Abstract
Purpose
The aim of the study was to evaluate the safety and determine the maximum tolerated dose (MTD) of intravenous catumaxomab, a trifunctional bispecific antibody that binds to EpCAM on epithelial cancer cells and CD3 on T cells.
Methods
The trial was a dose-escalation study with a 3 + 3 design in epithelial cancers with known EpCAM expression. The dose-limiting toxicity (DLT) period consisted of 4 weeks, with weekly intravenous administration of catumaxomab. Key DLTs were ≥grade 3 optimally treated non-hematological toxicity; ≥grade 3 infusion-related reactions refractory to supportive care; ≥grade 3 increase in liver enzymes and/or bilirubin not resolving to grade 2.
Results
Sixteen patients were enrolled receiving doses of 2 (n = 5), 4 (n = 3), 7 (n = 7) and 10 µg catumaxomab (n = 1). The most common treatment-emergent adverse events (TEAEs) were chills (93.8 %) and pyrexia (87.5 %). The most common TEAE of grade ≥3 was transient dose-dependent increases in aspartate aminotransferase (56.3 %). The intensity of toxicities decreased with the number of infusions. Also, serum IL-6 increased in a dose-dependent manner and reverted to low or undetectable levels after four infusions. A reversible decrease in liver function test (prothrombin time) at the 7-µg dose level was considered a DLT. The first patient at 10 µg experienced a fatal hepatic failure related to catumaxomab that led to the termination of the study.
Conclusions
The MTD of weekly intravenous catumaxomab was 7 µg. Major toxicities were cytokine release-related symptoms and hepatotoxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The epithelial cell adhesion molecule (EpCAM) is a transmembrane glycoprotein expressed in normal epithelium, certain squamous carcinomas, and in most adenocarcinomas including colorectal, gastric, esophageal, lung, ovarian, endometrial, breast and pancreas cancer [1–4]. Based on this wide variety of EpCAM expressing tumor types, EpCAM has been suggested as an attractive molecule for targeted anticancer therapy [1, 5, 6].
Catumaxomab (anti-EpCAM x anti-CD3) is a trifunctional bispecific antibody that binds to the EpCAM antigen and the CD3 antigen on T cells via its two antigen-binding sites. In addition, catumaxomab binds to Fcγ-receptor type I-, IIa-, and III-positive accessory cells, such as macrophages and natural killer cells via a functional Fc region. Catumaxomab consists of a mouse immunoglobulin G (IgG)2a and a rat IgG2b part [7]. The simultaneous activation of different immune effector cells (T cells and accessory cells) at the tumor site results in efficient killing of tumor cells by perforin-mediated lysis, antibody-dependent cellular toxicity, phagocytosis and cytotoxicity related to release of cytokines [8–12]. Catumaxomab was approved in the European Union in April 2009 for the intraperitoneal (i.p.) treatment of malignant ascites [13] based on a randomized trial showing that catumaxomab in combination with paracentesis significantly decreases the need for ascites drainage compared to control with paracentesis alone [14]. Adverse reactions were generally manageable and reversible with cytokine release-related syndrome, transient increases in liver parameters and decreases in lymphocyte counts as the most frequent events. Interestingly, an explorative sub-group analysis showed a survival benefit for gastric cancer patients in the catumaxomab arm compared to the control arm [14]. Furthermore, in isolated cases, regression of distant metastases was noted following intraperitoneal administration [15, 16]. Both observations indicate that local intraperitoneal administration apart from the palliative effect might have additional systemic antitumor activity supporting the development of the more convenient intravenous administration route. So far, only limited experience with intravenous catumaxomab as single dose is available in non-small cell lung cancer [17]. Therefore, this phase I study evaluates the safety and toxicity of repetitive intravenously administered catumaxomab in solid tumor patients with progressive disease during or after standard therapy.
Patients and methods
Study aim
The primary objective of the study was to evaluate the safety and tolerability of intravenously administered catumaxomab in order to determine the maximum tolerated dose (MTD). Secondary objectives were to evaluate pharmacokinetics, pharmacodynamics and efficacy.
Study design
The trial was an open-label, dose-escalation study with a 3 + 3 design commonly applied in phase I trials [18]. Based on previous clinical data [17, 19], the starting dose of catumaxomab was 2 µg. Subsequent dose levels to be investigated were 4, 7, 10, 14, 19, 25, 33, 43 and 56 µg according to a modified Fibonacci sequence. No intrapatient dose escalation was allowed. The period to determine the dose-limiting toxicity (DLT) consisted of 4 weeks, including four single intravenous administrations of catumaxomab followed by 1 week for safety observation.
DLTs were defined as (1) any grade 3 treatment-related non-hematological toxicity or higher with duration of >3 days, except grade 3 events not optimally treated with standard medication; (2) any grade 3 infusion-related reactions or higher except for reversible grade 3 infusion-related reactions resolving with a reduced infusion rate, supportive care and/or the administration of corticosteroids; (3) inability to administer the next dose due to the persistence of a treatment-related adverse event; (4) grade 3 or higher increase in alanine aminotransferase (ALT), aspartate aminotransferase (AST) and/or bilirubin not resolved to grade ≤2 prior to next dosing (this criterion was added after the completion of the 2-µg dose cohort); (5) grade 4 neutropenia (ANC < 500/µl) for more than 7 days; (6) grade 3 or 4 febrile neutropenia; (7) grade 4 thrombocytopenia (platelet count <25,000/µl); (8) treatment delay >7 days in total for recovery from toxicity during the first four catumaxomab infusions within the DLT period. Fatigue grade 3 for ≤14 days and isolated laboratory abnormalities grade ≥3 that returned to baseline or grade 1 within 7 days were not considered DLT. After the completion of the 2-µg dose cohort, the study protocol was amended and laboratory abnormalities grade ≥3 deemed not clinically relevant as assessed by the investigator were not regarded as DLT. Dose escalation occurred if three patients within a cohort completed at least four doses of catumaxomab and no DLT was observed. Patients who completed less than four administrations of catumaxomab for non-DLT-related reasons were replaced. If one of three patients experienced DLT at a given dose level, an additional three patients were enrolled and treated at the same dose level before proceeding to the next dose level. If a second patient experienced a DLT, the MTD had been exceeded and the next lower dose level was determined as the MTD. Thus, the MTD was defined as the highest dose at which ≤1 of a maximum of six patients experienced DLT. After each dose level, a Dose Steering Board (DSB) reviewed the safety data from the DLT period and gave approval to escalate the dose to the next cohort. The study was conducted in accordance with the Declaration of Helsinki. Favorable opinion was obtained from the local independent ethics committees, and approval was given by the national health authorities. Written informed consent was obtained from each patient included in the study (EudraCT number: 2010-022974-15; ClinicalTrials.gov identifier: NCT01320020).
Patients
Patients with epithelial cancers with a known frequency of EpCAM expression of at least 80 % according to the literature [1, 2] and progressing on or after standard therapy were considered eligible for the study. Key inclusion criteria were age ≥18 years, ECOG performance status ≤1, adequate hematology, liver and renal function, negative pregnancy test in females, evaluable according to response evaluation criteria in solid tumors (RECIST). Patients were excluded from the study if they had known clinically symptomatic brain metastases, any known active or chronic infection, congestive heart failure (New York Heart Association class III or IV) or clinically relevant cardiac arrhythmia. Liver cirrhosis was amended as an exclusion criterion after the completion of the 2-µg cohort. Patients had to have discontinued immunosuppressive agents for at least 4 weeks. No systemic corticosteroids were allowed for at least 5 days prior to the first administration of catumaxomab.
Treatment
Catumaxomab was prediluted in an appropriate volume of 0.9 % sodium chloride solution and administered weekly as a 6-h constant rate intravenous infusion by means of a CADD-MS 3 ambulatory infusion pump (Smiths Medical). Concurrently with each catumaxomab infusion, 1000 mL 0.9 % sodium chloride solution was given intravenously to all patients. Recommended premedication for the suppression of cytokine release-related symptoms (CRRS) included non-steroidal anti-inflammatory agents (e.g., ibuprofen, diclofenac, metamizole), pethidine and/or paracetamol. When paracetamol was used, the daily dosage (defined as 24 h) was not allowed to exceeded 2000 mg. Corticosteroids were to be avoided unless in case of medical emergency. After completion of the DLT period, all patients were offered continuation of catumaxomab treatment at the same dose. The maximum length of treatment, however, was restricted to an additional 12 weeks after the DLT period, resulting in maximum treatment duration of 17 weeks in total (including at maximum 1 week for recovery from toxicity during the first four catumaxomab infusions).
Assessments
Safety parameters included recording of treatment-emergent adverse events (TEAEs) throughout the study period and the evaluation of the relationship to the study drug based on causality criteria (“certain,” “probable” and “possible” were considered as related to study drug and “unlikely” and “unrelated” as not related). The intensity of TEAEs was graded according to the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE), version 4.03. Assessment of laboratory safety parameters, physical examination, vital signs, 12-lead ECG and assessment of left ventricular ejection fraction by echocardiography or multi-gated acquisition scan were performed at screening and after the fourth infusion of catumaxomab. Tumor measurements were performed according to the RECIST 1.1 criteria every 8 weeks.
Blood samples for pharmacokinetic (PK) analyses were collected pre-dose, 1, 2, 4, 6, 9, 12, 24, 48 and 72 h after the second infusion. Limited PK sampling was done after all other infusions than the second infusion (e.g., pre-dose, 6 and 24 h). Catumaxomab plasma concentrations were measured using an enzyme-linked immunosorbent assay. Key PK parameters to be evaluated included maximum observed plasma concentration (C max), pre-dose plasma concentration (C min), observed time of maximum plasma concentration (T max), terminal half-life (t 1/2) and area under the plasma concentration–time curve (AUC). Parallel to the PK assessments, antidrug antibodies (ADA) were measured at the same time points as the PK samples using a double antigen-binding enzyme-linked immunosorbent assay.
Cytokines IL-2, IL-4, IL-6, IL-8, IL-10, IL-12, IFN-γ, TNF-α and GM-CSF were measured by flow cytometry using the commercially available CBA Flex Assay kits (Becton–Dickinson). Various subsets of immune cells from pre-dose blood samples were analyzed at the local laboratories using commercially available test kits.
Statistical analyses
A mixed model analysis was performed on logarithmic transformed data to assess the effect of dose and number of infusions on measured serum cytokines and transaminases. Log-rank analysis and the Kaplan–Meier method were used to compare time to the appearance of ADA in three cohorts. Cox univariate regression analysis was used to identify variables correlated to the appearance of ADA. The frequencies of CCRS after the first and last infusion in the DLT period were compared by the McNemar’s test. Correlation was assessed by Spearman’s analysis. All statistical analyses were done by use of SPSS version 19.
Results
Patients
From February 2011 to April 2012, 16 patients were enrolled at three centers in Denmark, Austria and Spain. The median age was 63 years (range 44–79). Twelve patients were male (75 %). Thirteen patients had colorectal cancer. The remaining three patients had ovarian cancer, bile duct cancer and adenocarcinoma of the gastro-esophageal junction. All patients had disseminated disease including seven patients with liver metastases. The most commonly used prior anticancer agents were 5-FU derivatives (15), oxaliplatin (10), irinotecan (9), bevacizumab (4), cetuximab (3), gemcitabine (3), carboplatin (3) and panitumumab (2). A histological assessment of the EpCAM status was not required according to study protocol, but was available for five patients, who all were EpCAM positive. Two of the 16 patients (13 %) completed the entire 16-week treatment period. Fourteen patients (88 %) prematurely terminated the study. Primary reasons for discontinuation were disease progression (8; 50 %), death (2; 13 %), DLT (1; 6 %), withdrawal of consent (1; 6 %), TEAEs other than DLT (1; 6 %) and termination of the study (1; 6 %). Four patients went off study after the first infusion without completing the DLT period, including one patient in the 2-μg cohort without resolution of transaminase increase prior to the second infusion, two patients in the 4-μg cohort with progressive disease and with increase in INR and one patient in the 10-μg cohort due to a fatal event. Patient demographics and baseline characteristics, cancer type and end of study status per dose cohort are detailed in Table 1.
Dose-limiting toxicity
In the 2-μg dose cohort, two of five patients experienced signs of impairment of liver function. A grade 3 hyperbilirubinemia that did not resolve to baseline or grade 1 within 1 week was observed in a 70-year-old male with adenocarcinoma of the rectum. Disease progression encompassing liver metastasis was evident in this patient, and elevated serum bilirubin levels were primarily attributed to biliary obstruction. Since the study treatment could not be excluded as contributing to the increase in serum bilirubin, the adverse event was graded provisionally as a possible DLT. A 63-year-old male patient in this cohort suffering from colorectal adenocarcinoma went off study after the first infusion, because he experienced a DLT with grade 3 increase in serum bilirubin and ALT which did not resolve to baseline or CTCAE grade 1 within 1 week. In view of these two potential DLTs, the inclusion of further patients into this cohort was stopped. The DSB considered the elevations of bilirubin and ALT in both patients as transient and fairly moderate, and in line with the reversible increase in liver parameters known from intraperitoneal administration of catumaxomab. The DSB regarded the changes in liver function parameters observed in the 2-μg cohort as not dose limiting and gave approval to proceed to the next dose level.
No DLTs were observed in the 4-μg dose cohort. The first patient of the 7-μg cohort experienced a drop in prothrombin time to 0.26, and an increase in international normalized ratio (INR) to 1.8, representing grade 2 toxicity. This new signal involving the synthesis function of the liver was considered possibly indicative of a more severe liver toxicity; thus, following a conservative approach, the event was considered a possible DLT, although formally it did not meet the DLT criteria. The alterations in coagulation parameters normalized within 2 days. Nonetheless, in a DSB meeting, it was decided to withdraw the patient from further treatment and to extend the cohort to six patients in order to gain more safety data in this cohort. One patient was replaced due to disease progression during the DLT period resulting in final size of seven patients in the cohort. None of the other patients from the 7-µg cohort had any DLT. The pattern of changes in liver function in the 7-µg cohort was similar to the preceding cohorts, i.e., transient increase in liver parameters that reversed to normal levels. Since no further DLT was observed in the 7-µg cohort, dose escalation was performed according to the protocol.
The first patient enrolled in the 10-μg cohort was a 49-year-old female with a sigmoid carcinoma with multiple lung metastases but no involvement of the liver. Prior chemotherapy consisted of leucovorin, 5-FU, capecitabine, oxaliplatin, irinotecan and bevacizumab. During treatment with irinotecan, she developed a persistent grade 1 increase in transaminases and her baseline CT scan showed steatosis which was confirmed postmortem. She experienced CRRS and severe hepatotoxicity leading to acute hepatic failure. Despite all salvage measures, this event was fatal within 24 h of catumaxomab infusion. The investigator classified the event as certainly related to study drug. The study was immediately put on hold and subsequently terminated in accordance with the DSB. Dose level 7 µg was declared the MTD.
Overall safety and tolerability
A total of 494 TEAEs were observed, and all patients experienced at least one TEAE. Of these, the majority (367, 74 %) were considered to be treatment-related. The most common TEAEs (Table 2) were CRRS like chills (94 % of patients), pyrexia (88 %), vomiting (63 %) and nausea (63 %). Other frequently reported TEAEs were increased hepatic enzymes such as alkaline phosphatase (69 % of patients), AST (63 %), gamma-glutamyltransferase (GGT) (63 %) and ALT (56 %), as well as decreased appetite (50 %), fatigue (50 %) and hyperbilirubinemia (44 %). Transaminase increase lasted in general less than 1 week returning to base line or grade 1 before the next infusion, except in two patients in accordance with the serum elimination half-life for ALT and AST of 44 and 17 h, respectively [20]. In contrast, elevations in GGT, alkaline phosphatase and bilirubin lasted beyond 1 week reflecting their longer serum elimination half-life. A dose-dependent increase in the peak of transaminases was observed (p < 0.0001). The frequency of TEAEs per patient appeared to decrease over the four infusions in the DLT period. In the 7-µg cohort, a significant reduction in patients experiencing CCRS was recorded comparing the first infusion to the last infusion in the DLT period (p = 0.031). The frequency decreased from seven patients to one patient with CCRS out of a total seven patients. In the smaller 4-µg cohort, the CCRS frequency dropped nonsignificantly from 3/3 to 1/3. In a mixed model analysis, the peak elevation of AST (p = 0.003) and ALT (p = 0.008) decreased significantly across cohorts as more infusions were delivered during the DLT period (data not shown).
Most of the TEAEs (78 %) were of grade 1 or 2 severity, and 22 % of TEAEs were grade ≥3. All 16 patients had at least one TEAE of grade ≥3. The most commonly reported TEAE of grade ≥3 were increased AST (56 %), increased GGT (44 %), decreased lymphocyte count (38 %) and hypertension (38 %).
Ten serious adverse events (SAEs) were reported in seven patients (44 %), five of these SAEs observed in four patients were considered treatment-related. Treatment-related SAEs comprised liver toxicity (acute hepatic failure, abnormal hepatic function, hyperbilirubinemia and increased hepatic enzymes) and pyrexia. No apparent associations between liver toxicity and existing liver metastases, prior liver resection or hepatotoxic chemotherapy, were noted. All SAEs occurred after the first administration of catumaxomab. Fatal outcomes of SAEs were seen in two patients: one patient in the 2-µg cohort died due to intestinal occlusion secondary to peritoneal metastases considered unrelated to study drug, whereas the patient of the 10-µg cohort died due to acute hepatic failure, which was considered to be related to catumaxomab treatment. Three SAEs led to the discontinuation of treatment; these SAEs were hyperbilirubinemia, abnormal hepatic function and the fatal acute hepatic failure.
None of the patients was positive for antidrug antibodies (ADA) prior to the first catumaxomab treatment. By the end of the study, eight patients (50 %) were positive for ADA. Study drug-related TEAEs were very rare (12 out of a total of 494 recorded TEAEs) in these ADA-positive patients while still receiving catumaxomab.
Efficacy
None of the patients had an objective response during the 16-week study period according to RECIST criteria. At the end of the observation period, two patients had stable disease (both in the 7-μg cohort) and nine patients had disease progression; the remaining five patients did not have an assessment at their end of study visit either due to premature discontinuation after first administration of catumaxomab (4) or due to termination of the study (1).
Pharmacokinetics and pharmacodynamics
Complete plasma concentration time profiles were only available in three patients because plasma concentrations of catumaxomab were below the lower limit of quantification (LLOQ) of the assay at later time points. Cmax occurred at or shortly after the end of the 6-h infusion of catumaxomab. No dose proportionality could be demonstrated with dose-normalized Cmax. Summary of pharmacokinetic parameters is presented in Table 3.
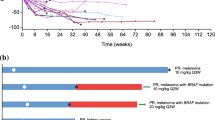
There was no obvious pattern of on-treatment changes for absolute and relative immune cell counts (T cells, helper T cells, cytotoxic T cells, B cells and NK cells). The predominant cytokines observed in all cohorts were IL-6 and IL-8, with maximum concentrations of these cytokines observed 6–9 h after the start of catumaxomab infusion. In a mixed model analysis, 6 h post-infusion serum IL-6 increased significantly (p < 0.001) in a dose-dependent manner (Fig. 1a). With increasing numbers of infusions, IL-6 reverted gradually to low or undetectable baseline values after four infusions (Fig. 1b, p = 0.004). IFN-γ and TNF-α appeared in the plasma in the majority of patients after the first infusion and became undetectable after the fourth infusion in all but two patients who had very low serum concentrations. Levels of IL-6, IL-8, IFN-γ and TNF-α, 6 h after the first infusion, were highly correlated with correlation coefficients ranging between 0.70 and 0.89 (p = 0.0001–0.001). Median time to onset of ADA was 21 (95 %CI 15–27), 28 (95 % CI 17–39) days and not reached for dose levels 7, 4 and 2 µg, respectively (p = 0.17, Fig. 2). In the 2-µg cohort, only one patient prior to the fourth administration showed ADA positivity, whereas all patients of the 4-µg cohort and four of seven patients of the 7-µg cohort had detectable ADA. In a univariate Cox regression analysis, the serum level of IL-6 after the first infusion was associated with the time to appearance of ADA (p = 0.044).
Discussion
This phase I study was designed to determine the MTD and to evaluate safety of intravenously infused catumaxomab in EpCAM-positive solid tumors. The study was terminated due to a fatal study drug-related event consisting of a possibly immune-mediated hepatic failure. The fatal event highlights the quite narrow therapeutic index of immune activating agents. In 2006, in a phase I study, all participating healthy volunteers treated with the potent T cell receptor superagonist TGN1412 experienced severe uncontrolled cytokine storms at the initial dose level [21]. Clearly, potent anticancer immunotherapies are generally faced with the challenge to manage and control these processes.
As part of the pharmacovigilance program of intraperitoneal catumaxomab, an analysis was undertaken to determine whether similar episodes were reported among patients registered in the safety database of the sponsor. Only single cases of hepatic failure related to catumaxomab had been reported since the beginning of the catumaxomab development program. However, transient increase in hepatic enzymes was commonly observed after the intraperitoneal administration. These changes in laboratory parameters were not clinically relevant and mostly returned to baseline after end of treatment.
The understanding of the differences between the intraperitoneal and intravenous administration may be key to avoid serious adverse effects of the intravenous catumaxomab application. A prominent difference between the two modes of application and schedules is the gradual increase in dose over four intraperitoneal administrations in a 10-day period as compared to the fixed intravenous dosing used in this trial. The gradual dose increase during the intraperitoneal administration was implemented to adapt the immune system to catumaxomab and mitigate unwanted systemic immune reactions. This adaptation was based on early experiences with intraperitoneal application, where it was found that lower starting doses were better tolerated compared to higher starting doses. The present data confirm that an adaptation of the immune system occurs with increasing number of intravenous administrations. SAEs only occurred after the first infusion and never following subsequent infusions. The frequency of CRRS as well as the peak in IL-6 and transaminases declined significantly along with increasing number of infusions. A similar but nonsignificant trend was observed for IL-8, IFN-γ and TNF-α. The cellular source of the cytokine release was not addressed in this study. However, ex vivo incubation of patient-derived peripheral blood mononuclear cells with catumaxomab led to substantial release of IFN-γ and TNF-α within the T cell CD4+/CD8+ population exceeded by co-incubation with EpCAM-positive cells [22], indicating that the observed increase in serum IFN-γ and TNF-α could be a result of a direct effect on T cells. The activation of macrophages/monocytes, NK cells or other accessory cells through the Fcγ-receptor is a mechanism for cytokine release involving IL-6 and IL-8 [23]. As catumaxomab recognizes Fcγ-receptor type I, IIa and III, IL-6 and IL-8 could possibly have been released from systemic as well as hepatic accessory immune cells, e.g., Kupffer cells. A possible mechanism behind the immune adaption could be mediated by a neutralizing effect of ADA as no CRRS were recorded in any patient after the appearance of circulating ADA. However, as similar results were observed after intraperitoneal administration of catumaxomab [14, 24] before appearance of ADA, it is likely that immune adaptation may occur independently from neutralizing effects. The pattern of decreasing infusion reactions with more infusions delivered is typical for the cytokine release syndrome. The mechanism is poorly understood but in most cases, the syndrome is mainly a first-dose phenomenon. For example, infusion reactions caused by rituximab decrease from 80 % after the first infusion to 40 % after subsequent infusions [23].
Differences in pharmacokinetics of the intraperitoneal and intravenous route could influence the toxicity profile. However, both terminal half-life and C max are in the same range for the two routes of administration (i.p. and i.v.) making it unlikely that the route of administration in itself plays a major role in this context. The slower release from the abdominal cavity and localized immunological processes in the abdominal cavity may contribute to a reduced systemic immune reaction and the generally better tolerability observed with intraperitoneal application.
Corticosteroids represent an established option to suppress immune hyper reactions. Varying doses of dexamethasone were used as pre-medication in a previous phase I trial evaluating single-dose intravenous catumaxomab given in NSCLC patients [17]. In this study, a dose of 5 µg catumaxomab with a pre-medication of 40 mg dexamethasone was determined as maximum tolerated dose (MTD). However, based on preclinical data, it can be anticipated that the co/pre-medication of corticosteroids can impair the potential anticancer effect of catumaxomab (data on file). Therefore, in the present study, the administration of corticosteroids was reserved for treatment of CTCAE grade ≥2 infusion reactions, whereas non-steroidal anti-inflammatory drugs were allowed as standard co/pre-medication.
No objective antitumor activity was observed in this trial. The lack of antitumor responses could be due to the small sample size or due to the fact that the preponderant tumor entity colorectal cancer did not respond to this approach. We acknowledge that late responses after initial increase in tumor burden occasionally observed after immunotherapy could be missed due to lack of appropriate follow-up period. A strong signal of survival benefit after repetitive intraperitoneal catumaxomab treatment has been observed in the subgroup of gastric cancer patients with malignant ascites enrolled in the pivotal randomized study [14]. Furthermore, intraperitoneal catumaxomab efficaciously reduced the need for ascites drainage even when retreated after an initial cycle of catumaxomab [25, 26].
The narrow therapeutic index reflected by the reported fatal drug-related event undoubtedly represents a major challenge calling for meticulous monitoring of liver function and caution if combined with potential hepatotoxic chemotherapy. Adaption of the immune response by gradual increase in catumaxomab dose or low-dose premedication with corticosteroids represents possible strategies to mitigate severe immunological reactions in the future development of catumaxomab for intravenous use.
References
Went P, Lugli A, Meier S et al (2004) Frequent EpCAM protein expression in human carcinomas. Hum Pathol 35:122–128
Went P, Vasei M, Bubendorf L et al (2006) Frequent high-level expression of the immunotherapeutic target EpCAM in colon, stomach, prostate and lung cancers. Br J Cancer 94:128–135
Spizzo G, Went P, Dirnhofer S et al (2004) High EpCAM expression is associated with poor prognosis in node-positive breast cancer. Breast Cancer Res Treat 86:207–213
Spizzo G, Went P, Dirnhofer S et al (2006) Overexpression of epithelial cell adhesion molecule (EpCAM) is an independent prognostic marker for reduced survival of patients with epithelial ovarian cancer. Gynecol Oncol 103:483–488
Balzar M, Winter MJ, de Boer CJ et al (1999) The biology of the 17-1A antigen (EpCAM). J Mol Mod 77:699–712
Pauli C, Muenz M, Kieu C et al (2003) Tumor-specific glycosylation of the carcinoma-associated epithelial cell adhesion molecule EpCAM in head and neck carcinomas. Cancer Lett 193:25–32
Lindhofer H, Mocikat R, Steipe B et al (1995) Preferential species-restricted heavy/light chain pairing in rat/mouse quadromas. Implications for a single-step purification of bispecific antibodies. J Immunol 155:219–225
Zeidler R, Reisbach G, Wollenberg B et al (1999) Simultaneous activation of T cells and accessory cells by a new class of intact bispecific antibody results in efficient tumor cell killing. J Immunol 163:1246–1252
Zhang S, Zhang HS, Cordon-Cardo C et al (1998) Selection of tumor antigens as targets for immune attack using immunohistochemistry: protein antigens. Clin Cancer Res 4:2669–2676
Riesenberg R, Buchner A, Pohla H et al (2001) Lysis of prostate carcinoma cells by trifunctional bispecific antibodies (alpha EpCAM x alpha CD3). J Histochem Cytochem 49:911–917
Zeidler R, Mysliwietz J, Csanady M et al (2000) The Fc-region of a new class of intact bispecific antibody mediates activation of accessory cells and NK cells and induces direct phagocytosis of tumour cells. Br J Cancer 83:261–266
Schmitt M, Schmitt A, Reinhardt P et al (2004) Opsonization with a trifunctional bispecific (alphaCD3 x alphaEpCAM) antibody results in efficient lysis in vitro and in vivo of EpCAM positive tumor cells by cytotoxic T lymphocytes. Int J Oncol 25:841–848
Seimetz D, Lindhofer H, Bokemeyer C (2010) Development and approval of the trifunctional antibody catumaxomab (anti-EpCAM x anti-CD3) as a targeted cancer immunotherapy. Cancer Treat Rev 36:458–467
Heiss MM, Murawa P, Koralewski P et al (2010) The trifunctional antibody catumaxomab for the treatment of malignant ascites due to epithelial cancer: results of a prospective randomized phase II/III trial. Int J Cancer 127:2209–2221
Petrelli F, Borgonovo K, Lonati V et al (2013) Regression of liver metastases after treatment with intraperitoneal catumaxomab for malignant ascites due to breast cancer. Target Oncol 8:291–294
Bezan A, Hohla F, Meissnitzer T et al (2013) Systemic effect of catumaxomab in a patient with metastasized colorectal cancer: a case report. BMC Cancer 13:618
Sebastian M, Passlick B, Friccius-Quecke H et al (2007) Treatment of non-small cell lung cancer patients with the trifunctional monoclonal antibody catumaxomab (anti-EpCAM x anti-CD3): a phase I study. Cancer Immunol Immunother 56:1637–1644
Le Tourneau C, Lee JJ, Siu LL (2009) Dose escalation methods in phase I cancer clinical trials. J Natl Cancer Inst 101:708–720
Ruf P, Kluge M, Jäger M et al (2010) Pharmacokinetics, immunogenicity and bioactivity of the therapeutic antibody catumaxomab intraperitoneally administered to cancer patients. Br J Clin Pharmacol 69:617–625
Amacher DE (1998) Serum transaminase elevations as indicators of hepatic injury following the administration of drugs. Regul Toxicol Pharmacol 27:119–130
Suntharalingam G, Perry MR, Ward S et al (2006) Cytokine storm in a phase 1 trial of the anti-CD28 monoclonal antibody TGN1412. N Engl J Med 355:1018–1028
Riechelmann H, Wiesneth M, Schauwecker P et al (2007) Adoptive therapy of head and neck squamous cell carcinoma with antibody coated immune cells: a pilot clinical trial. Cancer Immunol Immunother 56:1397–1406
Bugelski PJ, Achuthanandam R, Capocasale RJ et al (2009) Monoclonal antibody-induced cytokine-release syndrome. Expert Rev Clin Immunol 5:499–521
Burges A, Wimberger P, Kümper C et al (2007) Effective relief of malignant ascites in patients with advanced ovarian cancer by a trifunctional anti-EpCAM x anti-CD3 antibody: a phase I/II study. Clin Cancer Res 13:3899–3905
Pietzner K, Vergote I, Santoro A et al (2014) Re-challenge with catumaxomab in patients with malignant ascites: results from the SECIMAS study. Med Oncol 31:308
Thomaidis T, Wörns MA, Galle PR et al (2014) Treatment of malignant ascites with a second cycle of catumaxomab in gastric signet cell carcinoma—a report of 2 cases. Oncol Res Treat 37:674–677
Acknowledgments
We are grateful to the participating patients and their families. Professor Meinolf Karthaus (Chair) and Professor Lena Specht served as voting members of the Dose Steering Board. Statistician Ib Jarle Christensen is acknowledged for excellent statistical advice. The trial was sponsored by Neovii Biotech GmbH, formerly Fresenius Biotech GmbH. Medical writing assistance was provided by Neovii Biotech GmbH.
Conflict of interest
M.M.S served on an advisory board for Fresenius Biotech GmbH. C.D declares no potential conflict of interest concerning catumaxomab and its development. R.D declares no potential conflicts of interest. U.L declares no potential conflict of interest W.B declares no potential conflict of interest concerning catumaxomab and its development. H.M is an employee of Neovii Biotech GmbH. J.T declares no potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mau-Sørensen, M., Dittrich, C., Dienstmann, R. et al. A phase I trial of intravenous catumaxomab: a bispecific monoclonal antibody targeting EpCAM and the T cell coreceptor CD3. Cancer Chemother Pharmacol 75, 1065–1073 (2015). https://doi.org/10.1007/s00280-015-2728-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-015-2728-5