mTOR inhibition with everolimus in CD20+, B-cell lymphomas after HDC consolidative therapy. Maintenance treatment consisted of rituximab 375 mg/m2 every 90 days (four infusions) and oral everolimus daily for 1 year. Maintenance therapy was initiated after hematologic recovery during a window period of 6–11 weeks after the start HDC (50 mg/kg/day cyclophosphamide for four consecutive days) to allow for full hematopoietic recovery. Everolimus, supplied by Novartis, was taken in the evening and trough levels were obtained with morning labs every 14 days for the first 90 days and then monthly. Patients kept medication diaries to record compliance and consented for 3 years of follow-up. Everolimus levels were determined by whole blood mass spectrometry utilizing an Endura Mass Spectometer [13].
If everolimus dose-adjustments were made, serum levels were then obtained in 14 days and then returned to monthly screening if levels were within target range. For everolimus levels below or exceeding 3.0–15.0 ng/mL, in the absence of III-IV grade non-hematologic toxicity (CTCAE version IV), everolimus was either increased or decreased by 2.5 mg per day to bring levels within range. For non-hematologic grade ≥ III toxicities, everolimus was held until the toxicity was ≤ II and restarted − 2.5 mg/day. For hematologic grade ≥ III toxicity management, please see addendum (1) For the management of stomatitis, non-infectious pneumonitis, and hyperlipidemia/hyperglycemia, please see addendum (2) The lowest everolimus dose allowed was 2.5 mg every fourth day.
Through day 365, Herpes and Pneumocystis jiroveci primary prophylaxis were mandated and serum IgG levels, checked monthly, were maintained > 500 mg/dL with IVIg. Re-immunizations started on day + 395: addendum 3.
After IRB approval (NCT01665768) this protocol was activated in September 2012 and was planned to evaluate over 3 years approximately 60 subjects. Eligible patients included those ≥ 18 years of age who received HDC for mantle cell lymphoma (MCL) in first partial response (PR) or greater, high risk chronic lymphocytic leukemia (CLL): del (17p; 11q) or unmutated IGHV sequence in first PR or greater, gray zone or double hit lymphoma in first complete response (CR), or any low grade CD20+ lymphoma in second PR. Stopping rules were established for unmanageable toxicities requiring protocol discontinuation. Patients with active Hepatitis C and HIV were excluded from participation. All grade toxicities were recorded through 8/23/13 [a median of 135 (range 21–330) patient days] for the first 13 patients; therefore, only grade III/IV toxicities were record. Data were locked on January 26th 2017 for this analysis.
The expected accrual rate for this study was to be 20 patients per year. The safety objective of this trial was based on the precision of estimating grade 3 or higher toxicities. We had determined sixty patients will allow us to estimate the proportion of patients experiencing grade 3 or higher toxicities with a precision of ± 13%. As everolimus dose would be managed to target a therapeutic window, toxicity evaluation in this study were based on events that would indicate either the therapeutic dose was too toxic to maintain or that this method increased the probability of unexpected complications. These events include any patient for which the minimum everolimus dose was not tolerable or any unexpected hospitalizations during protocol participation. If it becomes evident that the proportion of failures convincingly exceeds 15%, the study would have been halted for a safety consultation.
During the life of the study several key protocol amendments were IRB approved. The initial starting dose of everolimus was 10 mg nightly. Given the near universal serum levels above target range; this was reduced to 5.0 mg and then, again, reduced to 2.5 mg nightly (starting with subject 51). Trimethoprim sulfamethoxazole served our primary prophylaxis for P. jiroveci infection; after an encapsulated bacterial infection occurred while on dapsone as primary P. jiroveci prophylaxis, encapsulated gram positive coverage with amoxicillin was recommended for sulfa allergic patients. After the enrollment of the seventh patient, to reduce the incidence of rituximab induced neutropenia; rituximab was not given if the ANC was < 1500 K/mL on the day of planned infusion. After IRB approval, one patient participated whose ANC was 1500 K/mL at the start of maintenance therapy and one patient’s maintenance was delayed until day + 90 to allow for the resolution of diabetic ketoacidosis.
Results
Between September 2012 and November 2016, 56 patients consented and 49 patients received study treatment. Among the patients who did not receive study treatment, two had disease progression before scheduled initiation of study treatment and seven were ineligible for study treatment as a result of cytopenias. From this point on, the analysis refers only to patients who received study treatment. The median age of the 49 patients who started maintenance therapy was 59.0 (range 37.0–72.3) years. The median time between the first day of consolidation and the first day of maintenance was 65 (range 44–92) days for the entire group and 64 (range 50–89) for the MCL cohort. Thirty-five of 49 patients (71.4%) were treated with HDC/mTOR in first response. The baseline characteristics of these patients are in Table 1.
MCL was the diagnosis in 26 of 49 patients (53%). Their median age at the time of consolidation was 59.4 (range 47.7–72.3) years. Six (23.0%) were older than 65 years. Before induction treatment, IGHV sequencing revealed nine (34.6%) subjects with an unmutated sequence, four with a mutated sequence, four with an indeterminate sequence and nine patients did have this testing performed. Induction therapy included BRx6 (4), BR x4 (10), BRx3 (6), RCHOP x4 (1), RCHOP x6 (2), FCR x4 (1), HyperCVAD (2). 24/26 (92.3%) were treated with HDC in first response.
CLL was the diagnosis in 10 of 49 patients (20.0%). Their median age at the time of consolidation was 59.4 (range 49.2–68.2) years. Before consolidative treatment, nine patients (90%) had an unmutated IGHV sequence, 8 had del(11q) and none had del(17p) as determined by fluorescence in-situ hybridization. Eight patients were in partial response (PR) before the start of HDC and remained in PR at the start of maintenance therapy. Forty percent of patients were treated with HDC in first response.
Transformed diffuse large B cell lymphoma was the diagnosis in 7 of 49 patients (14.3%) with median age 62.5 (range 47.8–70.5) years. Four (57.1%) patients were treated in first response (presentation or indication for treatment was the concurrent diagnosis of diffuse large B cell lymphoma). Five patients were in CR (for all histologies) before the start of HDC and six were in CR before the start of maintenance therapy.
Retention of protocol participation during active maintenance therapy
One year of maintenance therapy was completed in 71.4% of patients. Two patients (4%) stopped maintenance therapy due to the potentially-attributable adverse events of H. influenza bacteremia and metapneumovirus pneumonia after 11 and 9 months of participation, respectively. No other patients discontinued participation secondary to everolimus or rituximab toxicity. Two patients with documented large granular lymphocytosis (LGL) mediated cytopenias before maintenance participated; however, both were removed from study as their LGL persisted and required additional immunosuppressive therapy. Seven (14.3%) patients were taken off of study for disease progression. Three (6%) subjects remain on active therapy.
Toxicities
Hematologic toxicities were common. At least one episode of grade III/IV neutropenia, thrombocytopenia or anemia was experienced by 30 (61.2%), 8 (16.3%) and 4 (8.2%) patients, respectively. Most non-hematologic toxicities were grade I/II. The expected grade III/IV toxicities of hyperglycemia 9 (18.4%), hypertriglyceridemia 9 (18.4%) and oral ulcers 3 (6.1%) were readily responsive to treatment. Table 2, summarizes all grade I-II encountered by the first 13 patients and all grade III-IV toxicities for the entire group. Three patients were hospitalized for bacterial sepsis: two during active therapy and another 1.8 years after the completion of maintenance therapy. One patient was briefly hospitalized for culture negative neutropenic fever and four other patients were transiently hospitalized for non-life threatening conditions. Hypogammaglobinemia with a serum IgG < 500 mg/dL was experienced by 14 (28.6%) patients. For those requiring IVIg replacement, a median of 2 (range 1–6) IVIg infusions were given.
Dose interruptions due to elevated serum everolimus levels or adverse events
46 patients have completed active maintenance therapy; they were instructed to hold 9.1% (range 0.0–56.4%) of their planned doses. Reducing the initial everolimus dosing from 10 mg (n = 6) to ≤ 5.0 mg (n = 40) daily reduced the held doses from 14.1 to 8.5%. During the life of the study, the most frequent everolimus dosing has been 2.5 mg daily or 2.5 mg every other day. Patients received 97.31% of planned doses. For the six patients whose starting everolimus dose was 10 mg daily, five required a dose reduction during their first month of therapy for asymptomatic supratherapeutic serum levels. For the 37 patients whose starting everolimus dose was 5 mg daily, only three patients completed the 12 months of planned maintenance therapy without requiring a dose modification. 31 (84%) required dose modifications, including 11 (29%) for asymptomatic supratherapeutic serum everolimus levels, their median time to first dose modification was 40 days. The median of scheduled rituximab doses held due to toxicity was 0% (range 0–75%) with 14 patients missing ≥ 50% of the scheduled doses. During the study period, no medication interactions were apparent that influenced everolimus serum levels. However, co-administration of strong CYP3A4 inhibitors was avoided and the co-administration of moderate CYP3A inhibitors (i.e. clarithromycin) were limited.
Oncologic outcomes
The median OS for the 49 patients has not been reached (Fig. 1) with a 30 month OS of 93% (95% CI 85, 100). The overall median EFS is 36.4 months and the 30 months EFS is 58% (95% CI 45, 76). The 30 month EFS for CLL, transformed lymphoma and MCL are 27% (95% CI 9, 80), 57% (95% CI 30, 100) and 76% (95% CI 60, 98), respectively (Figs. 2, 3). Of the eight (80%) CLL patients who relapsed: two have not required additional therapy, three have their disease controlled with ibrutinib, two underwent alloBMT and are in remission and one acquired a deletion 17p mutation and is being evaluated for alloBMT. Three (43%) transformed lymphoma patients relapsed; one has died; one underwent alloBMT and is in CR and one relapsed and is back in CR after relapsing with his lymphocyte predominate Hodgkin lymphoma. Five (20%) MCL patients relapsed and three of these patients died and one is being evaluated for alloBMT.
Discussion
Everolimus is an mTOR inhibitor clinically used as an antineoplastic for renal cell carcinoma, breast cancer, and pancreatic derived neuroendocrine tumors [14]. mTOR inhibition can directly reduce tumor growth and proliferation and can indirectly act as an anticancer agent by angiogenesis inhibition.
This trial was designed to assess tolerability and efficacy. With regard to tolerability, the toxicity experienced in our heavily pre-treated patient cohort was comparatively low and only two patients discontinued maintenance treatment because of toxicity potentially associated with drug. While accrual was not met, as the 3 years open enrollment period ended, had remainder of the expected patients enrolled, given the observed the low discontinuation rate due to toxicity, the safety stopping rules of this protocol would have not been likely been met. The most common toxicities associated with protocol treatment were hematologic which may be attributable to either rituximab or everolimus or the combination. Neutropenia is a well-established complication of rituximab [15, 16]. We note that everolimus dose interruption became less frequent as the initiation dose was decreased from 10 to 2.5 mg and the rituximab hold parameter was instituted. Importantly, the most commonly prescribed dosing schedules of everolimus to maintain adequate serum levels while limiting grade II toxicities were 2.5 mg daily and 2.5 mg every other day, with nearly all patients for the majority of time maintaining serum levels ≥ 5 ng/dL. A single patient required 2.5 mg every fourth day to limit toxicity and still maintain in the targeted everolimus serum level range. This contrasts sharply with the recommended starting dose of 10 mg daily. The diversity of patients in this protocol adds to the safety interpretation as mTOR inhibition toxicity is not malignancy-dependent but results from the medications off-target effects.
As a class, mTOR inhibitors have well known drug–drug interactions and toxicity. Concurrent use of CYP3A4 and/or PgP inhibitors can increase serum levels and toxicity, while CYP3A4 and/or PgP inducers can lower serum levels. mTOR inhibition is associated with stomatitis, fatigue, infections, non-infectious pneumonitis, viral reactivation, cytopenias, electrolyte abnormalities, hyperglycemia and hyperlipidemia.
Everolimus has been studied in the treatment of many malignancies and in combinations with other biologics and or chemotherapeutics [6, 17,18,19,20]. Importantly, nearly all trials evaluating everolimus have utilized a flat dosing schedule, were utilized in the relapsed refractory setting and designed for a relatively short medication time exposure [21, 22]. With a flat dosing schedule, not only are Grade III/IV mTOR induced hematologic toxicities common but a third of patients experience stomatitis which can impact adherence and life quality [23]. Many everolimus trials report a 10% adverse event discontinuation rate and some studies were closed secondary to adverse events [24,25,26,27,28]. The Pillar-2 trial randomized DLBCL patients in PET confirmed CR1 who had received R-CHOP or R-EPOCH (5–8 cycles) with an ECOG performance status of 0–2 to everolimus 10 mg daily for one year or placebo. While the 2-year DFS was the same in both arms, grade III/IV stomatitis was significantly more common in the everolimus group there was a 52% discontinuation rate in the everolimus arm versus a 33% discontinuation rate in the placebo arm, secondary to adverse events [29]. Longer follow-up is required to determine if everolimus maintenance will improve event free survival as compared to our previous HDC consolidative trial [10].
As supported this trial, therapeutic drug monitoring may avert serious adverse events [30,31,32] and thus allow for protracted everolimus use. As cytopenias were the most commonly encountered toxicity in this trial, which was potentially attributable to rituximab and their considerable previous therapy, it is likely that a higher serum everolimus level should be well tolerated. This report supports serum-based dosing can lessen everolimus toxicities in lymphoma patients and is likely applicable to other patient populations.
References
Petroulakis E, Mamane Y, Le Bacquer O et al (2007) mTOR signaling: implications for cancer and anticancer therapy. Br J Cancer 96:R11–R15
Hartford CM, Ratain MJ (2007) Rapamycin: something old, something new, sometimes borrowed and now renewed. Clin Pharmacol Ther 82:381–388
Wang M, Popplewell LL, Collins RH Jr et al (2014) Everolimus for patients with mantle cell lymphoma refractory to or intolerant of bortezomib: multicentre, single-arm, phase 2 study. Br J Haematol 165:510–518
Conconi A, Raderer M, Franceschetti S et al (2014) Clinical activity of everolimus in relapsed/refractory marginal zone B-cell lymphomas: results of a phase II study of the International Extranodal Lymphoma Study Group. Br J Haematol 166:69–76
Witzig TE, Reeder CB, LaPlant BR et al (2011) A phase II trial of the oral mTOR inhibitor everolimus in relapsed aggressive lymphoma. Leukemia 25:341–347
Yardley DA, Bosserman LD, O’Shaughnessy JA et al (2015) Paclitaxel, bevacizumab, and everolimus/placebo as first-line treatment for patients with metastatic HER2-negative breast cancer: a randomized placebo-controlled phase II trial of the Sarah Cannon Research Institute. Breast Cancer Res Treat 154:89–97
Kirchner GI, Meier-Wiedenbach I, Manns MP (2004) Clinical pharmacokinetics of everolimus. Clin Pharmacokinet 43:83–95
Yee KW, Zeng Z, Konopleva M et al (2006) Phase I/II study of the mammalian target of rapamycin inhibitor everolimus (RAD001) in patients with relapsed or refractory hematologic malignancies. Clin Cancer Res 12:5165–5173
Shipkova M, Hesselink DA, Holt DW et al (2016) Therapeutic Drug monitoring of everolimus: a consensus report. Ther Drug Monit 38:143–169
Gladstone DE, Bolanos-Meade J, Huff CA et al (2011) High-dose cyclophosphamide and rituximab without stem cell transplant: a feasibility study for low grade B-cell, transformed and mantle cell lymphomas. Leuk Lymphoma 52:2076–2081
Wanner K, Hipp S, Oelsner M et al (2006) Mammalian target of rapamycin inhibition induces cell cycle arrest in diffuse large B cell lymphoma (DLBCL) cells and sensitises DLBCL cells to rituximab. Br J Haematol 134:475–484
Haritunians T, Mori A, O’Kelly J et al (2007) Antiproliferative activity of RAD001 (everolimus) as a single agent and combined with other agents in mantle cell lymphoma. Leukemia 21:333–339
Yu B, DiBussolo J, Van Natta K, Kozak M (2014) Quantitation of immunosuppressant drugs in whole blood using the prelude-SPLC system and TSQ endura mass spectrometer for reasearch. https://assets.thermofisher.com/TFS-Assets/CMD/Application-Notes/AN-64043-Immunosupressants-Whole-Blood-AN604-EN-HR.pdf. Accessed 1 Oct 2017
Novartis (2016) Affinitor (everolimus) tablets prescribing information. https://www.pharma.us.novartis.com/sites/www.pharma.us.novartis.com/files/afinitor.pdf. Accessed 1 Oct 2017
Nitta E, Izutsu K, Sato T et al (2007) A high incidence of late-onset neutropenia following rituximab-containing chemotherapy as a primary treatment of CD20-positive B-cell lymphoma: a single-institution study. Ann Oncol 18:364–369
Tesfa D, Palmblad J (2011) Late-onset neutropenia following rituximab therapy: incidence, clinical features and possible mechanisms. Expert Rev Hematol 4:619–625
Kim SJ, Shin DY, Kim JS et al (2016) A phase II study of everolimus (RAD001), an mTOR inhibitor plus CHOP for newly diagnosed peripheral T-cell lymphomas. Ann Oncol 27:712–718
Ghobrial IM, Redd R, Armand P et al (2015) Phase I/II trial of everolimus in combination with bortezomib and rituximab (RVR) in relapsed/refractory Waldenstrom macroglobulinemia. Leukemia 29:2338–2346
McRee AJ, Davies JM, Sanoff HG et al (2014) A phase I trial of everolimus in combination with 5-FU/LV, mFOLFOX6 and mFOLFOX6 plus panitumumab in patients with refractory solid tumors. Cancer Chemother Pharmacol 74:117–123
Kanesvaran R, Watt K, Turnbull JD et al (2015) A Single-Arm Phase 1b Study of everolimus and sunitinib in patients with advanced renal cell carcinoma. Clin Genitourin Cancer 13:319–327
Witzig TE, Reeder C, Han JJ et al (2015) The mTORC1 inhibitor everolimus has antitumor activity in vitro and produces tumor responses in patients with relapsed T-cell lymphoma. Blood 126:328–335
Powles T, Wheater M, Din O et al (2016) A Randomised Phase 2 Study of AZD2014 versus everolimus in patients with VEGF-refractory metastatic clear cell renal cancer. Eur Urol 69:450–456
Rugo HS, Pritchard KI, Gnant M et al (2014) Incidence and time course of everolimus-related adverse events in postmenopausal women with hormone receptor-positive advanced breast cancer: insights from BOLERO-2. Ann Oncol 25:808–815
Motzer RJ, Alyasova A, Ye D et al (2016) Phase II trial of second-line everolimus in patients with metastatic renal cell carcinoma (RECORD-4). Ann Oncol 27:441–448
Yao JC, Fazio N, Singh S et al (2016) Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet 387:968–977
Hurvitz SA, Andre F, Jiang Z et al (2015) Combination of everolimus with trastuzumab plus paclitaxel as first-line treatment for patients with HER2-positive advanced breast cancer (BOLERO-1): a phase 3, randomised, double-blind, multicentre trial. Lancet Oncol 16:816–829
Motzer RJ, Escudier B, McDermott DF et al (2015) Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med 373:1803–1813
Choueiri TK, Escudier B, Powles T et al (2015) Cabozantinib versus everolimus in advanced renal-cell carcinoma. N Engl J Med 373:1814–1823
Witzig TE, Tobinai K, Rigacci L et al (2016) PILLAR-2: A randomized, double-blind, placebo-controlled, phase III study of adjuvant everolimus (EVE) in patients (pts) with poor-risk diffuse large B-cell lymphoma (DLBCL). J Clin Oncol 34:7506–7506
Duran I, Goebell PJ, Papazisis K et al (2014) Drug-induced pneumonitis in cancer patients treated with mTOR inhibitors: management and insights into possible mechanisms. Expert Opin Drug Saf 13:361–372
Deppenweiler M, Falkowski S, Saint-Marcoux F et al (2017) Towards therapeutic drug monitoring of everolimus in cancer? Results of an exploratory study of exposure-effect relationship. Pharmacol Res 121:138–144
Laborde L, Oz F, Ristov M et al (2017) Continuous low plasma concentrations of everolimus provides equivalent efficacy to oral daily dosing in mouse xenograft models of human cancer. Cancer Chemother Pharmacol 80(4):869–878
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No financial or other conflicts of interest to disclose.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schoch, L.K., Asiama, A., Zahurak, M. et al. Pharmacokinetically-targeted dosed everolimus maintenance therapy in lymphoma patients. Cancer Chemother Pharmacol 81, 347–354 (2018). https://doi.org/10.1007/s00280-017-3499-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-017-3499-y